Abstract
Patients with sarcoidosis have a high risk of development of malignant lymphoma, and this association was coined the term “sarcoidosis-lymphoma syndrome”. Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) is a distinct clinicopathological entity, and the stomach is the most common site. The occurrence of this type of lymphoma in the esophagus is extremely rare. In this report, we describe the first documented case of sarcoidal granulomas in the mediastinal lymph nodes after treatment for MALT lymphoma of the esophagus. A 60-year-old Japanese female was found to have a submucosal tumor in the esophagus. Histopathological study revealed proliferation of small- to medium-sized lymphoid cells with convoluted nuclei, and immunohistochemically, these lymphoid cells were diffusely positive for CD20, bcl-2, and MUM1. R-CHOP therapy was performed, which led to tumor remission. Two years later, swelling of the mediastinal lymph nodes was detected. Histopathological study of the lymph nodes revealed presence of variably-sized epithelioid granulomas without caseating necrosis but no malignant lymphoma was noted. Sarcoidal granulomas can be observed in patients with malignant tumors including malignant lymphoma and carcinoma without history of systemic sarcoidosis. It is important to recognize that systemic sarcoidosis and sarcoidal reaction without evidence of systemic disease can occur after development of malignant lymphoma, therefore, sarcoidal reaction must be included in the differential diagnostic consideration of recurrent malignant lymphoma.
Keywords: Sarcoidosis, marginal zone lymphoma, sarcoidosis-lymphoma syndrome, esophagus
Introduction
Sarcoidosis is a chronic systemic inflammatory disorder of unknown etiology, which is characterized histopathologically by the presence of non-caseating epithelioid granulomas, and involves multiple organs including the lung, lymph node, eye, and skin [1]. Some reports demonstrated that patients with sarcoidosis had a high risk of development of malignant lymphoma [2-4]. Brincker first pointed out this association, and coined the term “sarcoidosis-lymphoma syndrome” [2]. The most common subtype of malignant lymphoma associated with sarcoidosis is Hodgkin lymphoma, but diffuse large B-cell lymphoma, follicular lymphoma, and multiple myeloma may also be involved in sarcoidosis-lymphoma syndrome [2,5].
Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) is a distinct clinicopathological entity of low-grade malignant B-cell lymphoma, and comprises of 7-8% of all B-cell lymphomas [6]. The stomach is the most common site of this type of lymphoma, followed by the small intestine, salivary gland, lung, and ocular adnexa [6]. Occurrence of MALT lymphoma in the esophagus is extremely rare, and less than 20 cases have been reported in the English literature [7-11]. Development of MALT lymphoma have only been documented in four patients with sarcoidosis (the primary sites were skin, kidney, stomach, and conjunctiva) in the English literature [12-15].
In this report, we describe the first documented case of development of sarcoidal granulomas in the mediastinal lymph nodes after treatment for MALT lymphoma of the esophagus and review the clinicopathological features of sarcoidosis-lymphoma syndrome.
Case report
A 60-year-Japanese female without history of any autoimmune diseases including sarcoidosis was found to have a submucosal tumor, measuring 50 x 20 x 5 mm, in the lower esophagus, which was located 39-44 cm from the incision (Figure 1). Biopsy from the tumor was performed, which led to an ultimate diagnosis of MALT lymphoma of the esophagus because systemic surveillance failed to detect other tumorous lesions or swelling of the lymph nodes. Eradication of Helicobacter pylori was performed, however, the tumor did not decrease in size. Thus, six courses of R-CHOP therapy were performed, which led to complete tumor remission.
Figure 1.
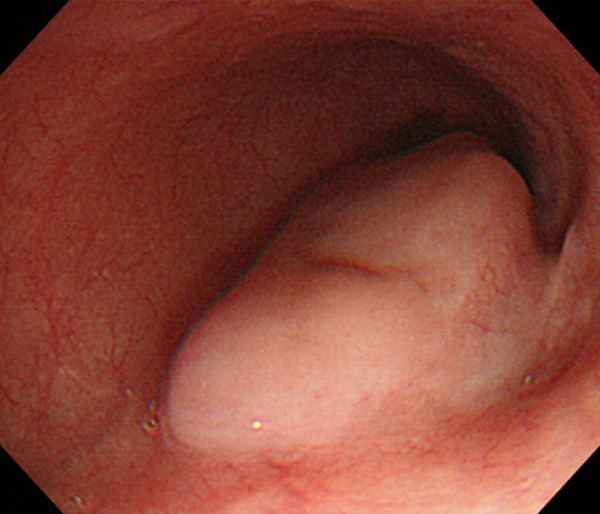
Endoscopic examination showing a submucosal tumor in the esophagus.
Two years after the detection of the esophageal lesion, the patient was found to have swelling in multiple mediastinal lymph node by follow-up computed tomography (Figure 2), and hypermetabolic lesions were shown by positron emission tomography. Biopsy of the mediastinal lymph nodes was performed by medianoscopy under a clinical diagnosis of recurrence of malignant lymphoma.
Figure 2.
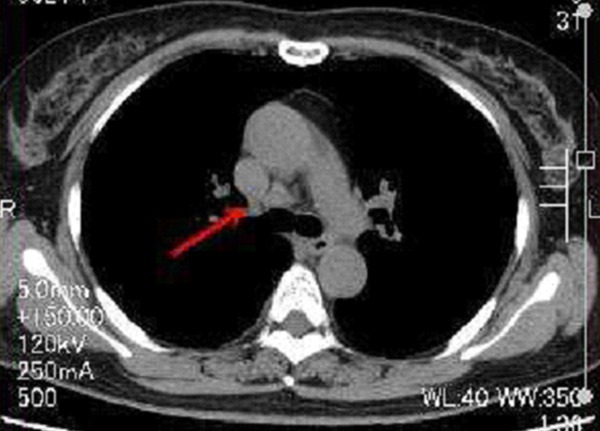
Computed tomography demonstrating swelling of the mediastinal lymph nodes (arrow).
Histopathological study of the biopsy specimens of the submucosal tumor of the esophagus revealed diffuse proliferation of small- to medium-sized lymphocytes containing convoluted nuclei and inconspicuous nucleoli (Figure 3A). Some of them had clear cytoplasm (Figure 3A). No lymphoid follicle formation was noted, and plasma cell infiltration was hardly detected. Proliferation of large-sized lymphocytes was not observed.
Figure 3.
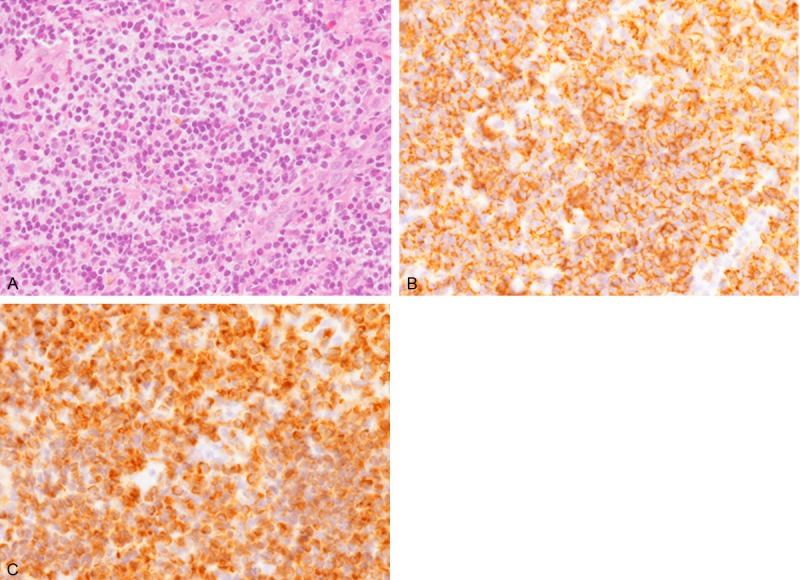
Histopathological and immunohistochemical features of the submucosal tumor of the esophagus. A. Diffuse proliferation of small- to medium-sized lymphocytes with convoluted nuclei and inconspicuous nucleoli. Some of them have clear cytoplasm. HE, x 400. B. CD20 is diffusely expressed in these lymphocytes x 400. C. Bcl-2 is also diffusely expressed x 400.
Immunohistochemical studies were performed using an autostainer (Ventana) by the same method as previously reported [16-20]. These lymphoid cells were diffusely positive for CD20, bcl-2, and MUM1 (Figure 3B, 3C), but negative for CD3, CD5, CD10, bcl-6, and cyclin D1.
Accordingly, an ultimate diagnosis of MALT lymphoma of the esophagus was made.
Histopathological study of the mediastinal lymph node revealed presence of variably-sized epithelioid granulomas without caseating necrosis (Figure 4A, 4B). Multinucleated giant cells were also noted (Figure 4B). However, malignant lymphoma was not observed.
Figure 4.
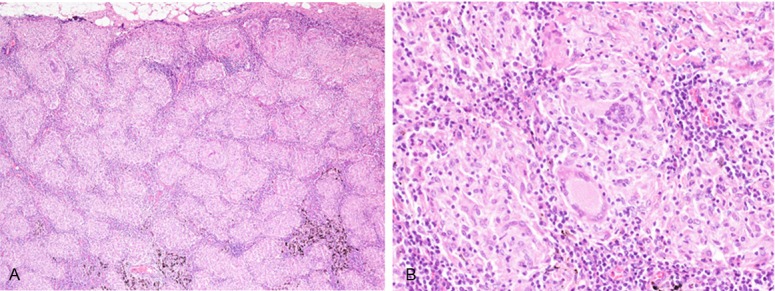
Histopathological features of the mediastinal lymph nodes. A. Variaby-sized epithelioid granulomas without caseating necrosis in the lymph node. HE, x 40. B. Multinucleated giant cells are also observed. HE, x 100.
Therefore, a diagnosis of sarcoidal granulomas in the lymph node after treatment for MALT lymphoma of the esophagus was made.
Discussion
Sarcoidal (non-caseating epithelioid) granuloma can be observed in various sites in patients with malignant tumors without history of systemic sarcoidosis [21-26]. It is well recognized that Hodgkin lymphoma occasionally accompany sarcoidal granulomas, and non-Hodgkin lymphoma can also have sarcoidal granulomas within the lesion [21,25,26]. Albeit relatively rare, this change can occur in patients with carcinoma, which may be due to tumor-related immunoreaction, but not indicative of systemic sarcoidosis [21]. Brincker reported that sarcoidal reaction occur in 4.4% of carcinoma cases, even in the non-regional tissues, and concluded that sarcoidal reaction may be so extensive on occasion that it complicates the diagnosis of the underlying malignant disease. Moreover, distinguishing between tumor-related sarcoidal reaction and true systemic sarcoidosis may be problematic [21].
Sarcoidosis-lymphoma syndrome was first proposed by Brincker as shown by the evidence that patients with sarcoidosis have a high incidence of development of malignant lymphoma [2]. He reported and summarized the largest series of lymphoproliferative diseases (including malignant lymphoma, multiple myeloma, and leukemia) with sarcoidosis [2]. According to his analysis of 65 cases, the occurrence of lymphoproliferative disease was observed after the diagnosis of sarcoidosis in most cases (94%). Therefore, he speculated that early presentation of sarcoidosis represents a paraneoplastic syndrome [2]. However, only a few cases of lymphoproliferative disease occurred before sarcoidosis (2 cases were Hodgkin lymphoma, 1 case was non-Hodgkin lymphoma, and the remaining case was acute lymphocytic leukemia) [2].
Table 1 summarizes the clinicopathological features of the previously reported cases of MALT lymphoma with sarcoidosis as well as the present one [12-15]. Females are commonly affected, and the original site of MALT lymphoma is variable. In four of five cases, sarcoidosis was present before the occurrence of MALT lymphoma [12-15]. The present case is unique because sarcoidal granulomas were observed in the mediastinal lymph nodes 2 years after treatment for MALT lymphoma of the esophagus. Therefore, it is important to recognize that systemic sarcoidosis and sarcoidal reaction without evidence of systemic disease can occur after development of malignant lymphoma; therefore, sarcoidal reaction must be included in the differential diagnostic consideration of recurrent malignant lymphoma.
Table 1.
Clinicopathological features of MALT lymphoma with sarcoidal granulomas
| Case No. | Age | Gender | Site of MM | Order of the lesions | Reference |
|---|---|---|---|---|---|
| 46 | Female | Skin | Sarcoidosis → MM | [12] | |
| 2 | 53 | Female | Kidney | Sarcoidosis → MM | [13] |
| 3 | 23 | Male | Stomach | Sarcoidosis → MM | [14] |
| 4 | 59 | Female | Conjunctiva | Sarcoidosis → MM | [15] |
| Present Case | 60 | Female | Esophagus | MM → Sarcoidosis |
MM, Malignant lymphoma.
Albeit rare, MALT lymphoma can occur in the esophagus. Jung et al. summarized the clinicopathological features of this type of malignant lymphoma [8]. This disease affects middle-aged individuals, and males and females are at equal risk [8]. No standard treatment has not been established yet. Chemotherapy (R-CHOP) or radiation therapy was performed in most cases, and endoscopic or surgical resection was performed in some cases [8]. The vast majority of MALT lymphoma of the esophagus cases was found to have low-malignant potential, as seen in the present case [8].
In conclusion, we describe the first documented case of occurrence of sarcoidal granulomas in the mediastinal lymph nodes after treatment for MALT lymphoma of the esophagus. Sarcoidosis is thought to be associated with the occurrence of malignant lymphoma, and in most cases, sarcoidosis is present before development of malignant lymphoma. Albeit rare, sarcoidal granulomas can be seen after occurrence of malignant lymphoma including MALT lymphoma. Therefore, it is important to include this condition in the differential diagnostic consideration of recurrent malignant lymphoma.
Disclosure of conflict of interest
None.
References
- 1.Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. New Engl J Med. 2007;357:2153–2165. doi: 10.1056/NEJMra071714. [DOI] [PubMed] [Google Scholar]
- 2.Brincker H. Coexistence of sarcoidosis and malignant disease: causality or coincidence? Sarcoidosis. 1989;6:31–43. [PubMed] [Google Scholar]
- 3.Mellemkjaer L, Pfeiffer RM, Engels EA, Gridley G, Wheeler W, Hemminki K, Olsen JH, Dreyer L, Linet MS, Goldin LR, Landgren O. Autoimmune disease in individuals and close family members and susceptibility to non-Hodgkin lymphoma. Arthritis Rheum. 2008;58:657–666. doi: 10.1002/art.23267. [DOI] [PubMed] [Google Scholar]
- 4.Reich JM, Mullooly JP, Johnson RE. Linkage analysis of malignancy-associated sarcoidosis. Chest. 1995;107:605–613. doi: 10.1378/chest.107.3.605. [DOI] [PubMed] [Google Scholar]
- 5.Goswami T, Siddique S, Cohen P, Cheson BD. The sarcoid-lymphoma syndrome. Clin Lymphoma Myeloma Leuk. 2010;10:241–247. doi: 10.3816/CLML.2010.n.052. [DOI] [PubMed] [Google Scholar]
- 6.Isaacson PG, Chott A, Nakamura S, Muller-Hermelink HK, Harris NL, Swerdlow SH. Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC Press; 2008. pp. 214–217. [Google Scholar]
- 7.Tsujii Y, Nishida T, Kato M, Inoue T, Yamamoto S, Hayashi Y, Akasaka T, Kondo J, Yamada T, Shinzaki S, Iijima H, Tsujii M, Takehara T. Mucosa-associated lymphoid tissue (MALT) lymphoma of the esophagus. Dis Esophagus. 2013;26:349–350. doi: 10.1111/j.1442-2050.2012.01387.x. [DOI] [PubMed] [Google Scholar]
- 8.Jung JG, Kang HW, Hahn SJ, Choi JS, Kim EJ. Primary mucosa-associated lymphoid tissue lymphoma of the esophagus, manifesting as a submucosal tumor. Korean J Gastroenterol. 2013;62:117–121. doi: 10.4166/kjg.2013.62.2.117. [DOI] [PubMed] [Google Scholar]
- 9.Kishi K, Maeda H, Nakamura Y, Shirai S, Sato M. Radiotherapy for mucosa-associated lymphoid tissue (MALT) lymphoma of the esophagus: a case report with a diagnostic and therapeutic discussion. Int J Clin Oncol. 2012;17:174–180. doi: 10.1007/s10147-011-0265-8. [DOI] [PubMed] [Google Scholar]
- 10.Chung JJ, Kim MJ, Kie JH, Kim KW. Mucosa-associated lymphoid tissue lymphoma of the esophagus coexistent with bronchus-associated lymphoid tissue lymphoma of the lung. Yonsei Med J. 2005;46:562–566. doi: 10.3349/ymj.2005.46.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miyazaki T, Kato H, Masuda N, Nakajima M, Manda R, Fukuchi M, Tsukada K, Kojima M, Nakajima T, Kuwano H. Mucosa-associated lymphoid tissue lymphoma of the esophagus: case report and review of the literature. Hepatogastroenterology. 2004;51:750–753. [PubMed] [Google Scholar]
- 12.Sharma OP. Sarcoidosis and B-cell MALT lymphoma. Sarcoidosis Vasc Diffuse Lung Dis. 2002;19:235. [PubMed] [Google Scholar]
- 13.Qiu L, Unger PD, Dillon RW, Strauchen JA. Low-grade mucosa-associated lymphoid tissue lymphoma involving the kidney: report of 3 cases and review of the literature. Arch Pathol Lab Med. 2006;130:86–89. doi: 10.5858/2006-130-86-LMLTLI. [DOI] [PubMed] [Google Scholar]
- 14.Fukuda T, Sato K, Tachikawa S, Ohnuki K, Ohtani H, Suzuki T. Mucosa-associated lymphoid tissue lymphoma coexisting with epithelioid granulomas in the stomach of a patient with systemic sarcoidosis. Pathol Int. 1997;47:870–875. doi: 10.1111/j.1440-1827.1997.tb03720.x. [DOI] [PubMed] [Google Scholar]
- 15.Cauvain A, Delmer A, Godeau MJ, Molina T, Durdux C, Marinho E, Crickx B, Descamps V. MALT (mucosal associated lymphoid tissue) lymphoma of the palpebral conjunctiva. Ann Dermatol Venereol. 2006;133:168–170. doi: 10.1016/s0151-9638(06)70871-7. [DOI] [PubMed] [Google Scholar]
- 16.Ishida M, Hodohara K, Okuno H, Yoshii M, Horinouchi A, Shirakawa A, Harada A, Iwai M, Yoshida K, Kagotani A, Yoshida T, Okabe H. IgD plasmablastic myeloma: a case report with emphasis on the cytological features. Int J Clin Exp Pathol. 2014;7:1250–1254. [PMC free article] [PubMed] [Google Scholar]
- 17.Ishida M, Hodohara K, Furuya A, Fujishiro A, Okuno H, Yoshii M, Horinouchi A, Shirakawa A, Harada A, Iwai M, Yoshida K, Kagotani A, Yoshida T, Okabe H. Concomitant occurrence of IgG4-related pleuritis and periaortitis: a case report with review of the literature. Int J Clin Exp Pathol. 2014;7:808–814. [PMC free article] [PubMed] [Google Scholar]
- 18.Ishida M, Iwai M, Yoshida K, Kagotani A, Yoshida T, Okabe H. Rhabdoid melanoma: a case report with review of the literature. Int J Clin Exp Pathol. 2014;7:840–843. [PMC free article] [PubMed] [Google Scholar]
- 19.Ishida M, Iwai M, Yoshida K, Kagotani A, Okabe H. Sebaceous carcinoma associated with Bowen’s disease: a case report with emphasis on the pathogenesis of sebaceous carcinoma. Int J Clin Exp Pathol. 2013;6:3029–3032. [PMC free article] [PubMed] [Google Scholar]
- 20.Ishida M, Iwai M, Yoshida K, Kagotani A, Okabe H. Ectopic respiratory mucosa in the rectum: the second documented case with discussion of its histogenesis. Int J Clin Exp Pathol. 2014;7:1819–1822. [PMC free article] [PubMed] [Google Scholar]
- 21.Brincker H. Sarcoid reactions in malignant tumours. Cancer Treat Rev. 1986;13:147–156. doi: 10.1016/0305-7372(86)90002-2. [DOI] [PubMed] [Google Scholar]
- 22.Bässler R, Birke F. Histopathology of tumour associated sarcoid-like stromal reaction in breast cancer. An analysis of 5 cases with immunohistochemical investigations. Virchows Arch A Pathol Anat Histopathol. 1988;412:231–239. doi: 10.1007/BF00737147. [DOI] [PubMed] [Google Scholar]
- 23.Kojima M, Nakamura S, Fujisaki M, Hirahata S, Hasegawa H, Maeda D, Suito T, Motoori T, Joshita T, Suzuki K, Suchi T. Sarcoid-like reaction in the regional lymph nodes and spleen in gastric carcinoma: a clinicopathologic study of five cases. Gen Diagn Pathol. 1997;142:347–352. [PubMed] [Google Scholar]
- 24.Kurata A, Terado Y, Schulz A, Fujioka Y, Franke FE. Inflammatory cells in the formation of tumor-related sarcoid reactions. Hum Pathol. 2005;36:546–554. doi: 10.1016/j.humpath.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 25.Ishida M, Okabe H. Reactive lymphoid follicles with germinal centers in granulomatous mycosis fungoides: a case report with review of the literature. J Cutan Pathol. 2013;40:284–285. doi: 10.1111/cup.12012. [DOI] [PubMed] [Google Scholar]
- 26.Ishida M, Hotta M, Takikita-Suzuki M, Kojima F, Okabe H. CD8-positive granulomatous mycosis fungoides: a case report with review of the literature. J Cutan Pathol. 2010;37:1072–1076. doi: 10.1111/j.1600-0560.2010.01577.x. [DOI] [PubMed] [Google Scholar]


