Abstract
Objective
To determine the effect of PNS on pain reduction for those with refractory SIS, and to evaluate the association with reduced disability, impairment, and safety. Our hypotheses are that PNS will be associated with a reduction in pain, impairment and disability, and improvement in quality of life while demonstrating safety.
Methods
Adults with shoulder pain of at least 6 months duration were recruited from for a 3-week treatment of percutaneous peripheral nerve stimulation applied through a percutaneous electrode to the axillary motor points of the deltoid muscle. Subjects were followed for 12 weeks after treatment. The primary outcome was the worst pain in the last week, and secondary outcomes included pain interference, the Disabilities of the Arm Shoulder Hand questionnaire, shoulder abduction range of motion, and safety. Analysis was with a linear mixed model.
Results
Ten subjects were recruited. Longitudinal analysis demonstrated significant reduction in pain relative to baseline (F(1, 66)=12.9, p<0.01). After correcting for multiple comparisons, there were significant reductions at explant and all follow-up time points when compared to baseline. There were also significant improvements in pain interference (F(1,65)=15.0, P <0.01), the Disabilities of the Arm Shoulder Hand questionnaire (F(1,35)=7.0, P =0.01), and shoulder abduction range of motion (F(1,35)=6.3, P =0.02).
Conclusion
Intramuscular peripheral nerve stimulation for chronic shoulder pain due to subacromial impingement syndrome is a safe treatment associated with pain reduction, lower pain interference with ADLs, reduced disability, and improved shoulder abduction. Pain reduction is maintained for at least 12 weeks after treatment.
Keywords: Chronic Pain, Electrode Placement, Nonmalignant pain, Percutaneous nerve stimulation, Peripheral nerve stimulation, subacromial impingement syndrome, shoulder pain, electrical stimulation
Introduction
Shoulder pain is a common problem in the healthy adult population, accounting for 16% of musculoskeletal complaints1 and 12 million physician visits annually in the United States.2 The point prevalence of shoulder pain has been estimated to be 7–7% in adults less than 70 years old, with 12-month prevalence being up to 47%.3 While there are multiple causes of shoulder pain, subacromial impingement syndrome (SIS) is the most common cause, estimated to comprise up to 48% of incident cases.4
The clinical syndrome of SIS is typically associated with pain with movement of the shoulder, most commonly when raising the arm overhead. Anatomically, SIS refers to the supraspinatus tendon impinging on the undersurface of the anterior acromion as the shoulder is abducted or flexed. Multiple pathologies, such as subacromial bursitis, rotator cuff tendinopathy, partial rotator cuff tears, and even small tears, either in isolation or through a combination, can create the syndrome of subacromial impingement. Regardless of the exact pathology, conservative treatment is aimed at controlling pain with rest, non-steroidal anti-inflammatory drugs, corticosteroid injections, and improving biomechanics of the shoulder through physical therapy. Approximately half of the patients will respond acutely to conservative management.5
When conservative treatment has failed and chronic pain persists, patients are often referred for surgical management of subacromial decompression.6, 7 Unfortunately, randomized controlled trials have not shown surgical management of SIS to be better than conservative therapy.8–11 Presently, there are no established treatments for those with SIS who have failed conservative treatment.
We previously published a case-report of successful treatment of chronic pain due to SIS, in a participant who had failed treatment of physical therapy and corticosteroid injection, with treatment by percutaneous peripheral nerve stimulation (PNS).12 The treatment of SIS with PNS involves the temporary placement of a single, percutaneously placed electrode that provides stimulation to the terminal branches of the axillary nerve to the deltoid muscle for 3 weeks. This study presents the results of a complete case-series of 10 participants with refractory SIS treated with PNS for pain relief. The objective is to determine the effect of PNS on pain reduction for those with refractory SIS, and to evaluate the association with reduced disability, impairment, and safety. Our hypotheses are that PNS will be associated with a reduction in pain, impairment and disability, and improvement in quality of life while demonstrating safety.
Methods
Participants
This was a single center, unblinded case series of percutaneous PNS for SIS. Eligible participants were adults aged 21 years and older with shoulder pain subjectively rated at least a 4 out of 10 on the 11-point numeric rating scale of the Brief Pain inventory Short Form, question 3 (BPI-SF3). 13, 14 The pain had to be present 6 months or longer, and the participant had to have previously participated in physical or occupational therapy for shoulder pain and previous subacromial corticosteroid injection at the affected shoulder. Participants had to have a positive response to Neer’s test15 (subacromial injection of 5cc 2% lidocaine), defined as 50% or greater reduction in pain with shoulder flexion and external rotation. To exclude large rotator cuff tears, participants had to have a muscle strength of at least a 4 out of 5 grading (Medical Research Council Scale16) in shoulder abduction, internal rotation, and external rotation after subacromial lidocaine injection. Participants were required to have the ability to check their skin, or have the availability of the assistance of a reliable adult. Exclusion criteria included evidence of joint or overlying skin infection or history of recurrent skin infections; the need for sustained release opioid analgesics for shoulder pain or other chronic pain syndrome; subacromial corticosteroid injections to the shoulder in the previous 8 weeks; currently receiving physical or occupational therapies for shoulder pain; bleeding disorder or INR > 3.0 for those on Coumadin; medical instability; pregnancy; uncontrolled seizures (>1 per month for the last 6 months); evidence of pain (local tenderness or from provocative testing) at the long-head biceps tendon or acromioclavicular joint that contributed significantly to pain in the affected shoulder; moderate to severe depression (Beck Depression Inventory-Fast Screen17 13 or above); other confounding neurological conditions involving the affected the upper limb; allergy to skin-surface electrodes or lidocaine; an implanted electronic device such as cardiac pacemaker or defibrillator; valvular heart disease including artificial valves; or compromised immune system.
The study took place at an urban, academic rehabilitation center in the United States from April, 2011 through March, 2013. The protocol was approved by the local institutional review board.
Treatment and Evaluation
After obtaining informed consent, all participants received a percutaneously placed lead to stimulate the terminal branches of the axillary nerve to the middle and posterior deltoids. The procedure was previously described (see Figure 1).12 The electrode remained in place for a one-week stabilization period without delivery of stimulation. The lead was then connected to the stimulator and parameters were set to stimulate the middle and posterior deltoids at 12 Hz and 20 mA. Pulse duration, with a range of 20–200 microseconds, was adjusted to produce the strongest muscle contraction of the middle and posterior deltoids without causing discomfort to the participant. Participants were prescribed 6 hours of stimulation per day for 3 weeks, to be completed in single or divided doses, for a total of 126 hours of stimulation. The rationale for 3 weeks of treatment came from review of data from a prior trial of PNS in hemiplegic shoulder pain18 in which the data suggested that many of those subjects who experienced pain reduction did so after 3 weeks of treatment. Two subsequent studies in which 3 weeks of stimulation was prescribed for hemiplegic shoulder pain found an association with successful pain relief.19, 20 The stimulator completed a cycle every 30 seconds consisting of 5 seconds to ramp up, 10 seconds at maximum stimulation, 5 seconds to ramp down, and 10 seconds of no stimulation. At the conclusion of the 3-week stimulation period, the lead was removed by gently pulling on its exposed end. Afterward, participants underwent anterior-posterior and scapular-Y view radiographs of the shoulder for surveillance for retained lead fragments.
Figure 1.
Percutaneous IM PNS Smartpatch™ System. Top: Percutaneous IM Electrode loaded in a 20-gauge introducer. Bottom left: External stimulator mounted on the pad (anode electrode-embedded battery). Bottom right: Configuration on participant.
The electrical stimulation was provided by a small (58 × 36 × 14 mm) body-worn device (Smartpatch™, SPR Therapeutics, Cleveland, OH). The stimulator attached to the skin using the Smartpatch Pad, a custom surface electrode that includes an embedded battery (see Figure 1). The device has a compliance monitor that records the total time of stimulator usage.
Participants underwent outcomes assessments by a physical therapist at implantation (week 0), start of stimulation (week 1), end of stimulation (week 4), and follow-up assessments at weeks 5, 8, and 16. Two telephone assessments also were completed at weeks 2 and 3 to assess the primary (BPI-SF3) and one secondary outcome (BPI-SF9).
The primary outcome measure was BPI-SF313, 21, which asks participants to rate their worst shoulder pain in the last week on a 0 to 10 numeric rating scale, where “0” indicates “No pain” and “10” indicates “Pain as bad as you can imagine.” Secondary outcomes included: 1) pain interference with activities of daily living, BPI-SF question 9 (BPI-SF 9)13, 21, which assesses the degree to which pain interferes with general activity, mood, walking ability, normal work, interpersonal relationships, sleep and enjoyment of life on a 0–10 numeric rating scale, where “0” indicates no interference and “10” indicates complete interference; 2) the Disabilities of the Arm, Shoulder, and Hand questionnaire (DASH)22, 23, a 30-item questionnaire measuring physical function and symptoms in people with musculoskeletal disorders of the upper limb on a scale of 0 to 100, with 0 indicating least disability and 100 indicating most disability; 3) active, pain-free abduction range of motion24 measured with a standard goniometer from a standing position; 4) the Patient Global Impression of Change (PGIC) Scale25, in which participants rate how much their quality of life has changed since the beginning of the study; and, 4) and a measure of secondary hyperalgesia, the pressure-pain threshold (PPT). The PPTs were measured at the deltoid of the affected shoulder, unaffected shoulder, and the tibialis anterior muscle on the unaffected side. The PPT is a measure of deep somatic tissue sensitivity, indicated by the amount of pressure (kg/cm2) from a handheld algometer where a sensation of pressure first changes to pain.26 The average of 3 measurements at each location is reported.
Treatment success was defined as a reduction in the worst pain in the past week (BPI-SF3) of 2 points or 30% at end of treatment. A 2-point or 30% reduction has been shown to be a clinically relevant reduction in pain, and has been recommended as an outcome in chronic pain trials.27, 28
Statistical Analysis
Due to the exploratory nature of this study, a formal power analysis was not completed. The effect of treatment group over time was analyzed using a linear mixed model for repeated measures with random effects for intercept and a first-order ante-dependent covariance structure, since it is reasonable to assume that for each individual there is a greater correlation between assessments that are closer together and that variance might be different at different assessments. The dependent variable was week (continuous), representing a change over the course of the study. To evaluate the dependent variables at discrete time points, the same model was used with the dependent variable week (ordinal). Pairwise comparisons between baseline and the discrete time points of end of treatment (EOT, week 4) and follow-up time points (weeks 5, 8, and 16) of the least squares means were computed from the model with discrete time points, and significance levels were interpreted using a Bonferroni correction (alpha=0.0125). In both models, missing data were handled by a maximum likelihood algorithm and the analyses were conducted by the available-case, intention-to-treat method.
The association of changes in PPTs with a successful outcome were evaluated in a similar fashion but with the dependent variable being an indicator for group (success or not) and variables for week (continuous, ordinal) , a group interaction by week interaction, and a covariate for gender, which is known to affect PPTs.29
All statistical analyses were made with SAS/STAT® 9.3 software (SAS Institute Inc., Cary, NC, USA).
Results
Ten participants were recruited. Demographics are shown in Table 1. Three participants did not complete all outcomes assessments. One was lost to follow-up after completing the 5-week assessment. Two withdrew after having a corticosteroid injection, one of the subacromial space and the other of the long-head biceps tendon, both occurring after the 8-week assessment. Overall, 7 participants completed all outcomes assessments.
Table 1.
Baseline demographics
| n | 10 |
| Age (year, +/− SD) | 52.2 (+/−7.6) |
| Female | 6 |
| White | 5 |
| Black | 4 |
| Hispanic | 1 |
| Worst pain in 7d (baseline, +/− SD) | 8.5 (+/− 1.9) |
| Duration of pain (year, +/− SD) | 4.3 (+/− 5.6) |
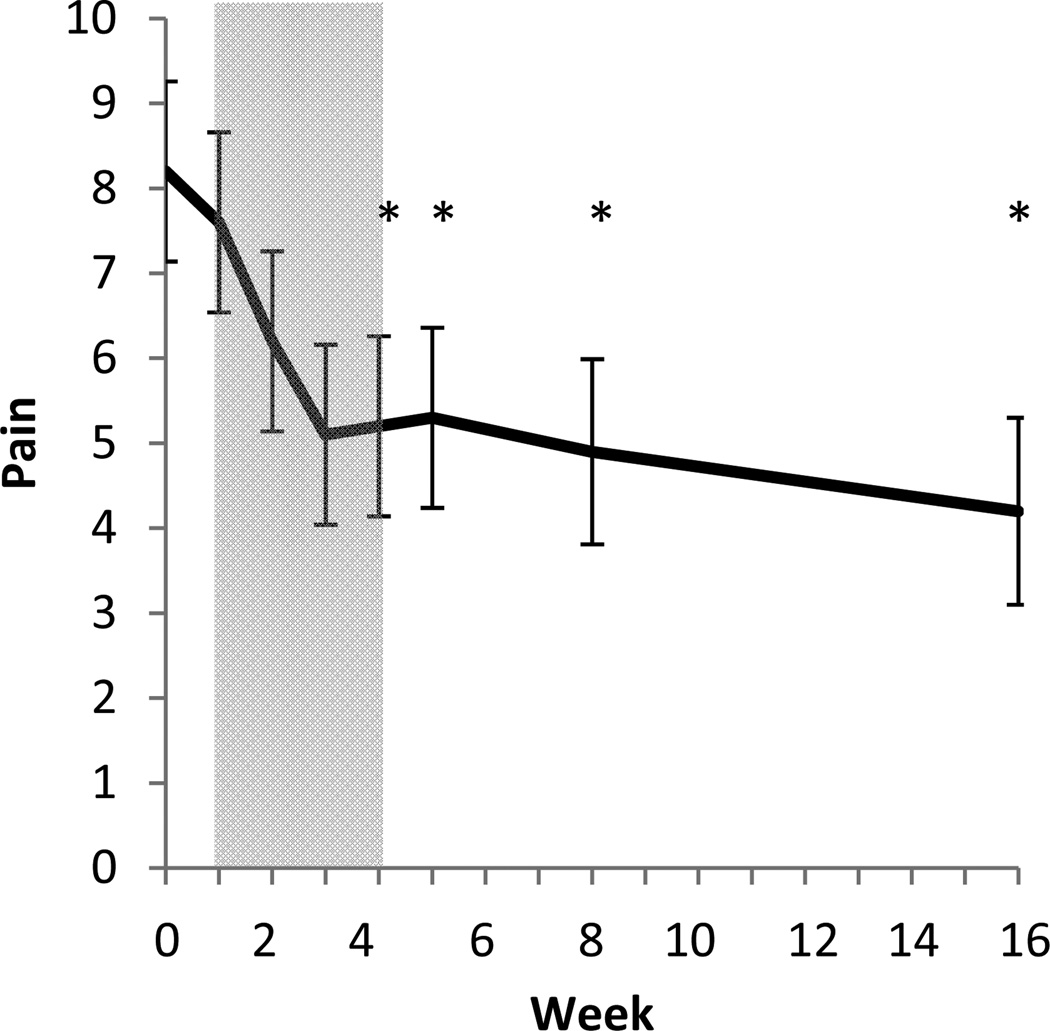
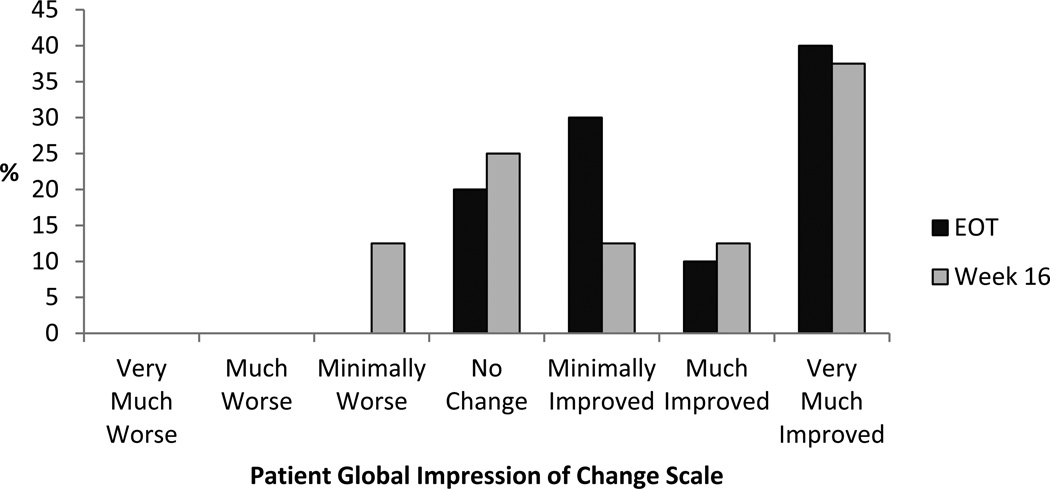
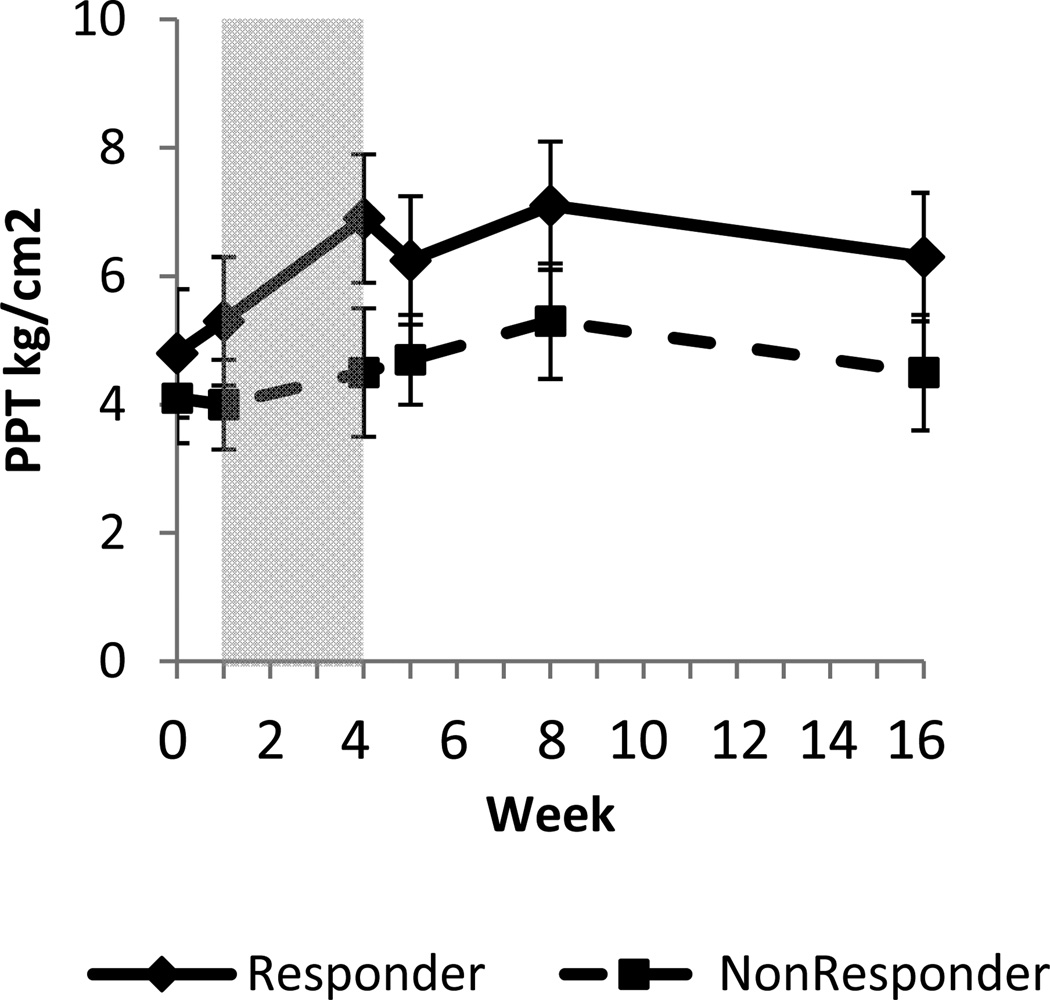
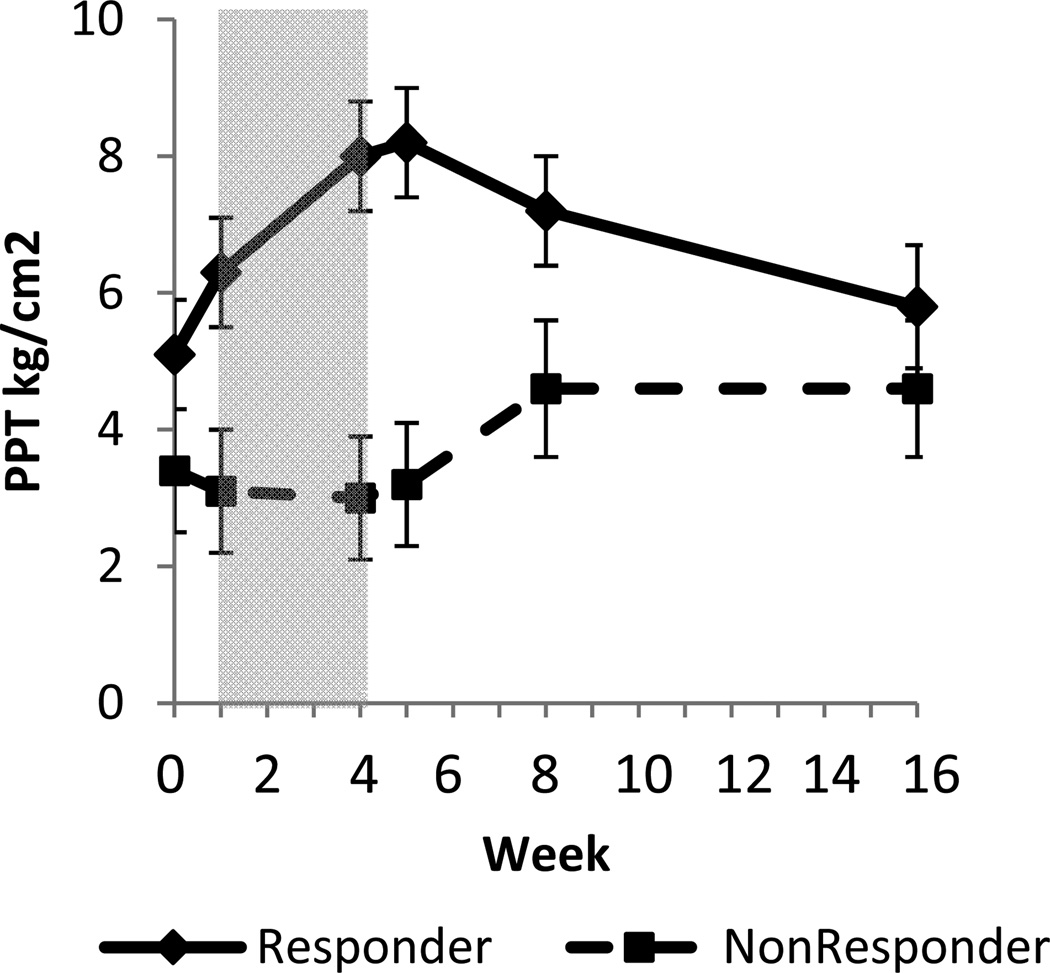
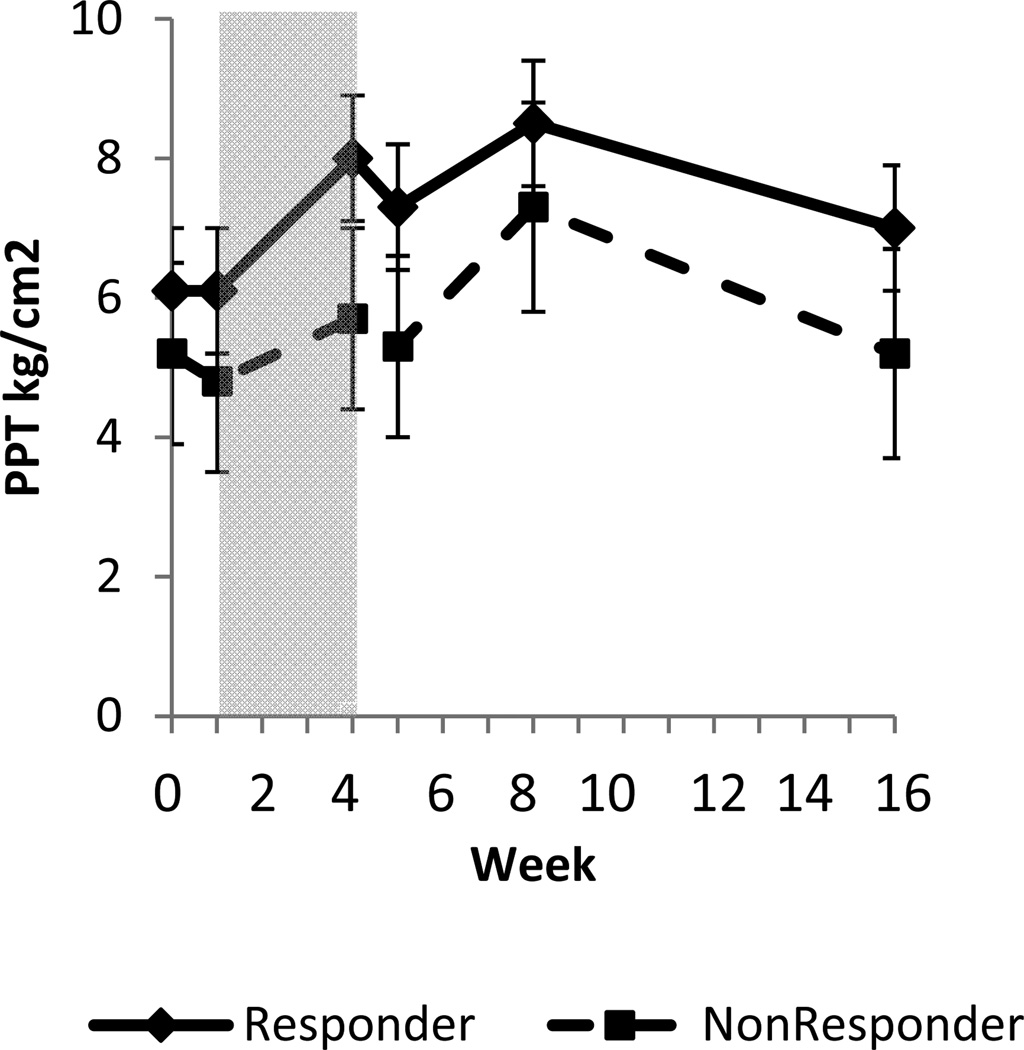
Pain. There was a significant reduction in pain in the longitudinal analysis (BPI-SF3, F(1, 66)=12.9, p<0.01, Table 2, Figure 2). Compared to baseline and taking into account multiple comparisons (alpha=0.0125), there were significant reductions in pain at EOT (36.6%, P<0.01), at week 5 (35.4%, P <0.01), at week 8 (40.2%, P <0.01), and at week 16 (48.8%, P <0.01). Treatment success (a 2 point or 30% reduction in pain at EOT) was met for 60% (6 out of 10) participants. Disability. There was a significant reduction in shoulder-related disability in the longitudinal analysis (DASH, F(1,35)=7.0, P =0.01, Table 2). Compared to baseline, there were significant reductions at EOT (45.5%, P <0.01), week 5 (37.4%, P =0.01), week 8 (53.7%, P <0.01), and week 16 (47.5%, P <0.01). Pain interference. There was a significant reduction in pain interference in the longitudinal analysis (BPI-SF9, F(1,65)=15.0, P <0.01, Table 2). Compared to baseline, there were significant reductions at EOT (52.0%, P <0.01), week 5 (46.0%, P <0.01), week 8 (60.0%, P <0.01), and week 16 (58.0%, P <0.01). Range of Motion. The longitudinal analysis showed a significant increase in pain-free active range of motion (aROM, F(1,35)=6.3, P =0.02, Table 2). Compared to baseline, there were significant increases in aROM at week 8 (47.6%, P <0.01), and week 16 (48.6%, P <0.01). Quality of Life. The PGIC also showed an improvement in quality of life (Minimally Improved, Much Improved, or Very Much Improved) for 80% (8 of 10) at EOT and 62.5% (5 of 8) at week 16 (Figure 3). Pressure-Pain Thresholds. While the PPTs for participants who met the criteria for Global Success of Pain Relief appear to differ when compared to those who did not have successful treatment (Figure 4), there was not a statistically significant difference in the longitudinal analysis at the affected shoulder (F(1,44)=0.1, P =0.7), non-affected shoulder (F(1,44)=0.1, P =0.8), or tibialis anterior (F(1,44)<0.1, P =0.8.) Safety. There were 10 electrodes implanted in 10 participants. Seven participants (70%) developed a granuloma at the electrode site that resolved by the end of the follow-up period. No electrodes fractured during treatment, though 5 (50%) fractured on explantation. No adverse events were experienced as a result of the retained electrodes during the 12-wk follow-up period. No participant experienced an infection at the electrode site.
Table 2.
Outcomes
| Week 0 | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 8 | Week 16 | |
|---|---|---|---|---|---|---|---|---|
| Pain (+/− SE) | 8.2 (1.1) | 7.6 (1.1) | 6.2 (1.1) | 5.1 (1.1) | 5.2 (1.1) | 5.3 (1.1) | 4.9 (1.1) | 4.2 (1.1) |
| Pain Interference (+/− SE) | 5.0 (0.8) | 4.7 (0.8) | 3.9 (0.8) | 3 (0.8) | 2.4 (0.8) | 2.7 (0.8) | 2.0 (0.6) | 2.1 (0.8) |
| DASH (+/− SE) | 48.4 (6.9) | 26.4 (6.9) | 30.3 (6.9) | 22.4 (7.4) | 25.4 (7.4) | |||
| Range of Motion (Degrees, (+/− SE) | 84.6 (14.6) | 116.1 (14.6) | 119.0 (14.6) | 124.9 (15.6) | 125.7 (15.6) |
Abbreviations: SE- Standard Error; DASH- Disabilities of the Arm, Shoulder, Hand Questionnaire
Figure 2.
Worst Pain in the Last Week (0-10), BPI-SF3. Longitudinal analysis revealed a significant changed over time (BPI-SF3, F(1, 66)=12.9, p<0.01). Compared to baseline, there were significant reductions at weeks 4, 5, 8, and 16. Stimulation was provided during time represented by shaded area.
Figure 3.
Patient Global Impression of Change Scale. Participants rated how much their quality of life has changed since the beginning of the study to end of treatment (EOT) and at the end of the follow period (Week 16).
Figure 4.
4a (unaffected shoulder), 4b (affected shoulder), 4c (tibialis anterior). Pressure Pain Thresholds (PPT) of responders (2pt or 30% reduction at end of treatment) compared to non-responders. The period of stimulation is represented by the shaded area.
Discussion
This case-series supports the findings of the prior case-report that PNS may be an effective treatment for SIS. In general, there was a reduction in pain associated with PNS treatment that was maintained for 12 weeks after treatment. The reduction in pain was also accompanied by a reduction in impairment and an improvement in use of the affected arm. These changes may be responsible for the improvement in quality of life documented for most participants. It is notable that the participants in this study were those who did not find sustained relief with a subacromial corticosteroid injection and physical therapy. Such participants have limited options for treatment of their shoulder pain, often being referred for surgery, which has not been shown to result in better outcomes than conservative treatment.8
The mechanism of action of PNS is unknown. The stimulation provided by PNS is different than the electrical stimulation provided by transcutaneous electrical nerve stimulation (TENS), which is thought to improve pain by providing paresthesias in the area of pain.30 No paresthesias are experienced with percutaneous PNS because the insulated electrode allows the electrical current to bypass the cutaneous sensory receptors. There is also no discomfort with the use of percutaneous PNS because the large diameter motor nerves are stimulated at a lower intensity than the small diameter sensory nerves, allowing a comfortable muscle contraction. This is one advantage of percutaneous PNS to surface neuromoscular electrical stimulation (NMES), which is often limited by the discomfort created by the high intensity needed to cause muscle contraction through the skin.31
It is possible that PNS affects chronic pain through central mechanisms. Prior work has shown that chronic pain due to SIS is associated with central sensitization32, 33, an alteration in the function of the central nervous system that can result in hyperalgesia and allodynia due to augmentation of nociceptive pathways in the central nervous system.34–36 In this study, those who experienced successful pain relief also experienced a non-significant increase in PPTs, or a lower sensitivity to pain, at sites remote from the area of stimulation that was more pronounced during the period of stimulation (Figure 4). The differences at EOT in the PPTs, for responders and non-responders, at the affected shoulder of 3.8 kg/cm2 (95% CI 1.0 – 6.6) and at the non-affected shoulder of 3.2 kg/cm2 (95% CI 0.9 – 5.5), are greater than the differences in PPTs for those with chronic SIS and the pain-free population.32 That the changes in PPTs were seen in the non-affected shoulder, an area not near the point of stimulation, suggests that an alteration of a central process was associated with pain relief from PNS.
Treatment of chronic shoulder pain due to SIS with PNS was safe in this sample. Granulomas are a common reaction to an inert foreign body37 and all of those that were experienced in this study resolved within the follow-up period. Those participants who experienced a retained electrode did not have any adverse events as a result during the 12 week follow up period. In our randomized controlled trial of percutaneous PNS for the treatment of hemiplegic shoulder pain, there were no retained electrode related complications after an average follow up period of 18.8 months.38 The rate in this study is higher than studies of PNS in hemiplegic shoulder pain, which range from 0–21.4%.18–20, 39 It’s not clear why the rate of retained electrodes was higher in this study, though it is possible that a difference exists between the granulation tissue that forms around the electrode in the able-bodied, who likely use their shoulder to a greater extent than those with hemiplegia, or the greater activity may weaken the electrode and increase the likelihood of fracture. Subjects with retained electrodes will continue to be monitored per routine clinical care.
There are limitations to this study. First, this is a case-series without a control group to which the outcomes of the treatment group can be compared. It is possible that the improvement was a placebo response or natural recovery, though natural recovery seems less likely given that the average duration of shoulder pain in this study was 4.3 years (+/− SD 5.6 years). There is also a limitation due to the lack of accounting for daily analgesic consumption, which could affect the outcomes measured in this study. There is a limitation in the inference that can be made about the mechanism of action of PNS treatment due to lack of outcome measures to show whether any anatomical changes at the shoulder occurred in association with successful treatment. It is also notable that this study included a relatively short follow-up period for a chronic pain condition where long-term pain relief is an important outcome. Unfortunately, the level of funding that was obtained for this study did not allow a longer follow-up period, though we plan to increase the duration of follow-up in future studies. It is also possible that all subjects who continued to have pain after the 3-week treatment period would respond more favorably to a longer period of stimulation, whether on the order of weeks or with a fully implanted PNS system, though this possibility was not explored in this trial. Finally, due to the small sample size, it is possible that the differences in PPTs between subgroups are spurious, though the patterns were consistent across multiple measurements.
Conclusion
Peripheral nerve stimulation may be an efficacious treatment for chronic shoulder pain due to SIS. Treatment with percutaneous PNS is also associated with reduced shoulder disability, reduced pain interference, improved range of motion, and improved quality of life. Treatment with PNS is safe, and may be a new treatment for those with chronic SIS. A blinded randomized controlled trial is the next step in the continued development and evaluation of this treatment modality for chronic shoulder pain due to SIS.
Acknowledgments
AUTHORSHIP STATEMENT: Drs. Wilson, Harris, Gunzler, Chae, and Mrs. Bennett designed and conducted the study, including patient recruitment, data collection, and data analysis. Dr. Wilson prepared the manuscript draft with important intellectual input from Drs. Harris, Gunzler, Chae, and Mrs. Bennett. All authors approved the final manuscript. This publication was, in part, made possible by the Case Western Reserve University/Cleveland Clinic CTSA Grant Number UL1 RR024989 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health and NIH roadmap for Medical Research. Secure data storage was made possible through grants M01 RR00080 and UL1 RR024989 from NCRR/NIH. Funding was also provided, in part, by SPR Therapeutics, LLC.
Footnotes
CONFLICT OF INTEREST:
Richard D. Wilson is a consultant to SPR Therapeutics, LLC. Maria Bennett is an employee of and owns equity in SPR Therapeutics, LLC. John Chae is a consultant and Chief Medical Advisor to SPR Therapeutics, LLC. Dr. Chae owns equity in SPR Therapeutics, LLC.
Dr. Chae and Mrs. Bennett are patent holders for intramuscular peripheral nerve stimulation for the treatment of chronic pain. SPR Therapeutics, LLC. has a commercial interest in the device presented in this manuscript.
References
- 1.Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57(11):649–655. doi: 10.1136/ard.57.11.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson MP, Crossley KL, O'neil ME, Al-Zakwani IS. Estimates of Direct Health Care Expenditures Among Individuals With Shoulder Dysfunction in the United States. J Ortho Sports Phys Ther. 2005;35(1,A4) [Google Scholar]
- 3.Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81. doi: 10.1080/03009740310004667. [DOI] [PubMed] [Google Scholar]
- 4.van der Windt DA, Koes BW, de Jong BA, Boulter LM. Shoulder disorders in general practice: incidence, patient characteristics and management. Ann Rheum Dis. 1995;54(12):959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Heijden GJ. Shoulder disorders: a state-of-the-art review. Baillieres Clin Rheumatol. 1999;13(2):287–309. [PubMed] [Google Scholar]
- 6.Codsi MJ. The painful shoulder: when to inject and when to refer. Cleve Clin J Med. 2007;74(7):473–474. 7–8, 80–82 passim. doi: 10.3949/ccjm.74.7.473. [DOI] [PubMed] [Google Scholar]
- 7.Cummins CA, Sasso LM, Nicholson D. Impingement syndrome: temporal outcomes of nonoperative treatment. J Shoulder Elbow Surg. 2009;18(2):172–177. doi: 10.1016/j.jse.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg. 2009;18(4):652–660. doi: 10.1016/j.jse.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg Br. 2009;91(10):1326–1334. doi: 10.1302/0301-620X.91B10.22094. [DOI] [PubMed] [Google Scholar]
- 10.Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4–8-years' follow-up in a prospective, randomized study. Scand J Rheumatol. 2006;35(3):224–228. doi: 10.1080/03009740600556167. [DOI] [PubMed] [Google Scholar]
- 11.Haahr JP, Ostergaard S, Dalsgaard J, Norup K, Frost P, Lausen S, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis. 2005;64(5):760–764. doi: 10.1136/ard.2004.021188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson RD, Harris MA, Bennett ME, Chae J. Single-lead percutaneous peripheral nerve stimulation for the treatment of shoulder pain from subacromial impingement syndrome. Pm R. 2012;4(8):624–628. doi: 10.1016/j.pmrj.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 15.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50. [PubMed] [Google Scholar]
- 16.Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty's Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O'Brien for the Guarantors of Brain. Saunders Elsevier:: 2010; pp,. [8] 64 and 94 Figures. Brain. 2010;133(10):2838–2844. doi: 10.1093/brain/awq270. [DOI] [PubMed] [Google Scholar]
- 17.Beck AT, Steer RA, Brown GK. BDI-FastScreen for medical patients: Manual. San Antonio, TX: The Psychological Corporation; 2000. [Google Scholar]
- 18.Yu DT, Chae J, Walker ME, Kirsteins A, Elovic EP, Flanagan SR, et al. Intramuscular neuromuscular electrical stimulation for post-stroke shoulder pain: A multi-center randomized clinical trial. Arch Phys Med Rehabil. 2004;85:695–704. doi: 10.1016/j.apmr.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Chae J, Wilson RD, Bennett ME, Lechman TE, Stager KW. Single-lead percutaneous peripheral nerve stimulation for the treatment of hemiplegic shoulder pain: a case series. Pain practice. 2013;13(1):59–67. doi: 10.1111/j.1533-2500.2012.00541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson RD, Gunzler DD, Bennett ME, Chae J. Intramuscular Peripheral Nerve Stimulation compared to Usual Care for Pain Relief of Hemiplegic Shoulder Pain: A Randomized Controlled Trial. Am J Phys Med Rehabil. doi: 10.1097/PHM.0000000000000011. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 22.Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–146. [PubMed] [Google Scholar]
- 23.Kitis A, Celik E, Aslan UB, Zencir M. DASH questionnaire for the analysis of musculoskeletal symptoms in industry workers: a validity and reliability study. Appl Ergon. 2009;40(2):251–255. doi: 10.1016/j.apergo.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47(4):289–294. doi: 10.1016/s0004-9514(14)60274-9. [DOI] [PubMed] [Google Scholar]
- 25.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 26.Vanderweeen L, Oostendorp RA, Vaes P, Duquet W. Pressure algometry in manual therapy. Man Ther. 1996;1(5):258–265. doi: 10.1054/math.1996.0276. [DOI] [PubMed] [Google Scholar]
- 27.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Chesterton LS, Barlas P, Foster NE, Baxter GD, Wright CC. Gender differences in pressure pain threshold in healthy humans. Pain. 2003;101(3):259–266. doi: 10.1016/S0304-3959(02)00330-5. [DOI] [PubMed] [Google Scholar]
- 30.Melzack R. Prolonged relief of pain by brief, intense transcutaneous somatic stimulation. Pain. 1975;1(4):357–373. doi: 10.1016/0304-3959(75)90073-1. [DOI] [PubMed] [Google Scholar]
- 31.Yu DT, Chae J, Walker ME, Hart RL, Petroski GF. Comparing stimulation-induced pain during percutaneous (intramuscular) and transcutaneous neuromuscular electric stimulation for treating shoulder subluxation in hemiplegia. Arch Phys Med Rehabil. 2001;82(6):756–760. doi: 10.1053/apmr.2001.23310. [DOI] [PubMed] [Google Scholar]
- 32.Paul TM, Soo Hoo J, Chae J, Wilson RD. Central hypersensitivity in patients with subacromial impingement syndrome. Arch Phys Med Rehabil. 2012;93(12):2206–2209. doi: 10.1016/j.apmr.2012.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hidalgo-Lozano A, Fernandez-de-las-Penas C, Alonso-Blanco C, Ge HY, Arendt-Nielsen L, Arroyo-Morales M. Muscle trigger points and pressure pain hyperalgesia in the shoulder muscles in patients with unilateral shoulder impingement: a blinded, controlled study. Exp Brain Res. 2010;202(4):915–925. doi: 10.1007/s00221-010-2196-4. [DOI] [PubMed] [Google Scholar]
- 34.Petersen-Felix S, Curatolo M. Neuroplasticity--an important factor in acute and chronic pain. Swiss Med Wkly. 2002;132(21–22):273–278. doi: 10.4414/smw.2002.09913. [DOI] [PubMed] [Google Scholar]
- 35.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Curatolo M, Arendt-Nielsen L, Petersen-Felix S. Central hypersensitivity in chronic pain: mechanisms and clinical implications. Phys Med Rehabil Clin N Am. 2006;17(2):287–302. doi: 10.1016/j.pmr.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Cotran RS, Kumar V, Collins T, Robbins SL. Robbins pathologic basis of disease. 6th ed. Philadelphia: Saunders; 1999. [Google Scholar]
- 38.Chae J, Yu DT, Walker ME, Kirsteins A, Elovic EP, Flanagan SR, et al. Intramuscular electrical stimulation for hemiplegic shoulder pain: a 12-month follow-up of a multiple-center, randomized clinical trial. Am J Phys Med Rehabil. 2005;84(11):832–842. doi: 10.1097/01.phm.0000184154.01880.72. [DOI] [PubMed] [Google Scholar]
- 39.Renzenbrink GJ, Ijzerman M. Percutaneous neuromuscular electrical stimulation (P-NMES) for treating shoulder pain in chronic hemiplegia. Effects on shoulder pain and quality of life. Clin Rehabil. 2004;18(4):359–365. doi: 10.1191/0269215504cr759oa. [DOI] [PubMed] [Google Scholar]