Given its importance as an integral part of the human body, the loss of a hand – regardless of cause – can be a highly traumatic experience requiring extended periods of psychological and physical rehabilitation. Attempts to reintegrate hand amputees back into society using state-of-the-art, contemporary technology can be documented to as far back as antiquity and the middle ages. Despite astounding progress in the field, a highly functional, cosmetically appealing replacement has eluded clinicians and researchers. However, more recent advances in robotic technology, hand restoration and even hand transplantation have shown promising results.
Keywords: Hand amputation, Hand amputee, Hand prosthesis, Hand transplantation, Myoeletric prosthesis, Targeted reinnervation
Abstract
The hand is an integral component of the human body, with an incredible spectrum of functionality. In addition to possessing gross and fine motor capabilities essential for physical survival, the hand is fundamental to social conventions, enabling greeting, grooming, artistic expression and syntactical communication. The loss of one or both hands is, thus, a devastating experience, requiring significant psychological support and physical rehabilitation. The majority of hand amputations occur in working-age males, most commonly as a result of work-related trauma or as casualties sustained during combat. For millennia, humans have used state-of-the-art technology to design clever devices to facilitate the reintegration of hand amputees into society. The present article provides a historical overview of the progress in replacing a missing hand, from early iron hands intended primarily for use in battle, to today’s standard body-powered and myoelectric prostheses, to revolutionary advancements in the restoration of sensorimotor control with targeted reinnervation and hand transplantation.
Abstract
La main, dont le spectre fonctionnel est incroyable, fait partie intégrante du corps humain. En plus de la motricité globale et de la motricité fine essentielles à la survie physique, la main est fondamentale dans le cadre des conventions sociales, permettant de souhaiter la bienvenue, de se nettoyer, de démontrer son expression artistique et sa communication syntaxique. La perte d’une main ou des deux mains est donc une expérience dévastatrice, qui exige un soutien psychologique et une réadaptation physique considérables. La majorité des amputations de la main se produisent chez des hommes en âge de travailler, surtout après un traumatisme lié au travail ou d’incidents au combat. Depuis des millénaires, les humains recourent avec ingéniosité à la technologie de pointe pour concevoir des dispositifs afin d’aider les amputés de la main à réintégrer la société. Le présent article propose un aperçu historique de l’évolution du remplacement d’une main manquante, en commençant par les premières mains de fer conçues principalement pour les combats, en passant par les prothèses standards myoélectriques ou activées par le corps actuelles, jusqu’aux progrès révolutionnaires dans la restauration du contrôle sensorimoteur avec réinnervation ciblée et transplantation de la main.
From grasping and manipulating objects to grooming and communication, the versatility of the human hand is integral to both physical survival and social conventions. The loss of one or more hands is, thus, a devastating experience, requiring significant psychological support and physical rehabilitation. The majority of upper extremity amputations occur in working-age males, most commonly from occupational or combat trauma. Congenital deficiencies, cancers and vascular disease are also major causes of amputations (1). For millennia, humans have used state-of-the-art technology to help hand amputees reintegrate into society. Despite outstanding progress in this field, however, creating an ideal functional and cosmetic replacement for a missing hand continues to challenge clinicians and researchers. The present article provides a historical overview of approaches to replacing a missing hand, from early iron hands, to today’s standard prostheses, to revolutionary advancements in sensorimotor restoration.
FROM ANTIQUITY TO THE MIDDLE AGES: IRON HANDS
One of the earliest records of a prosthetic hand was described in 77 AD by Roman scholar Pliny the Elder in his encyclopedia Naturalis Historia. After losing a hand in the Second Punic War (218–201 BC), Marcus Sergius, a Roman general, received a prosthesis that enabled him to return successfully to battle.
Sergius in his second campaign lost his right hand… He had a right hand of iron made for him and going into action with it tied to his arm, raised the siege of Cremona…
(2).
Among the most famous examples of an early hand prosthesis was the iron hand of German knight Götz von Berlichingen (3). After Götz lost his hand during the Siege of Landshut (circa 1505) in Bavaria, an artisan fashioned him an iron hand with digits that could be flexed and extended passively at the metacarpophalangeal, proximal interphalangeal and distal interphalangeal joints, as well as the thumb interphalangeal joint (Figures 1 and 2). On strapping on the prosthesis, Götz was able to hold reins, grip weapons and return to battle. The device was modelled as an extension of battle armour rather than a human arm and, due to its weight, needed to be attached to Götz’s armour with thick leather straps.
Figure 1).
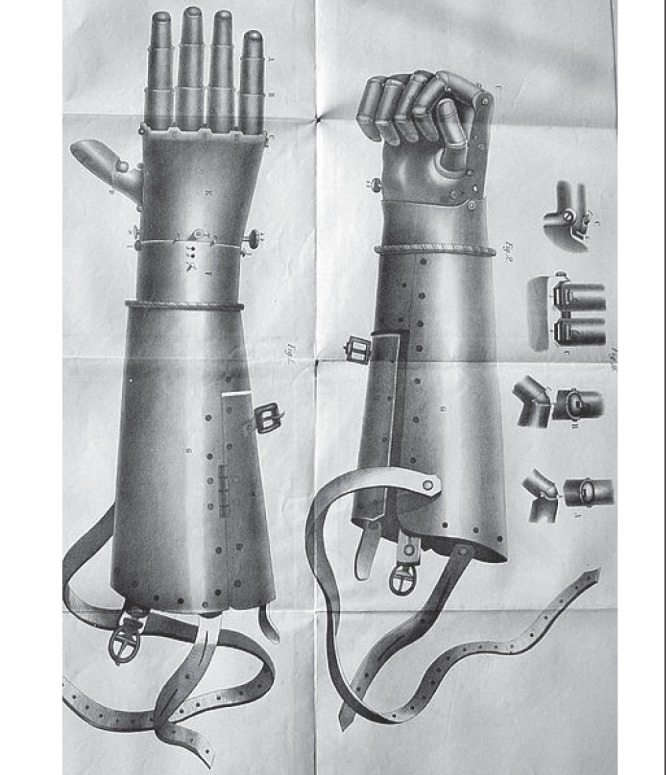
The iron hand of Götz von Berlichingen featured articulations at the metacarpophalangeal, proximal interphalangeal and distal interphalangeal joints, as well as the thumb interphalangeal joint. The prosthesis was attached to Götz’s armour with leather straps. Image retrieved from Wikimedia Commons <www.commons.wikimedia.org>
Figure 2).

Illustration of the numerous components of Götz’s medieval hand prosthesis. Image retrieved from Wikimedia Commons <www.commons.wikimedia.org>
Italian historian and physician Paolo Giovio recorded that the Turkish pirate Horuk Barbarossa lost his right hand in the Battle of Bugia (circa 1517) against Spain, and received an iron replacement that enabled him to continue in battle. Another example of an iron hand was that created by a Dutch craftsman for Duke Christian of Brunswick, who had lost his left hand in the Battle of Fleury (circa 1622). One of the first descriptions of a noncombative hand prosthesis was in 1600 by Italian surgeon Giovanni Tommaso Minadoi, who described an amputee who could remove his hat, untie a purse and even write with a quill (3). In the 16th century, French military surgeon Ambroise Paré drew the first detailed design of a spring-loaded prosthetic hand, nicknamed ‘Le Petit Lorrain’ after the craftsman who fashioned it (Figure 3). Paré also drew a prosthetic arm for an above-elbow amputation (Figure 4) (4).
Figure 3).
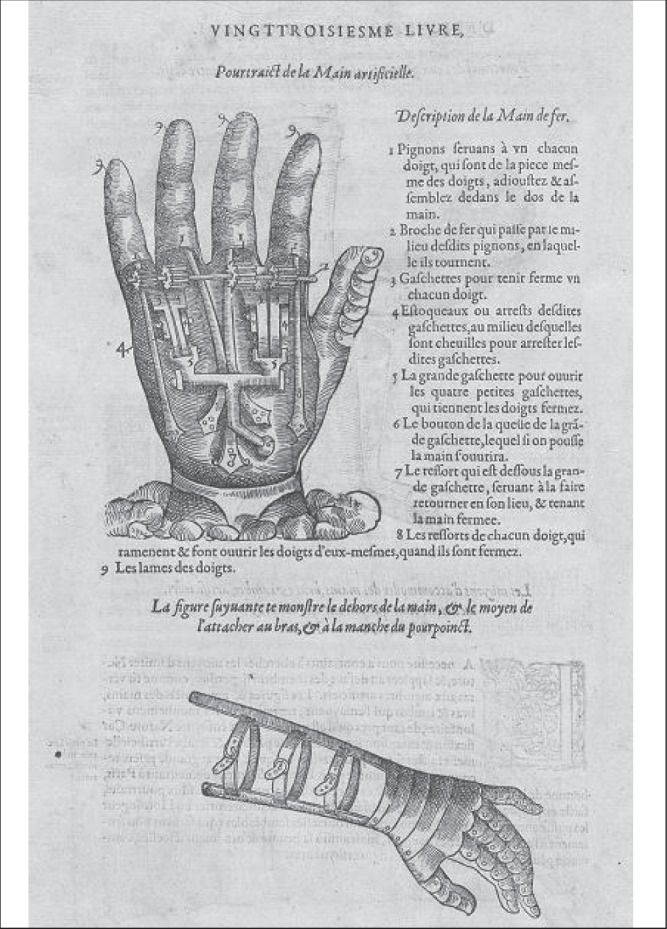
Ambroise Paré’s illustration of the ‘Le Petit Lorrain’ prosthetic hand published in 1575 in his book Les oeuvres d’Ambroise Paré (The Works of Ambroise Paré). Although the wrist is immobile, the fingers are held in extension by four springs fixed in the palm. The fingers may be brought into flexion and are kept in position by sprockets controlled by metal levers, thereby allowing a reliable grip on objects. The hand is connected to the forearm stump with two metal bars and leather straps. Image retrieved from US National Library of Medicine <www.nlm.nih.gov/exhibition/historicalanatomies/home.html>
Figure 4).

Description of Paré’s iron arm design for an above-elbow amputee. A lever-sprocket mechanism controls elbow flexion and extension. Image retrieved from US National Library of Medicine <www.nlm.nih.gov/exhibition/historicalanatomies/home.html>
Despite being heavy and requiring control by the contralateral intact hand of an amputee, early prosthetic hands successfully restored a knight’s ability to hold a shield or weapon in battle. These prostheses were carefully crafted with the shape and appearance of human hands, rather than simply inanimate tools to hold objects. Nevertheless, accounts of early hand prostheses are rare because severe trauma inevitably resulted in hemorrhage and infection, and only the wealthy could afford such customized devices.
BODY-POWERED PROSTHESES, TWO WORLD WARS AND THE CREATION OF DEDICATED PROSTHETICS ORGANIZATIONS
The concept of an ‘automatic’ body-powered upper limb prosthesis was pioneered by German dentist Peter Baliff in 1818 (5). Using transmission of tension through leather straps, Baliff’s device enabled the intact muscles of the trunk and shoulder girdle to elicit motion in a terminal device attached to the amputation stump. For the first time, an amputee was able to operate his prosthesis with fluid body motions, rather than as a distinct foreign object. In the 1860s, the Comte de Beaufort in France adapted the design for use by wounded soldiers. A shoulder harness with a strap buttoned to the trousers was passed through a loop to the contralateral axilla and missing limb, allowing an amputee to manipulate the strap tension to open and close a double spring hook, or flex and extend the thumb on a simple hand with fused fingers (5,6).
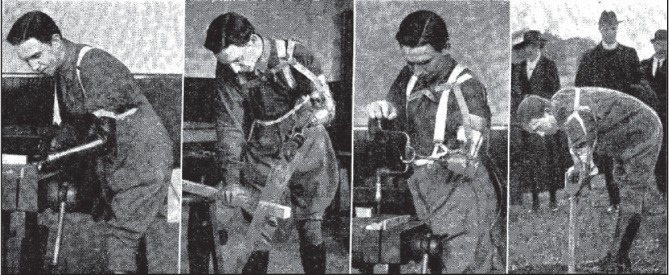
In 1916, German surgeon Dr Ferdinand Sauerbruch described his prosthetic design with digits controlled by transmission of upper arm muscle movements (Figure 5) (7). Video captures from the era show amputees effectively using the prosthesis to drink from a teacup and even to remove a match from a box to light a cigarette (8). Unfortunately, due to the high cost of production, few individuals were able to afford the device.
Figure 5).

Sauerbruch’s prosthetic hand design in the early 20th century gave many amputees a high degree of functional independence. Video captures of patients using the prosthesis to perform various activities may be viewed at http://vlp.mpiwg-berlin.mpg.de/library/data/lit38416. Image credit: Hermann von Helmholtz Center for Cultural Technology, Humboldt University of Berlin <http://www.sammlungen.hu-berlin.de/objekt-desmonats/2005/11/>
World War I (1914 to 1918) resulted in casualties in numbers previously unimagined. In the United States (US), amputee rehabilitation programs were created to help the >4400 amputees, of which the majority (54%) were upper limb (9), to regain some ability to work on farms or in factories. The distribution of prosthetics with sockets and a universal terminal device allowed the attachment of various work tools (Figure 6) (5). In 1917, the Surgeon General of the US Army issued a landmark invitation for limb makers to meet in Washington, DC. The result was the creation of the Association of Limb Manufacturers of America, today the American Orthotic & Prosthetic Association. In Canada, a national charter in 1920 recognized the need to provide support to amputees, leading to the creation of the Amputations Association of The Great War, today known as the War Amps (10).
Figure 6).
The interchangeability of terminal devices allowed various jobs to be performed using a body-powered prosthesis. Image reprinted with permission from Elsevier: Marshall CJ. Modern artificial limbs: The work of the arm-training centre at Roehampton. Lancet. 25 June 1921
During World War II (1939 to 1945), improved shock management and antibiotics saved lives but resulted in 3475 upper limb amputees in the US (9). The huge demand for artificial limbs led to the creation of a US Committee on Prosthetics Research and Development in 1945 and the Canadian Association of Prosthetics and Orthotics in 1955 (11,12). The thalidomide tragedy (1958 to 1962) resulted in the birth of many children with shortened limbs, further driving demand and investment for improved prosthetics (13).
In 1948, the Bowden cable body-powered prosthesis was introduced, replacing bulky straps with a sleek, sturdy cable. Despite new materials and improved craftsmanship, today’s body-powered prostheses are essentially adaptations of the Bowden design (Figure 7). Durable, portable and relatively affordable, body-powered prostheses allow the user an impressive range of motion, speed and force in operating a terminal device – most commonly a two-pronged hook – by changing the tension in a cable via preserved shoulder and body movements. The ability to use both hands simultaneously, rather than requiring a healthy hand to control the prosthesis, permits the user to complete tasks more efficiently. Furthermore, by sensing cable tension, the amputee is able to predict and adjust the position of the prosthesis without visual feedback. Although prolonged wearing can be uncomfortable, complicated motor tasks are limited and appearance is not human-like, body-powered prostheses are widely used (14).
Figure 7).
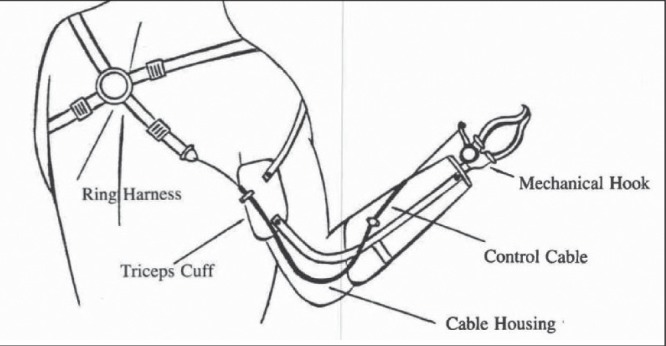
Bowden cable body powered prosthesis. Image reprinted with permission from Journal of Prosthetics & Orthotics Online Library: Billock JN. Upper limb prosthetic terminal devices: hands versus hooks. Clin Prosthet Orthot 1986;10:57–65
ROBOTIC TECHNOLOGY MYOELECTRIC PROSTHESES
In 1919, a German book titled Ersatzglieder und Arbeitshilfen (Limb Substitutes and Work Aids) contained conceptual designs for the first externally powered prostheses, using pneumatic and electric power sources (Figures 8 and 9). Unfortunately, these revolutionary designs were too complex to be feasible with contemporary technology (11).
Figure 8).
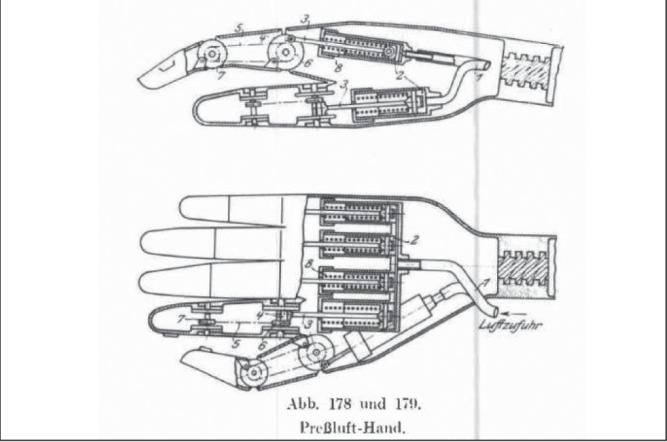
Early compressed gas-powered prosthetic hand from 1919 German book Ersatzglieder under Arbeitshilfen (Limb Substitutes and Work Aids). Image reprinted with permission from Journal of Prosthetics & Orthotics Online Library: Childress DS. Historical aspects of powered limb prostheses. Clin Prosthet Orthot 1985:9:2–13
Figure 9).
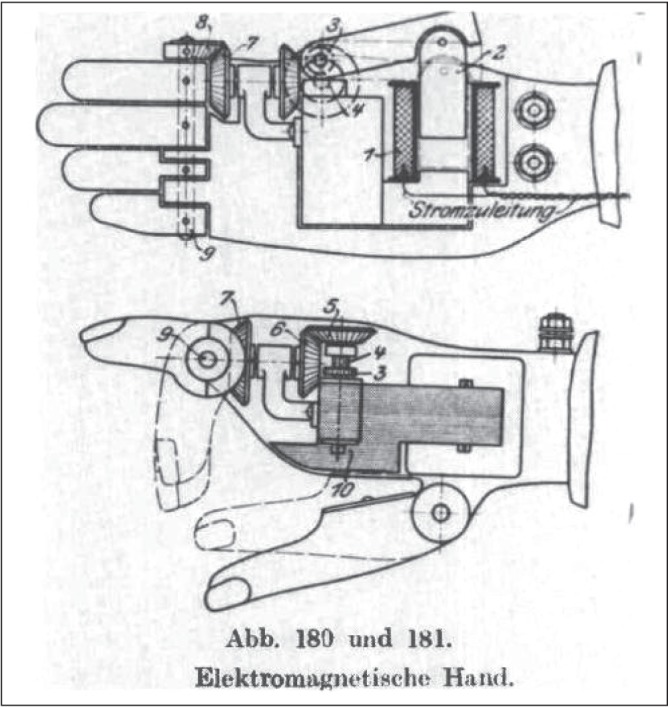
Electromagnetic hand prosthesis from 1919 German book Ersatzglieder under Arbeitshilfen (Limb Substitutes and Work Aids). Image reprinted with permission from J Prosthet Orthot Online Library: Childress DS. Historical aspects of powered limb prostheses. Clin Prosthet Orthot 1985:9:2–13
In 1948, Reinhold Reiter, a physics student at Munich University (Munich, Germany), created the first myoelectric prosthesis, a device that amplifies surface electromyography (EMG) potentials to power motorized parts. Although Reiter published his work (15), it was not widely appreciated, and this potentially ground-breaking invention did not gain commercial or clinical acceptance (16).
The first clinically significant myoelectric prosthesis was unveiled by Russian scientist Alexander Kobrinski in 1960. The use of transistors reduced bulk and allowed portability of the device, with the batteries and electronics worn on a belt and connected to the prosthesis by wires. The prosthesis also featured a skin-coloured rubber cosmetic glove (17). Although sold in Britain and Canada, this ‘Russian Hand’ had numerous problems: it was heavy, movement was slow, pinch force was weak, wire connections were susceptible to damage and electrical interference compromised reliability (16).
By the 1980s, myoelectric prostheses were being used in rehabilitation centres around the world and, today, they are a common option for amputees (Figure 10) (18). Improvement in materials has permitted lighter and more ergonomic designs, while power has evolved from compressed gas to rechargeable nickel-cadmium batteries (19). Compared with body-powered prostheses, myoelectric prostheses feature superior comfort and aesthetics, with no unsightly cables and a diverse selection of life-like silicone hand and skin overlays (Figure 11). In addition, signal detection is noninvasive on the skin surface, and operation effort is comparable with a normal limb (20). The control muscles vary according to the patient’s amputation level. For example, most below-elbow (transradial) amputees will use the preserved wrist flexor and extensor muscles to control the prosthetic hand, while above-elbow (transhumeral) amputees will also involve the biceps and triceps muscles to control the prosthetic elbow (21).
Figure 10).
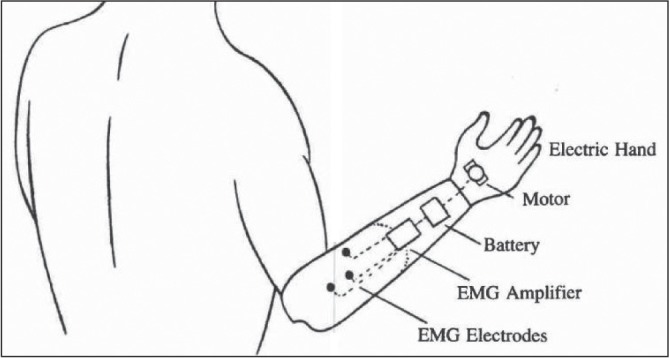
Myoelectric below-elbow prosthesis, controlled by electomyographic (EMG) potentials from residual muscles at the amputation stump. Image reprinted with permission from J Prosthet Orthot Online Library: Billock JN. Upper limb prosthetic terminal devices: Hands versus hooks. Clin Prosthet Orthot 1986;10:57–65
Figure 11).
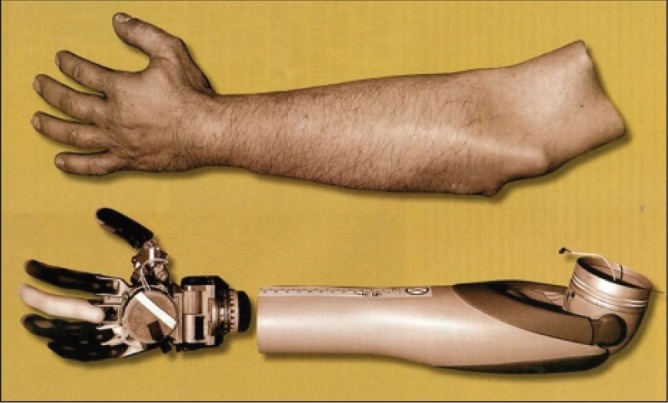
Myoelectric prostheses may be covered with realistic silicone skin overlays designed to match the size, skin tone, hair distribution, nail characteristics, etc, of the amputee. Image credit: The Johns Hopkins University Applied Physics Laboratory <www.jhuapl.edu/newscenter/pressreleases/2007/070426_image2.asp>
In contrast to body-powered prostheses, however, myoelectric prostheses are externally powered and must be recharged regularly (22,23). Learning to isolate muscle signals is tedious, involving multiple training phases, and complex movements requiring simultaneous articulation at the fingers, wrist and elbow may not be possible (24). There is a delay between initiation of movement command and mechanical response, and minute variations, such as shifting electrode positions or changing skin conditions (eg, sweating), may interfere with EMG signals (21). Due to the lack of sensory feedback, visual input must be constant, which is tiring, prone to error and unnatural (25). While cosmetic overlays are impressive in their realism, durability is an issue, with users complaining of frequent glove replacements due to wear, cuts and stains (19).
The use of osseointegration, the direct attachment of a titanium fixture into living bone, eliminates the need for a socket and increases stability and comfort at the interface between prosthesis and residual limb (Figure 12). Osseointegration was developed in the 1950s by Swedish surgeon Per-Ingvar Brånemark, but it was his son Rickard Brånemark who pioneered its application to extremity prostheses (26). By providing stable fixation, osseointegrated prostheses eliminate socket-related problems, such as chafing and sweating, while increasing the amputee’s range of motion (27). The intimate prosthesis-skeletal junction also allows users to experience improved pressure and vibratory sensation (28). Between 1990 and 2010, Brånemark’s team fitted 10 transradial and 16 transhumeral osseointegrated prostheses. Only three patients were later unable to use their prosthesis due to implant fracture, traumatic damage or incomplete integration (27). Infection and implant cost are major limitations to greater adoption of osseointegration in upper extremity amputees.
Figure 12).

A to C Using osseointegration, a titanium fixture is surgically attached to the bone at the site of amputation which enables a myoelectric prosthesis to be connected reliably. The direct attachment eliminates the need for a socket and ensures stable fixation, thereby improving function. Image reprinted with permission from Elsevier: Kang NV, Pendegrass C, Marks, L, Blunn G. Osseocutaneous integration of an intraosseous transcutaneous amputation prosthesis implant used for reconstruction of a transhumeral amputee: Case report. J Hand Surg Am 2010;35:1130–4
Despite widespread availability, myoelectric technology is expensive and may not be covered by insurance plans. In the 1990s, a myoelectric prosthesis with a terminal device cost approximately six times more for a below-elbow amputee than a body-powered prosthesis. In Canada, transradial myoelectric hands cost from $7,500 to $29,500, and transhumeral myoelectric prostheses cost up to $80,000; in comparison, a conventional body-powered prosthesis may cost approximately $5,500 (22).
INTUITIVE MYOELECTRIC CONTROL WITH TARGETED REINNERVATION
A major advancement in intuitive artificial limb control is via the technique of targeted motor reinnervation (TMR), first described in 2004 by Dr Todd Kuiken and Dr Gregory Dumanian in the US (29). By rerouting the cut (ie, amputated) peripheral nerves from an amputated limb to intact spare (target) muscles, the resultant EMG signals of the target muscles now represent motor input to the missing limb muscles (Figure 13) (30). For example, if the median nerve is transferred into the middle pectoralis major muscle belly, then when the amputee thinks ‘flex digits’, the middle region of the pectoralis major will contract, generating a robust EMG to close a prosthetic hand. Unlike body-powered and conventional myoelectric prostheses, TMR is intuitive and enables patients to simultaneously move multiple joints, such as opening and closing the prosthesis while flexing and extending the elbow, increasing the speed of task performance by two- to sixfold (21,31).
Figure 13).
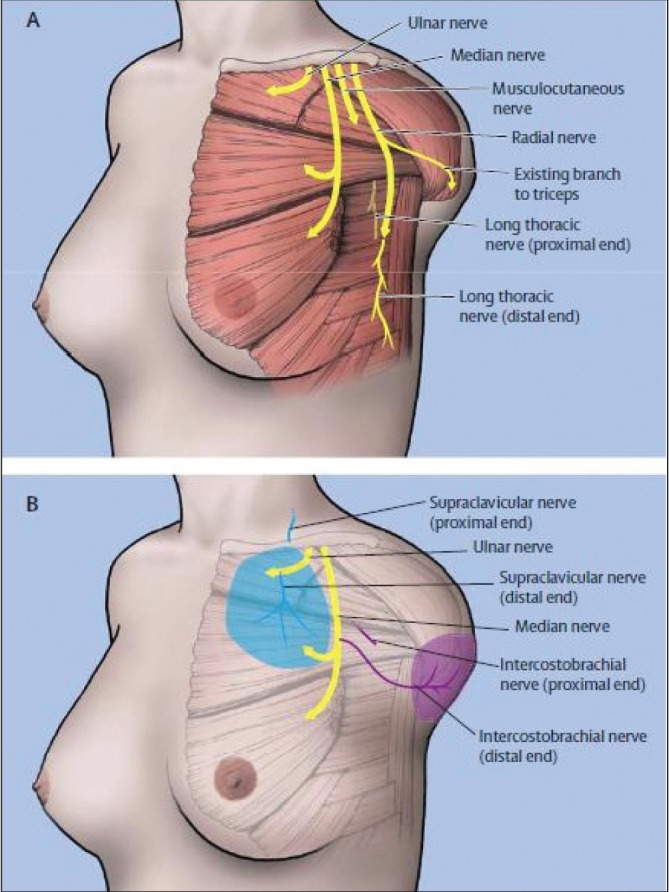
Targeted motor reinnervation (Panel A) and targeted sensory reinnervation (Panel B) involve the surgical re-routing of stump nerves to a denervated target muscle or cutaneous area. Contraction of the reinnervated target muscle enables intuitive control of a myoelectric prosthesis and stimulation of reinnervated skin permits sensory feedback. Image reprinted with permission from Elsevier: Kuiken TA, Miller LA, Lipschutz RD, et al. Targeted reinnervation for enhanced prosthetic arm function in a woman with a proximal amputation: A case study. Lancet 2007;369(9559):371–80
In addition to improved motor control, early TMR patients were found to have sensory recovery in the skin overlying the reinnervated muscle. When reinnervated skin was stimulated, sensation was perceived in the body region the amputated nerve used to innervate; that is, the amputee felt touch on a particular part of the missing limb (Figure 14) (32). With this knowledge, the targeted reinnervation technique was extended to include reattaching sensory nerves to the main peripheral nerve trunks (30). A variation of this surgical method to identify, separate and redirect individual sensory nerve fibres from the median and ulnar nerves to target cutaneous sensory areas distant from the reinnervated muscle is being developed by a multidisciplinary team at the University of Alberta (Edmonton, Alberta). This technique, known as fascicular targeted sensory reinnervation, creates a discrete spatial sensory hand map over a selected area of receptor skin away from the prosthesis interface. By incorporating a sensory feedback device, the patient is able to feel and, thus, coordinate the strength of force applied by the myoelectric prosthesis when handling an object. Early results show effective recovery of discriminative pressure sensation (up to four discrete levels of force with 75% to 85% accuracy), the ability to grip and release objects, and the ability to discriminate between size (mean [± SD] 93±6% accuracy) and density (100% accuracy) without visual or auditory stimuli (33).
Figure 14).
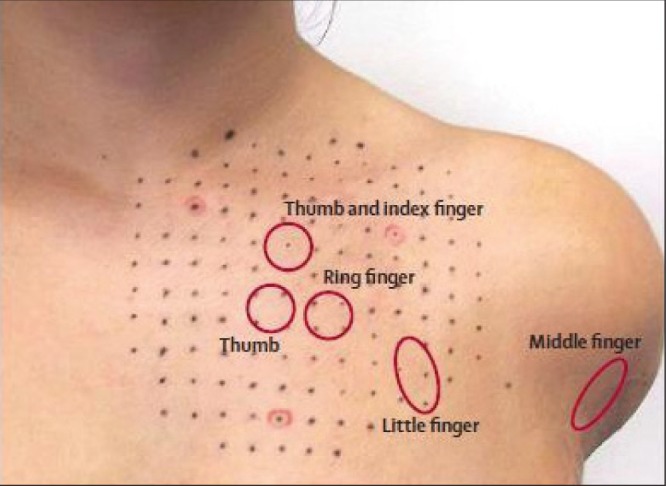
Targeted sensory reinnervation allows the creation of cutaneous ‘maps’ that, when stimulated, cause the patient to feel sensation on the missing hand. Image reprinted with permission from Elsevier: Kuiken TA, Miller LA, Lipschutz RD, et al. Targeted reinnervation for enhanced prosthetic arm function in a woman with a proximal amputation: A case study. Lancet 2007;369:371–80
Reported complications of the targeted reinnervation procedure include cellulitis, seroma and transiently increased phantom limb pain. The cost of the surgical procedure, hospitalization, prosthesis and rehabilitation ranges from USD$150,000 to $250,000 (34). Although early in its development, as of 2011, targeted reinnervation has been performed on >40 patients worldwide (21).
BIOLOGIC HAND RESTORATION: HAND TRANSPLANTATION
One of the most intriguing developments in hand ‘prostheses’ is vascularized composite allotransplantation (VCA), which involves the transfer of multiple tissue types (skin, muscle, nerve, vessels and bone) as a functional unit (Figure 15).
Figure 15).

Hand transplantation is a highly technical procedure requiring the transfer of bone, muscle, nerves and vessels as a functional unit. Photo courtesy of Jewish Hospital; Kleinert, Kutz and Associates Hand Care Center; and University of Louisville <www.handtransplant.com/QuickLinksfortheMedia/PhotoGallery/tabid/87/AlbumID/404-1/Default.aspx>
The first attempt at hand transplantation was performed in Ecuador in 1964 by Dr Robert Gilbert. Unfortunately, after three weeks, the hand was amputated due to acute organ rejection (35,36). In 1998, the world’s first successful hand transplantation was performed in Lyon, France by an international team led by Dr Jean-Michel Dubernard (37). The 48-year-old patient received the right hand of a 41-year-old brain-dead donor in a 13 h procedure (38,39). Despite technical success and rehabilitative progress, poor medication compliance led to graft rejection, and the hand was removed after a total of 29 months (40). A subsequent transplantation, performed in Louisville (Kentucky, USA) in 1999 on 37-year-old Matthew Scott, had greater postoperative success. Scott, now 50 years of age, is the longest surviving hand transplant recipient in the world (38). In 2000, the world’s first bilateral hand transplantation was performed in Lyon, France on a 33-year-old man who lost both of his hands in a blast injury (41).
For motivated and compliant patients, the International Federation of Societies for Surgery of the Hand declared that:
…a remarkably good recovery of sensibility has been documented in all transplanted hands…protective sensation was achieved in all patients within 6 to 12 months…90% showed tactile and 72% of the discriminative sensibility, thus providing a true benefit over prosthetic wear
(39).
Within one year, patients are able to turn doorknobs, pick up objects, hold utensils, catch balls and tie shoes (42). Hand transplantation also restores the normal appearance of a human limb, with an immeasurable psychological benefit (34). Improvement in quality of life has been stated by 75% of hand transplant recipients, with many returning to work (Figure 16) (43).
Figure 16).
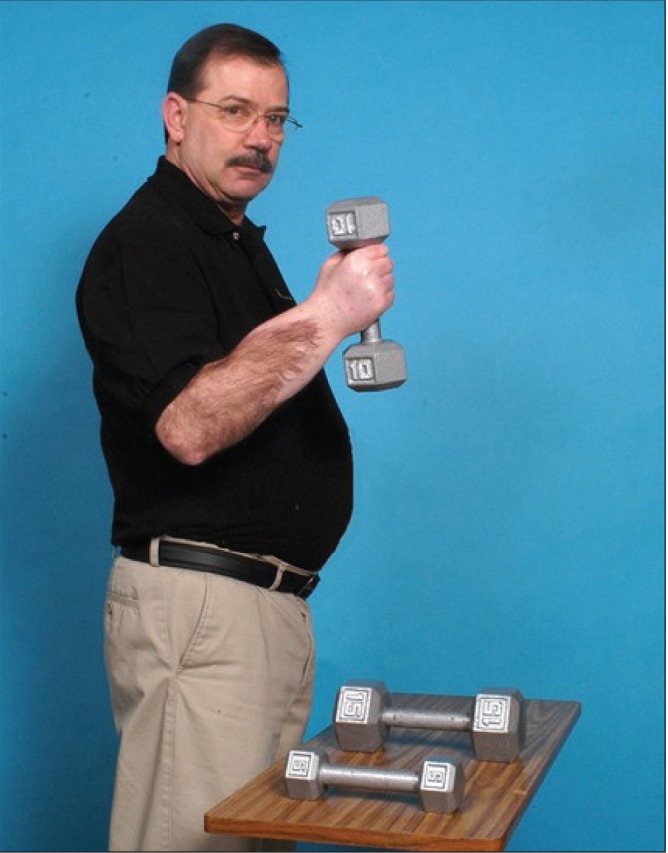
Hand transplant recipients have demonstrated good recovery of function with many returning to work. Photo courtesy of Jewish Hospital; Kleinert, Kutz and Associates Hand Care Center; and University of Louisville <www.handtransplant.com/QuickLinksfortheMedia/PhotoGallery/tabid/87/AlbumID/404-30/Default.aspx>
Despite these successes, hand transplantation is a topic of intense controversy due to associated complications, ethical concerns and unique patient considerations. Immunosuppression is crucial because each tissue in a composite allograft differs in its antigenicity and may be rejected by unique humoral or cellular mechanisms. Typical protocols include prednisone, tacrolimus and mycophenolate mofetil, with complications including opportunistic infections, skin cancer, sepsis and renal failure (43). The long-term effects are unknown, but chronic organ rejection has yet to be observed. Unlike solid organ transplantation, however, the goal of hand transplantation is not to save a life, but to improve the quality of life. With this in mind, critics question the ethics of subjecting a patient to the consequences of life-long immunosuppression when other options for hand replacement are widely available. Others emphasize that not all transplant patients achieve satisfactory tactile control, grip strength or thermoregulation (44). Psychological prescreening for highly motivated patients is crucial because the patient’s commitment to rigorous rehabilitation and immunosuppression is of paramount importance to the overall success of the procedure.
Currently, 30 single hand and 21 double hand transplantations have been performed worldwide (45). Although the costs are estimated to be >$500,000 (46), hand transplantation is the most frequently performed VCA procedure. In 2010, the Mayo Clinic in Rochester (Minnesota, USA) created the first nonexperimental hand transplantation program in North America (47). No hand transplantations have been performed yet in Canada, but work is underway to develop a VCA program in Ontario. The University of Toronto (Toronto, Ontario) has submitted a proposal for upper extremity transplantation to the Ministry of Health for approval. Progress in immunoregulatory protocols with decreased toxicity is a major step toward increasing acceptance for hand transplantation.
CONCLUSION AND THE FUTURE
The act of replacing a missing hand to restore both function and form has challenged humans for millennia. While materials and designs have evolved greatly, we have yet to build or create a totally satisfactory substitute for the 41,000 individuals in the US with major upper limb amputations (48).
The future of hand replacement is exciting. There is no doubt that current technology – body-powered prostheses, myoelectric prostheses, targeted reinnervation and hand transplantation – will be improved on and become more accessible. With cutting-edge advancements in regenerative medicine and tissue engineering, however, prostheses could one day become obsolete. The idea of a ‘petri dish hand’ is particularly intriguing; the ability to create a phenotypically identical hand to replace a severed one could provide optimal integration in terms of biological compatibility, functional control, social communication, sensory feedback and, of course, aesthetics.
Acknowledgments
The authors thank Dr Dawna M Gilchrist, Director of the History of Medicine Program, University of Alberta, and Dr Jacqueline S Hebert, Associate Research Chair in Clinical Rehabilitation, University of Alberta, for their generous support and guidance in the preparation of this work.
REFERENCES
- 1.Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. South Med J. 2002;95:875–83. doi: 10.1097/00007611-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Pliny’s Natural History . In: Book VII, Chapter XXVIII. Rackham H, Jones WHS, Eicholz DE, Heinemann W, translators. < www.masseiana.org/pliny.htm#BOOKXXVIII> (Accessed July 2, 2012) [Google Scholar]
- 3.Putti V. Historical prostheses. Scritti Medici. 1925;IX(4 to 5) First published La chirurgia degli organi di movimento. [Google Scholar]
- 4.Paré A. Les Oeuvres d’Ambroise Paré. Quatriesme Edition. Paris: Gabriel Buon, Avec privilege du Roy; 1585. < wwwnlm.nih.gov/exhibition/historicalanatomies/pare_home.html> (Accessed February 3, 2013) [Google Scholar]
- 5.Meier RH. Functional Restoration of Adults and Children with Upper Limb Amputation. New York: Demos Medical Publishing; 2004. History of arm amputation, prosthetic restoration, and arm amputation rehabilitation; pp. 1–8. [Google Scholar]
- 6.Wyse WM. Macmillan’s Magazine. XL. London: 1879. Alms and Legs in France; pp. 438–440. < http://books.google.ca/books?id=nmsJAAAAQAAJ&source=gbs_navlinks_s>. (Accessed July 4, 2012) [Google Scholar]
- 7.Sauerbruch F. Die willkürlich bewegbare künstliche Hand Eine Anleitung für Chirurgen und Techniker. Berlin: J. Springer; 1916. [Google Scholar]
- 8.Max Planck Institute for the History of Science, Berlin The Virtual Laboratory – Essays and Resources on the Experimentalization of Life. Excerpt from the movie: Die willkürlich bewegbare künstliche Hand. < http://vlp.mpiwg-berlin.mpg.de/library/data/lit38416> (Accessed July 9, 2012) [Google Scholar]
- 9.Petri RP, Aguila E. The military upper extremity amputee. Phys Med Rehabil Clin N Am. 2002;13:17–43. doi: 10.1016/s1047-9651(03)00070-6. [DOI] [PubMed] [Google Scholar]
- 10.The War Amps Who We Are: History. < www.waramps.ca/history.html> (Accessed July 20, 2012)
- 11.Childress DS. Historical aspects of powered limb prostheses. Clin Prosthet Orthot. 1985;9:2–13. [Google Scholar]
- 12.About CAPO Canadian Association for Prosthetics and Orthotics. < www.pando.ca/about.php#2> (Accessed July 20, 2012)
- 13.Gaine WJ, Smart C, Bransby-Zachary M. Upper limb traumatic amputees. J Hand Surg (British and European Volume) 1997;22:73–6. doi: 10.1016/s0266-7681(97)80023-x. [DOI] [PubMed] [Google Scholar]
- 14.Østlie K, Lesjø IM, Franklin RJ, et al. Prosthesis use in adult acquired major upper-limb amputees: Patterns of wear, prosthetic skills and the actual use of prostheses in activities of daily life. Disabil Rehabil Assist Technol. 2012;7:479–93. doi: 10.3109/17483107.2011.653296. [DOI] [PubMed] [Google Scholar]
- 15.Reiter R. Eine neue Electrokunsthand. Grenzgebiete der Medizin. 1948;4:133–5. [PubMed] [Google Scholar]
- 16.Scott RN. Myoelectric control of prostheses: A brief history. Presentation at Proceedings of the 1992 MyoElectric Controls/Powered Prosthetics Symposium; Fredericton. August, 1992. [Google Scholar]
- 17.Sherman ED. A Russian Bioelectric-Controlled Prosthesis. Can Med Assoc J. 1964;91:1268–70. [PMC free article] [PubMed] [Google Scholar]
- 18.Behrend C, Reizner W, Marchessault JA, et al. Update on advances in upper extremity prosthetics. J Hand Surg Am. 2011;36:1711–7. doi: 10.1016/j.jhsa.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 19.Scott RN, Parker PA. Myoelectric prostheses: State of the art. J Med Eng Technol. 1988;12:143–51. doi: 10.3109/03091908809030173. [DOI] [PubMed] [Google Scholar]
- 20.Parker P, Englehart K, Hudgins B. Myoelectric signal processing for control of powered limb prostheses. J Electromyogr Kinesiol. 2006;16:541–8. doi: 10.1016/j.jelekin.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Schultz AE, Kuiken TA. Neural interfaces for control of upper limb prostheses: The state of the art and future possibilities. PMR. 2011;3:55–67. doi: 10.1016/j.pmrj.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 22.WorkSafeBC Evidence-Based Practice Group. Edeer D, Martin CW. Upper limb prostheses – a review of the literature with a focus on myoelectric hands. Richmond, BC: WorksafeBC Evidence-Based Practice Group; Feb, 2011. < http://worksafebc.com/health_care_providers/Assets/PDF/UpperLimbProstheses2011.pdf> (Accessed September 20, 2012) [Google Scholar]
- 23.McFarland LV, Hubbard Winkler SL, Heinemann AW, et al. Unilateral upper-limb loss: Satisfaction and prosthetic-device use in veterans and service members from Vietnam and OIF/OEF conflicts. J Rehabil Res Dev. 2010;47:299–316. doi: 10.1682/jrrd.2009.03.0027. [DOI] [PubMed] [Google Scholar]
- 24.The War Amps Using a Myoelectric Arm to its Full Potential. < www.waramps.ca/nac/life/myoarm.html> (Accessed September 20, 2012)
- 25.Light CM, Chappell PH, Hudgins B, et al. Intelligent multifunction myoelectric control of hand prostheses. J Med Eng Technol. 2002;26:139–46. doi: 10.1080/03091900210142459. [DOI] [PubMed] [Google Scholar]
- 26.Brånemark R, Ohrnell LO, Nilsson P, et al. Biomechanical characterization of osseointegration during healing: An experimental in vivo study in the rat. Biomaterials. 1997;18:969–78. doi: 10.1016/s0142-9612(97)00018-5. [DOI] [PubMed] [Google Scholar]
- 27.Jönsson S, Caine-Winterberger K, Brånemark R. Osseointegration amputation prostheses on the upper limbs: Methods, prosthetics and rehabilitation. Prosthet Orthot Int. 2011;35:190–200. doi: 10.1177/0309364611409003. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs R, Brånemark R, Olmarker K, et al. Evaluation of the psychophysical detection threshold level for vibrotactile and pressure stimulation of prosthetic limbs using bone anchorage or soft tissue support. Prosthet Orthot Int. 2000;24:133–42. doi: 10.1080/03093640008726536. [DOI] [PubMed] [Google Scholar]
- 29.Kuiken TA, Dumanian GA, Lipschutz RD, et al. The use of targeted muscle reinnervation for improved myoelectric prosthesis control in a bilateral shoulder disarticulation amputee. Prosthet Orthot Int. 2004;28:245–53. doi: 10.3109/03093640409167756. [DOI] [PubMed] [Google Scholar]
- 30.Kuiken TA, Miller LA, Lipschutz RD, et al. Targeted reinnervation for enhanced prosthetic arm function in a woman with a proximal amputation: A case study. Lancet. 2007;369:371–80. doi: 10.1016/S0140-6736(07)60193-7. [DOI] [PubMed] [Google Scholar]
- 31.Miller LA, Lipschutz RD, Stubblefield KA, et al. Control of a six degree of freedom prosthetic arm after targeted muscle reinnervation surgery. Arch Phys Med Rehabil. 2008;89:2057–65. doi: 10.1016/j.apmr.2008.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marasco PD, Schultz AE, Kuiken TA. Sensory capacity of reinnervated skin after redirection of amputated upper limb nerves to the chest. Brain. 2009;132:1441–8. doi: 10.1093/brain/awp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hebert JS, Olson JL, Morhart MJ, et al. Novel targeted sensory reinnervation technique to restore functional hand sensation after transhumeral amputation. IEEE Trans Neural Syst Rehabil Eng. doi: 10.1109/TNSRE.2013.2294907. (In press) [DOI] [PubMed] [Google Scholar]
- 34.Agnew SP, Ko J, De La Garza M, et al. Limb transplantation and targeted reinnervation: A practical comparison. J Reconstr Microsurg. 2012;28:63–8. doi: 10.1055/s-0031-1281522. [DOI] [PubMed] [Google Scholar]
- 35.Gilbert R. Transplant is successful with a cadaver forearm. Med Trib Med News. 1964;5:20. [Google Scholar]
- 36.Gilbert R. Hand transplanted from cadaver is reamputated. Med Trib Med News. 1964;5:23. [Google Scholar]
- 37.Dubernard JM, Owen E, Herzberg G, et al. Human hand allograft: Report on first 6 months. Lancet. 1999;353:1315–20. doi: 10.1016/S0140-6736(99)02062-0. [DOI] [PubMed] [Google Scholar]
- 38.Composite Tissue Allotransplantation Transplant Recipients. < www.handtransplant.com/ThePatients/tabid/66/Default.aspx> (Accessed July 14, 2012)
- 39.International Federation of Societies for Surgery of the Hand. Moran SL. Hand Transplantation – IFSSH Report 2010. < www.ifssh.info/Handtransplantation.pdf> (Accessed September 2, 2012) [DOI] [PubMed]
- 40.Kanitakis J, Jullien D, Petruzzo P, et al. Clinicopathologic features of graft rejection of the first human hand allograft. Transplantation. 2003;76:688. doi: 10.1097/01.TP.0000079458.81970.9A. [DOI] [PubMed] [Google Scholar]
- 41.Dubernard JM, Petruzzo P, Lanzetta M, et al. Functional results of the first human double-hand transplantation. Ann Surg. 2003;238:128–36. doi: 10.1097/01.SLA.0000078945.70869.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaufman CL, Blair B, Murphy E, et al. A new option for amputees: Transplantation of the hand. J Rehabil Res Dev. 2009;46:395–404. [PubMed] [Google Scholar]
- 43.Petruzzo P, Lanzetta M, Dubernard JM, et al. The International Registry on Hand and Composite Tissue Transplantation. Transplantation. 2010;90:1590–4. doi: 10.1097/TP.0b013e3181ff1472. [DOI] [PubMed] [Google Scholar]
- 44.Jones NF. Concerns about human hand transplantation in the 21st century. J Hand Surg Am. 2002;27:771–87. doi: 10.1053/jhsu.2002.34373. [DOI] [PubMed] [Google Scholar]
- 45.International Registry on Hand and Composite Tissue Transplantation World Experience. < www.handregistry.com/page.asp?page=4> (Accessed November 14, 2012)
- 46.Chung KC, Oda T, Saddawi-Konefka D, et al. An economic analysis of hand transplantation in the United States. Plast Reconstr Surg. 2010;125:589–98. doi: 10.1097/PRS.0b013e3181c82eb6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Amer H, Carlsen BT, Dusso JL, et al. Hand transplantation. Minnesota Medicine. 2011;94:40–43. [PubMed] [Google Scholar]
- 48.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]


