Abstract
Acute type B aortic dissection (ABAD) is a serious cardiovascular emergency in which morbidity and mortality are often related to the presence of complications at clinical presentation. Visceral, renal, and limb ischemia occur in up to 30% of patients with ABAD and are associated with higher in-hospital mortality. The aim of the open fenestration is to resolve the malperfusion by creating a single aortic lumen at the suprarenal or infrarenal level. This surgical procedure is less invasive than total aortic replacement, thus not requiring extracorporeal support and allowing preservation of the intercostal arteries, which results in decreased risk of paraplegia. Surgical aortic fenestration represents an effective and durable option for treating ischemic complications of ABAD, particularly for patients with no aortic dilatation. In the current endovascular era, this open technique serves as an alternative option in case of contraindications or failure of endovascular management of complicated ABAD.
Keywords: Acute type B aortic dissection, open fenestration, malperfusion
Introduction
Acute type B aortic dissection (ABAD) is a serious cardiovascular emergency in which morbidity and mortality are often related to the presence of complications at clinical presentation. Visceral, renal, and limb ischemia occur in up to 30% of patients with ABAD and are associated with higher in-hospital mortality. Surgical or endovascular interventions for ABAD are indicated in case of malperfusion syndromes, extension of dissection, and/or aortic rupture. Surgical aortic fenestration was the first operation for the management of complicated aortic dissection, performed for the first time in 1935 by Gurin and colleagues (1). The technique is based on the concept of creating a single lumen, which is believed to resolve malperfusion and limits the risks of intestinal infarction, acute renal failure, and limb ischemia.
Malperfusion syndrome occurs when there is end-organ ischemia secondary to aortic branch compromise from the dissecting process. This can involve one or more aortic branches simultaneously. As consequence, the morbid clinical events will vary as a function of the vascular territory involved.
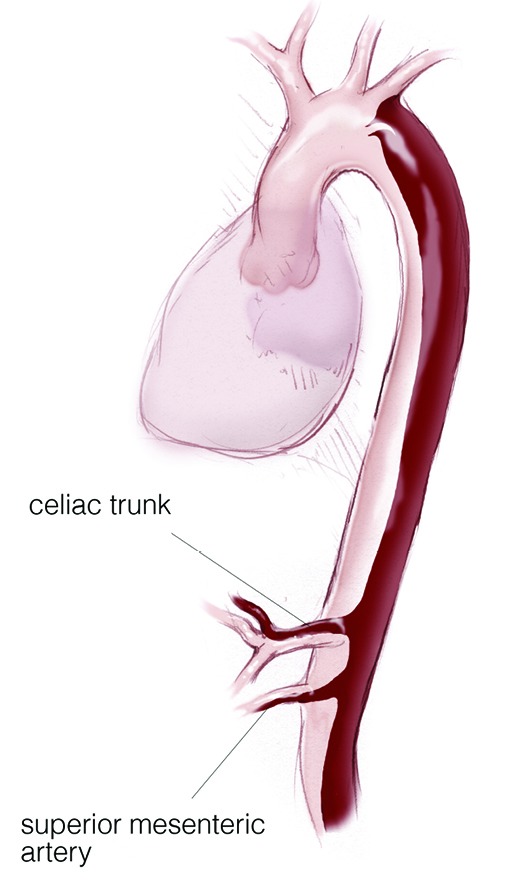
In the presence of a proximal tear and absence of distal re-entries, the false lumen pressure increases, leading to compression of the true lumen. Such mechanisms can potentially lead to impaired perfusion of distal organs, increasing the risk for visceral and renal ischemia (Figure 1). In acute dissections, treatment priority should be assigned to the most life-threatening condition. In acute dissections, treatment priority should be assigned to the most life-threatening conditions. Among these, mesenteric ischemia is highly associated with poor outcome, and may require initial urgent management also in type A dissections, before central aortic repair.
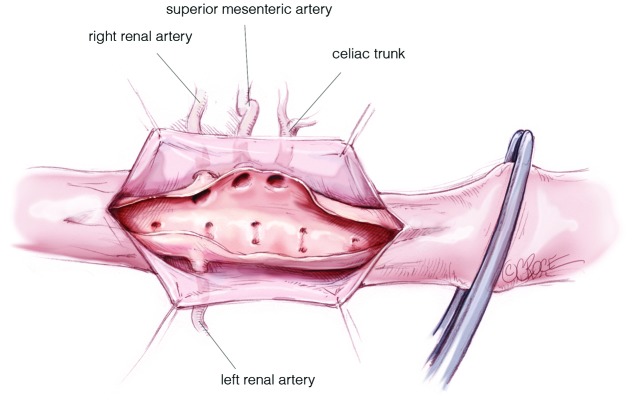
Figure 1.
Complete dissection of the thoraco-abdominal-aorta (type B) below the origin of the subclavian artery to the left common iliac artery. In this case the celiac trunk and the superior mesenteric artery are dissected and the left renal artery is excluded.
In the current era, endovascular procedures, such as thoracic endovascular aortic repair (TEVAR) or fenestration, represent the first line of treatment in ABAD complicated by malperfusion. Open surgical fenestration may be used as an alternative treatment should contraindications or failure of endovascular management arise. It has been associated with favorable short and long-term outcome.
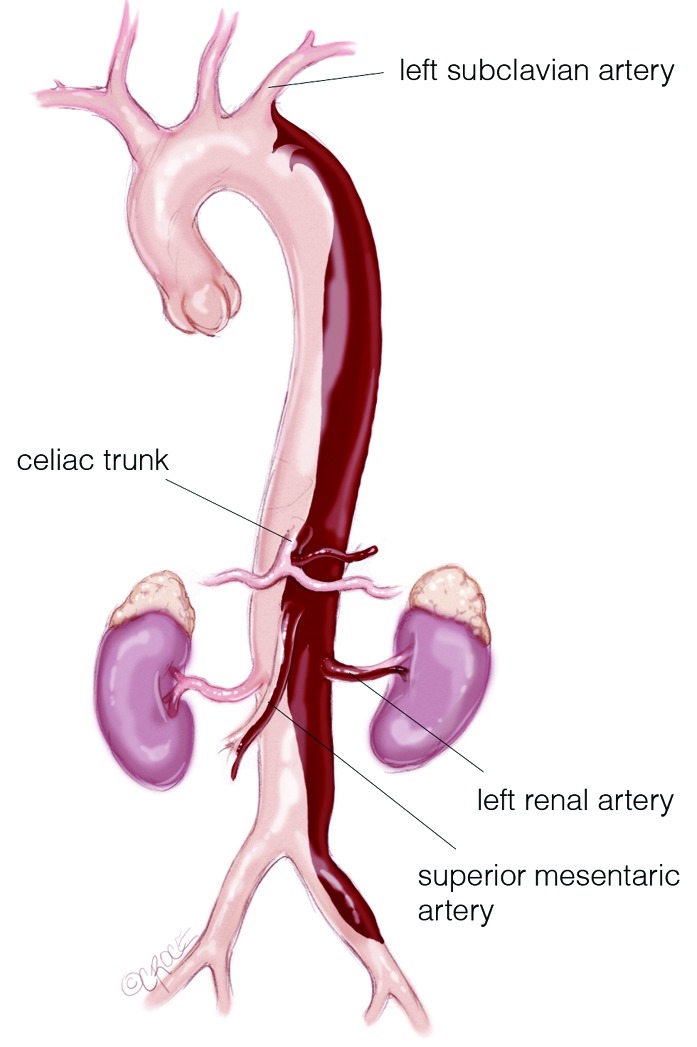
Two mechanisms for aortic branch vessel compromise have been identified, each of which has specific treatment implications in the management of malperfusion syndromes (Figure 2).
Figure 2.
Aortic axial view showing dynamic (A) dynamic and (B) static obstruction.
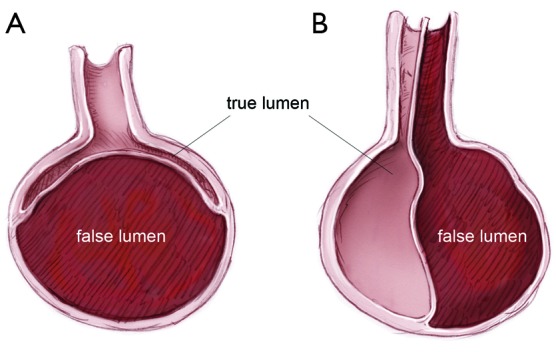
Dynamic obstruction
Dynamic obstruction is the more common mechanism of aortic branch malperfusion, caused by the prolapse of the dissection flap into the vessel ostium (Figure 3). Such occlusion is usually evident during the aortic systole, and causes about 80% of malperfusion syndromes. Dynamic obstruction can be determined by cardiac output, blood pressure, heart rate, peripheral resistance of the outflow vessel, and the circumference involvement of the dissected aorta. Typically, in ABAD with peripheral malperfusion, arterial pulses may not be continuously present because of the variability of these hemodynamic and anatomic conditions. Management of the aortic true lumen, based on the coverage of the proximal entry tear using stent-grafts, usually restores an adequate branch inflow.
Figure 3.
In dynamic obstruction (A,B), the septum may prolapse into the vessel ostium during the cardiac cycle, and the compressed true lumen flow is inadequate to perfuse branch vessel ostia, which remain anatomically intact.
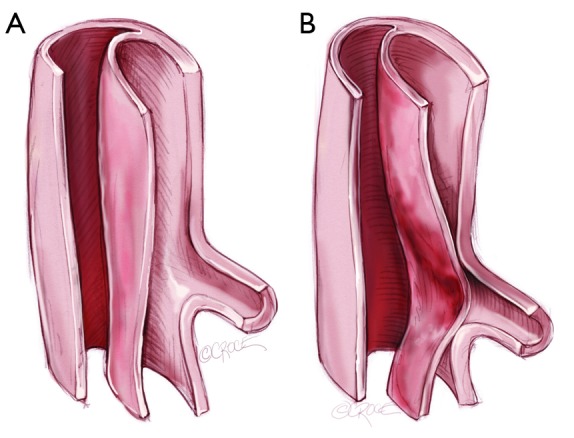
Static obstruction
In ABAD, obstruction of the aortic branch vessels may be related to a blind end of false lumen, which can compress and thrombose aortic branches (Figure 4A). In other cases, the intimal flap may extend into the branch vessels. The simultaneous presence of the true and false lumen within the artery can be associated with compression and the subsequent reduction or loss of the proper area for the blood flow (Figure 4B). Additionally, false lumen may be thrombosed due to the blind end of the arterial branch dissection in absence of distal re-entry tears. Thrombosis of the true lumen beyond the compromised ostia may further degrade distal perfusion (Figure 4C). All these mechanisms for malperfusion syndrome are defined as static obstruction. In these circumstances the restoration of the aortic branch true lumen flow requires management of the vessel itself (stent, fenestration, bypass graft).
Figure 4.
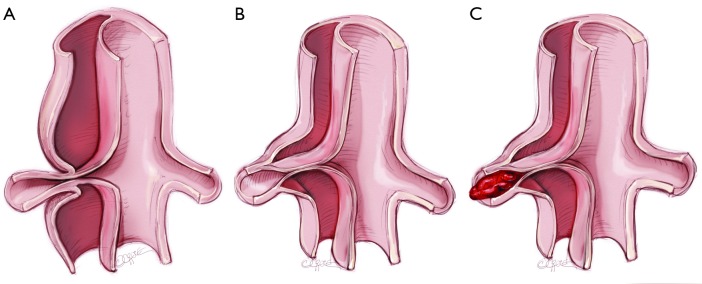
Mechanisms of static obstruction. (A) Compression of the vessel by blind ends of the false lumen; (B) presence of true and false lumen in the vessel causing further compression; (C) thrombosis of the vessel distal to the compromised ostia.
Operative technique
In ABAD patients with visceral or renal ischemia who require open surgery (Figure 5), the surgical approach is performed through a thoraco-abdominal incision in the 8th or 10th intercostal space (Figure 6). This incision allows adequate exposure of the supraceliac and infra-diaphragmatic aorta (Figure 7).
Figure 5.
Acute type B aortic dissection (ABAD) involving visceral segment.
Figure 6.
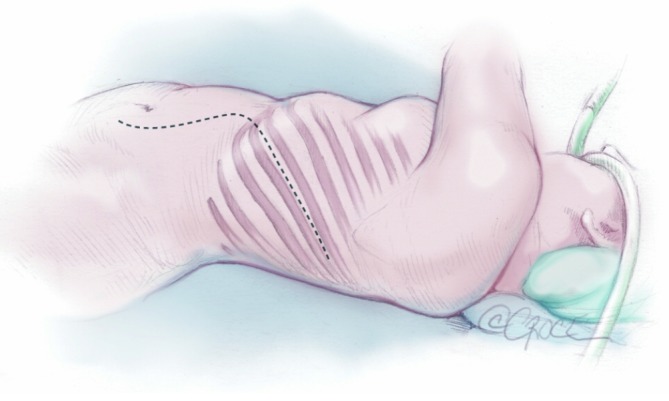
Exposure is achieved through a thoraco-abdominal incision in the 8th or 10th intercostal spaces.
Figure 7.
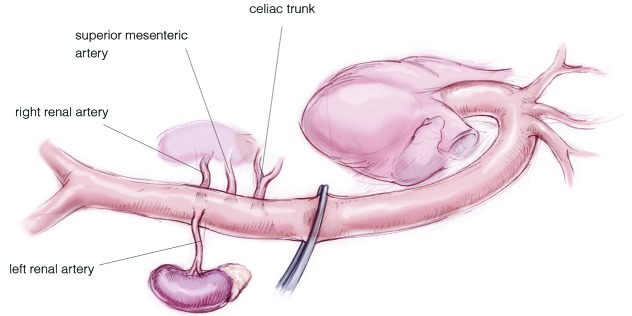
The visceral segment of the aorta is exposed.
After preparation of thoracoabdominal aorta and its branches, a supra-diaphragmatic clamp is placed without the use of any extracorporeal support. Distally, the aorta is clamped at the level of its bifurcation. A longitudinal aortotomy is performed (typically 5-8 cm), and the true and false lumens are identified (Figure 8).
Figure 8.
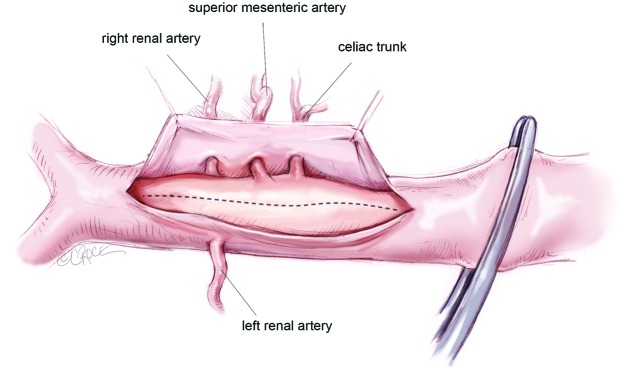
The true and false lumen of the aorta is identified.
The intimal membrane is widely resected, leaving behind the adherent intima. The dissected flap is proximally and distally resected in a triangular shape, to maximize the single aortic lumen. If the dissection extended into the visceral and/or renal arteries, a similar technique is adopted in these arteries (Figure 9).
Figure 9.
The visceral ostia after the removal of the intimal flap.
The longitudinal aortotomy is then sutured and reinforced with strips of Teflon, which resulted in a slightly reduced aortic diameter (Figure 10).
Figure 10.
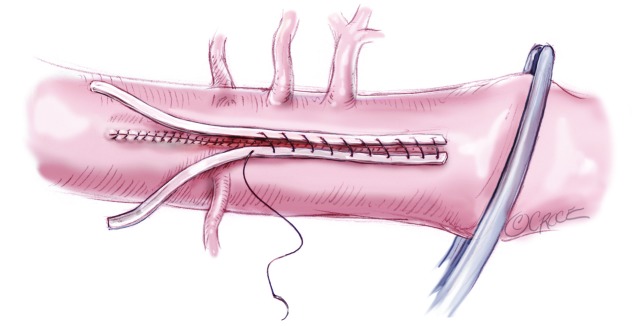
The suture is reinforced with Teflon strips.
In ABAD patients with limb ischemia and no visceral/renal malperfusion, the open treatment is conducted through a median laparotomy.
The aorta is clamped at the suprarenal of infrarenal level and at the iliac arteries, and then opened in a crossway. After identification of the true and false lumen, the dissected flap is resected longitudinally for 2 to 3 cm, from above to just below the level of the renal arteries. The intimal flap is resected proximally in a triangular shape to maximize the single aortic lumen (Figure 11). The distal extent of the intimal flap is fixed to adventitia, and the aortic wall is reinforced both internally and externally with strips of Teflon (Figure 12A). Aortic replacement with a Dacron graft is performed in those cases with complete infrarenal aortic or iliac occlusion and/or abdominal aortic aneurysm (Figure 12B).
Figure 11.
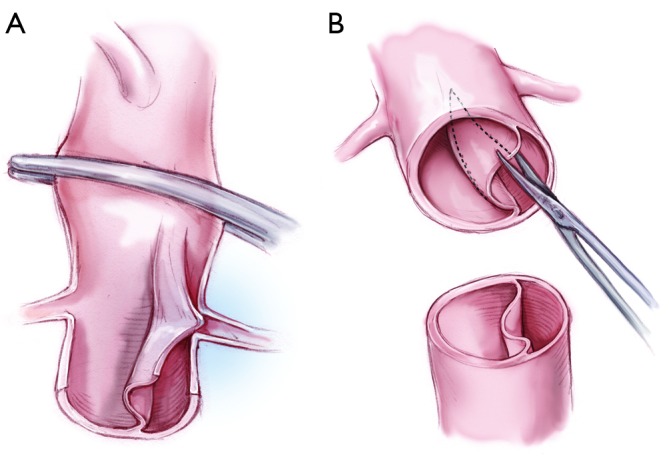
This represents the particular of another fenestration technique: (A) transection of the aorta; (B) septum resection.
Figure 12.
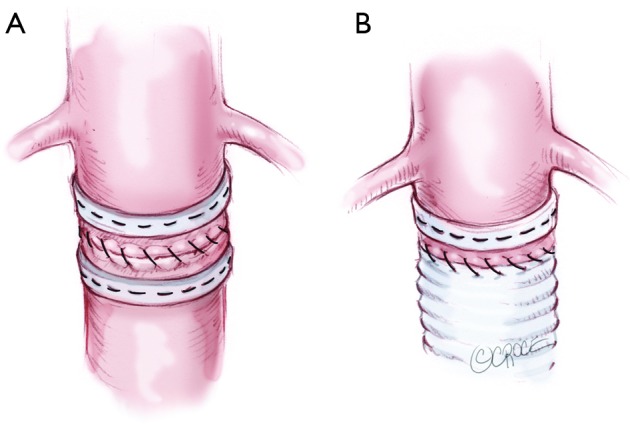
This represents two type of repair: (A) aortic walls sutures with two Teflon felt stripes; (B) the infrarenal tract of the aorta is also replaced with a surgical graft.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Gurin D, Bulmer JW, Derby R. Dissecting aneurysm of the aorta: diagnosis and operative relief of acute arterial obstruction due to this cause. NY State J Med 1935;35:1200-2 [Google Scholar]