Abstract
In taste cells, taste receptors, their coupled G proteins, and downstream signaling elements mediate detection and transduction of sweet, bitter and umami compounds. In some intestinal endocrine cells, taste receptors and gustducin contribute to the release of glucagon-like peptide-1 (GLP-1) and other gut hormones in response to glucose and non-caloric sweeteners. Conversely, taste cells have been found to express multiple hormones typically found in intestinal endocrine cells, e.g. GLP-1, glucagon, somatostatin and ghrelin. By immunohistochemistry multiple subsets of taste cells were found to express GLP-1. The release of GLP-1 from “endocrine taste cells” into the bloodstream was examined. In wild-type mice, even after esophagealectomy and vagotomy, application of glucose to the tongue induced an elevation of GLP-1 in the bloodstream within 10 minutes of stimulation of the taste buds with glucose. Glucose stimulation of taste cell explants from wild-type mice led to release of GLP-1 into the medium. Knocking out the T1R3 gene did not eliminate glucose-stimulated GLP-1 release from taste cells in vivo. Our results indicate that a portion of the cephalic phase rise in circulating GLP-1 is mediated by direct release of GLP-1 from taste cells into the bloodstream.
Keywords: taste receptor, T1R3, glucagon-like peptide-1, cephalic phase
Introduction
Type I taste receptors (T1Rs), α-gustducin and other taste signaling elements well known for their roles in taste transduction have recently gained additional interest for their function in extra-oral tissues. In the proximal small intestine many taste signaling proteins have been found in enteroendocrine L cells where they are involved in secretion of glucagon-like peptide 1 (GLP-1) in response to sugars and non-caloric sweeteners(1). In colon, where many GLP-1-producing cells also express α-gustducin, it is not known which gustducin-coupled receptors might elicit GLP-1 release. Interestingly, GLP-1 and other proglucagon gene products also are expressed in taste cells. Indeed, many gut hormones and neuropeptides (e.g. serotonin, cholecystokinin (CCK), vasoactive intestinal peptide (VIP), and neuropeptide Y (NPY)), are expressed in taste cells and act on neighboring taste cells through paracrine effects(2,3,4). GLP-1 released from taste cells modulates taste sensitivity to sweet compounds and mice lacking the GLP-1 receptor show reduced responses to sweeteners in behavioral assays(5). Some taste receptor cells also express glucagon, and genetic or pharmacological disruption of glucagon signaling significantly reduces the taste preferences of mice for sugars(6).
The cephalic phase of digestive secretion, or “psychic reflex”, as Pavlov introduced it, is mediated by actions of the central and peripheral nervous systems. It has been determined that oral exposure to food initiates the cephalic phase of digestion. The cephalic phase of feeding is a set of conditional reflexes regulated by taste, odor and visual stimuli. At the peripheral level the cephalic phase is mediated by several hormones acting at the onset of digestive process before food is digested. Among the hormones shown to be released at this stage are insulin and ghrelin(7, 8). These hormones are thought to be released primarily from endocrine cells responding to nerve stimuli.
Here we show that GLP-1 secretion from the taste cells themselves may contribute to the anticipatory cephalic phase. In particular, sweet sensing taste cells may contribute important information about carbohydrate content of food and through secretion of GLP-1 help the organism prepare for post-cephalic phases of digestion.
Materials and Methods
Reagents
All chemicals were purchased from Sigma-Aldrich or Invitrogen unless otherwise specified.
Animals
T1R3 null (T1R3KO) mice were described previously(9). Mice were bred at Monell’s animal facility. Wild type (WT) controls were littermates or C57Bl/6 mice purchased from the Jackson Laboratory (Bar Harbor, ME). All mice, 12 to 16 week old males, were maintained on a 12h light, 12h dark cycle and fed standard rodent chow. All experimental protocols and procedures were approved by Monell’s Institutional Animal Care and Use Committee in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Immunohistochemistry
Immunohistochemistry of frozen circumvallate papilla sections was as described(10). The anterior tip and lingual tissues containing the foliate and circumvallate were dissected out and placed in fresh 4% paraformaldehyde for 1h at 4C. Tissue samples were then transferred to an ascending series of 10–30% sucrose (Sigma, St. Louis, MO) over two days for cryoprotection. Tissues samples were briefly rinsed in 0.1M phosphate buffer solution pH 7.4 (PBS), mounted in OCT and frozen in a 100% alcohol ice bath. Frozen sections were cut at a thickness of 5μm and mounted on Superfrost slides (Fisher, Waltham, MA). A double immunofluorescence technique was used to determine colocalization of GLP-1 and specific taste cell types. Labeling of primary antibodies was done sequentially in which anti-GLP-1 was incubated and labeled first then followed by a second primary for specific taste cell types. Briefly, 5μm frozen sections were dried in an oven at 45°C for 15 mins then rehydrated with 0.1M phosphate buffer solution pH 7.4 + 0.1% Triton X-100 (PBST). A mouse-on-mouse (M.O.M) kit was used (BMK-2202, Vector Laboratories, Burlingame, CA) to label mouse anti-GLP-1 (1:100, G2040-13Q, US Biological, Swampscott, MA). The mouse anti-GLP-1 antibody is directed against a full-length peptide (31 aa) corresponding to human GLP-1 according to manufacturer’s datasheet. Following the manufacturer’s protocol, a secondary streptavidin Dylight 488 antibody (1:500, SA-5488, Vector) was used for detection. Tissues were then washed with PBST three times over 1hr with shaking and nonspecific binding was blocked with Superblock neat (Pierce, Rockford, IL) at room temperature for 1–2 h. Specific taste type cell markers were used to label type I cells (rabbit anti-NTPDase2, 1:500, Centre de Recherche du CHUL, Quebec, CA), type II cells (guinea pig anti-TrpM5, 1:500, gift from Dr. Emily Liman; goat anti-T1R3, 1:250, sc-25458, Santa Cruz Biotechnology, Dallax, TX) and type III cells (rabbit anti-5HT, 1:500, #20080, Immunostar, Hudson, WI). For serotonin detection, mice were injected with 5-hydroxy-L-tryptophan (H9772, Sigma) 1h before sacrificed. Primary antibodies for specific taste cell types were incubated overnight at 4°C in a humidified chamber. After three 20 min washes with PBST, tissues were incubated for 1 h at room temperature with one of the following fluorescent secondary antibodies (1:300-500) in PBS: Dylight 647donkey anti-rabbit (Jackson ImmunoResearch, West Grove, PA) for immunofluorescence of rabbit primaries, Alexa 647 donkey anti-goat (Invitrogen, Grand Island, NY) for immunofluorescence of goat primaries and Dylight 647 donkey anti-guinea pig (Jackson ImmunoResearch) for immunofluorescence of guinea pig primary. Tissues were washed with PBST three times over 1h with shaking, then rinsed with dH2O for 10 min. Nuclei were labeled with 4′,6-diamidino-2-phenylindole (DAPI, 1:1,000; Invitrogen) for 5 mins for cell counting purposes. Slides were mounted with Vectorshield (Vector). Supplemental Figure 1 shows the positive and negative controls for the primary and secondary antibodies for GLP-1. A positive control was done on mouse pancreas and expected labeling of the α-cells in the Islets of Langerhans observed. Negative controls were done with anti-GLP and the omission of the secondary antibody, the omission of primary antibody and streptavidin Dylight 488 anti-mouse secondary, and anti-GLP-1 with various secondary antibodies to show non-cross reactivity. No anti-GLP-1 labeling was observed for any of the negative control conditions.
Imaging
Double immunofluorescence images were captured with a Leica TCS SP2 Spectral Confocal Microscope (Leica Microsystems Inc., Mannheim, Germany) using UV, Ar, GeNe and HeNe lasers and appropriate excitation spectra. Leica Scanware software was used to acquire Z-series stacks captured at a 0.25–0.35μm step size. Images were scanned at a 512X512 pixel format with four lines plus one frame averaging. The brightness and contrast of the digital images were adjusted linearly for background standardization and arranged using Photoshop CS (Adobe Systems, Inc., San Jose, California). For negative controls, all images were taken with the same acquisition settings (i.e., laser power, gain, offset, and PMT settings) as positive labeling for each secondary antibody. No adjustments to brightness or contrast were made to positive and negative control images.
Cell counting
Three-four sections of foliate and circumvallate papillae from two WT mice and 6–10 sections of fungiform papillae from one WT mouse were used for cell counting. Sections spaced over 60μm were selected and only taste cells with identifiable DAPI-labeled nuclei were considered. A small Z-stack of a thickness between 3–4μm was imaged at a magnification of 20X with digital zoom in which individual taste cells can be clearly identified. Cells were counted manually in Photoshop which allow visualization of each RBG channel separately to confirm co-localization.
Tastant application
Mice were anesthetized by ip injection with Avertin (125 mg per kg of body weight). Unconscious mice were placed on a warm (37°C) plate to maintain body temperature, the mouth was opened and the tongue pulled out slightly with blunt-end forceps to get access to posterior portion. A small piece of Whatman filter paper (10mm × 4mm), soaked in water (Control) or water containing 100 mM glucose was placed on top of the posterior tongue. This concentration of glucose has been shown to be effective in stimulating behavioral and nerve responses in mice(9).
Surgery
For unilateral cervical vagotomy anesthetized mice were laid on their back and an approximately 1.5 cm long incision was made on the right side of the neck. Muscles were retracted to yield access to the carotid trunk. The vagus nerve was gently separated from the carotid artery and cut in cross-section. For esophagectomy/truncal vagotomy anesthetized mice were laparotomized, organs were retracted, and esophagus revealed. The esophagus was tightly ligated with a silk suture approximately 1 cm above the gastroesophageal junction, and cut circumferentially between the suture and the gastroesophageal junction such that the proximal portion was separated entirely from the gastric portion.
Blood collection
Tastants were applied on the posterior tongue as described and blood was collected from surgically intact mice and mice that had undergone unilateral cervical vagotomy from the orbital sinus with a heparin coated fine glass pipette. For mice that had undergone esophagectomy/truncal vagotomy blood was collected from the hepatic portal vein. Blood samples were centrifuged, DPP4 inhibitor added and stored on −80°C for GLP-1 measurement.
Taste papilla explants
Explants of circumvallate (CV) papilla taste tissue were prepared as described(11). CV explants were incubated for 2 hours in IMDM buffer (control samples) or in IMDM buffer containing 100 mM glucose. Medium was collected and stored at −80°C for GLP-1 measurements. Each CV papilla consists of two bean shaped parts of equal sizes. To ensure similar number of taste buds and taste cells in all preparations, CV papillae were bisected with a razor blade, one half was used as a control, and the other part was incubated with glucose/tastant-containing medium.
GLP-1 Immunoassay
GLP-1 in blood or medium was measured using a GLP-1 ELISA assay sensitive for the active form of mouse/rat GLP-1 (Linco). Determinations were done in duplicate for the numbers of mice indicated.
Statistical analysis
Significance was examined by either the unpaired t-test or by multiple-comparisons analysis of variance (ANOVA) and post-test, as appropriate. All data are presented as mean±SE; P < 0.05 was considered statistically significant. Graphics as well as statistical analyses were performed using GraphPad Prism (GraphPad Software, San Diego, CA).
Results
Taste cells express and secrete GLP-1
Given the presence of taste signaling proteins in enteroendocrine cells(1) and the presence of multiple gut hormones in taste cells (12,13) we sought to determine if taste cells might directly release hormones into the bloodstream as part of the cephalic phase of hormone release. We focused on taste cell secretion of GLP-1, previously shown to be expressed in certain type II taste cells(5).
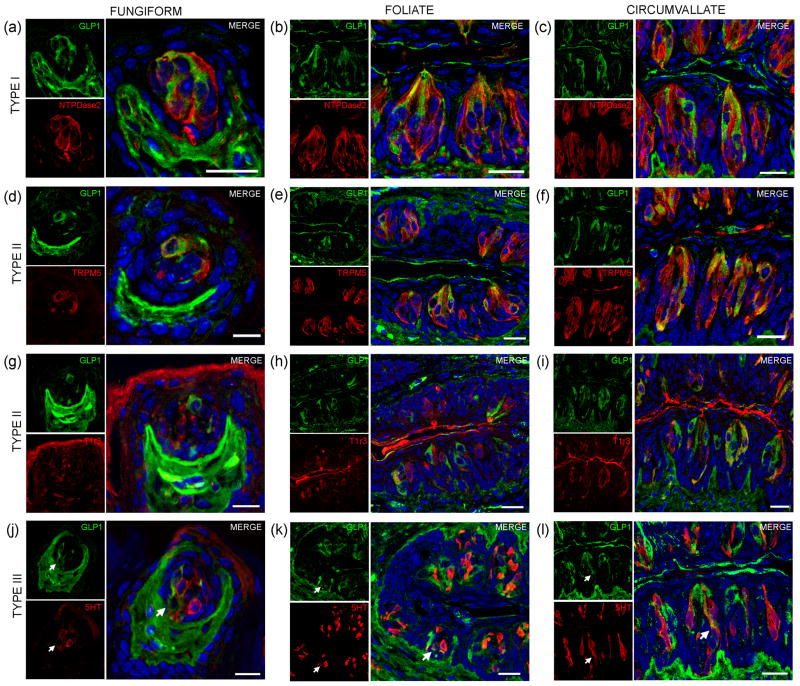
To determine which types of taste cells express GLP-1, we performed double-immunohistochemistry with markers specific for taste cells of types I, II and III. Double immunohistochemistry with fungiform, foliate and CV papilla sections showed that GLP-1 was most often co-expressed in type II taste cells as assessed by coexpression with TrpM5 (Fig. 1D–F). In posterior taste fields ~91–93% of the GLP-1-expressing cells also expressed TrpM5, although they constituted only about 20–27% of the total type II taste cells (Table 1). In fungiform papillae only ~23% of the GLP-1 cells also expressed TrpM5. Double immunostaining for GLP-1 and the T1R3-expressing subset of type II taste cells (Fig. 1G–I) showed that only ~13–35% of the GLP-1-expressing cells also expressed T1R3 (Table 1), indicating that among type II taste cells it is more often the cells that do not express T1R3 that express GLP-1. Double-immunohistochemistry with triphosphate diphosphohydrolase-2 (NTPDase2) showed that GLP-1 is generally not expressed in type I taste cells (Fig. 1A–C). Double immunochemistry with serotonin (5HT) and GLP-1 indicated that ~6–17% of GLP-1 cells expressed serotonin (Fig. 1J–L, Table 1). Our results contrast to those of Shin et al.(5) who found in CV taste cells that ~52% of GLP-1 cells expressed T1R3, and ~44% of GLP-1 cells expressed serotonin.
Fig. 1. Expression of GLP-1 in taste cell types in anterior and posterior taste fields.
Mouse fungiform, foliate and circumvallate papillae sections were double stained with antibodies against GLP-1 and markers for taste cell subtypes. (A–C) Double staining for GLP-1 (green) and the type I cell marker NTPDase2 (red) found no doubly positive taste cells. (D–F) Double staining of GLP-1 (green) and the type II cell marker TrpM5 (red) identified frequent doubly positive taste cells. (G–I) Double staining of GLP-1 (green) and the type II cell sweet/umami receptor subunit T1R3 (red) identified few doubly positive taste cells. (J–L) Double staining of GLP-1 (green) and the type III cell marker serotonin (5HT) (red) identified occasional doubly positive taste cells. Arrows indicate doubly stained GLP-1+/5HT+ type III taste cells. DAPI (blue) was used to label cell nuclei. Scale bars = 20μm.
Table 1.
Co-Expression of GLP-1 with Trpm5, T1R3 and Serotonin in Mouse Taste Cells.
| A. Numbers of taste cells expressing GLP-1 and TrpM5. | ||||
|---|---|---|---|---|
| Tissue | GLP-1 | TrpM5 | GLP-1+TrpM5/GLP1 | GLP-1+TrpM5/TrpM5 |
| Fungiform [9] | 17 | 24 | 4/17 (23.5%) | 4/24 (16.7%) |
| Foliate [83] | 63 | 293 | 57/63 (90.5%) | 57/293 (19.5%) |
| CV [119] | 122 | 427 | 115/123 (93.5%) | 115/427 (26.9%) |
| B. Numbers of taste cells expressing GLP-1 and T1R3. | ||||
|---|---|---|---|---|
| Tissue | GLP-1 | T1R3 | GLP-1+T1R3/GLP1 | GLP-1+T1R3/T1R3 |
| Fungiform [6] | 15 | 14 | 2/15 (13.3%) | 2/14 (14.3%) |
| Foliate [62] | 54 | 100 | 14/54 (25.9%) | 14/100 (14%) |
| CV [135] | 178 | 241 | 62/178 (34.8%) | 62/241 (25.7%) |
| C. Numbers of taste cells expressing GLP-1 and Serotonin (5HT). | ||||
|---|---|---|---|---|
| Tissue | GLP-1 | 5HT | GLP-1+5HT/GLP1 | GLP-1+5HT/5HT |
| Fungiform [8] | 12 | 24 | 2/12 (16.6%) | 2/24 (8.3%) |
| Foliate [60] | 59 | 111 | 4/59 (6.8%) | 4/111 (3.6%) |
| CV [84] | 71 | 200 | 4/71 (5.6%) | 4/200 (2.0%) |
Taste cells from fungiform, foliate and circumvallate (CV) papillae were doubly stained for GLP-1 and either TrpM5, T1R3 or 5HT. Then doubly labeled taste cells were counted in the fungiform (A), foliate (B), and circumvallate (C) papillae. The number of taste buds counted is shown in brackets. The percentage of co-expression is shown in parentheses.
We measured glucose-elicited release of GLP-1 from CV papillae explants in culture medium from wild type (WT) mice or knockout mice lacking T1R3 (T1R3KO). Glucose elicited GLP-1 release from CV explants from both WT and T1R3 KO mice (Fig. 2A). To determine if taste cells might act as endocrine cells to release hormones into the circulation we measured effects of oral stimulation of glucose on GLP-1 secretion in WT and T1R3KO mice. We measured blood GLP-1 before stimulation and at 10 and 20 minutes after oral stimulation with glucose. In WT mice, oral stimulation with glucose induced significant GLP-1 release after glucose application on the tongue (20% and 40% above baseline, at 10 and 20 minutes, respectively), compared to control, non-stimulated animals (Fig. 2B). In addition, at 20 minutes glucose induced GLP-1 release from T1R3KO mice (Fig. 2B), indicating that the T1R2+T1R3 sweet taste receptor is not required for glucose-stimulated GLP-1 release from taste cells.
Fig. 2. Release of GLP-1 from taste cells.
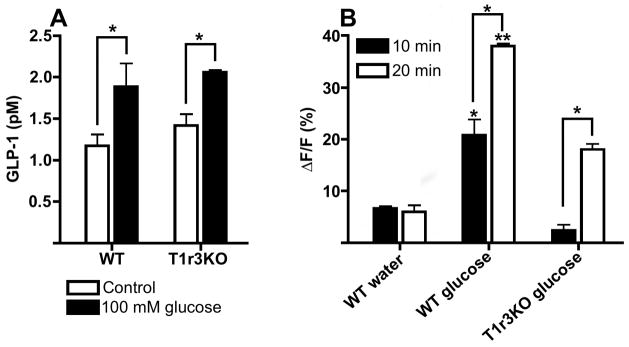
(A) Glucose-elicited release of GLP-1 in vitro from circumvallate papillae explants of wild type (WT) and T1R3 knockout (T1R3KO) mice. Explants were incubated for 2 hours in IMDM buffer (Control, open bars) or IMDM buffer containing 100 mM glucose (closed bars). n=4 explants for each experiment, * p<0.05. (B) Secretion of GLP-1 in intact mice after oral stimulation with sweeteners. Wild type (WT) and T1R3KO mice were stimulated by oral application of water or 100 mM glucose. Blood was collected at 10 and 20 minutes (closed and open bars respectively) after oral stimulation. ΔF/F indicates the percentage change of blood GLP-1 vs. basal level (0 min, not shown). n=4 mice for each experiment, * p<0.05, ** p<0.01.
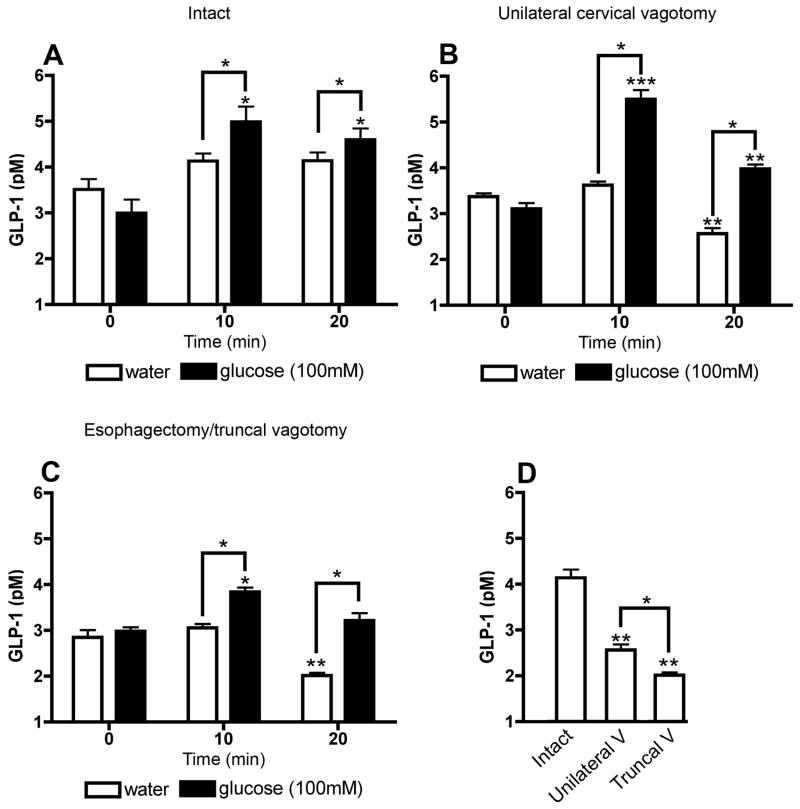
Unilateral cervical vagotomy reduces vagally mediated effects but does not eliminate cephalic phase hormone release through activation of vagal-efferent fibers in response to food-related sensory stimuli. In intact WT mice and ones that had been cervically vagotomized unilaterally, oral stimulation by glucose elicited an increase in circulating GLP-1 levels (Fig. 3A, B). However, in the unilaterally vagotomized mice this effect could be mediated by the remaining intact vagus nerve acting to stimulate GLP-1 release from gastrointestinal endocrine cells. To completely exclude vagal effects on GLP-1 release after oral stimulation we monitored circulating GLP-1 levels in mice after a combined truncal vagotomy and esophagectomy. This procedure dissects both branches of the vagus nerve below the esophageal hiatus and thus eliminates efferent effects from the gastric and pancreatic branches of the vagus, as well as from vagal branches innervating the small and large intestines. We found that oral stimulation by glucose in mice that had received truncal resection of the vagus still elicited GLP-1 release (Fig. 3C). Both unilateral cervical vagotomy and truncal vagotomy reduced baseline blood GLP-1 levels at 20 minutes after nerve resection with a more pronounced effect from the truncal vagotomy (Fig. 3D). However, oral stimulation by glucose in mice that had received truncal vagotomy still elicited a significant rise in blood GLP-1 levels at 10 and 20 minutes (Fig. 3C). Comparing the GLP-1 response in intact vs. vagotomized mice by two-tailed t test indicated that differences were significant at both 10 min (P=0.034) and at 20 min (P=0.032). This rise of GLP-1 is independent of vagal efferent actions and thus may be the result of direct release of GLP-1 from endocrine taste cells into the bloodstream. Consistent with this inference is our observation that CV tissue explants can release GLP-1 into the culture medium upon stimulation with glucose (Fig. 2A).
Fig. 3. Secretion of GLP-1 from taste cells in vagotomized mice.
(A) Intact wild type mice were stimulated by oral application of water (open bars) or 100 mM glucose (closed bars), then blood was collected before (0 min) and at 10 or 20 minutes after oral stimulation and assayed for blood GLP-1 levels. (B, C) Same procedures as in A except that mice underwent unilateral cervical vagotomy (B) or esophagectomy/truncal vagotomy (C) prior to the oral stimulation. (D) Baseline blood GLP-1 levels 20 minutes after surgical procedures (Intact mice, Unilateral vagotomy, Truncal vagotomy). n=5 for each experiment, * p<0.05, ** p<0.01, *** p<0.005.
Discussion
A number of “gut” hormones have been found to be expressed in taste cells(2–5). Notably, the incretin GLP-1 that is co-expressed with taste receptors and gustducin in enteroendocrine cells in the gut(1), is expressed also in taste cells(5). In the present study we observed most of the GLP-1-expressing taste cells in posterior taste fields to be TrpM5-expressing type II receptor cells. Only a small number of GLP-1-expressing cells were found among type III cells marked by expression of serotonin. Among type II taste cells GLP-1 was most often found in the TrpM5-positive/T1R3-negative cells: these are likely to be α-gustducin-positive cells. Among the GLP-1-expressing taste cells in CV papillae Shin et al.(5) found between 44%–56% also expressed either serotonin, T1R3 or α-gustducin. We cannot at present explain the differences in co-expressing cells in our study vs. Shin et al; we did not examine co-expression of α-gustducin with GLP-1.
Mice that lack the sweet receptor subunit T1R3 have little or no chorda tympani nerve response to non-caloric sweeteners, but still respond normally to sugars(9). That taste cells also express sugar sensors and transporters typically found in intestine and pancreas (e.g. SGLT1, GLUTs and KATP) may explain how T1R3 knockout mice can still respond to sugars(10). Here we found that glucose releases GLP-1 from taste cells. Moreover, mice lacking T1R3 secreted GLP-1 in response to orally applied glucose indicating that GLP-1 release from taste cells may be mediated independently of T1R2+T1R3 sweet receptors, e.g. by sugar transporters and KATP shown to be present in T1R3-positive taste cells(10).
Food digestion is often divided into multiple phases, e.g. neural/cephalic, gastric, and intestinal phases. The neural/cephalic phase of digestion is a set of physiological, endocrine and autonomic responses of the digestive system that result from stimulation of sensory systems at the cephalic level(14). Cephalic phase responses are well established for insulin and ghrelin(7,8), but controversial or thought not to occur with the incretin hormones GLP-1 and GIP (glucose-dependent insulinotropic peptide)(15).
In rats the involvement of taste receptor cells in the cephalic phase of digestion is well documented. The cephalic phase for insulin release (CPIR) in rats appears as early as 1–1.5 minutes after stimulation with saccharin or glucose(16). In humans the presence of a CPIR and its physiological importance is somewhat controversial. “Tease feeding” (exposure to sights and smells of a meal), or ingestion of the non-caloric sweetener aspartame individually fail to stimulate an early cephalic response for insulin. However, the combination of a tease meal plus aspartame elicits a drop in blood glucose and a rise in serum insulin and C-peptide within 5 minutes(17). Other investigators have found that sweet taste stimuli provided as nutritive and non-nutritive sweetened tablets significantly decrease plasma glucose and insulin, and only sucrose causes plasma glucose and insulin to rise(18). One set of experiments with nutritive and non-nutritive stimuli (aspartame, saccharin, sucrose) showed that sweeteners in solutions do not provide adequate stimuli to elicit CPIR(19). However, others found that sucrose and saccharin applied on the tongue, elicited a significant increase in plasma insulin concentrations within 10 minutes, even when applied to the oral cavity only(20). Studies using Functional Magnetic Resonance Imaging to monitor hypothalamic responses show that sweet taste (aspartame) or energy content (maltodextrin) individually do not elicit CPIR, but together sweet taste and energy content (glucose) trigger CPIR(21).
We have found in WT and T1R3KO mice that local stimulation of taste cells of the tongue by glucose produces a significant increase in blood GLP-1 levels. Our results show that even after truncal vagotomy, which included esophagotomy that would prevent any solution to enter the stomach, blood GLP-1 levels increased after tongue stimulation with glucose. Thus, in mouse there is the possibility that any early cephalic phase of GLP-1 release originates in from GLP-1-expressing taste cells of the tongue. This is an altogether novel basis for cephalic phase hormone release for a hormone that was thought not to be released during the cephalic phase(15). Because food and digestion products do not reach the intestines for several minutes after feeding, any early cephalic GLP-1 responses could be mediated by release from endocrine taste cells and/or by efferent actions of the vagus nerve to stimulate intestinal enteroendocrine L cells to release GLP-1. It remains to be determined if such mechanisms hold true in humans.
Acknowledgments
This work was supported by NIH grants DC03055, DC03155, DK081421 to RFM. Imaging was performed at the Monell Histology and Cellular Localization Core, which is supported in part by funding from NIH-NIDCD core grant 1P30DC011735-01.
Footnotes
The authors declare that they have no conflicts of interest
ZK, KKY, BM and RFM designed experiments; ZK, KKY, EI, KI, YL collected and analyzed data; all authors contributed to writing the manuscript.
References
- 1.Jang HJ, Kokrashvili Z, Theodorakis MJ, et al. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci U S A. 2007;104:15069–15074. doi: 10.1073/pnas.0706890104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shen T, Kaya N, Zhao FL, et al. Co-expression patterns of the neuropeptides vasoactive intestinal peptide and cholecystokinin with the transduction molecules alpha-gustducin and T1R2 in rat taste receptor cells. Neuroscience. 2005;130:229–238. doi: 10.1016/j.neuroscience.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Herness S, Zhao FL. The neuropeptides CCK and NPY and the changing view of cell-to-cell communication in the taste bud. Physiol Behav. 2009;97:581–591. doi: 10.1016/j.physbeh.2009.02.043. [DOI] [PubMed] [Google Scholar]
- 4.Huang YA, Dando R, Roper SD. Autocrine and paracrine roles for ATP and serotonin in mouse taste buds. J Neurosci. 2009;29:13909–13918. doi: 10.1523/JNEUROSCI.2351-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shin YK, Martin B, Golden E, et al. Modulation of taste sensitivity by GLP-1 signaling. J Neurochem. 2008;106:455–463. doi: 10.1111/j.1471-4159.2008.05397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elson AE, Dotson CD, Egan JM, et al. Glucagon signaling modulates sweet taste responsiveness. FASEB J. 2010;24:3960–3969. doi: 10.1096/fj.10-158105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Power ML, Schulkin J. Anticipatory physiological regulation in feeding biology: cephalic phase responses. Appetite. 2008;50:194–206. doi: 10.1016/j.appet.2007.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drazen DL, Vahl TP, D’Alessio DA, et al. Effects of a fixed meal pattern on ghrelin secretion: evidence for a learned response independent of nutrient status. Endocrinology. 2006;147:23–30. doi: 10.1210/en.2005-0973. [DOI] [PubMed] [Google Scholar]
- 9.Damak S, Rong M, Yasumatsu K, et al. Detection of sweet and umami taste in the absence of taste receptor T1r3. Science. 2003;301:850–853. doi: 10.1126/science.1087155. [DOI] [PubMed] [Google Scholar]
- 10.Yee KK, Sukumaran SK, Kotha R, et al. Glucose transporters and ATP-gated K+ (KATP) metabolic sensors are present in type 1 taste receptor 3 (T1r3)-expressing taste cells. Proc Natl Acad Sci U S A. 2011;108:5431–5436. doi: 10.1073/pnas.1100495108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozdener H, Yee KK, Cao J, et al. Characterization and long-term maintenance of rat taste cells in culture. Chem Senses. 2006;31:279–290. doi: 10.1093/chemse/bjj030. [DOI] [PubMed] [Google Scholar]
- 12.Shin YK, Martin B, Kim W, et al. Ghrelin is produced in taste cells and ghrelin receptor null mice show reduced taste responsivity to salty (NaCl) and sour (citric acid) tastants. PLoS One. 2010;5:e12729. doi: 10.1371/journal.pone.0012729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Acosta A, Hurtado MD, Gorbatyuk O, et al. Salivary PYY: a putative bypass to satiety. PLoS One. 2011;6:e26137. doi: 10.1371/journal.pone.0026137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zafra MA, Molina F, Puerto A. The neural/cephalic phase reflexes in the physiology of nutrition. Neurosci Biobehav Rev. 2006;30:1032–1044. doi: 10.1016/j.neubiorev.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Ahrén B, Holst JJ. The cephalic insulin response to meal ingestion in humans is dependent on both cholinergic and noncholinergic mechanisms and is important for postprandial glycemia. Diabetes. 2001;50:1030–8. doi: 10.2337/diabetes.50.5.1030. [DOI] [PubMed] [Google Scholar]
- 16.Ionescu E, Rohner-Jeanrenaud F, Proietto J, et al. Taste-induced changes in plasma insulin and glucose turnover in lean and genetically obese rats. Diabetes. 1988;37:773–779. doi: 10.2337/diab.37.6.773. [DOI] [PubMed] [Google Scholar]
- 17.Bruce DG, Storlien LH, Furler SM, et al. Cephalic phase metabolic responses in normal weight adults. Metabolism. 1987;36:721–725. doi: 10.1016/0026-0495(87)90106-5. [DOI] [PubMed] [Google Scholar]
- 18.Abdallah L, Chabert M, Louis-Sylvestre J. Cephalic phase responses to sweet taste. Am J Clin Nutr. 1997;65:737–743. doi: 10.1093/ajcn/65.3.737. [DOI] [PubMed] [Google Scholar]
- 19.Teff KL, Devine J, Engelman K. Sweet taste: effect on cephalic phase insulin release in men. Physiol Behav. 1995;57:1089–1095. doi: 10.1016/0031-9384(94)00373-d. [DOI] [PubMed] [Google Scholar]
- 20.Just T, Pau HW, Engel U, et al. Cephalic phase insulin release in healthy humans after taste stimulation? Appetite. 2008;51:622–627. doi: 10.1016/j.appet.2008.04.271. [DOI] [PubMed] [Google Scholar]
- 21.Smeets PA, de Graaf C, Stafleu A, et al. Functional magnetic resonance imaging of human hypothalamic responses to sweet taste and calories. Am J Clin Nutr. 2005;82:1011–1016. doi: 10.1093/ajcn/82.5.1011. [DOI] [PubMed] [Google Scholar]