Abstract
The study was designed to assess the relationship between glomerular filtration rate (GFR) and urinary stone-forming constituents, and to assess the effect of renal insufficiency on stone recurrence risk in first stone formers (SF). Baseline serum creatinine levels were obtained, and renal insufficiency was defined as creatinine clearance ≤60 mL/min (Cockroft-Gault). This retrospective case-control study consists of 342 first SF; 171 SF with normal renal function were selected with 1:1 propensity scores matched to 171 SF with renal insufficiency. Urinary metabolic evaluation was compared to renal function. GFR was positively correlated with urinary calcium, uric acid, and citrate excretion. Subjects with renal insufficiency had significantly lower urinary calcium, uric acid, and citrate excretion than those with normal renal function, but not urine volume. With regard to urinary metabolic abnormalities, similar results were obtained. SF with renal insufficiency had lower calcium oxalate supersaturation indexes and stone recurrence rates than SF with normal renal function. Kaplan-Meier curves showed similar results. In conclusion, GFR correlates positively with urinary excretion of stone-forming constituents in SF. This finding implies that renal insufficiency is not a risk factor for stone recurrence.
Graphical Abstract
Keywords: Urinary Calculi, Recurrence, Renal Insufficiency, Creatinine
INTRODUCTION
Urolithiasis is one of the most common diseases, with increasing incidence and prevalence worldwide (1, 2). It is painful and costly, requiring hospitalizations, interventions and absence from work, and imposes a major economic burden (3, 4, 5). Urolithiasis may be associated with various degrees of renal insufficiency (6, 7, 8). Frequent stone recurrence, combined with urinary tract infection and obstruction, and frequent urological interventions are responsible for loss of renal function (9). Moreover, percutaneous and extracorporeal urological methods for the treatment of renal stones may also lead to chronic deterioration of renal function (10, 11). A study described that the glomerular filtration rate (GFR) falls in chronic renal disease patients, and that increased fractional excretion of uric acid, calcium, phosphorus, and magnesium is observed (12). These findings suggest the existence of a vicious cycle between renal function impairment and urolithiasis, such that the presence of one condition predisposes the patient to the other. This may cause psychological stress to patients and physicians concerned about progressive renal function deterioration and recurrent stone episodes. By contrast, another study showed that lower eGFR correlated with lower urine pH, lower calcium excretion, and greater oxalate excretion. Unfortunately, there are sparse data on the association between renal function and urinary excretion of stone-forming constituents (13). Moreover, no clinical data were published in the literature on the impact of chronic kidney disease on the development of kidney stones. It is our hypothesis that the renal function of patients with urolithiasis may portend unique aberrations in urine physicochemistry and stone risk. To our knowledge, this is the first study designed to evaluate the effect of renal insufficiency on stone recurrence in patients with urolithiasis.
This study assessed the relationship between glomerular filtration rates and urinary excretion of stone-forming constituents, and observed the effect of renal insufficiency on stone recurrence in patients with urolithiasis.
MATERIALS AND METHODS
Patient characteristics and data collection
We retrospectively reviewed the medical records of 1,692 stone-forming patients who visited the urological office of our institution between January 2007 and December 2011. Of the 1,692 consecutive stone formers (SF), patients with staghorn calculi (n=33), recurrent stone episode (n=430), urinary tract obstruction (n=27), single kidney (n=12), or congenital urological anomaly (n=19) were excluded from the study. Patients with end-stage renal disease undergoing regular dialysis were also excluded (n=9). As a result, 1,195 subjects satisfied the inclusion criteria (there is some overlap in categories).
Baseline serum creatinine levels were obtained in all patients and renal insufficiency was defined as creatinine clearance≤60 mL/min per 1.73 m2 (Cockroft-Gault), a cut-off value previously proposed by the National Foundation's Kidney Disease Outcome Quality Initiative Advisory Board (14). Almost 14.3% of the patients (n=171) had renal insufficiency based on estimated GFR and were stratified into case groups; of the remaining subjects with normal renal function (n=1,024), 171 controls were matched to these 171 renal insufficiency patients by propensity score analysis (171 cases and 171 controls).
Measurement and definition of parameters
Creatinine levels were used to calculate baseline creatinine clearance according to the formula proposed by Cockcroft and Gault. Creatinine clearance was corrected by a factor of 0.85 for women to account for differences in lean body mass (15). Metabolic evaluation was conducted at least 4 weeks after the last stone episode. All SF were instructed to follow a general recommended diet, such as low salt, low animal protein, and high fluid, and none were placed on a low-calcium diet. Urinary stone risk was evaluated in urine on the basis of the following parameters: sodium (ion-selective electrode method), calcium (ocresolphthalein complex), uric acid (uricase colorimetry method), oxalate (oxalate oxidase method), citrate (citrate lyase method), and magnesium (xylidyl blue method). Urinary metabolic abnormalities were classified using the definitions of Lifshitz et al. (16). Calcium oxalate supersaturation was estimated using the AP (CaOx) index EQ (Tiselius) and pKCaOx values (Ogawa) (17, 18). Stone recurrence was defined as the radiographic appearance of stones that were not present on the previous examination. The time between the previous and new stone-detecting examination was defined as the time to stone recurrence.
Statistical analysis
We used propensity score methods to balance the observed covariates between the case and control groups. Propensity scores were calculated for each patient using multivariable logistic regression based upon the covariates: age, gender, and BMI. Matching was performed using the R package matching. Results were expressed as means±standard deviations. The differences in urine variables between groups were assessed by Mann-Whitney U-test. Categorical variables were compared by chi-square test or Fisher's exact test if appropriate. The correlation between eGFR and urinary constituents was assessed by partial correlation analysis adjusted for age, sex, and BMI. The impact of renal insufficiency on metabolic abnormalities was studied by logistic regression analysis. The Kaplan-Meier method was used to estimate recurrence-free survival, and differences were assessed using log-rank statistics. All statistical analyses were performed using the SPSS® 20.0 software. All tests were performed with 2-tailed analyses and P<0.05 was considered statistically significant.
Ethics statement
The institutional review board of Chungbuk National University Hospital reviewed and approved this study protocol (IRB approval number 2006-01-001). Written informed consent was obtained from each subject.
RESULTS
Baseline characteristics
The baseline characteristics of the study population are presented in Table 1. The mean age, BMI distribution, and gender differences between SF with renal insufficiency and SF with normal renal function were not significant.
Table 1.
Baseline characteristics
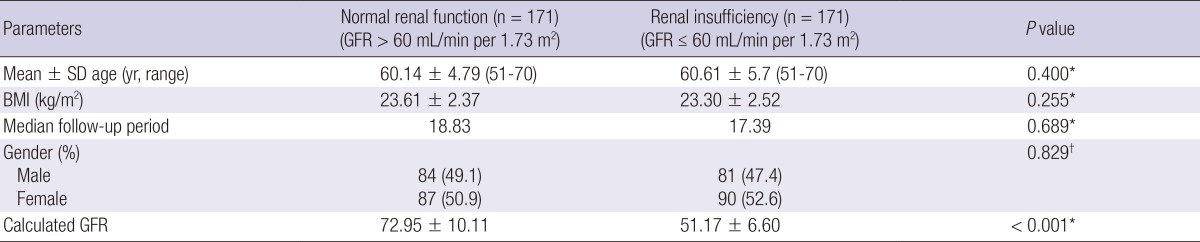
P values are based on the *Mann-Whitney U-test and †Fisher's exact test. BMI, body mass index; GFR, glomerular filtration rate.
Correlation between creatinine clearance and urinary variables
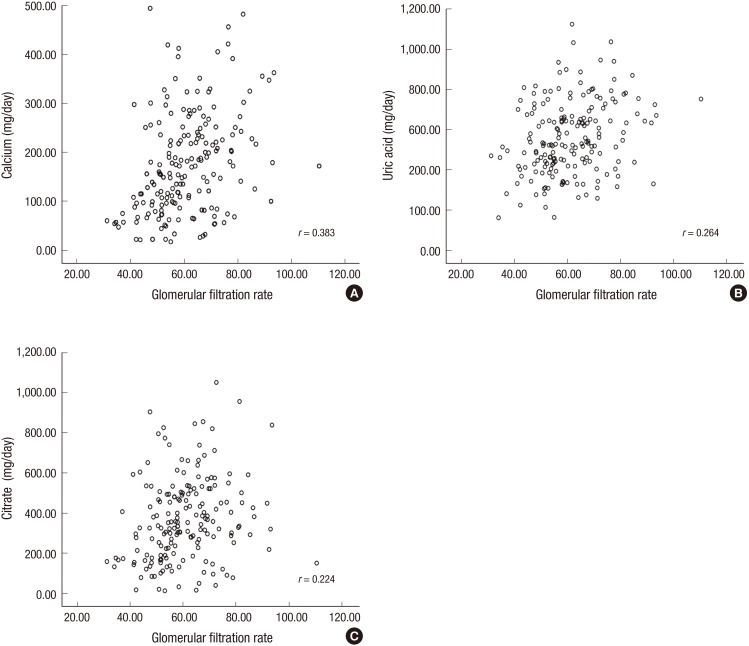
After adjusting for age, sex, and BMI, the estimated GFR correlated positively with urinary calcium (r=0.383, P<0.001), uric acid (r=0.264, P<0.001), and citrate (r=0.224, P=0.003) (Table 2 and Fig. 1).
Table 2.
Correlation between estimated GFR and 24-hr urine constituents in the entire study population
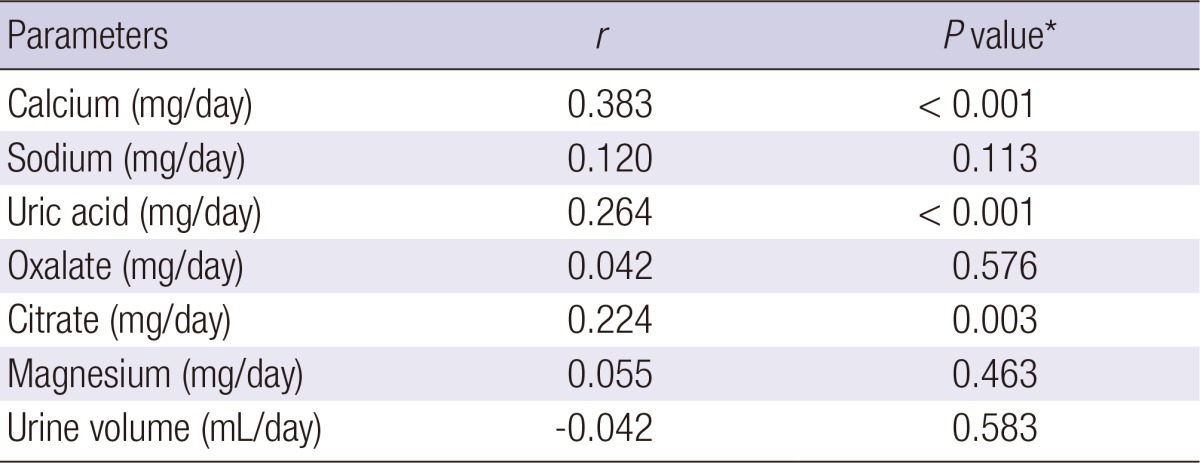
*P values are based on partial correlation analysis. r, partial correlation coefficient adjusted by age, sex, and BMI.
Fig. 1.
Correlation between estimated GFR and 24-hr urine constituents in the entire study population. (A) Calcium (P < 0.001), (B) Uric acid (P < 0.001), (C) Citrate (P = 0.003). r, partial correlation coefficient adjusted by age, sex and BMI.
Comparison between the control and renal insufficiency groups in terms of urinary variables and urinary metabolic abnormalities
There was no significant difference in 24-hr urine volume between SF with renal insufficiency (1,788.27±772.98) and SF with normal renal function (1,847. 69±785.04) (P=0.486). Urinary excretion of calcium, uric acid, and citrate was significantly different according to the presence of renal insufficiency (P<0.001, P=0.001, and P=0.001, respectively). SF with renal insufficiency had significantly lower levels of urinary calcium, uric acid, and citrate than SF with normal renal function. With regard to urinary metabolic abnormalities, compared to SF with normal renal function, SF with renal insufficiency were less likely to have hypercalciuria (P=0.041) and hyperuricosuria (P=0.014). By contrast, the renal insufficiency group had a higher incidence of hypocitraturia than the group with normal renal function (P=0.014) (Table 3).
Table 3.
Comparison of 24-hr urine constituents between SF with normal renal function and SF with renal insufficiency
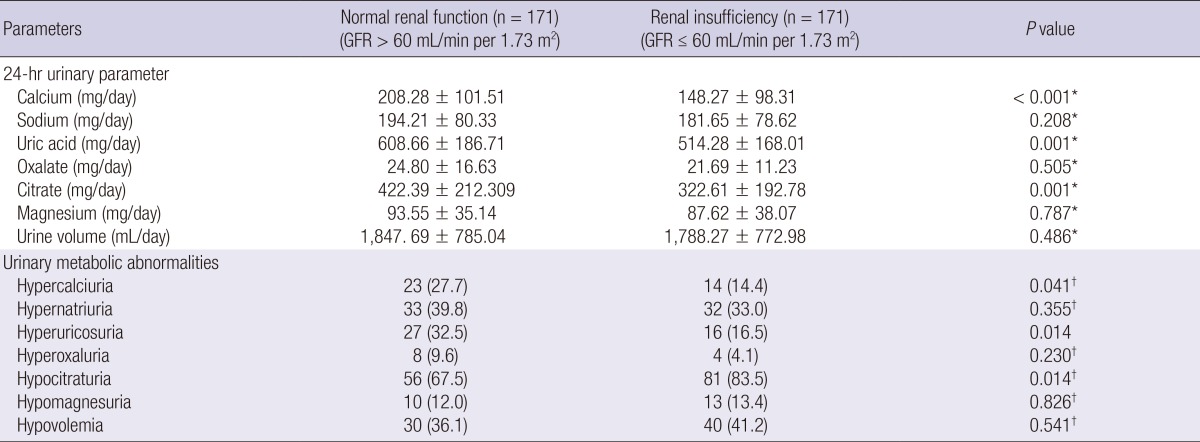
P values are based on the *Mann-Whitney U-test and †Fisher's exact test.
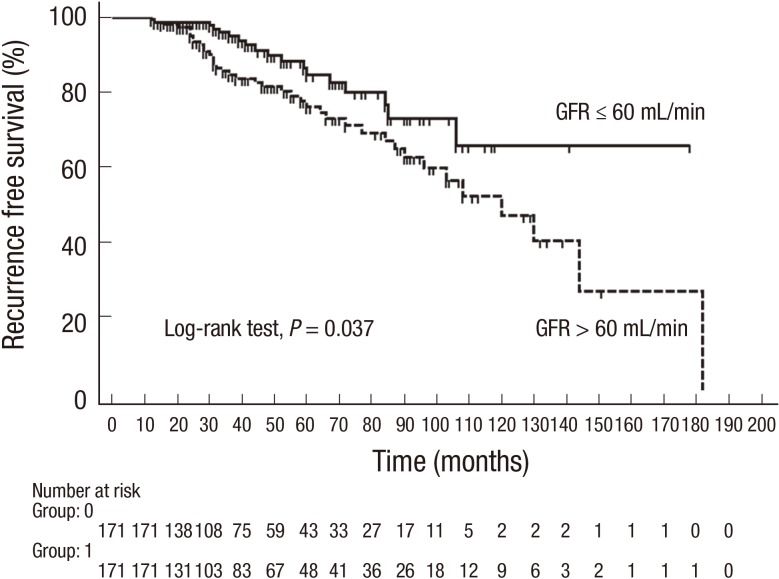
Impact of renal insufficiency on calcium oxalate supersaturation indexes and stone recurrence
Calcium oxalate supersaturation indexes and stone recurrence rates showed significant differences according to the presence of renal insufficiency. SF with renal insufficiency had lower calcium oxalate supersaturation indexes (Tiselius, P=0.016 and Ogawa, P=0.002) and stone recurrence rates (P=0.002) than SF with normal renal function (Table 4). Kaplan-Meier estimates revealed that SF with renal insufficiency had a significantly longer stone recurrence-free period than SF with normal renal function (log-rank test P=0.037) (Fig. 2).
Table 4.
Impact of renal insufficiency on calcium oxalate supersaturation and stone recurrence
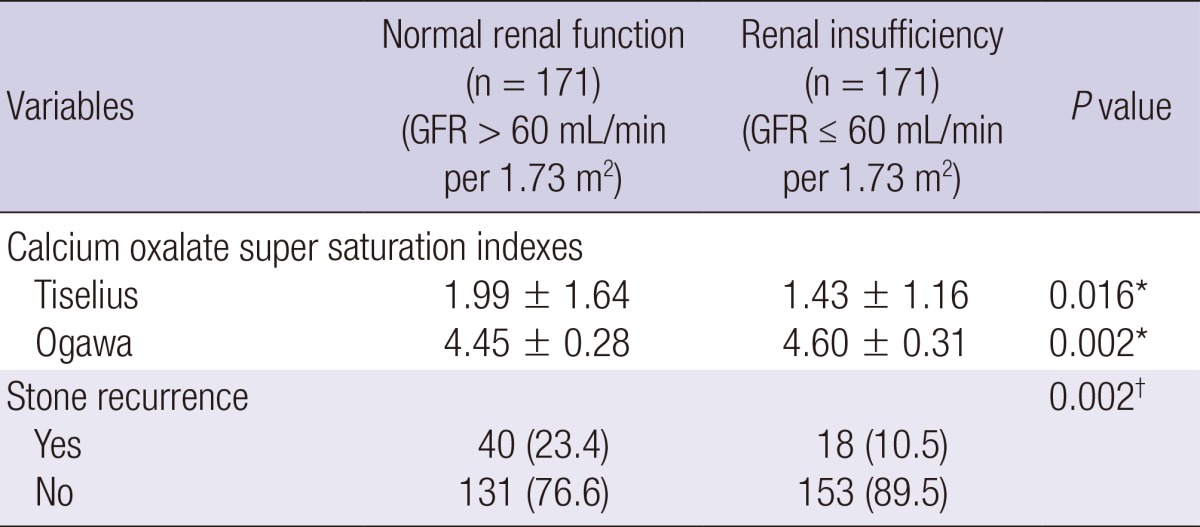
P values are based on the *Mann-Whitney U-test and †Fisher's exact test.
Fig. 2.
Stone-recurrence-free survival stratified by estimated GFR (GFR ≤ 60 mL/min vs. GFR > 60 mL/min).
DISCUSSION
In this study, the estimated GFR was positively correlated with urinary calcium, uric acid, and citrate excretion in patients with urolithiasis. Patients with renal insufficiency had lower calcium oxalate supersaturation indexes and stone recurrence rates than those with normal renal function. This finding implies that renal insufficiency is not a risk factor for stone recurrence in patients with urolithiasis.
Nephrolithiasis, a worldwide health problem, is responsible for significant economic cost to society and has a significant impact on quality of life (19, 20). Nephrolithiasis is a significant and independent risk factor for chronic kidney disease in the general population (11). Chronic renal failure in the presence of calculous disease is attributable to partial obstruction, infection, or frequent urological interventions. Once chronic renal failure is established, the disease is likely to progress due to hyperperfusion in the remaining functional nephrons (21). The stone recurrence rate and the number of stone procedures are other factors that influence renal function. The true prevalence of obstructive nephropathy associated with nephrolithiasis is unknown. Jungers et al. suggested that the overall proportion of nephrolithiasis-related end-stage renal disease in patients on maintenance dialysis was 3.2%, while others estimated the prevalence of urinary stone disease to be between 1.9% and 7.7% in patients with CKD (22, 23). Patients who suffer from recurrent stone episodes experience psychological distress and concern about progressive deterioration of renal function. However, the effect of renal insufficiency on urinary excretion of stone-forming metabolites has not been sufficiently investigated in patients with urolithiasis. One study in the literature describes that GFR falls in chronic renal disease patients, with increased fractional excretion of uric acid, calcium, phosphorus, and magnesium (12). Glomerular hyperfiltration secondary to chronic renal damage leads to osmotic diuresis, which increases tubule urinary flux and consequently reduces electrolyte tubular reabsorption. In addition, tubular dysfunction secondary to chronic renal damage leads to a reduction in electrolyte reabsorption and consequent urinary loss (12, 24). By contrast, another study showed that lower eGFR correlated with lower urine pH, lower calcium excretion, and greater oxalate excretion. The authors also found that uric acid stones were associated with a lower eGFR and that calcium phosphate stones were associated with a greater eGFR (13). Our result is similar to that of the previous study in which patients with renal insufficiency had lower urinary calcium, but differs in other urinary profiles such as oxalate, citrate, and uric acid. Different inclusion criteria between studies may explain this discrepancy. Further research should be performed to confirm the potential relationship between renal function and urinary stone-forming constituents in patients with urolithiasis. Normal aging and associated stone-related diseases, such as diabetes mellitus and hypertension, contribute to progressive glomerular filtration reduction (25, 26, 27, 28). Moreover, several reports suggest that the decision to deliver aggressive therapy for total stone clearance in patients with renal failure should be weighed against the risk of further loss of kidney function (21, 29, 30). Thus, strict dietary modification, correction of underlying disease and timely management of obstructive uropathy are essential in patients with renal insufficiency.
There are possible weaknesses in this study. The retrospective design means that there may have been some sampling bias. We used the propensity score matching model to minimize any selection bias in analyses involving age, sex, and BMI. Another limitation is the fact that stone composition was not considered in this analysis. The presence of calcium- and non-calcium-containing stones in the patient population can be a confounding factor.
In conclusion, the estimated GFR correlates positively with the urinary excretion of stone-forming constituents in SF. Patients with renal insufficiency have lower urinary lithogenic constituents and stone recurrence rates than those with normal renal function. These results imply that renal insufficiency is not a risk factor for stone recurrence in patients with urolithiasis.
ACKNOWLEDGMENTS
The biospecimens for this study were provided by the Chungbuk National University Hospital, a member of the National Biobank of Korea, which is supported by the Ministry of Health, Welfare and Family Affairs. All samples derived from the National Biobank of Korea were obtained with informed consent under institutional review board-approved protocols.
Footnotes
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2008-0062611, 2013R1A1A2004740) and by a grant from the Next-Generation BioGreen 21 Program (No. PJ009621), Rural Development Administration, Republic of Korea.
The authors have no conflicts of interest to disclose.
References
- 1.Knoll T, Schubert AB, Fahlenkamp D, Leusmann DB, Wendt-Nordahl G, Schubert G. Urolithiasis through the ages: data on more than 200,000 urinary stone analyses. J Urol. 2011;185:1304–1311. doi: 10.1016/j.juro.2010.11.073. [DOI] [PubMed] [Google Scholar]
- 2.Knoll T. Epidemiology, pathogenesis, and pathophysiology of urolithiasis. Eur Urol Suppl. 2010;9:802–806. [Google Scholar]
- 3.Lotan Y. Economics and cost of care of stone disease. Adv Chronic Kidney Dis. 2009;16:5–10. doi: 10.1053/j.ackd.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Clark JY, Thompson IM, Optenberg SA. Economic impact of urolithiasis in the United States. J Urol. 1995;154:2020–2024. [PubMed] [Google Scholar]
- 5.Matlaga BR, Jansen JP, Meckley LM, Byrne TW, Lingeman JE. Economic outcomes of treatment for ureteral and renal stones: a systematic literature review. J Urol. 2012;188:449–454. doi: 10.1016/j.juro.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marangella M, Bruno M, Cosseddu D, Manganaro M, Tricerri A, Vitale C, Linari F. Prevalence of chronic renal insufficiency in the course of idiopathic recurrent calcium stone disease: risk factors and patterns of progression. Nephron. 1990;54:302–306. doi: 10.1159/000185884. [DOI] [PubMed] [Google Scholar]
- 7.Worcester EM, Parks JH, Evan AP, Coe FL. Renal function in patients with nephrolithiasis. J Urol. 2006;176:600–603. doi: 10.1016/j.juro.2006.03.095. [DOI] [PubMed] [Google Scholar]
- 8.Worcester E, Parks JH, Josephson MA, Thisted RA, Coe FL. Causes and consequences of kidney loss in patients with nephrolithiasis. Kidney Int. 2003;64:2204–2213. doi: 10.1046/j.1523-1755.2003.00317.x. [DOI] [PubMed] [Google Scholar]
- 9.Gillen DL, Worcester EM, Coe FL. Decreased renal function among adults with a history of nephrolithiasis: a study of NHANES III. Kidney Int. 2005;67:685–690. doi: 10.1111/j.1523-1755.2005.67128.x. [DOI] [PubMed] [Google Scholar]
- 10.Chaussy C, Schüller J, Schmiedt E, Brandl H, Jocham D, Liedl B. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology. 1984;23:59–66. doi: 10.1016/0090-4295(84)90243-7. [DOI] [PubMed] [Google Scholar]
- 11.Rule AD, Bergstralh EJ, Melton LJ, Li X, Weaver AL, Lieske JC. Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol. 2009;4:804–811. doi: 10.2215/CJN.05811108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Musso CG, Juarez R, Vilas M, Navarro M, Rivera H, Jauregui R. Renal calcium, phosphorus, magnesium and uric acid handling: comparison between stage III chronic kidney disease patients and healthy oldest old. Int Urol Nephrol. 2012;44:1559–1562. doi: 10.1007/s11255-012-0230-0. [DOI] [PubMed] [Google Scholar]
- 13.Kadlec AO, Greco KA, Fridirici ZC, Gerber D, Turk TM. Effect of renal function on urinary mineral excretion and stone composition. Urology. 2011;78:744–747. doi: 10.1016/j.urology.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Eknoyan G, Levin NW. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- 15.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 16.Lifshitz DA, Shalhav AL, Lingeman JE, Evan AP. Metabolic evaluation of stone disease patients: a practical approach. J Endourol. 1999;13:669–678. doi: 10.1089/end.1999.13.669. [DOI] [PubMed] [Google Scholar]
- 17.Ogawa Y, Hatano T. Comparison of the Equil2 program and other methods for estimating the ion-activity product of urinary calcium oxalate: a new simplified method is proposed. Int J Urol. 1996;3:383–385. doi: 10.1111/j.1442-2042.1996.tb00558.x. [DOI] [PubMed] [Google Scholar]
- 18.Tiselius HG. Aspects on estimation of the risk of calcium oxalate crystallization in urine. Urol Int. 1991;47:255–259. doi: 10.1159/000282232. [DOI] [PubMed] [Google Scholar]
- 19.Bryant M, Angell J, Tu H, Goodman M, Pattaras J, Ogan K. Health related quality of life for stone formers. J Urol. 2012;188:436–440. doi: 10.1016/j.juro.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 20.Lim GS, Jang SH, Son JH, Lee JW, Hwang JS, Lim CH, Kim DJ, Cho DS. Comparison of non-contrast-enhanced computed tomography and intravenous pyelogram for detection of patients with urinary calculi. Korean J Urol. 2014;55:120–123. doi: 10.4111/kju.2014.55.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goel MC, Ahlawat R, Kumar M, Kapoor R. Chronic renal failure and nephrolithiasis in a solitary kidney: role of intervention. J Urol. 1997;157:1574–1577. [PubMed] [Google Scholar]
- 22.Sairam K, Scoffone CM, Alken P, Turna B, Sodha HS, Rioja J, Wolf JS, Jr, de la Rosette JJ CROES PCNL Study Group. Percutaneous nephrolithotomy and chronic kidney disease: results from the CROES PCNL Global Study. J Urol. 2012;188:1195–1200. doi: 10.1016/j.juro.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 23.Jungers P, Joly D, Barbey F, Choukroun G, Daudon M. ESRD caused by nephrolithiasis: prevalence, mechanisms, and prevention. Am J Kidney Dis. 2004;44:799–805. [PubMed] [Google Scholar]
- 24.Lang F. Renal handling of calcium and phosphate. Klin Wochenschr. 1980;58:985–1003. doi: 10.1007/BF01476869. [DOI] [PubMed] [Google Scholar]
- 25.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 26.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 27.Levey AS, Coresh J. Chronic kidney disease. Lancet. 2012;379:165–180. doi: 10.1016/S0140-6736(11)60178-5. [DOI] [PubMed] [Google Scholar]
- 28.Kim IY, Hwang IH, Lee KN, Lee DW, Lee SB, Shin MJ, Rhee H, Yang B, Song SH, Seong EY, et al. Decreased renal function is an independent predictor of severity of coronary artery disease: an application of gensini score. J Korean Med Sci. 2013;28:1615–1621. doi: 10.3346/jkms.2013.28.11.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paryani JP, Ather MH. Improvement in serum creatinine following definite treatment of urolithiasis in patients with concurrent renal insufficiency. Scand J Urol Nephrol. 2002;36:134–136. doi: 10.1080/003655902753679436. [DOI] [PubMed] [Google Scholar]
- 30.Gupta M, Bolton DM, Gupta PN, Stoller ML. Improved renal function following aggressive treatment of urolithiasis and concurrent mild to moderate renal insufficiency. J Urol. 1994;152:1086–1090. doi: 10.1016/s0022-5347(17)32509-0. [DOI] [PubMed] [Google Scholar]