Abstract
A number of case-control studies have been conducted to clarify the association between ApoE polymorphisms and myocardial infarction (MI); however, the results are inconsistent. This meta-analysis was performed to clarify this issue using all the available evidence. Searching in PubMed retrieved all eligible articles. A total of 33 studies were included in this meta-analysis, including 18752 MI cases and 18963 controls. The pooled analysis based on all included studies showed that the MI patients had a decreased frequency of the ε2 allele (OR = 0.78, 95% CI = 0.70–0.87) and an increased frequency of the ε4 allele (OR = 1.15, 95% CI = 1.10–1.20); The results also showed a decreased susceptibility of MI in the ε2ε3 vs. ε3ε3 analysis (OR = 0.79, 95% CI = 0.68–0.90) and in the ε2 vs. ε3 analysis (OR = 0.78, 95% CI = 0.69–0.89), an increased susceptibility of MI in the ε3ε4 vs. ε3ε3 analysis (OR = 1.26, 95% CI = 1.12–1.41), in the ε4 vs. ε3 analysis (OR = 1.22, 95% CI = 1.12–1.32) and in the ε4ε4 vs. ε3ε3 analysis (OR = 1.59, 95% CI = 1.15–2.19). However, there were no significant associations among polymorphisms and MI for the following genetic models: frequency of the ε3 allele (OR = 0.99, 95% CI = 0.96–1.02); ε2ε2 vs. ε3ε3 analysis (OR = 0.73, 95% CI = 0.40–1.32); or ε2ε4 vs. ε3ε3 analysis (OR = 1.10, 95% CI = 0.99–1.21). Our results suggested that the ε4 allele of ApoE is a risk factor for the development of MI and the ε2 allele of ApoE is a protective factor in the development of MI.
Introduction
Myocardial infarction (MI) is a leading cause of death worldwide, and is a multifactorial disease, influenced by genetic and environmental factors [1]. The main risk factors for MI include hypertension, hypercholesterolemia, diabetes, obesity, and smoking. In addition, recent studies have also shown the importance of genetic factors caused by polymorphisms in the pathogenesis of MI [2]–[7].
Apolipoprotein E (Apo E) is a serum glycoprotein found in circulating chylomicrons (remnants), very low density lipoproteins, intermediate density lipoproteins and high-density lipoproteins [8]. ApoE is considered as an excellent candidate gene for studying the susceptibility to coronary heart disease (CHD) and MI because of its pivotal roles in the metabolisms of cholesterol and triglyceride [9]. The most extensively studied polymorphism in the ApoE gene codes for three variant alleles: ε2, ε3 and ε4, which yield six possible genotypes: ε2/ε2, ε2/ε3, ε2/ε4, ε3/ε3, ε3/ε4 and ε4/ε4 in general population [10]. The products of the three alleles differ in their properties such as their affinity for binding low density lipoprotein receptors and lipoprotein particles; therefore, this ApoE polymorphism could affect the serum levels of cholesterol and triglyceride, thus contributing to the progression of atherosclerosis. In fact, ApoE polymorphisms have been found to be associated with many lipid-related diseases and cardiovascular and cerebrovascular diseases [11]–[14].
Numerous studies have been conducted to explore the association of this ApoE polymorphism and CHD; some of the studies found a significant association between the ApoE ε4 allele and CHD [15]–[17]. A meta-analysis conducted in 2004 provided evidence that the ε4 allele of ApoE was a risk factor for the development of CHD [18]. Another meta- analysis conducted in 2013 further confirmed this finding in a Chinese population [19]. However, no meta-analysis has been conducted to explore the association between this ApoE gene polymorphism and MI. In spite of the presence of advanced CHD, only a subset of patients develops MI during their life. The reasons for these individual differences in susceptibility to MI are poorly understood. Therefore, it is important to explore the association between ApoE gene polymorphisms and MI. In fact, a number of case-control studies have been conducted to clarify the association between ApoE gene polymorphisms and MI [20]–[52]; however, the results are inconsistent. Therefore, we conducted this meta-analysis including all of the evidence produced to date to explore this issue.
Materials and Methods
Search strategy
We searched all published studies in the Pubmed database (up to January 20, 2014) using the following combination of keywords: “Apolipoprotein E” OR “ApoE” AND “acute coronary syndrome” OR “myocardial infarction” AND “polymorphism” OR “polymorphisms” OR “variants” OR “variant”. In addition, manual searches for related articles were also performed to avoid missing any relevant studies.
Inclusion and exclusion criteria
The inclusion criteria for identified articles were as follows: 1) Case-control studies with full text articles on the relationship of ApoE polymorphisms and MI; 2) sufficient data for estimating an odds ratio (OR) with 95% confidence interval (CI). Those not designed as case-control studies, systemic reviews, those not written in English or Chinese, and those that provided no usable data, were excluded.
Data extraction
Two authors independently extracted the data from all included studies using a predesigned data extraction table. The following information was extracted from each included article: first author, year of publication, ethnicity and country, source of controls, total numbers of MI cases and controls, distribution of genotypes and alleles in MI cases and controls, and evidence of conforming to the Hardy-Weinberg equilibrium (HWE).
Statistical analysis
We firstly used chi-squared (χ2) test and and I2 statistic to assess heterogeneity across studies. A fixed effect model (Mantel–Haenszel) was used in the absence of heterogeneity. Otherwise, the random effect model (DerSimonian–Laird) was adopted. The strength of the association between the ApoE gene polymorphism and MI was assessed by odds ratios (ORs) with the corresponding 95% CI for each study. The ORs and their 95% CIs were assessed for the following seven genetic models: 1) ε2ε2 vs. ε3ε3; 2) ε2ε3 vs. ε3ε3; 3) ε2ε4 vs. ε3ε3; 4) ε3ε4 vs. ε3ε3; 5) ε4ε4 vs. ε3ε3; 6) ε2 vs. ε3; 7) ε4 vs. ε3. The allele frequencies of ε2, ε3 and ε4 were also assessed using the same method. Cumulative meta-analysis was also performed for the above genetic models. Subgroup analysis for ethnicity (Asian and Caucasian) was also performed. To find potential outliers, influence analysis was performed by omitting each study in turn. A funnel plot, calculated using Begg’s and Egger’s tests, was adopted for assessing potential publication bias. Statistical analysis was conducted using STATA statistical software (version 11; StataCorp, College Station, Texas, USA). A P value less than 0.05 was considered statistically significant.
Results
Literature selection and study characteristics
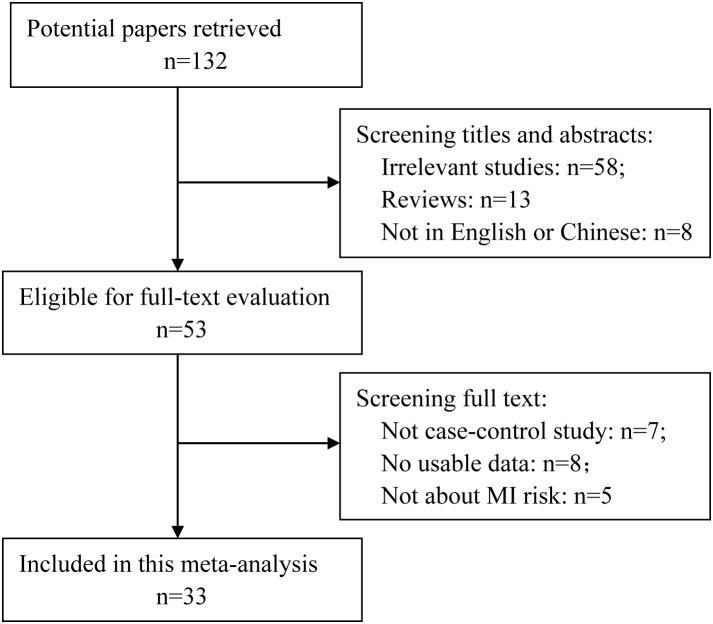
One hundred and thirty two articles were retrieved from PubMed, 79 of which were excluded after screening the titles and abstracts (58 were irrelevant studies, 13 were reviews and eight were not published in English or Chinese). Fifty-three articles were selected for detailed assessment, which excluded a further 20 articles (seven were not case-control studies, eight had no usable data (no case and control numbers according to the genotypes) and five were not about MI). Finally, 33 studies were included in this meta-analysis, which included 18752 MI cases and 18963 controls. The detailed selection procedure is shown in Figure 1 . There were three studies did not follow the HWE. The detailed characteristics of the included studies are shown in Table 1 . The present study met the PRISMA statement requirements ( Checklist S1 and Figure 1 ).
Figure 1. Flowchart of the study selection.
Table 1. Detailed characteristics of studies included in this meta-analysis.
| Genotypes distribution (Cases/controls) | |||||||||||||||
| Study [Reference] | Year | Country | Ethnicity | Study | HWE | Total sample | ε2/ε2 | ε2/ε3 | ε3/ε3 | ε2/ε4 | ε3/ε4 | ε4/ε4 | ε2 | ε3 | ε4 |
| type | Case/Control | ||||||||||||||
| Utermann1984[20] | 1984 | Germany | Caucasion | HCC | Yes | 523/1031 | 7/120 | x68/124 | 333/617 | 11/15 | 92/236 | 12/29 | 86/359 | 493/977 | 115/280 |
| Cumming1984[21] | 1984 | Scotland | Caucasion | PCC | Yes | 239/400 | 0/2 | 18/51 | 128/233 | 10/11 | 77/99 | 6/4 | 28/64 | 223/383 | 93/114 |
| Lenzen1986[22] | 1986 | France | Caucasion | PCC | Yes | 570/624 | 1/6 | 50/67 | 360/393 | 10/20 | 137/125 | 12/13 | 61/93 | 547/585 | 159/158 |
| Eichner 1993[23] | 1993 | USA | Caucasion | PCC | Yes | 114/412 | 0/2 | 16/35 | 67/276 | 0/4 | 30/85 | 1/10 | 16/41 | 113/396 | 31/99 |
| Luc 1994[24] | 1994 | France | Caucasion | PCC | Yes | 574/680 | 3/6 | 54/92 | 352/428 | 14/14 | 133/126 | 18/14 | 71/112 | 539/646 | 165/154 |
| Hergenc 1995'[25] | 1995 | Turkey | Caucasion | HCC | Yes | 50/60 | 0/0 | 7/6 | 41/47 | 0/2 | 2/5 | 0/0 | 7/8 | 50/58 | 2/7 |
| Kim 1995[26] | 1995 | Korea | Asian | HCC | Yes | 97/137 | 2/1 | 17/25 | 57/95 | 0/4 | 20/12 | 1/0 | 19/30 | 94/132 | 21/16 |
| Nakai 1998[27] | 1998 | Japan | Asian | PCC | Yes | 254/422 | 0/0 | 10/16 | 178/327 | 2/4 | 52/74 | 6/1 | 12/20 | 240/417 | 60/79 |
| Scaglione1999[28] | 1999 | Italy | Caucasion | HCC | No | 98/98 | NR | NR | NR | NR | NR | NR | 3/3 | 84/87 | 11/8 |
| Lambert 2000[29] | 2000 | France | Caucasion | PCC | Yes | 567/678 | 3/4 | 67/100 | 332/420 | 0/3 | 152/138 | 18/13 | 70/107 | 551/658 | 170/154 |
| Benes2000[30] | 2000 | Czech | Caucasion | PCC | Yes | 114/222 | 1/0 | 12/30 | 71/147 | 3/2 | 23/43 | 4/0 | 16/32 | 106/220 | 30/45 |
| Batalla 2000[31] | 2000 | Spain | Caucasion | PCC | Yes | 220/200 | 0/0 | 9/18 | 174/151 | 1/1 | 32/28 | 4/2 | 10/19 | 215/197 | 37/31 |
| Raslová 2001[32] | 2001 | Canada | Caucasion | PCC | Yes | 69/69 | 2/1 | 8/5 | 46/47 | 1/0 | 11/15 | 1/1 | 11/6 | 65/67 | 13/16 |
| Bai 2001[33] | 2001 | China | Asian | PCC | Yes | 47/50 | 0/0 | 4/5 | 40/39 | 0/0 | 6/3 | 0/0 | 4/5 | 50/47 | 6/3 |
| Freitas 2002[34] | 2002 | Australia | Caucasion | PCC | Yes | 411/624 | 3/4 | 24/67 | 254/372 | 9/15 | 111/147 | 10/19 | 36/86 | 389/586 | 130/181 |
| Mamotte 2002[35] | 2002 | Australia | Caucasion | PCC | Yes | 359/639 | 4/4 | 24/68 | 217/383 | 7/16 | 96/149 | 11/19 | 35/88 | 337/600 | 114/184 |
| Kolovou 2002[36] | 2002 | Greece | Caucasion | PCC | Yes | 124/240 | 0/0 | 3/34 | 94/159 | 0/5 | 27/40 | 0/2 | 3/39 | 124/233 | 27/47 |
| Keavney 2003[37] | 2003 | UK | Caucasion | PCC | Yes | 4487/5757 | NR | 440/686 | 2566/3384 | NR | 1206/1376 | NR | 440/686 | 4212/5446 | 1206/1376 |
| Kolovou 2003[38] | 2003 | Greece | Caucasion | PCC | Yes | 165/165 | 0/0 | 3/16 | 129/118 | 1/4 | 29/23 | 1/0 | 4/20 | 161/157 | 31/27 |
| Kumar 2003[39] | 2003 | India | Caucasion | PCC | Yes | 35/45 | 0/2 | 6/9 | 12/32 | 1/0 | 6/0 | 10/2 | 7/9 | 24/41 | 17/2 |
| Marques 2003[40] | 2003 | France | Caucasion | HCC | Yes | 400/338 | NR | NR | 272/228 | NR | NR | NR | 37/40 | 272/228 | 91/70 |
| Keavney 2004[41] | 2004 | UK | Caucasion | PCC | Yes | 4685/3460 | NR | 440/406 | 2566/1949 | 1206/810 | NR | NR | 1646/1216 | 3006/2355 | 1206/810 |
| Ranjith 2004[42] | 2004 | South Africa | Caucasion | PCC | Yes | 195/300 | 0/3 | 7/18 | 139/228 | 3/3 | 45/43 | 1/5 | 10/24 | 191/289 | 49/51 |
| Baum 2006[43] | 2006 | China | Asian | PCC | Yes | 231/331 | 0/2 | 13/60 | 164/203 | 4/6 | 46/39 | 4/1 | 17/68 | 223/302 | 54/46 |
| Aasvee 2006[44] | 2006 | Estonia | Caucasion | PCC | Yes | 71/85 | 1/1 | 4/13 | 45/52 | 2/3 | 16/16 | 3/0 | 7/17 | 65/81 | 21/19 |
| Koch 2008[45] | 2008 | Germany | Caucasion | PCC | Yes | 3657/1211 | 26/7 | 402/164 | 2279/736 | 63/23 | 809/263 | 78/18 | 491/194 | 3490/1163 | 950/304 |
| Kolovou 2009[46] | 2009 | Greece | Caucasion | PCC | Yes | 124/240 | NR | NR | NR | NR | NR | NR | 5/19 | 106/197 | 13/24 |
| Bahri 2008[47] | 2008 | Tunisia | Caucasion | PCC | Yes | 80/100 | 0/0 | 6/8 | 61/78 | 0/1 | 13/13 | 0/0 | 6/9 | 80/199 | 13/14 |
| Martinelli 2009[48] | 2009 | Italy | Caucasion | HCC | Yes | 394/287 | NR | NR | NR | NR | NR | NR | 34/25 | 285/220 | 76/42 |
| Al-Bustan 2009[49] | 2009 | Kuwaiti | Caucasion | HCC | No | 88/122 | 4/9 | 2/2 | 72/98 | 2/3 | 8/9 | 0/1 | 6/11 | 90/33 | 16/5 |
| Onrat 2012[50] | 2012 | Turkey | Caucasion | PCC | Yes | 36/100 | 0/0 | 12/4 | 72/27 | 0/0 | 16/4 | 0/1 | 12/4 | 100/35 | 16/5 |
| Tanguturi 2013[51] | 2013 | USA | Caucasion | HCC | Yes | 202/210 | 0/0 | 8/14 | 142/167 | 4/3 | 37/23 | 11/3 | 12/17 | 187/204 | 52/29 |
| Zende 2013[52] | 2013 | India | Caucasion | HCC | No | 150/150 | 6/7 | 13/16 | 59/85 | 7/4 | 22/14 | 43/24 | 26/27 | 94/115 | 72/42 |
HWE, Hardy-Weinberg equilibrium; NR, not reported; Cases, MI patients; HCC, hospital based case-control study; PCC, population based case-control study.
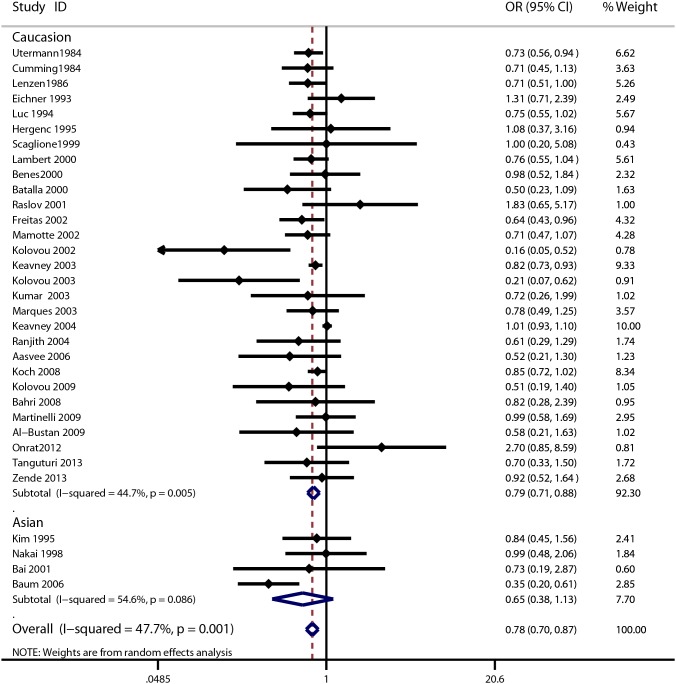
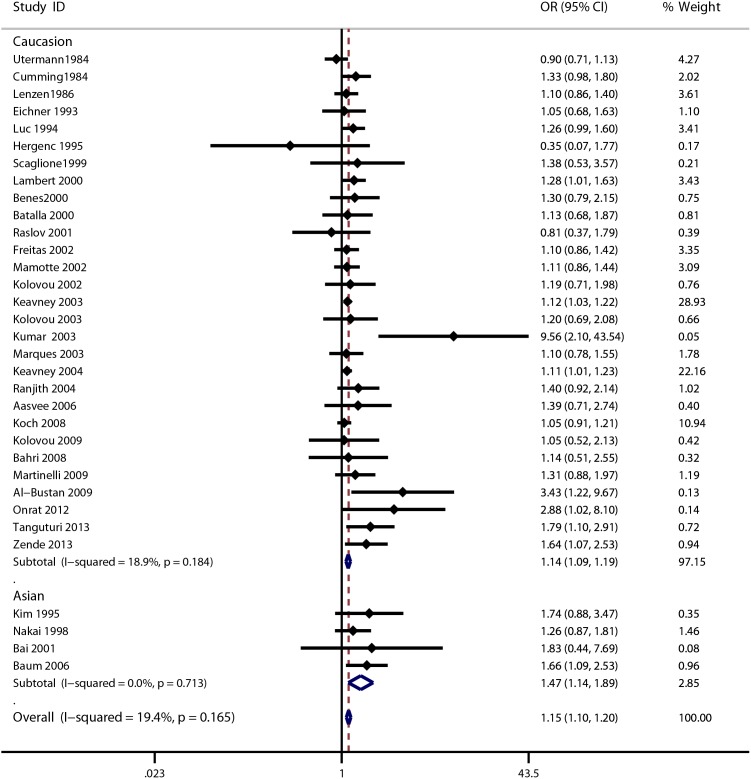
Quantitative data synthesis
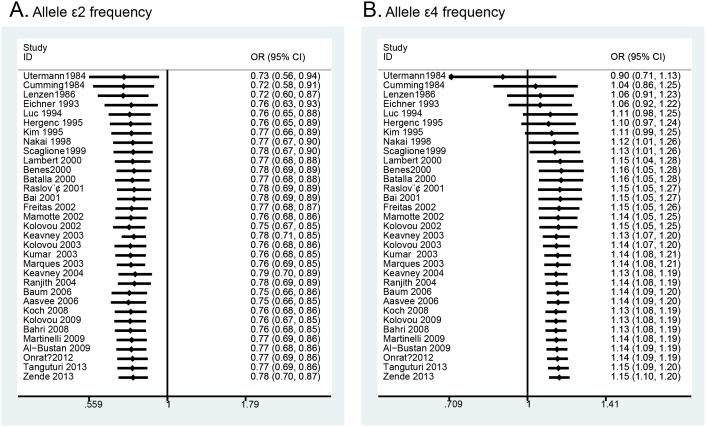
The meta-analysis of the included studies showed that there was significant association between the ApoE gene polymorphism and MI. The results showed that the MI patients had a decreased frequency of the ε2 allele (OR = 0.78, 95% CI = 0.70–0.87, Figure 2 ) and an increased frequency of the ε4 allele (OR = 1.15, 95% CI = 1.10–1.20, Figure 3 ). The results also showed a decreased susceptibility of MI in the ε2ε3 vs. ε3ε3 analysis (OR = 0.79, 95% CI = 0.68–0.90, Figure S1), and in the ε2 vs. ε3 analysis (OR = 0.78, 95% CI = 0.69–0.89, Figure S4), and an increased susceptibility of MI in the ε3ε4 vs. ε3ε3 analysis (OR = 1.26, 95% CI = 1.12–1.41, Figure S2) in the ε4ε4 vs. ε3ε3 analysis (OR = 1.59, 95% CI = 1.15–2.19, Figure S3) and in the ε4 vs. ε3 analysis (OR = 1.22, 95% CI = 1.12–1.32, Figure S5). However, there were no significant associations among polymorphisms and MI for the following genetic models: frequency of ε3 allele (OR = 0.99, 95% CI = 0.96–1.02); ε2ε2 vs. ε3ε3 analysis (OR = 0.73, 95% CI = 0.40–1.32); ε2ε4 vs. ε3ε3 analysis (OR = 1.10, 95% CI = 0.99–1.21). The detailed results are shown in Table 2 . Cumulative analysis further confirmed the results ( Figure 4 and Figure S6).
Figure 2. Forest plot for ApoE gene polymorphism and MI risk in the ε2 allele frequency analysis.
Figure 3. Forest plot for ApoE gene polymorphism and MI risk in the ε4 allele frequency analysis.
Table 2. Results of meta-analysis of ApoE polymorphism and MI.
| Overall | Caucasion | Asian | ||||
| Analysis | OR (95% CI) | P/Phet | OR (95% CI) | P/Phet | OR (95% CI) | P/Phet |
| ε2ε2 vs. ε3ε3 | 0.73 (0.40–1.32) | 0.29/0.005 | 0.70 (0.38–1.31) | 0.27/0.004 | 1.07 (0.08–13.78) | 0.96/0.18 |
| ε2ε3 vs. ε3ε3 | 0.79 (0.68–0.90) | 0.001/0.001 | 0.80 (0.70–0.92) | 0.001/0.008 | 0.70 (0.31–1.60) | 0.84/0.007 |
| ε2ε4 vs. ε3ε3 | 1.10 (0.99–1.21) | 0.07/0.70 | 1.10 (1.00–1.21) | 0.05/0.63 | 0.66 (0.26–1.70) | 0.39/0.61 |
| ε3ε4 vs. ε3ε3 | 1.26 (1.12–1.41) | <0.001/0.001 | 1.23 (1.09–1.38) | 0.001/0.001 | 1.51 (1.14–2.00) | 0.004/0.39 |
| ε4ε4 vs. ε3ε3 | 1.59 (1.15–2.19) | 0.005/0.04 | 1.47 (1.07–2.02) | 0.02/0.05 | 6.95 (1.75–27.65) | 0.006/0.85 |
| ε2 vs. ε3 | 0.78 (0.69–0.89) | <0.001/0.04 | 0.80 (0.71–0.90) | <0.001/0.04 | 0.67 (0.37–1.23) | 0.20/0.22 |
| ε4 vs. ε3 | 1.22 (1.12–1.32) | <0.001/0.02 | 1.20 (1.10–1.30) | <0.001/0.02 | 1.49 (1.15–1.93) | 0.002/<0.001 |
| ε2 allele frequency | 0.78 (0.70–0.87) | <0.001/0.001 | 0.79 (0.71–0.88) | <0.001/0.005 | 0.65 (0.38–1.13) | 0.13/0.09 |
| ε3 allele frequency | 0.99 (0.96–1.02) | 0.38/1.00 | 0.99 (0.96–1.02) | 0.39/1.00 | 0.99 (0.86–1.13) | 0.22/0.94 |
| ε4 allele frequency | 1.15 (1.10–1.20) | 0.001/0.17 | 1.14 (1.09–1.19) | 0.001/0.18 | 1.47 (1.14–1.89) | 0.003/0.70 |
P, p value of the test on the association estimate; Phet, p value of the heterogeneity test.
Figure 4. Cumulative meta-analysis of ApoE gene polymorphism and MI risk: A) ε2 allele frequency analysis; B) ε4 allele frequency analysis.
Tests of heterogeneity and subgroup analysis
Significant between-study heterogeneity existed in the analyses of seven genetic models: ε2 ε2 vs. ε3ε3 (p = 0.005); ε2ε3 vs. ε3ε3 (p = 0.001); ε3ε4 vs. ε3ε3 (p = 0.001); ε4ε4 vs. ε3ε3 (p = 0.04), ε2 vs. ε3 (p = 0.04), ε2 vs. ε3 (p = 0.02) and the ε2 allele frequency (p = 0.001). A random effects model was adopted for these analyses.
Furthermore, we performed subgroup analysis based on ethnicity and found a decreased susceptibility of MI in the ε2ε3 vs. ε3ε3 analysis (OR = 0.80, 95% CI = 0.70–0.92) and ε2 allele frequency (OR = 0.79, 95% CI = 0.71–0.88) among Caucasian populations. We also found an increased susceptibility of MI in the ε3ε4 vs. ε3ε3 analysis (OR = 1.23, 95% CI = 1.09–1.38), ε4ε4 vs. ε3ε3 analysis (OR = 1.47, 95% CI = 1.07–2.02) and the ε4 allele frequency (OR = 1.14, 95% CI = 1.09–1.19) among Caucasian populations. Among Asian populations, we also found an increased susceptibility of MI in the ε3ε4 vs. ε3ε3 analysis, ε4ε4 vs. ε3ε3 analysis and for the ε4 allele frequency; the detailed results are shown in Table 2 .
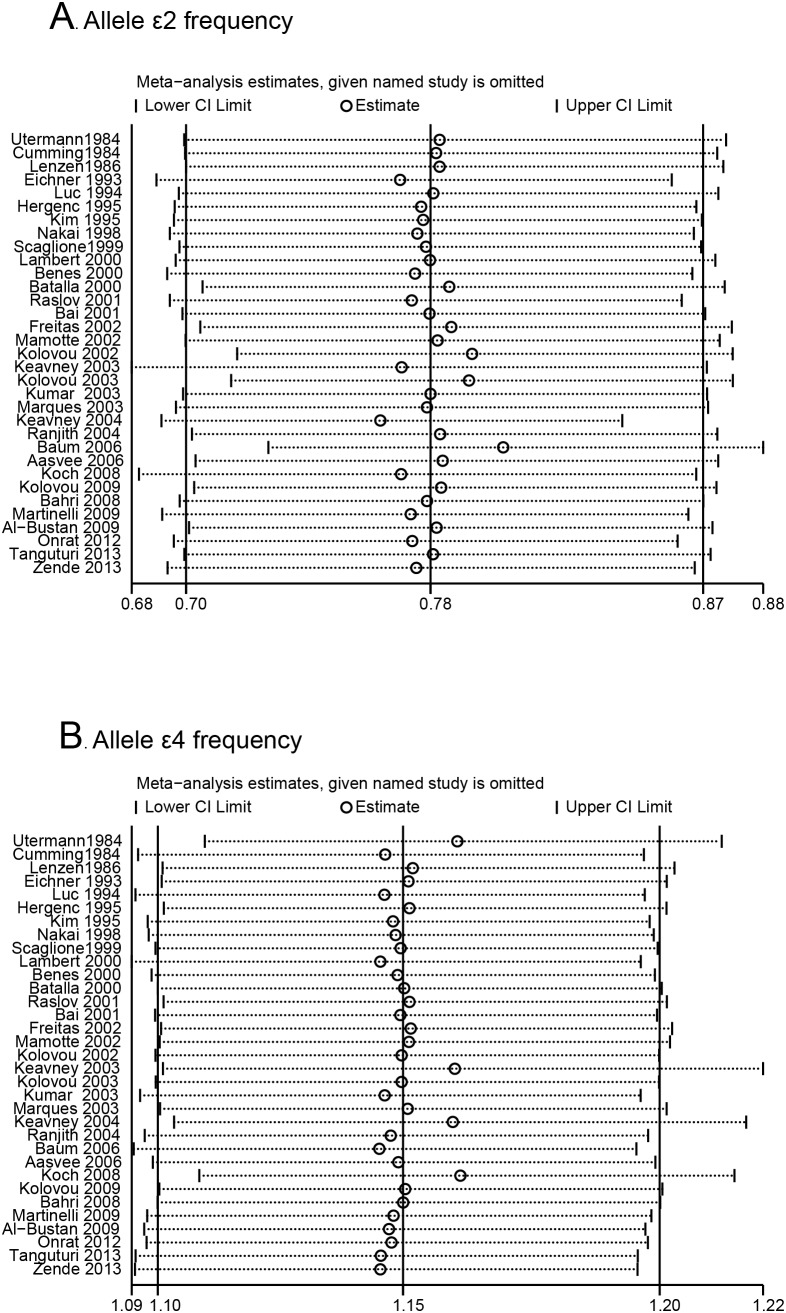
Sensitivity analysis
We conducted influence analysis to assess the sensitivity of each individual study on the pooled ORs by sequential omission of each individual study. The results suggested that no individual study significantly affected the pooled ORs in the ε2 allele and ε4 allele frequency analysis ( Figure 5 ), and in the ε2ε3 vs. ε3ε3 analysis, ε3ε4 vs. ε3ε3 analysis and ε4ε4 vs. ε3ε3 analysis (Figure S7).
Figure 5. Influence analysis of ApoE gene polymorphism and MI risk: A) ε2 allele frequency analysis; B) ε4 allele frequency analysis.
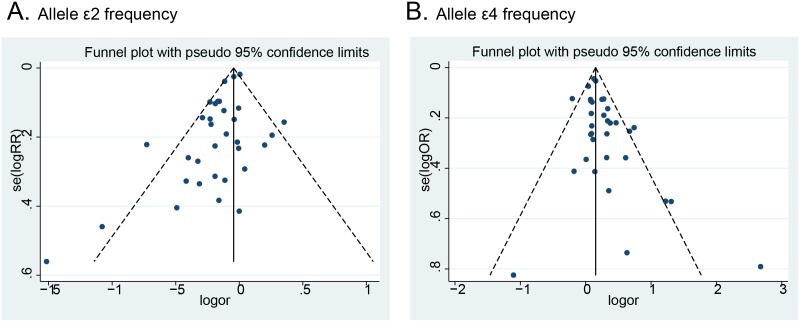
Publication bias
Funnel plots examined potential publication bias qualitatively and no obvious asymmetry was observed in any genetic model, as shown in Figure 6 . Furthermore, the results from Begg’s and Egger’s tests did not provide any evidence of publication bias (Table S1).
Figure 6. Funnel plot of ApoE gene polymorphism and MI risk: A) ε2 allele frequency analysis; B) ε4 allele frequency analysis.
Discussion
To the best of our knowledge, this is the first meta-analysis to evaluate the association between an ApoE polymorphism and susceptibility of MI. In this meta-analysis, we discovered an increased susceptibility of MI in the ε4 allele frequency analysis. Moreover, the individuals with ε2ε4 genotype, ε3ε4 genotype and ε4ε4 genotype had a significantly higher susceptibility of developing MI compared to those with the ε3ε3 genotype. Therefore, it is reasonable to assume that the ε4 allele of ApoE is an risk factor for the development of MI. These results were consistent with a previous meta-analysis, which showed that ε4 allele of ApoE is a risk factor for the development of CHD [11], [12]. In addition, we found a decreased susceptibility of MI in the ε2 allele frequency analysis and in the ε2ε3 vs. ε3ε3 analysis, which indicate that the ε2 allele is a protective factor in the development of MI. Cumulative meta-analysis also confirmed these findings. Considering the large sample size in the pooled analysis in this meta-analysis, we believe that our results are robust and reliable.
ApoE is a multifunctional protein that plays an important role in the metabolism of cholesterol and triglycerides, by binding to its receptors to help mediate clearance of chylomicron and remnant particles [53]. The three common isoforms, ε2, ε3 and ε4, have different receptor-binding abilities and could yield different circulating levels of cholesterol and triglycerides. Compared with ε3 homozygotes, carriers of the ε2 allele have lower circulating cholesterol levels, whereas carriers of the ε4 allele appear to have higher plasma levels of total and low-density lipoprotein cholesterol [54]. According to these mechanisms, our meta-analysis suggested that carrying the ε4 allele is a risk factor for MI and that the ε2 allele has a protective role in the development of MI. When stratifying the studies by ethnicity, the ε4 allele remained a risk factor and the ε2 allele was still protective in the development of MI among Caucasian populations; however, only the ε4 allele remained as a risk factor for MI among Asian population. This may be due to the small sample size in the analysis among Asian populations; in fact, there were only four studies that included Asian populations [19], [20], [26], [36]. Therefore, further studies are warranted among Asian populations. In addition, genotype distributions in the controls from Scaglione’s study [28], Bustan’s study [49] and Zende’s study [52] were not in agreement with HWE, therefore, the results may be biased. However, sensitivity analysis suggested that the pooled results were not significantly changed after excluding the three studies (data not shown). This may be due to the large sample size even though the three studies were excluded.
Although the primary results of this meta-analysis are suggestive, some limitations still exist. First, between-study heterogeneity existed in some of the genetic model analysis, which may have affected the results of the present meta-analysis, although a random effects model was adopted for these analyses. Second, publication bias may have occurred because our analyses were based wholly on published studies only in English and Chinese. Third, the results of this meta-analysis were based on unadjusted estimates because of the lack of adjusted estimates. Currently, some risk factors have been identified for MI, such as hypertension, hypercholesterolemia, diabetes, obesity and smoking. A more precise analysis should be performed if these data could be extracted from primary articles.
In conclusion, this comprehensive meta-analysis has evaluated all published data currently available on the association between the ApoE polymorphism and MI. Our meta-analysis suggested that the ε4 allele of ApoE is an risk factor for the development of MI and the ε2 allele of ApoE is a protective factor in the development of MI. This may be explained by the fact that ε4 allele of ApoE elevates the plasma levels of total and low-density lipoprotein cholesterol while the ε2 allele of ApoE lowers the circulating cholesterol levels. Further studies with larger sample sizes are warranted among Asian populations.
Supporting Information
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε2ε3 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε3ε4 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε4ε4 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε2 vs. ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε4 vs. ε3 analysis.
(TIF)
Cumulative meta-analysis of ApoE gene polymorphism and MI risk: A) ε2ε3 vs. ε3ε3 analysis; B) ε3ε4 vs. ε3ε3 analysi; C) ε4ε4 vs. ε3ε3 analysis.
(TIF)
Influence analysis of ApoE gene polymorphism and MI risk: A) ε2ε3 vs. ε3ε3 analysis; B) ε3ε4 vs. ε3ε3 analysi; C) ε4ε4 vs. ε3ε3 analysis.
(TIF)
Results of Egger’s and Begger’s test.
(XLS)
PRISMA Checklist.
(DOC)
Acknowledgments
We thank Dr Weifeng Qu for her excellent editorial work.
Funding Statement
This study was supported by the National Natural Science Foundation of China (NO.81200093) and the 2012 Shanghai College Special Research Funding for Outstanding Young Teachers (NO.82013011900002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 367: 1747–1757. [DOI] [PubMed] [Google Scholar]
- 2. Gu JY, Li LW (2014) ALDH2 Glu504Lys Polymorphism and Susceptibility to Coronary Artery Disease and Myocardial Infarction in East Asians: A Meta-analysis. Arch Med Res 45: 76–83. [DOI] [PubMed] [Google Scholar]
- 3. Wang J, Xu D, Wu X, Zhou C, Wang H, et al. (2011) Polymorphisms of matrix metalloproteinases in myocardial infarction: a meta-analysis. Heart 97: 1542–1546. [DOI] [PubMed] [Google Scholar]
- 4. Ozaki K, Tanaka T (2005) Genome-wide association study to identify SNPs conferring risk of myocardial infarction and their functional analyses. Cell Mol Life Sci 62: 1804–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Szpakowicz A, Pepinski W, Waszkiewicz E, Maciorkowska D, Skawronska M, et al. (2014) Retraction: polymorphism of 9p21.3 locus is associated with 5-year survival in high-risk patients with myocardial infarction. PLoS One 9: e95513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jin Y, Wang Q, Wang G, Zhang X, Yan B, et al. (2014) Common polymorphisms in the interleukin-6 gene and myocardial infarction risk: a meta-analysis. Genet Test Mol Biomarkers 18: 330–340. [DOI] [PubMed] [Google Scholar]
- 7. Wang Q, Zhou SB, Wang LJ, Lei MM, Wang Y, et al. (2014) Seven functional polymorphisms in the CETP gene and myocardial infarction risk: a meta-analysis and meta-regression. PLoS One 9: e88118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scott J, Knott TJ, Shaw DJ, Brook JD (1985) Localization of genes encoding apolipoproteins CI, CII, and E to the p13–cen region of human chromosome 19. Hum Genet 71: 144–146. [DOI] [PubMed] [Google Scholar]
- 9. Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH (1991) A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med 325: 373–381. [DOI] [PubMed] [Google Scholar]
- 10. Lahiri DK, Sambamurti K, Bennett DA (2004) Apolipoprotein gene and its interaction with the environmentally driven risk factors: molecular, genetic and epidemiological studies of Alzheimer’s disease. Neurobiol Aging 25: 651–660. [DOI] [PubMed] [Google Scholar]
- 11. Zhang R, Wang X, Tang Z, Liu J, Yang S, et al. (2014) Apolipoprotein E gene polymorphism and the risk of intracerebral hemorrhage: a meta-analysis of epidemiologic studies. Lipids Health Dis 13: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shin MH, Choi JS, Rhee JA, Lee YH, Nam HS, et al. (2014) APOE polymorphism and carotid atherosclerosis in Korean population: the Dong-gu Study and the Namwon Study. Atherosclerosis 232: 180–185. [DOI] [PubMed] [Google Scholar]
- 13.Singh NK, Banerjee BD, Bala K, Mitrabasu, Dung Dung AA, et al. (2014) APOE and LRPAP1 gene polymorphism and risk of Parkinson’s disease. Neurol Sci. [DOI] [PubMed]
- 14. Zhu S, Wang Z, Wu X, Shu Y, Lu D (2014) Apolipoprotein E polymorphism is associated with lower extremity deep venous thrombosis: color-flow Doppler ultrasound evaluation. Lipids Health Dis 13: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takeuchi F, Isono M, Katsuya T, Yokota M, Yamamoto K, et al. (2012) Association of genetic variants influencing lipid levels with coronary artery disease in Japanese individuals. PLoS One 7: e46385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chaudhary R, Likidlilid A, Peerapatdit T, Tresukosol D, Srisuma S, et al. (2012) Apolipoprotein E gene polymorphism: effects on plasma lipids and risk of type 2 diabetes and coronary artery disease. Cardiovasc Diabetol 11: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Atabek ME, Ozkul Y, Eklioglu BS, Kurtoglu S, Baykara M (2012) Association between apolipoprotein E polymorphism and subclinic atherosclerosis in patients with type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol 4: 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Song Y, Stampfer MJ, Liu S (2004) Meta-analysis: apolipoprotein E genotypes and risk for coronary heart disease. Ann Intern Med 141: 137–147. [DOI] [PubMed] [Google Scholar]
- 19. Yin YW, Sun QQ, Zhang BB, Hu AM, Liu HL, et al. (2013) Association between apolipoprotein E gene polymorphism and the risk of coronary artery disease in Chinese population: evidence from a meta-analysis of 40 studies. PLoS One 8: e66924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Utermann G, Hardewig A, Zimmer F (1984) Apolipoprotein E phenotypes in patients with myocardial infarction. Hum Genet 65: 237–241. [DOI] [PubMed] [Google Scholar]
- 21. Cumming AM, Robertson FW (1984) Polymorphism at the apoprotein-E locus in relation to risk of coronary disease. Clin Genet 25: 310–313. [DOI] [PubMed] [Google Scholar]
- 22. Lenzen HJ, Assmann G, Buchwalsky R, Schulte H (1986) Association of apolipoprotein E polymorphism, low-density lipoprotein cholesterol, and coronary artery disease. Clin Chem 32: 778–781. [PubMed] [Google Scholar]
- 23. Eichner JE, Kuller LH, Orchard TJ, Grandits GA, McCallum LM, et al. (1993) Relation of apolipoprotein E phenotype to myocardial infarction and mortality from coronary artery disease. Am J Cardiol 71: 160–165. [DOI] [PubMed] [Google Scholar]
- 24. Luc G, Bard JM, Arveiler D, Evans A, Cambou JP, et al. (1994) Impact of apolipoprotein E polymorphism on lipoproteins and risk of myocardial infarction. The ECTIM Study. Arterioscler Thromb 14: 1412–1419. [DOI] [PubMed] [Google Scholar]
- 25. Hergenc G, Taga Y, Emerk K, Cirakoglu B (1995) Apolipoprotein E Genotyping in Turkish Myocardial Infarction Survivors and Healthy Controls. J Biomed Sci 2: 46–49. [DOI] [PubMed] [Google Scholar]
- 26. Kim IJ, Hong BK, Lee BK, Kwon HM, Kim D, et al. (1999) Apolipoprotein E polymorphism in non-diabetic patients with acute coronary syndrome. Yonsei Med J 40: 377–382. [DOI] [PubMed] [Google Scholar]
- 27. Nakai K, Fusazaki T, Zhang T, Shiroto T, Osawa M, et al. (1998) Polymorphism of the apolipoprotein E and angiotensin I converting enzyme genes in Japanese patients with myocardial infarction. Coron Artery Dis 9: 329–334. [DOI] [PubMed] [Google Scholar]
- 28. Scaglione L, Bergerone S, Gambino R, Imazio M, Macchia G, et al. (1999) Role of lipid, apolipoprotein levels and apolipoprotein E genotype in young Italian patients with myocardial infarction. Nutr Metab Cardiovasc Dis 9: 118–124. [PubMed] [Google Scholar]
- 29. Lambert JC, Brousseau T, Defosse V, Evans A, Arveiler D, et al. (2000) Independent association of an APOE gene promoter polymorphism with increased risk of myocardial infarction and decreased APOE plasma concentrations-the ECTIM study. Hum Mol Genet 9: 57–61. [DOI] [PubMed] [Google Scholar]
- 30. Benes P, Muzik J, Benedik J, Frelich M, Elbl L, et al. (2000) Single effects of apolipoprotein B, (a), and E polymorphisms and interaction between plasminogen activator inhibitor-1 and apolipoprotein(a) genotypes and the risk of coronary artery disease in Czech male caucasians. Mol Genet Metab 69: 137–143. [DOI] [PubMed] [Google Scholar]
- 31. Batalla A, Alvarez R, Reguero JR, Hevia S, Iglesias-Cubero G, et al. (2000) Synergistic effect between apolipoprotein E and angiotensinogen gene polymorphisms in the risk for early myocardial infarction. Clin Chem 46: 1910–1915. [PubMed] [Google Scholar]
- 32. Raslova K, Smolkova B, Vohnout B, Gasparovic J, Frohlich JJ (2001) Risk factors for atherosclerosis in survivors of myocardial infarction and their spouses: comparison to controls without personal and family history of atherosclerosis. Metabolism 50: 24–29. [DOI] [PubMed] [Google Scholar]
- 33. Bai X, Zhao M, Wang B (2001) [Dyslipidemia-related risk factors for myocardial infarction and polymorphism of ApoE gene among myocardial infarction patients and their siblings]. Zhonghua Yi Xue Za Zhi 81: 340–343. [PubMed] [Google Scholar]
- 34. Freitas EM, Phan TC, Herbison CE, Christiansen FT, Taylor RR, et al. (2002) The poliovirus receptor related 2 (PRR2) and apolipoprotein E genes and coronary heart disease. J Cardiovasc Risk 9: 59–65. [DOI] [PubMed] [Google Scholar]
- 35. Mamotte CD, Burke V, Taylor RR, van Bockxmeer FM (2002) Evidence of reduced coronary artery disease risk for apolipoprotein epsilon2/3 heterozygotes. Eur J Intern Med 13: 250–255. [DOI] [PubMed] [Google Scholar]
- 36. Kolovou G, Yiannakouris N, Hatzivassiliou M, Malakos J, Daskalova D, et al. (2002) Association of apolipoprotein E polymorphism with myocardial infarction in Greek patients with coronary artery disease. Curr Med Res Opin 18: 118–124. [DOI] [PubMed] [Google Scholar]
- 37. Keavney B, Parish S, Palmer A, Clark S, Youngman L, et al. (2003) Large-scale evidence that the cardiotoxicity of smoking is not significantly modified by the apolipoprotein E epsilon2/epsilon3/epsilon4 genotype. Lancet 361: 396–398. [DOI] [PubMed] [Google Scholar]
- 38. Kolovou GD, Daskalova D, Hatzivassiliou M, Yiannakouris N, Pilatis ND, et al. (2003) The epsilon 2 and 4 alleles of apolipoprotein E and ischemic vascular events in the Greek population–implications for the interpretation of similar studies. Angiology 54: 51–58. [DOI] [PubMed] [Google Scholar]
- 39. Kumar P, Luthra K, Dwivedi M, Behl VK, Pandey RM, et al. (2003) Apolipoprotein E gene polymorphisms in patients with premature myocardial infarction: a case-controlled study in Asian Indians in North India. Ann Clin Biochem 40: 382–387. [DOI] [PubMed] [Google Scholar]
- 40. Marques-Vidal P, Bongard V, Ruidavets JB, Fauvel J, Perret B, et al. (2003) Effect of apolipoprotein E alleles and angiotensin-converting enzyme insertion/deletion polymorphisms on lipid and lipoprotein markers in middle-aged men and in patients with stable angina pectoris or healed myocardial infarction. Am J Cardiol 92: 1102–1105. [DOI] [PubMed] [Google Scholar]
- 41. Keavney B, Palmer A, Parish S, Clark S, Youngman L, et al. (2004) Lipid-related genes and myocardial infarction in 4685 cases and 3460 controls: discrepancies between genotype, blood lipid concentrations, and coronary disease risk. Int J Epidemiol 33: 1002–1013. [DOI] [PubMed] [Google Scholar]
- 42. Ranjith N, Pegoraro RJ, Rom L, Rajput MC, Naidoo DP (2004) Lp(a) and apoE polymorphisms in young South African Indians with myocardial infarction. Cardiovasc J S Afr 15: 111–117. [PubMed] [Google Scholar]
- 43. Baum L, Ng HK, Wong KS, Tomlinson B, Rainer TH, et al. (2006) Associations of apolipoprotein E exon 4 and lipoprotein lipase S447X polymorphisms with acute ischemic stroke and myocardial infarction. Clin Chem Lab Med 44: 274–281. [DOI] [PubMed] [Google Scholar]
- 44. Aasvee K, Jauhiainen M, Kurvinen E, Tur I, Sundvall J, et al. (2006) Determinants of risk factors of atherosclerosis in the postinfarction period: the Tallinn MI study. Scand J Clin Lab Invest 66: 191–199. [DOI] [PubMed] [Google Scholar]
- 45. Koch W, Hoppmann P, Schomig A, Kastrati A (2008) Apolipoprotein E gene epsilon2/epsilon3/epsilon4 polymorphism and myocardial infarction: case-control study in a large population sample. Int J Cardiol 125: 116–117. [DOI] [PubMed] [Google Scholar]
- 46. Kolovou GD, Anagnostopoulou KK, Cokkinos DV (2009) Apolipoprotein E gene polymorphism and myocardial infarction. Int J Cardiol 133: 264–265. [DOI] [PubMed] [Google Scholar]
- 47. Bahri R, Esteban E, Moral P, Hassine M, Ben Hamda K, et al. (2008) Apolipoprotein gene polymorphisms and plasma levels in healthy Tunisians and patients with coronary artery disease. Lipids Health Dis 7: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Martinelli N, Olivieri O, Shen GQ, Trabetti E, Pizzolo F, et al. (2009) Additive effect of LRP8/APOER2 R952Q variant to APOE epsilon2/epsilon3/epsilon4 genotype in modulating apolipoprotein E concentration and the risk of myocardial infarction: a case-control study. BMC Med Genet 10: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Al-Bustan SA, Alkhalaf M, Al-Rashdan I, Al-Otaibi S, Al-Baker E, et al. (2009) Apolipoprotein E, CI and B gene polymorphisms in a sample of patients with coronary heart disease in the Kuwaiti population. Med Princ Pract 18: 294–299. [DOI] [PubMed] [Google Scholar]
- 50. Onrat ST, Akci O, Soylemez Z, Onrat E, Avsar A (2012) Prevalence of myocardial infarction polymorphisms in Afyonkarahisar, Western Turkey. Mol Biol Rep 39: 9257–9264. [DOI] [PubMed] [Google Scholar]
- 51. Tanguturi P, Pullareddy B, Kumar PS, Murthy DK (2013) Association between apolipoprotein E gene polymorphism and myocardial infarction. Biochem Genet 51: 398–405. [DOI] [PubMed] [Google Scholar]
- 52. Zende PD, Bankar MP, Kamble PS, Momin AA (2013) Apolipoprotein e gene polymorphism and its effect on plasma lipids in arteriosclerosis. J Clin Diagn Res 7: 2149–2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Eichner JE, Dunn ST, Perveen G, Thompson DM, Stewart KE, et al. (2002) Apolipoprotein E polymorphism and cardiovascular disease: a HuGE review. Am J Epidemiol 155: 487–495. [DOI] [PubMed] [Google Scholar]
- 54. Dallongeville J, Lussier-Cacan S, Davignon J (1992) Modulation of plasma triglyceride levels by apoE phenotype: a meta-analysis. J Lipid Res 33: 447–454. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε2ε3 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε3ε4 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε4ε4 vs. ε3ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε2 vs. ε3 analysis.
(TIF)
Forest plot for ApoE gene polymorphism and MI risk in the genetic model of ε4 vs. ε3 analysis.
(TIF)
Cumulative meta-analysis of ApoE gene polymorphism and MI risk: A) ε2ε3 vs. ε3ε3 analysis; B) ε3ε4 vs. ε3ε3 analysi; C) ε4ε4 vs. ε3ε3 analysis.
(TIF)
Influence analysis of ApoE gene polymorphism and MI risk: A) ε2ε3 vs. ε3ε3 analysis; B) ε3ε4 vs. ε3ε3 analysi; C) ε4ε4 vs. ε3ε3 analysis.
(TIF)
Results of Egger’s and Begger’s test.
(XLS)
PRISMA Checklist.
(DOC)