Abstract
Self-compassion refers to having an accepting and caring orientation towards oneself. Although self-compassion has been studied primarily in healthy populations, one particularly compelling clinical context in which to examine self-compassion is social anxiety disorder (SAD). SAD is characterized by high levels of negative self-criticism as well as an abiding concern about others’ evaluation of one’s performance. In the present study, we tested the hypotheses that (1) people with SAD would demonstrate less self-compassion than healthy controls (HCs), (2) self-compassion would relate to severity of social anxiety and fear of evaluation among people with SAD, and (3) age would be negatively correlated with self-compassion for people with SAD, but not for HC. As expected, people with SAD reported less self-compassion than HCs on the Self-Compassion Scale and its subscales (Neff, 2003b). Within the SAD group, lesser self-compassion was not generally associated with severity of social anxiety, but it was associated with greater fear of both negative and positive evaluation. Age was negatively correlated with self-compassion for people with SAD, whereas age was positively correlated with self-compassion for HC. These findings suggest that self-compassion may be a particularly important target for assessment and treatment in persons with SAD.
Keywords: self-compassion, social anxiety, social phobia, self, compassion, treatment
After being rejected following a job interview or a date, most people engage in some degree of self-criticism. Such self-criticism is perhaps most intense in interpersonal contexts in which people feel judged (Blatt, 1991). For many, this automatic reaction is so common and habitual that they withstand the deluge of self-directed negativity without appreciating that they could have treated themselves in a kinder way. One kinder and potentially more adaptive stance in the face of life’s difficulties is self-compassion, which refers to having a warm and accepting stance towards the aspects of oneself that are disliked or painful (Neff, 2003a).
Self-Compassion
Self-compassion is a relatively new construct in psychology. Neff (Neff, 2003b) describes it as: 1) being kind and understanding towards oneself in instances of pain or failure rather than being harshly self-critical; 2) perceiving one’s experiences as part of the larger human experience rather than seeing them as isolating; and 3) holding painful thoughts and feelings in mindful awareness rather than over-identifying with them. When confronting suffering, inadequacy or failure, self-compassionate individuals offer themselves warmth and non-judgmental understanding rather than belittling their pain or berating themselves with self-criticism. This process also involves recognizing that being imperfect, making mistakes, and encountering life difficulties are part of the shared human experience — something that we all go through rather than being something that happens to “me” alone.
Social Anxiety Disorder (SAD)
Although everyone might benefit from having a more self-compassionate stance, one group that has demonstrated particularly high levels of self-criticism (Cox, Fleet, & Stein, 2004) is people with social anxiety disorder (SAD). SAD, the fourth most common psychiatric disorder (Kessler, et al., 2005), is often debilitating. It involves significant emotional distress and functional impairment in work and social domains (Acarturk, de Graaf, van Straten, Have, & Cuijpers, 2008; Schneier, et al., 1994; Tolman, et al., 2009). Cognitive models suggest that persons with SAD view the social world through a lens which emphasizes excessive negative self-judgment. These cognitive models suggest that fear of social situations, avoidance of social situations, and fear of negative evaluation are fundamental features of SAD (Clark & Wells, 1995; R. G. Heimberg, Brozovich, & Rapee, 2010; Hofmann, 2007; Rapee & Heimberg, 1997a). Recent work has also demonstrated a robust relationship between SAD and fear of positive evaluation as well (Fergus, et al., 2009; Weeks, Heimberg, Rodebaugh, & Norton, 2008).
Self-Compassion and SAD
In light of these cognitive biases and social difficulties, a logical “antidote” for those with SAD is self-compassion (Neff, 2003a). In the case of SAD, self-compassion might entail accepting oneself and treating oneself kindly in the face of social failure, uncontrollable negative self-critical thinking, or high physiological arousal. To date, no studies have investigated self-compassion in clinical samples of persons with SAD, although the closely related construct of mindfulness has been shown to be negatively correlated with social anxiety in a convenience sample of college students (Rasmussen & Pidgeon, in press). Self-compassion was a more robust predictor of symptom severity and quality of life in a recent study of 504 people seeking self-help for mixed anxiety and depression (Van Dam, Sheppard, Forsyth, & Earleywine, 2011). What is known about self-compassion’s relationship to anxiety and negative affect comes largely from studies of healthy samples which suggest that greater self-compassion is associated with many adaptive traits and characteristics — greater life satisfaction, emotional intelligence, social connectedness, and mastery of goals, as well as lesser self-criticism, depression, anxiety, rumination, thought suppression, perfectionism, performance goals, and disordered eating (Adams & Leary, 2007; Neff, 2003a; Neff, Hseih, & Dejitthirat, 2005; Neff, Rude, & Kirkpatrick, 2007). Such findings suggest that individuals with SAD should have lower levels of self-compassion than healthy control participants (HCs) and that self-compassion should be negatively correlated with severity of social anxiety and related constructs (fear of positive or negative evaluation by others Carleton, Collimore, & Asmundson, 2007; R. G. Heimberg, et al., 2010; Weeks, Heimberg, Rodebaugh, et al., 2008) among persons with SAD.
One core feature of SAD is its stability across the lifespan (Lovibond & Rapee, 1993). SAD is unlikely to remit spontaneously; it is a chronic condition with a relatively stable course that typically has its onset by the mid-teens and has an average duration of 20 years at the time of presentation (Davidson, Hughes, George, & Blazer, 1993; Witchen & Beloch, 1996). Unlike the preservation or even enhancement of socioemotional functioning associated with age in normal samples (Urry & Gross, 2010), it seems likely that for individuals with SAD, self-compassion would be negatively correlated with age, as the number of socially stressful life-events, anxious symptology, and limitations of SAD are compounded over time. The additive nature of social stressors may degrade one’s capacity for generating self-kindness and care over the life-span.
The Present Study
The aim of the present study was to examine self-compassion and its correlates in a treatment-seeking sample of persons with in SAD. Based on previous research, the following hypotheses were tested: First, we expected that, compared to healthy controls (HCs), persons with SAD would report lesser self-compassion on the Self-Compassion Scale (SCS; Neff, 2003a). Second, we expected that lower self-compassion as indexed by scores on the total scale and six subscales would be associated with greater severity of social anxiety and greater fear of both negative and positive social evaluation in persons with SAD. Third, we expected that age would be negatively correlated with self-compassion for people with SAD, but not for HC.
Method
Participants
Participants were 72 persons with a principal diagnosis of generalized SAD and 40 HCs (see Table 1 for demographic characteristics of study participants). Diagnostic status was determined using the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994) administered by doctoral-level clinical psychologists (KW or PG). Only persons with a score of 4 or more on the ADIS-IV-L Clinician’s Severity Rating for SAD and ratings of 4 or more for 5 or more social situations (all scales 0–8) or HCs with no history of Axis I DSM-IV disorders were enrolled. Among persons with SAD, current Axis I co-morbidity included 16 with generalized anxiety disorder, 7 with specific phobia, 7 with major depression, and 5 with dysthymia. Past Axis I co-morbidity included 19 with past major depression, 1 with past dysthymia, and 5 with past substance abuse. Thirty-nine persons with SAD reported past (i.e., ended more than 1 year ago) experience with psychotherapy, and 22 reported past psychotropic medication use.
Table 1.
Demographic and Clinical Measures for Social Anxiety Disorder (SAD) and Healthy Control (HC) Participants
| SAD (n = 72) | HC (n = 40) | |
|---|---|---|
| Age (years) | 33.8±8.2 | 33.9±9.2 |
| Gender | ||
| Men | 33 | 20 |
| Women | 39 | 20 |
| Education (years) | 16.8±1.8 | 17.6±1.6 |
| Ethnicity | ||
| Caucasian | 34 (47.2%) | 20 (50%) |
| Asian | 27 (37.5%) | 15 (37.5%) |
| Latino | 6 (8.3%) | 1 (2.5%) |
| More than one | 4 (5.5%) | 4 (10%) |
| Pacific Islander | 1 (1.3%) | 0 (0%) |
Exclusion Criteria
For the purposes of a larger study, participants were excluded if they reported current use of any psychotropic medication, current psychotherapy, history of neurological or cardiovascular disorders, diabetes mellitus, thyroid disease, head trauma with loss of consciousness greater than five minutes, daily cigarette use, or left-handedness. Persons with SAD were also excluded if they met criteria for past psychotic or bipolar disorder or any current DSM-IV (American Psychiatric Association, 1994) Axis I disorder assessed by the ADIS-IV-L with the exception of generalized anxiety disorder, depression, dysthymia, agoraphobia, or specific phobia. HCs were excluded if they met criteria for any current or past DSM-IV Axis I psychiatric disorder. All participants passed a MRI safety screen for a separate data collection session not included in this paper.
Procedure
Participants with SAD and HC were recruited through web-based community listings and referrals from local mental health clinics. Following a telephone screening to determine initial eligibility, participants were assessed using the ADIS-IV-L. If eligible, participants were administered a battery of online questionnaires in a separate laboratory session.
Measures
Self-Compassion
The Self-Compassion Scale (SCS; Neff, 2003b), a 26-item self-report measure which employs a 5-point Likert-type scale ranging from 1 (Almost never) to 5 (Almost always), assesses six facets of presence or absence of self-compassion: Self-kindness (5 items) refers to responding to difficulties or set-backs in a warm and understanding manner rather than with harshness and criticism. An example of self-kindness is: “I’m kind to myself when I’m experiencing suffering.” Self-judgment (5 items) refers to the opposite of self-kindness. An example of self-judgment is: “I’m intolerant and impatient towards those aspects of my personality I don’t like.” Common humanity (4 items) assesses the person’s beliefs that we are not alone, our experience is shared by others, and any suffering is just part of the human condition. An example of common humanity is: “When things are going badly for me, I see the difficulties as part of life that everyone goes through.” Isolation (4 items) is the opposite of common humanity. An example of isolation is: “When I fail at something that’s important to me I tend to feel alone in my failure.” Mindfulness (4 items) is a non-judgmental, receptive mind state in which one observes thoughts and feelings as they are, without trying to suppress or deny them. An example of mindfulness is: “When I’m feeling down I try to approach my feelings with curiosity and openness.” Over-identification (4 items) is when one becomes overwhelmed with negative emotion and identifies with it. An example of over-identification is: “When something painful happens I tend to blow the incident out of proportion.” Research by Neff has indicated strong convergent and discriminant validity (no correlation with social desirability), as well as good test-retest reliability (Neff, 2003b; Neff, et al., 2007). In the present sample, Cronbach alphas for the subscales were as follows: Self-kindness: .81; Self-judgment: .90; Common humanity: .81; Isolation: .93; Mindfulness: .78; and Over-Identification: .86. The Cronbach’s alpha for the full scale was .96.
Social Anxiety Scales
The self-report version of the Liebowitz Social Anxiety Scale (LSAS-SR; Fresco, et al., 2001; Rytwinski, et al., 2009), derived from the clinician administered Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987), was used to assess both fear and avoidance with respect to 24 specific social situations. These include 11 social interactions (e.g., going to a party) and 13 performance situations (e.g., giving a talk). Participants rate fear or anxiety ranging from 0 (None) to 3 (Severe) and avoidance ranging from 0 (Never, 0%) to 3 (Usually, 68–100%). The scale shows good psychometric characteristics in both clinician-administered (Baker, Heinrich, Kim, & Hoffman, 2002; R. G. Heimberg, Horner, K. J., Juster, H. R., Safren, S. A., Brown, E. J., Schneier, F. R., & Liebowitz, M. R, 1999; Weeks, et al., 2005) and self-report (Fresco, et al., 2001; Rytwinski, et al., 2009) formats. Specifically, there is ample evidence for the test-retest reliability, internal consistency, convergent and discriminant validity, and construct validity of the LSAS in either administration format. In the present sample, Cronbach’s alpha was .87 for the full scale.
The Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998), a 20-item scale that measures social anxiety in a variety of social interaction situations including dyads and groups, uses a 5-point Likert-type scale ranging from 0 (Not at all characteristic or true of me) to 4 (Extremely characteristic or true of me). The SIAS was designed to tap the cognitive, affective, and behavioral reactions to interpersonal situations. Sample items include “I find myself worrying that I won’t know what to say in social situations,” “I feel tense if I am alone with just one person,” and “I tense up if I meet an acquaintance on the street.” Researchers have found the SIAS to have high internal consistency, test-retest reliability and convergent and discriminant validity (Brown, et al., 1997; R. G. Heimberg, Mueller, Holt, Hope, & Liebowitz, 1992; Ries, et al., 1998). In the present sample, Cronbach’s alpha was .97.
Fear of Evaluation Scales
The Brief Fear of Negative Evaluation Scale (BFNE; Leary, 1983) is a 12-item self-report measure assessing concerns about negative evaluation by others. Items are rated on a 5-point Likert-type scale ranging from 0 (not at all characteristic of me) to 5 (extremely characteristic of me). A sample item is “If I know someone is judging me, it has little effect on me.” As suggested by previous research (Rodebaugh, et al., 2004; Weeks, et al., 2005), we conducted our analyses with the eight true-keyed items (BFNE-S). The BFNE-S has demonstrated excellent internal consistency (all α’s > .92), factorial validity, and construct validity in both non-clinical and clinical samples (Rodebaugh, et al., 2004; Weeks, et al., 2005). In the present sample, Cronbach’s alpha for the BFNE-S was .95.
The Fear of Positive Evaluation Scale (FPES; Weeks, Heimberg, & Rodebaugh, 2008) is a 10-item self report measure assessing concerns about positive evaluation by others. Items are rated on a 10-point Likert-type scale ranging from 0 (not at all true) to 9 (very true). Respondents are instructed to respond to items “as though it involves people that you do not know very well.” A sample item is “I feel uneasy when I receive praise from authority figures.” In undergraduate populations, the FPES has demonstrated strong internal consistency (α = .80) and 5-week test–retest reliability (intraclass correlation coefficient = .70) (Weeks, Heimberg, Rodebaugh, et al., 2008). In SAD, the FPES has demonstrated adequate reliability and good convergent and discriminant validity (Fergus, et al., 2009). In the present sample, Cronbach’s alpha was .85.
Depression and Anxiety Scales
Beck Depression Inventory-II (BDI-II) (Beck, Steer, & Brown, 1996). The BDI-II assesses depressive symptoms. The scale contains 21-items rated from 0 to 3 in terms of intensity, with scores ranging from 0–63. Sample areas of assessment include, feelings of worthlessness, loss of interest, and loss of pleasure. The BDI-II has demonstrated high internal consistency in outpatient samples (Beck, et al., 1996). The original BDI exhibited good internal consistency, validity, and test-retest reliability in a sample of patients with SAD (Coles, Gibb, & Heimberg, 2001). Internal consistency was good in the current samples. In the present sample, Cronbach’s alpha was .92.
Spielberger State Trait Anxiety Inventory (STAI-T) (Spielberger, Gorsuch, & Lushene, 1970). The STAI-T assesses the general frequency of anxiety symptoms. The scale contains 20-items rated on a 4 point scale of ‘almost never’, ‘sometimes’, ‘often’ and ‘almost always’. A sample item from the scale is: “I feel nervous and restless.” The STAI-T has demonstrated high internal consistency in outpatient samples (average >.89). The STAI-T exhibits good internal consistency, validity, and test-retest reliability (average r = .88) (Gros, Antony, Simms, & McCabe, 2007). Internal consistency was good in the current samples. In the present sample, Cronbach’s alpha was .91.
Results
There were no demographic differences between the SAD and HC groups. The two groups did not differ significantly on gender, age, education, or ethnicity (Table 1). Compared to HCs, persons with SAD reported significantly greater symptoms of social anxiety on the LSAS-SR and SIAS, and greater fear of evaluation on the BFNE-S and the FPES (Table 2).
Table 2.
Social Anxiety Symptoms and Fear of Evaluation in SAD and HC Participants
| SAD Mean ± SD | HC Mean ± SD | t | partial ηp2 | |
|---|---|---|---|---|
| LSAS-SR | 87.5±18.6 | 15.4±10.4 | .810 | |
| SIAS | 52.4±13.3 | 14.1±9.2 | −19.5*** | .688 |
| BFNE-S | 49.9±5.3 | 28.2±6.6 | −9.86*** | .758 |
| FPES | 48.7±15.7 | 19.7±11.7 | −15.1*** | .469 |
Note:
p < .001.
LSAS-SR= Liebowitz Social Anxiety Scale – Self Report Version, SIAS= Social Interaction Anxiety Scale, BFNE-S=Brief Fear of Negative Evaluation Scale (true-keyed item total), FPES=Fear of Positive Evaluation Scale.
Self-Compassion in Individuals with SAD versus HC
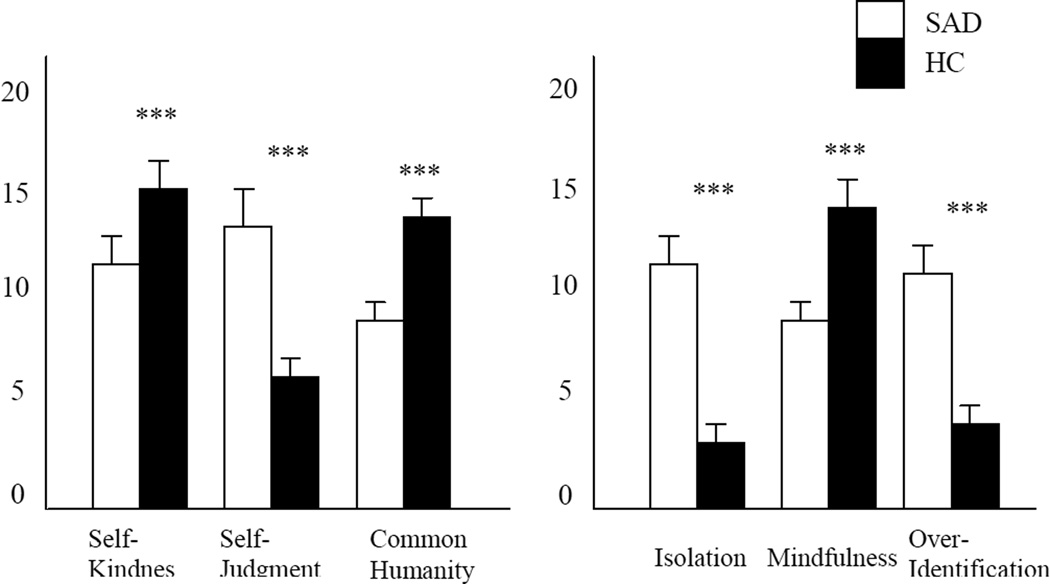
A between-groups t-test showed that, compared to HCs, persons with SAD reported lesser overall self-compassion t(110) = 11.61, p < .001; SAD: M = 2.2, SD = 0.50; HC: M = 3.5, SD = 0.62, partial ηp2 = 0.55. Further analyses revealed that, compared to HCs, persons with SAD achieved significantly lower scores on each of the six subscales of the SCS (all ts > 2.8; all ps < .001; all partial ηp2 = .24–.54; see Figure 1). The group comparisons for the total scale and all six subscales remained significant when controlling for the BDI-II and the STAI-T (all Fs > 14.07; all ps < .001; all partial ηp2 = .27–.69).
Figure 1.
Self-Compassion in Participants with Social Anxiety Disorder (SAD) and Healthy Control Participants (HC)
Self-Compassion, Anxiety Symptoms, and Fear of Social Evaluation
Pearson product-moment correlations showed that greater severity of social anxiety as assessed by either the LSAS-SR or the SIAS was not correlated with total scores on the SCS (Table 3). The SIAS was significantly and positively correlated with the subscales of self-judgment and isolation, but the LSAS-SR did not correlate significantly with any of the SCS subscales.
Table 3.
Correlations Between Self-Compassion and Social Anxiety and Fear of Evaluation in SAD Participants
| LSAS-SR | SIAS | BFNE-S | FPES | |
|---|---|---|---|---|
| Self-Kindness | .07 | −.03 | −.12 | −.27* |
| Self-Judgment | .20 | .28* | .50*** | .29* |
| Common Humanity | −.09 | −.01 | −.12 | −.18 |
| Isolation | .20 | .23* | .28* | .26* |
| Mindfulness | −.12 | .08 | .02 | −.32** |
| Over-Identification | .07 | .19 | .45*** | .23* |
| Total Scale | −.15 | −.18 | −.38*** | −.37* |
Note.
p < .05,
p < .01,
p < .001,
LSAS-SR= Liebowitz Social Anxiety Scale – Self Report Version, SIAS= Social Interaction Anxiety Scale, BFNE-S=Brief Fear of Negative Evaluation Scale (true-keyed item total), FPES=Fear of Positive Evaluation Scale.
Lesser self-compassion was associated with greater fear of both negative and positive evaluation. Both the BFNE-S and FPES were positively correlated with the self-judgment, isolation, and over-identification subscales. The FPES correlated inversely with the self-kindness and mindfulness subscales (Table 3), whereas no other measure of social anxiety or fear of evaluation did so. No measure correlated with the common humanity subscale.
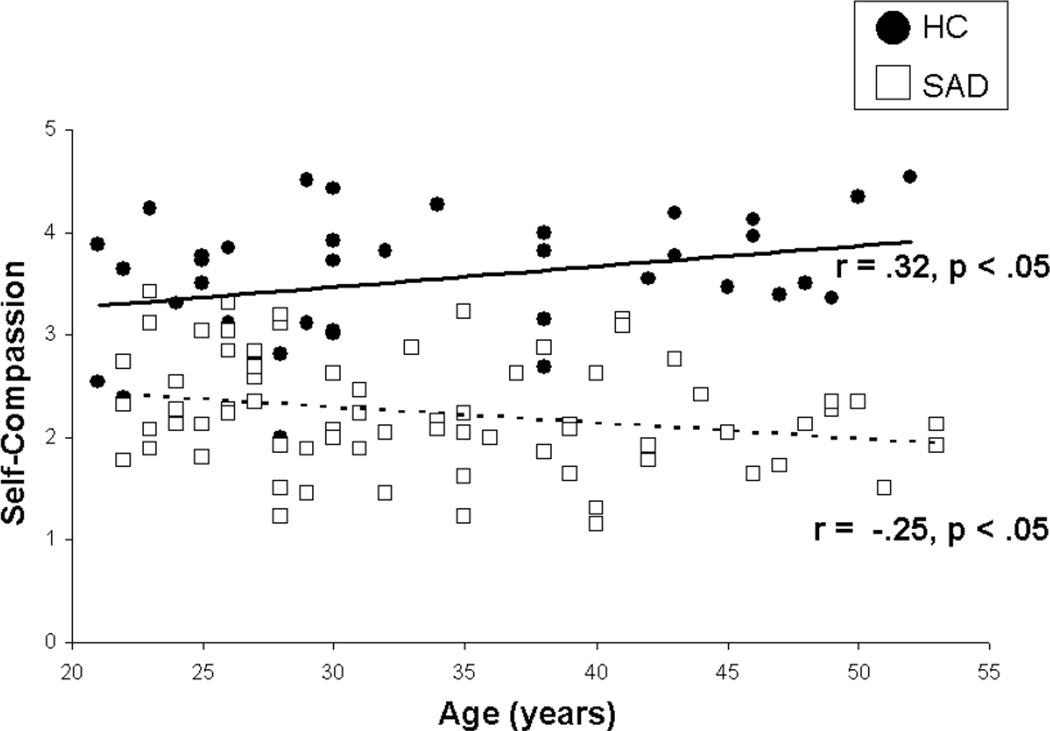
Self-Compassion and Age
In the SAD sample, age was negatively correlated with self-compassion, r(72) = −.24, p < .05. In contrast, age was positively correlated with self-compassion in the HC sample, r(40) = .32, p < .05. These correlations differed significantly (Zdiff = −2.83, p < .01) (see Figure 2).
Figure 2.
Scatterplot of Self-Compassion and Age in Social Anxiety Disorder (SAD) Healthy Control (HC) Samples
Discussion
Our goal in this study was to examine self-compassion in the context of SAD. Our expectation was that (1) people with SAD would demonstrate less self-compassion than HCs, (2) self-compassion would relate to symptom severity and fear of evaluation among people with SAD, and (3) age would be negatively correlated with self-compassion for people with SAD, but not for HC.
Self-Compassion in SAD
Persons with SAD did report less self-compassion than HCs. This finding is consistent with recent research relating SAD to diminished positive cognitions and emotions, such as lack of a positive inferential bias (Hirsch & Matthews, 2000; Huppert, Foa, Furr, Filip, & Mathews, 2003), anticipation of higher intensity negative emotional reactions to positive social events (Gilboa-Schechtman, Franklin, & Foa, 2000), and diminished positive affect and psychological experiences (e.g., curiosity) (Kashdan, 2007). Previous studies have shown that, compared to individuals with lower levels of self-compassion, individuals with higher self-compassion are better able to keep negative situations in perspective and are buffered against feelings of anxiety after experiencing a stressor (M. R. Leary, Tate, E. B., Adams, C. E., Allen, A. B., & Hancock, J, 2007; Neff, et al., 2007). Our findings suggest that people with SAD may not experience the same buffering effect of self-compassion, an area to be further explored.
Previous research has demonstrated a relationship between anxiety, depression and self-compassion (Raes, 2010). The current study is a first to show diminished self-compassion in persons with SAD specifically. We found that persons with SAD had significantly lower levels of self-compassion even when controlling for levels of depression and general anxiety. These findings suggest that a lack of self-compassion may be particularly relevant to patients with SAD.
We also observed significant group differences on all subscales of the self-compassion scale. In comparison to HCs, persons with SAD reported less self-kindness, greater self-judgment, less of a connection to a common humanity, greater isolation in their suffering, less emotional balance in the midst of negative emotions, and feeling more overwhelmed by negative emotions. People with SAD view themselves negatively from the observer perspective (Hackmann, Surawy, & Clark, 1998; Rapee & Heimberg, 1997b; Wells & Papageorgiou, 1999) and engage in excessive post-event rumination (Brozovich & Heimberg, 2008) – distorting their view of themselves in social situations. This distorted self-judgment may be all the more keenly felt, given the inability to take a distanced perspective implied by low scores on the mindfulness subscale of the SCS.
Furthermore, the intense and negative self focus of individuals with SAD may contribute to or be heightened by their sense of isolation and lack of connection with a common humanity such as the millions of other people who endure stress and anxiety in life as well. Cognitive models assert that people with SAD believe that they have little control over their emotional response (Hofmann, 2007), view their social skills as ineffective (Clark & Wells, 1995), and perceive extreme negative judgment by others of their behavior, appearance, and affect (Rapee & Heimberg, 1997). These statements are consistent with elevated scores on the SCS over-identification subscale. It is possible that these several aspects of self-compassion may play a maintaining role in the experience of SAD.
Overall, in theorizing about at a potential link between the cognitive model of SAD (Clark & Wells, 1995; Hofmann, 2007; Rapee & Heimberg, 1997a)and self-compassion, self-compassion may be a separable positive cognitive framework which can be implemented in tandem to the negative cognitive biases inherent in SAD. Self-compassion involves people with SAD becoming mindfully aware of their own conditioned habitual negative biases and interpretations outlined by the cognitive models, and simultaneously generating a caring and supportive stance towards the suffering that these negative biases engender in one’s body, mind and life.
Self-Compassion, Anxiety Symptoms, and Fear of Social Evaluation
To our surprise, the SCS total score did not correlate with the social anxiety measures. However, the SIAS correlated with the self judgment and isolation subscales. A recent study found that these two subscales were the most significant predictors of anxiety symptoms and quality of life in a treatment-seeking sample of people with mixed anxiety and depression (Van Dam, et al., 2011). Negative self-judgment and feelings of isolation may be a particularly important contributor to anxiety in social interactions for people with SAD. Overall, however, within the clinical group of persons with SAD, more severe social anxiety was only mildly related to difficulties in self-compassion. Self-compassion appeared to be more tightly linked to cognitive aspects of social anxiety, specifically fear of evaluation.
Both fear of positive and negative evaluation were associated with less self-compassion in persons with SAD. Research suggests that persons with SAD fear negative evaluation from others, placing great importance on these evaluations rather than their own balanced self-examination (Rodebaugh, et al., 2004; Weeks, et al., 2005). Self-compassion may help shift the evaluation of self-worth from external to more forgiving internal frames of reference. Evidence for this distinction may be related to the difference in mastery-based goals (goals that are related to intrinsic motivation) and performance-based goals (goals that focus on evaluations of success and failure and are motivated by a desire to enhance one’s self-worth or public image) (Dweck, 1986). Self-compassion is positively correlated with mastery-based goals and negatively associated with performance-based goals and lower reactivity to external events (M. R. Leary, Tate, E. B., Adams, C. E., Allen, A. B., & Hancock, J, 2007). Self-compassion may provide greater stability of self-worth and a respect for self and an internal sense of deservingness that mitigate the need for external approval.
Self-Compassion and Age
In HCs, there was a positive relationship between age and self-compassion. Although these data are cross-sectional rather than longitudinal, they are consistent with the view that as individuals progress through life, they naturally have more life experiences to draw upon, many of which are difficult ones. Dealing with life’s circumstances puts an individual in touch with humanity, and these experiences may cultivate self-compassion. Research suggests that older healthy adults more frequently ignore or forget negative information but remember positive information (dubbed the “positivity effect”; see review in Novak & Mather, 2007). Heightened self-compassion in HCs may reflect this positivity bias. Alternatively this finding may reflect an increased ability to regulate emotions (Urry & Gross, 2010) or increased activation of the amygdala and/or medial prefrontal cortex brain regions (e.g., Cacioppo, Berntson, Bechara, Tranel, & Hawkley, in press; Samanez-Larkin & Carstensen, in press) with age.
Unlike HCs, individuals with SAD showed a significant negative association between age and self-compassion. These data are consistent with the possibility that, as individuals with SAD age, there is a deterioration of the positive orientation towards the social self. Because few individuals with SAD receive treatment for SAD, social anxiety often remains a chronic problem throughout their lives (Cairney, et al., 2007), and they may experience ever increasing numbers of anxiety-related negative outcomes. Thus, distorted thinking about the self in SAD may inhibit normative increases in self-compassion and people with SAD may not experience the positive benefits of aging in this socioemotional realm of life. In addition to distorted thinking about the self, older people with SAD may have more life-events that precipitated the onset of the disorder and an exacerbation of symptoms over the years degrading the use of self-compassion.
Treatment Implications
The current study demonstrates that people with SAD have less self-compassion than HC and that the relation between age and self-compassion is positive for HCs but negative for individuals with SAD. People with SAD may have a reduced ability to generate positive thoughts and warmth and kindness toward themselves, and whatever ability they have may degrade further over time. Thus, it may be particularly important to develop self-compassion to possibly buffer against the negative cognitive biases and excessive self-criticism characteristic of SAD. Introducing explicit training in self-compassion into treatments for SAD may improve treatment outcome (Allen & Leary, 2010).
There are many techniques that show promise in helping to increase self-compassion in SAD. Mindfulness-based therapeutic techniques and interventions which emphasize the qualities of mindfulness are certainly relevant (Hayes, Strosahl, & Wilson, 1999; Linehan, 1993; Segal, Williams, & Teasdale, 2002), as they typically include an explicit focus on accepting the self and one’s difficult emotions in a non-judgmental and compassionate manner. However, a recent study demonstrated that self-compassion accounts for more of the variance in psychological distress than mindfulness – indicating that it may be the self-compassionate component of mindfulness-based treatments that are particularly important (Van Dam, et al., 2011). One type of meditation, loving-kindness meditation, may directly foster self-compassion (Ringu Tilku Rinpoche & Mullen, 2005). Adaptations of mindfulness-based therapeutic techniques have shown a decrease in negative symptoms associated with SAD and an improvement in overall quality of life (Dalrymple & Herbert, 2007; Kocovski, Fleming, & Rector, 2009; Ossman, Wilson, Storaasli, & McNeill, 2006). Mindfulness-based stress reduction (MBSR; Kabat-Zinn, 1990) has been shown to reduce anxiety and depression symptoms and increase self-esteem in persons with SAD (Goldin & Gross, 2010), although in the only direct comparison to date, it was somewhat less efficacious than cognitive behavior therapy (Goldin & Gross, 2010; Koszycki, Benger, Shlik, & Bradwejn, 2007). This may be due to the fact that self-compassion is not explicitly a focus, but rather a part of the attitudes that support and embrace MBSR and mindfulness-based practices.
Gilbert and colleagues have developed a compassion-based treatment for habitually self-critical individuals called Compassionate Mind Training (CMT; Gilbert & Irons, 2005). CMT trains participants in mindfulness, other-compassion, and self-compassion. Although research on the effectiveness of the approach is still in its early stages, initial results suggest that CMT significantly reduces self-hatred and associated feelings of anxiety and depression (Gilbert & Proctor, 2005).
It is likely that self-compassion is part of the larger etiological underpinnings of SAD. Existing therapies such as CBT may consider combining traditional techniques with important aspects of self-compassion. First, self-kindness – the sense of self-warmth in the face of personal failings – is lacking in SAD. Helping persons recognize that they have another option in the face of social failure and rejection – an option to comfort rather than berate themselves—may be helpful in SAD treatment. Secondly, the sense of common humanity central to self-compassion involves recognizing that all humans make mistakes and engage in unhealthy behaviors. Fostering self-compassion in this domain would have one connect one’s own imperfections to the shared human condition, so that features of the self are considered from a broad, inclusive perspective. Focusing on the interconnected aspects of experience may lessen self-evaluative concerns in SAD because it tends to satisfy the need for belonging that often drives them (M. R. Leary, 1999; Nathanson, 1987). Lastly, practicing mindfulness as anxiety arises would help a person with SAD maintain a distanced perspective on negative emotions. This would help the person to engage with, rather than avoid, emotion eliciting situations and should ultimately lessen the intensity of anxious feelings when they arise.
Limitations and Future Directions
The current study is the first to examine self-compassion in persons with SAD. Gaining an understanding of the six facets of self-compassion in SAD enhances our understanding of diminished adaptive functioning in SAD. We chose to use the SCS because, to date, it is the only widely used measure of self-compassion in the literature. Future research could study self-compassion with more objective behavioral measures in addition to the SCS.
It will also be important to examine self-compassion in other disorders, such as major depression or other anxiety disorders. In this way, one might investigate the role of self-compassion in the cause or maintenance of these disorders, as well as their treatment, and whether any of the findings reported herein are specific to SAD.
Furthermore, it will be important to examine the link between self-compassion, social anxiety, and fear of evaluation prospectively rather than cross-sectionally, as was done in the present study. It will be important to determine if changes in self-compassion are associated with changes in social anxiety, fear of evaluation, and quality of life over time. Researchers could look at momentary variation in self-compassion as well as temporal trends.
Our findings regarding the relationship of age and self-compassion in SAD and HC samples are also limited to aging through the middle years (21–55). Future longitudinal studies on self-compassion, age and SAD could more thoroughly determine how these change across the life-span.
Finally, further research is needed to determine if interventions explicitly emphasizing self-compassion could help individuals to foster healthy relationships (with self and other) and thereby assist in the reduction of symptoms and increase well-being.
Acknowledgments
This research was supported by NIMH Grant MH76074 to James Gross. The authors of this manuscript do not have any direct or indirect conflicts of interest, financial or personal relationships or affiliations to disclose.
References
- Acarturk C, de Graaf R, van Straten A, Have MT, Cuijpers P. Social phobia and number of social fears, and their association with comorbidity, health-related quality of life and help seeking: a population-based study. Social Psychiatry Psychiatric Epidemiology. 2008;43:273–279. doi: 10.1007/s00127-008-0309-1. [DOI] [PubMed] [Google Scholar]
- Adams CE, Leary MR. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. Journal of Social and Clinical Psychology. 2007;26:1120–1144. [Google Scholar]
- Allen A, Leary M. Self-compassion, stress and coping. Social and Personality Psychology Compass. 2010;4(2):107–118. doi: 10.1111/j.1751-9004.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Assoication; 1994. [Google Scholar]
- Baker SL, Heinrich N, Kim H-J, Hoffman SG. The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40:1087–1098. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Blatt SJ. A cognitive morphology of psychopathology. Journal of Nervous and Mental Disease. 1991;179:449–458. doi: 10.1097/00005053-199108000-00001. [DOI] [PubMed] [Google Scholar]
- Brown EJ, Turovsky J, Heimberg RG, Juster HR, Brown TA, Barlow DH. Validation of the Social Interaction Anxiety Scale and the Social Phobia Scale across the anxiety disorders. Psychological Assessment. 1997;9:21–27. [Google Scholar]
- Brozovich F, Heimberg RG. An analysis of post-event processing in social anxiety disorder. Clinical Psychology Review. 2008;28:891–903. doi: 10.1016/j.cpr.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG, Bechara A, Tranel D, Hawkley LC. Could an aging brain contribute to subjective well being?: The value added by a social neuroscience perspective. In: Tadorov A, Fiske ST, Prentice D, editors. Social Neuroscience: Toward Understanding the Underpinnings of the Social Mind. New York: Oxford University Press; (in press). [Google Scholar]
- Cairney J, McCabe L, Veldhuizen S, Corna LM, Streiner D, Herrmann N. Epidemiology of social phobia in later life. American Journal of Geriatric Psychiatry. 2007;15:224–233. doi: 10.1097/01.JGP.0000235702.77245.46. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Collimore KC, Asmundson GJG. Social anxiety and fear of negative evaluation: construct validity of the BFNE-II. Journal of anxiety. 2007;2:131–141. doi: 10.1016/j.janxdis.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social phobia: Diagnosis, assessment, and treatment. New York: Guilford Press; 1995. pp. 69–93. [Google Scholar]
- Coles ME, Gibb BE, Heimberg RG. Psychometric evaluation of the Beck Depression Inventory in adults with social anxiety disorder. Depression and Anxiety. 2001;14:145–148. doi: 10.1002/da.1057. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Fleet C, Stein MB. Self-criticism and social phobia in the US National Comorbidity Survey. Journal of Affective Disorders. 2004;82:227–234. doi: 10.1016/j.jad.2003.12.012. [DOI] [PubMed] [Google Scholar]
- Dalrymple KL, Herbert JD. Acceptance and Commitment Therapy for Generalized Social Anxiety Disorder: A pilot study. Behavior Modification. 2007;31:543–568. doi: 10.1177/0145445507302037. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Hughes DL, George LK, Blazer DG. The epidemiology of social phobia: Findings from the Duke Epidemiological Catchment Area Study. Psychological Medicine. 1993;(23):709–718. doi: 10.1017/s0033291700025484. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Dweck CS. Motivational processes affecting learning. American Psychologist. 1986;41:1040–1048. [Google Scholar]
- Fergus TA, Valentiner DP, McGrath PB, Stephenson K, Gier S, Jencius S. The Fear of Positive Evaluation Scale: Psychometric properties in a clinical sample. Journal of Anxiety Disorders. 2009;23:1177–1183. doi: 10.1016/j.janxdis.2009.07.024. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, et al. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Proctor S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2005;13(6):353–379. [Google Scholar]
- Gilboa-Schechtman E, Franklin ME, Foa EB. Anticipated reactions to social events: Differences among individuals with generalized social phobia, obsessive compulsive disorder and nonanxious controls. Cognitive Therapy and Research. 2000;24:731–747. [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gros DF, Antony MM, Simms LJ, McCabe RE. Psychometric properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): comparison to the State-Trait Anxiety Inventory (STAI) Psychological Assessment. 2007;19:369–381. doi: 10.1037/1040-3590.19.4.369. [DOI] [PubMed] [Google Scholar]
- Hackmann A, Surawy C, Clark DM. Seeing yourself through others’ eyes: A study of spontaneously occurring images in social phobia. Behavioural and Cognitive Psychotherapy. 1998;26:3–12. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson K. Acceptance and commitment therapy: An experiential approach to behavior change. New York: The Guilford Press; 1999. [Google Scholar]
- Heimberg RG, Brozovich FA, Rapee RM. A cognitive-behavioral model of social anxiety disorder: Update and extension. In: Hofmann SG, DiBartolo PM, editors. Social anxiety: Clinical, developmental, and social perspectives. New York: Academic Press; 2010. [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, Liebowitz MR. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine. 1999;29:199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Mueller GP, Holt CS, Hope DA, Liebowitz MR. Assessment of anxiety in social interaction and being observed by others: The Social Interaction Anxiety Scale and the Social Phobia Scale. Behavior Therapy. 1992;23:53–73. [Google Scholar]
- Hirsch CR, Matthews A. Impaired positive inferential bias in social phobia. Behaviour Research and Therapy. 2000;109:705–712. doi: 10.1037//0021-843x.109.4.705. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive Factors that Maintain Social Anxiety Disorder: a Comprehensive Model and its Treatment Implications. Cognitive Behaviour Therapy. 2007;36:195–209. doi: 10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huppert JD, Foa EB, Furr JM, Filip JC, Mathews A. Interpretation bias in social anxiety: A dimensional perspective. Cognitive Therapy and Research. 2003;27:569–577. [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York: Delacorte; 1990. [Google Scholar]
- Kashdan TB. Social anxiety spectrum and diminished positive experiences: Theoretical synthesis and meta-analysis. Clinical Psychology Review. 2007;27:348–365. doi: 10.1016/j.cpr.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PD, Demler O, Olga JR, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Rector NA. Mindfulness and Acceptance-Based Group Therapy for Social Anxiety Disorder: An Open Trial. Cognitive and Behavioral Practice. 2009;16:276–289. [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Leary MR. Making sense of self-esteem. Current Directions in Psychological Science. 1999;8:32–353. [Google Scholar]
- Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant Events: The implications of treating oneself kindly. Journal of Personality and Social Psychology. 2007;92:887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems in Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatmetn of borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- Lovibond PF, Rapee RM. The representation of feared outcomes. Behaviour Research and Therapy. 1993;(31):595–608. doi: 10.1016/0005-7967(93)90111-7. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Nathanson D, editor. The many faces of shame. New York: Guilford Press; 1987. [Google Scholar]
- Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003a;2:85–102. [Google Scholar]
- Neff KD. The Development and Validation of a Scale to Measure Self-Compassion. Self and Identity. 2003b;2:223–250. [Google Scholar]
- Neff KD, Hseih Y, Dejitthirat K. Self-compassion, achievement goals, and coping with academic failure. Self and Identity. 2005;4:263–287. [Google Scholar]
- Neff KD, Rude SS, Kirkpatrick K. An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality. 2007;41:908–916. [Google Scholar]
- Novak DL, Mather M. Aging and Variety Seeking. Psychology and Aging. 2007;22:728–737. doi: 10.1037/0882-7974.22.4.728. [DOI] [PubMed] [Google Scholar]
- Ossman WA, Wilson KG, Storaasli RD, McNeill JW. A preliminary investigation of the use of Acceptance and Commitment Therapy in group treatment for Social Phobia. International Journal of Psychology and Psychological Therapy. 2006;6:397–416. [Google Scholar]
- Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences. 2010;48:757–761. [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997a;35(8):741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997b;35:741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Rasmussen MK, Pidgeon AM. The direct and indirect benefits of dispositional mindfulness on self-esteem and social anxiety. Anxiety, Stress & Coping. doi: 10.1080/10615806.2010.515681. (in press). First published on: 22 September 2010 (iFirst). [DOI] [PubMed] [Google Scholar]
- Ries BJ, McNeil DW, Boone ML, Turk CL, Carter LE, Heimberg RG. Assessment of contemporary social phobia verbal report instruments. Behaviour Research and Therapy. 1998;36:983–994. doi: 10.1016/s0005-7967(98)00078-3. [DOI] [PubMed] [Google Scholar]
- Ringu Tilku Rinpoche, Mullen K. The Buddhist use of compassionate imagery in Buddhist mediation. In: Gilbert P, editor. Compassion: Conceptualisations, Research and Use in Psychotherapy. London: Brunner-Routledge; 2005. pp. 218–238. [Google Scholar]
- Rodebaugh TL, Woods CM, Thissen DM, Heimberg RG, Chambless DL, Rapee RM. More information from fewer questions: The factor structure and item properties of the original and Brief Fear of Negative Evaluation Scale. Psychological Assessment. 2004;16:169–181. doi: 10.1037/1040-3590.16.2.169. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowtitz MR, Cissell S, et al. Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. Depression and Anxiety. 2009;26:34–38. doi: 10.1002/da.20503. [DOI] [PubMed] [Google Scholar]
- Samanez-Larkin GR, Carstensen LL. Socioemotional functioning and the aging brain. In: Decety J, Cacioppo JT, editors. The Handbook of Social Neuroscience. New York: Oxford University Press; (in press). [Google Scholar]
- Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, et al. Functional impairment in social phobia. Journal of Clinical Psychiatry. 1994;55:322–331. [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale J. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- Spielberger CD, Gorsuch R, Lushene RE. The State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Psychologists Press; 1970. [Google Scholar]
- Tolman RM, Himle J, Bybee D, Abelson JL, Hoffman J, Van Etten-Lee M. Impact of Social Anxiety Disorder on Employment Among Women Receiving Welfare Benefits. Psychiatric Services. 2009;60:61–66. doi: 10.1176/ps.2009.60.1.61. [DOI] [PubMed] [Google Scholar]
- Urry HL, Gross JJ. Emotion regulation in older age. Current Directions in Psychological Science. 2010;19:352–357. [Google Scholar]
- Van Dam NT, Sheppard SC, Forsyth JP, Earleywine M. Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. Journal of Anxiety Disorders. 2011;25:123–130. doi: 10.1016/j.janxdis.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Fresco DM, Hart TA, Turk CL, Schneier FR, et al. Empirical validation and psychometric evaluation of the Brief Fear of Negative Evaluation Scale in clients with social anxiety disorder. Psychological Assessment. 2005;17:179–190. doi: 10.1037/1040-3590.17.2.179. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Rodebaugh TL. The Fear of Positive Evaluation Scale: Assessing a proposed cognitive component of social anxiety. Journal of Anxiety Disorders. 2008;22:44–55. doi: 10.1016/j.janxdis.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Heimberg RG, Rodebaugh TL, Norton PJ. Exploring the relationship between fear of positive evaluation and social anxiety. Journal of Anxiety Disorders. 2008;22:386–400. doi: 10.1016/j.janxdis.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Wells A, Papageorgiou C. The observer perspective: biased imagery in social phobia, agoraphobia, and blood/injury phobia. Behaviour Research and Therapy. 1999;37:653–658. doi: 10.1016/s0005-7967(98)00150-8. [DOI] [PubMed] [Google Scholar]
- Witchen HU, Beloch E. The impact of social phobia on quality of life. International Clinical Psychopharmacology. 1996;(11):15–23. doi: 10.1097/00004850-199606003-00004. [DOI] [PubMed] [Google Scholar]