Abstract
Airborne particles have been linked to increased mortality and morbidity. As most research has focused on fine particles (PM2.5), the health implications of coarse particles (PM10-2.5) are not well understood. We conducted a systematic review and meta-analysis of associations for short- and long-term PM10-2.5 concentrations with mortality and hospital admissions. Using 23 mortality and 10 hospital admissions studies, we documented suggestive evidence of increased morbidity and mortality in relation to higher short-term PM10-2.5 concentrations, with stronger relationships for respiratory than cardiovascular endpoints. Reported associations were highly heterogeneous, however, especially by geographic region and average PM10-2.5 concentrations. Adjustment for PM2.5 and publication bias resulted in weaker and less precise effect estimates, although positive associations remained for short-term PM10-2.5 concentrations. Inconsistent relationships between effect estimates for PM10-2.5 and correlations between PM10-2.5 and PM2.5 concentrations, however, indicate that PM10-2.5 associations cannot be solely explained by co-exposure to PM2.5. While suggestive evidence was found of increased mortality with long-term PM10-2.5 concentrations, these associations were not robust to control for PM2.5. Additional research is required to better understand sources of heterogeneity of associations between PM10-2.5 and adverse health outcomes.
Keywords: Air pollution, Coarse particulate matter, Health, Cardiovascular, Respiratory, Mortality, Hospitalizations, Time-series, Case-crossover
Introduction
Airborne particulate matter has been consistently linked to adverse health, including mortality and morbidity from respiratory and cardiovascular diseases [1]. As particles less than 10 μm in aerodynamic diameter (PM10) can reach the tracheobronchial and alveolar regions of the respiratory tract [2], these particles have been of prime interest for epidemiology studies. PM10 is comprised of two distinct types of particles with different morphologies and sources. Fine particles, < 2.5 μm (PM2.5), are typically generated by combustion or photochemical reactions in the atmosphere and are thus generally comprised of organic carbon, elemental carbon, sulfate, nitrate, and metals. In contrast, coarse particles (typically classified as 2.5–10 μm, PM10-2.5) are commonly formed by mechanical grinding and resuspension of solid material. This results in a primary composition of crustal elements, metals from suspended road dust, and organic debris [3–5]. These variations in composition, along with differential deposition in the body [2], suggest that PM2.5 and PM10-2.5 may differ in their impacts on human health.
To date, the vast majority of research has focused on PM2.5 or PM10; far less is known about the health implications of PM10-2.5. This represents a critical gap in our understanding with direct policy implications. For example, the United States Environmental Protection Agency (EPA) has stated that PM2.5 and PM10-2.5 should be considered separately under the National Ambient Air Quality Standards (NAAQS), but a unique PM10-2.5 standard has not yet been adopted. Rather, PM10-2.5 is regulated through the PM10 standard. This approach has been attributed in part due to the sparse epidemiological data available examining associations between exposures to PM10-2.5 and health effects [5].
Over the past decade, an increasing number of epidemiological investigations have explored PM10-2.5-related health effects. As reviewed by Brunekreef and Forsberg in 2005 [6], early evidence suggested the presence of associations for morbidity and mortality with short- but not long-term exposures to PM10-2.5. Associations were noted to differ by location, with stronger associations in more arid locations. Associations with respiratory hospitalizations were also notably as strong or stronger for PM10-2.5 than for PM2.5. Since PM10-2.5 associations were found to be sensitive to control for PM2.5 in the few studies reporting adjusted results, the authors encouraged future research to report multi-pollutant models.
This manuscript extends the work of Brunekreef and Forsberg [6] by incorporating newly published studies on PM10-2.5 with mortality and hospitalizations and conducting meta-analyses to generate summary estimates for relationships with PM10-2.5. To better understand factors that may modify associations between PM10-2.5 and health, we also explored heterogeneity by study location, lag period, ambient concentrations of pollution, the relative abundance of PM10-2.5 to PM2.5, and sampling methodology for PM10-2.5. We further investigated the impact of PM2.5 concentrations on associations with PM10-2.5 by summarizing results from multi-pollutant models and exploring how the magnitude of association between PM10-2.5 and health vary according to correlations between PM2.5 and PM10-2.5 concentrations.
Methods
A systematic review was conducted to identify all published studies of short- and long-term exposures to PM10-2.5 (or PM15-2.5) that reported associations with mortality or hospital admissions. We also compiled data for emergency department visits but restricted these papers to sensitivity analyses to focus our estimates on the most severe health endpoints. Literature searches using the Web of Knowledge and Medline were conducted with the key words “coarse particulate matter” or “PM10-2.5” and “health” through the end of December 2013. This approach was supplemented by a review of the reference lists of any identified publications, as well as earlier reviews by the Environmental Protection Agency [5] and Brunekreef and Forsberg [6].
Effect estimates and confidence intervals were extracted from each published report as well as descriptive information about the population, time period, outcome, and exposures. When data or results were discussed but not quantified, we contacted the authors for additional information. Papers were excluded if they did not report or we could not obtain effect estimates for PM10-2.5 with concurrent standard errors, confidence intervals, or t-values. When more than one study was available for the same population, we selected the report with the longest follow-up. Since associations for the case-crossover design are mathematically equivalent to those from time-series studies [7], we have used both designs in our meta-analyses, though we have restricted selection to papers employing a time-stratified referent selection strategy due to known bias with other designs [8]. When both case-crossover and time series approaches were presented, the time-series point estimates were included in our meta-analyses. Time-series analyses using non-parametric smoothing splines (except penalized splines) and generalized additive models in S-Plus were also excluded based on previously identified issues with model convergence and the underestimation of standard errors [9]. Citations were identified and summarized independently by two investigators.
To be included in our quantitative meta-analysis, five or more studies were required for a particular health endpoint. We identified associations a priori with the previous day (Lag 1), current day (Lag 0), and two days prior (Lag 2) as our primary analyses for total mortality, cardiovascular endpoints, and respiratory endpoints, respectively. When these exact lags were unavailable, we selected the next closest time point. All associations were standardized to a difference of 10 μg/m3 and summarized across investigations using meta-analysis (STATA v13, Stata Corp, College Station, TX). To account for heterogeneity across studies, we employed the DerSimonian and Liard random effects approach and report the I2 statistic as an indicator of the fraction of the variability due to true between-study differences as opposed to chance [10]. Publication bias was also explored using funnel plots, Egger’s test of asymmetry [11], and the “trim and fill” approach to estimate the associations that might have been observed in the absence of publication bias [12].
To explore possible causes for heterogeneity in effect estimates, we conducted analyses stratified by geographic location and lag period. We also examined non-linearity of the dose-response relationship through stratification by PM10-2.5 concentrations and meta-regression. Differences in associations by PM2.5 concentrations and the ratio of PM10-2.5 to PM10 were similarly explored to assess if PM10-2.5 from regions with more urban/industrial pollution from combustion had greater toxicity than PM10-2.5 from other settings. In addition, we summarized all available associations with PM10-2.5 adjusted for PM2.5 and investigated if PM10-2.5 associations were greater in locations with higher correlations between PM10-2.5 and PM2.5 concentrations. Finally, we explored if sampling methods suspected to have more (i.e., tapered element oscillating microbalance, TEOM) or less measurement error (i.e., dichotomous sampler) for PM10-2.5 [13] were found to impact associations.
Results
Papers Identified with Short-Term PM10-2.5 Exposures
A total of 34 published studies were identified that presented associations between short-term fluctuations in PM10-2.5 concentrations and mortality. Of these investigations, we excluded three manuscripts with incomplete reporting of numerical results [14–16]. An additional nine papers were excluded for use of non-parametric smoothing splines in GAM. Of these, seven [17–23] were replaced by later re-analysis of the same data [9], but two were without replication [24, 25]. Similarly, three papers were superseded by longer time series from the same populations [22, 26, 27], and one was excluded, as it was a sensitivity analysis of another report [28]. One final paper was excluded as it only explore stroke mortality [29]. This resulted in 23 studies for inclusion in this meta-analysis—19, 11, and 14 total cases of non-accidental [9, 30–32, 33••, 34, 35, 36••, 37, 38, 39••, 40–45], respiratory, [9, 33••, 34, 36••, 37, 38, 39••, 41, 42, 46, 47], and cardiovascular mortality [9, 33••, 34, 35, 36••, 37, 38, 39••, 41, 42, 46, 47], respectively. No other cause-specific mortality had sufficient counts to be included.
For hospital admissions, we identified 23 studies and one scientific report with published associations for short-term exposures to PM10-2.5. Of these investigations, we excluded eight manuscripts for using non-parametric smoothing splines in GAM or case-crossover reference strategies inconsistent with current recommendations [18, 24, 48–53]. Two of these investigations [18, 53] were re-analyzed [9], and therefore included in our analysis. An additional study was excluded for using an ordinary least squares approach for time-series [54], two as sensitivity analyses of primary results presented elsewhere [55, 56] and another four for including health outcomes with insufficient counts for meta-analysis [18, 52, 57, 58]. After these exclusions, there were a total of 10 papers for meta-analysis, resulting in sufficient counts to explore respiratory (n = 9) [42, 47, 59–61, 62••, 63••, 64, 65•] and cardiovascular hospitalizations (n = 6) [42, 47, 61, 62••, 64, 66]. An additional 12 papers [15, 35, 67–76] and one report [77] were identified on emergency department visits, although these included some extensions of earlier papers and some unique health outcomes that were not reported in a sufficient number of studies to support meta-analysis.
Table 1 summarizes the studies included in this meta-analysis. Across all of the investigations of short-term exposures to PM10-2.5, a total of 9.3 million non-accidental deaths, 0.75 million respiratory deaths, and 2.4 million cardiovascular deaths were enumerated. Additionally there were 2.8 and 5.4 million hospital admissions for respiratory and cardiovascular causes, respectively. Most of these investigations (80 %) utilized a time-series design and were conducted in either North America or Europe. In the regions studied, concentrations of PM10-2.5 and PM2.5 ranged from lows of 3.7 and 6.7 μg/m3 in the United States to highs of 101 and 94 μg/m3 in China, respectively. Correlations between these two pollutants were generally modest and ranged from -0.03 in the United States to 0.73 in France.
Table 1.
Descriptive information for short-term exposure studies included in the meta-analysis
| Study | Location | Time Period | Study Design | Restrictions | Reported or Estimated # of Events (Short-Term) or # of Participants (Long-Term) | Estimated Incidence Rate Ratios (95 % CI) per 10 μg/m3 of PM10–2.5 | Estimated Incidence Rate Ratios (95 % CI) per 10 μg/m3 of PM2.5 | Median or Mean† PM10–2.5 | Median or Mean† PM2.5 | Correlation of PM10–2.5 and PM2.5 |
|---|---|---|---|---|---|---|---|---|---|---|
| Short-Term Associations With Non-Accidental Mortality | ||||||||||
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | 278,545 | 1.018 (1.007, 1.030) | 1.000 (0.996, 1.004) | 7.0 | 15 | 0.22 | |
| Burnett et al. 2004 | 12 Cities, Canada | 1981–1999 | Time-Series | 1,450,251 | 1.006 (0.999, 1.014) | 1.005 (0.991, 1.020) | 11.4† | 12.8† | ||
| Chen et al. 2011 | 3 Cities, China | 2004–2008* | Time-Series | 308,904 | 1.003 (1.001, 1.004) | 1.003 (1.002, 1.004) | 49–101† | 55–94† | 0.28–0.53 | |
| Chock et al. 2000 | Allegheny County, United States | 1989–1991 | Time-Series | <75 years | 25,609 | 1.003 (0.993, 1.013) | 1.010 (0.992, 1.028) | |||
| Chock et al. 2000 | Allegheny County, United States | 1989–1991 | Time-Series | >75 years | 25,109 | 1.005 (0.995, 1.015) | 1.006 (0.988, 1.025) | |||
| Cifuentes et al. 2000 | Santiago metropolitan area, Chile | 1988–1996 | Time-Series | 165,668 | 1.006 (1.001, 1.012) | 1.005 (1.003, 1.008) | 44.3 | 42.6 | 0.52 | |
| Fairley 1999/HEI 2003 | Santa Clara, United States | 1986–1996 | Time-Series | 58,440 | 0.978 (0.922, 1.037) | 0.984 (0.962, 1.007) | 11† | 9† | 0.51 | |
| Janssen et al. 2013 | All Cities, Netherlands | 2008–2009 | Time-Series | 258,159 | 0.998 (0.987, 1.010) | 1.008 (1.003, 1.012) | 7.2 | 13.1 | 0.29 | |
| Klemm et al. 2004 | Atlanta, United States | 1998–2000 | Time-Series | >65 years | 10,841 | 1.006 (0.999, 1.014) | 1.003 (1.001, 1.005) | 9.3 | 18.1 | |
| Lippmann et al. 2000/HEI 2003 | Detroit, United States | 1992–1994 | Time-Series | 25,970 | 1.011 (0.991, 1.032) | 1.008 (0.993, 1.023) | 12 | 15 | 0.42 | |
| Lopez-Villarrubia et al. 2012 | Las Palmas de Gran Canaria, Canary Islands | 2001–2004 | Time-Series | 10,811 | 1.004 (0.981, 1.028) | 0.994 (0.959, 1.029) | 14.6 | 12.7 | 0.55 | |
| Lopez-Villarrubia et al. 2012 | Santa Cruz de Tenerife, Canary Islands | 2001–2004 | Time-Series | 6,428 | 1.004 (0.981, 1.028) | 0.994 (0.959, 1.029) | 20.3 | 11.3 | 0.55 | |
| Malig et al. 2009 | 15 California Counties, United States | 1999–2005 | Case-Crossover | 107,188 | 1.000 (0.989, 1.012) | 10.6–46.5† | 11.1–17.3† | -0.03–0.35 | ||
| Mallone et al. 2011 | Rome, Italy | 2001–2004 | Case-Crossover | 80,423 | 1.027 (1.011, 1.044) | 1.010 (0.995, 1.025) | 13.6, 18.3†† | 20.9, 24†† | 0.27, 0.18†† | |
| Meister et al. 2012 | Stockholm, Sweden | 2000–2008 | Time-Series | 93,398 | 1.017 (1.002, 1.032) | 1.015 (1.001, 1.028) | 7.1† | 8.6† | 0.27 | |
| Perez et al. 2008 | Barcelona, Spain | 2003–2004 | Case-Crossover | 24,850 | 1.027 (1.008, 1.046) | 1.040 (1.023, 1.057) | 12.9 | 22.4 | 0.33 | |
| Samoli et al. 2013 | 8 metropolitan areas, European Mediterranean | 2001–2010* | Time-Series | 578,191 | 1.003 (0.999, 1.007) | 1.006 (1.003, 1.008) | 8.0–15.8 | 13.6–27.7 | 0.19–0.68 | |
| Schwartz et al. 1996/HEI 2003 | 6 Cities, United States | 1979–1988 | Time-Series | >65 years | 103,841 | 1.001 (0.995, 1.007) | 1.008 (1.004, 1.013) | 9 | 14.7 | 0.23–0.69 |
| Tobias et al. 2011 | Madrid, Spain | 2003–2005 | Case-Crossover | Dust Days | 12,993 | 1.005 (0.987, 1.026) | 1.008 (0.980, 1.040) | 22 | 24 | |
| Tobias et al. 2011 | Madrid, Spain | 2003–2005 | Case-Crossover | Dust-Free Days | 53,997 | 1.021 (1.007, 1.035) | 1.030 (1.015, 1.043) | 12 | 16 | |
| Villeneuve et al. 2003 | Vancouver, Canada | 1986–1998 | Time-Series | >65 years | 28,210 | 0.990 (0.964, 1.016) | 1.013 (0.983, 1.044) | 7.8† | 10.7† | 0.46 |
| Zanobetti et al. 2009 | 47 Cities, United States | 1999–2005 | Time-Series | 5,609,349 | 1.005 (1.002, 1.007) | 1.010 (1.008, 1.012) | 3.7–33.1† | 6.7–21.7† | ||
| Short-Term Associations With Respiratory Mortality | ||||||||||
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | 42,262 | 1.001 (0.972, 1.031) | 1.009 (0.999, 1.019) | 7.0 | 15 | 0.22 | |
| Chen et al. 2011 | 3 Cities, China | 2004–2008* | Time-Series | 33,871 | 1.002 (0.996, 1.008) | 1.002 (0.999, 1.005) | 49–101† | 55–94† | 0.28–0.53 | |
| Halonen et al. 2009 | Helsinki metropolitan area, Finland | 1998–2004 | Time-Series | 3,701 | 1.005 (0.958, 1.054) | 1.000 (0.952, 1.051) | 7.5 | 9.5 | 0.25 | |
| Janssen et al. 2013 | All Cities, Netherlands | 2008–2009 | Time-Series | 27,759 | 1.038 (1.006, 1.072) | 1.016 (1.004, 1.029) | 7.2 | 13.1 | 0.29 | |
| Lippmann et al 2000/HEI 2003 | Detroit, United States | 1992–1994 | Time-Series | 12,250 | 1.025 (0.959, 1.096) | 1.012 (0.960, 1.067) | 12 | 15 | 0.42 | |
| Lopez-Villarrubia et al. 2012 | Las Palmas de Gran Canaria, Canary Islands | 2001–2004 | Time-Series | 979 | 1.060 (0.987, 1.137) | 1.059 (0.948, 1.184) | 14.6 | 12.7 | 0.55 | |
| Lopez-Villarrubia et al. 2012 | Santa Cruz de Tenerife, Canary Islands | 2001–2004 | Time-Series | 584 | 1.060 (0.987, 1.137) | 1.059 (0.948, 1.184) | 20.3 | 11.3 | 0.55 | |
| Mallone et al. 2011 | Rome, Italy | 2001–2004 | Case-Crossover | 4,574 | 1.117 (1.011, 1.233) | 1.002 (0.922, 1.089) | 13.6, 18.3†† | 20.9, 24†† | 0.27, 0.18†† | |
| Perez et al. 2012 | Barcelona, Spain | 2003–2007 | Case-Crossover | Dust Days | 540 | 1.035 (0.918, 1.167) | 1.020 (0.909, 1.145) | 11.5 | 17.3 | 0.01 |
| Perez et al. 2012 | Barcelona, Spain | 2003–2007 | Case-Crossover | Dust-Free Days | 5,812 | 1.048 (1.013, 1.085) | 1.028 (0.994, 1.062) | 12.4 | 19.2** | 0.01** |
| Samoli et al. 2013 | 8 metropolitan areas, European Mediterranean | 2001–2010* | Time-Series | 58,440 | 1.007 (0.997, 1.018) | 1.016 (1.006, 1.027) | 8.0–15.8 | 13.6–27.7** | 0.19–0.68** | |
| Villeneuve et al. 2003 | Vancouver, Canada | 1986–1998 | Time-Series | >65 years | 3,765 | 1.001 (0.942, 1.063) | 1.002 (0.919, 1.092) | 7.8† | 10.7† | 0.46 |
| Zanobetti et al. 2009 | 47 Cities, United States | 1999–2005 | Time-Series | 547,660 | 1.012 (1.004, 1.019) | 1.017 (1.010, 1.023) | 3.7–33.1† | 6.7–21.7† | ||
| Short-Term Associations With Cardiovascular Mortality | ||||||||||
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | 103,734 | 0.996 (0.977, 1.015) | 1.001 (0.994, 1.007) | 7.0 | 15 | 0.22 | |
| Chen et al. 2011 | 3 Cities, China | 2004–2008* | Time-Series | 126,988 | 1.001 (1.000, 1.003) | 1.005 (1.004, 1.007) | 49–101† | 55–94† | 0.28–0.53 | |
| Halonen et al. 2009 | Helsinki metropolitan area, Finland | 1998–2004 | Time-Series | 16,233 | 1.000 (0.979, 1.021) | 1.012 (0.989, 1.035) | 7.5 | 9.5 | 0.25 | |
| Janssen et al. 2013 | All Cities, Netherlands | 2008–2009 | Time-Series | 78,675 | 0.981 (0.961, 1.001) | 1.011 (1.002, 1.019) | 7.2 | 13.1 | 0.29 | |
| Lippmann et al. 2000/HEI 2003 | Detroit, United States | 1992–1994 | Time-Series | 1,960 | 1.024 (0.994, 1.055) | 1.008 (0.986, 1.030) | 12 | 15 | 0.42 | |
| Lopez-Villarrubia et al. 2012 | Las Palmas de Gran Canaria, Canary Islands | 2001–2004 | Time-Series | 2,338 | 1.023 (0.976, 1.072) | 1.026 (0.956, 1.101) | 14.6 | 12.7 | 0.55 | |
| Lopez-Villarrubia et al. 2012 | Santa Cruz de Tenerife, Canary Islands | 2001–2004 | Time-Series | 1,315 | 1.023 (0.976, 1.072) | 1.026 (0.956, 1.101) | 20.3 | 11.3 | 0.55 | |
| Malig et al. 2009 | 15 California Counties, United States | 1999–2005 | Case-Crossover | 45,036 | 1.003 (0.988, 1.017) | 10.6–46.5† | 11.1–17.3† | –0.03–0.35 | ||
| Mallone et al. 2011 | Rome, Italy | 2001–2004 | Case-Crossover | 24,773 | 1.034 (1.007, 1.062) | 1.011 (0.987, 1.035) | 13.6, 18.3†† | 20.9, 24†† | 0.27, 0.18 | |
| Mar et al 2000/2003 | Maricopa County, United States | 1995–1997 | Time-Series | 4,182 | 1.024 (1.003, 1.046) | 1.040 (0.984, 1.100) | 33.5† | 13.0† | 0.5–0.59 | |
| Ostro et al. 2000/2003 | Coachella Valley, United States | 1989–1998 | Time-Series | 8,073 | 1.011 (1.002, 1.020) | 0.944 (0.882, 1.010) | 30.5† | 16.8† | 0.28 | |
| Perez et al. 2012 | Barcelona, Spain | 2003–2007 | Case-Crossover | Dust Days | 1,650 | 1.104 (1.031, 1.181) | 1.041 (0.968, 1.122) | 11.5 | 17.3** | 0.01** |
| Perez et al. 2012 | Barcelona, Spain | 2003–2007 | Case-Crossover | Dust-Free Days | 16,513 | 1.041 (1.018, 1.066) | 1.030 (1.006, 1.054) | 12.4 | 19.2** | 0.01** |
| Samoli et al. 2013 | 8 metropolitan areas, European Mediterranean | 2001–2010* | Time-Series | 213,306 | 1.003 (0.996, 1.009) | 1.006 (1.001, 1.011) | 8.0–15.8 | 13.6–27.7 | 0.19–0.68 | |
| Villeneuve et al. 2003 | Vancouver, Canada | 1986–1998 | Time-Series | >65 years | 11,518 | 1.053 (1.010, 1.098) | 0.990 (0.942, 1.041) | 7.8† | 10.7† | 0.46 |
| Zanobetti et al. 2009 | 47 Cities, United States | 1999–2005 | Time-Series | 1,787,078 | 1.003 (1.000, 1.006) | 1.009 (1.005, 1.012) | 3.7–33.1† | 6.7–21.7† | ||
| Short-Term Associations With Respiratory Hospitalizations | ||||||||||
| Alessandrini et al. 2013 | Rome, Italy | 2001–2004 | Time-Series | <14 years | 11,157 | 0.986 (0.935, 1.038) | 0.999 (0.958, 1.041) | 14.6 to 20.7†† | 23.4 to 25.6†† | 0.25 |
| Alessandrini et al. 2013 | Rome, Italy | 2001–2004 | Time-Series | >35 years | 20,463 | 1.041 (1.004, 1.079) | 0.997 (0.969, 1.025) | 14.6 to 20.7†† | 23.4 to 25.6†† | 0.25 |
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | <14 years | 67,235 | 0.998 (0.973, 1.024) | 1.017 (1.009, 1.025) | 7.0 | 15 | 0.22 |
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | >65 years | 121,023 | 1.007 (0.988, 1.026) | 1.009 (1.003, 1.016) | 7.0 | 15 | 0.22 |
| Chen et al. 2005 | Vancouver, Canada | 1995–1999 | Time-Series | >65 years | 12,880 | 1.123 (1.048, 1.201) | 1.051 (0.975, 1.157) | 5.6† | 7.7† | 0.38 |
| Halonen et al. 2009 | Helsinki metropolitan area, Finland | 1998–2004 | Time-Series | 26,095 | 0.999 (0.981, 1.017) | 1.023 (1.004, 1.042) | 7.5 | 9.5 | 0.25 | |
| Host et al. 2008 | 6 French cities, France | 2000–2003* | Time-Series | <14 years | 56,387 | 1.062 (1.004, 1.123) | 1.004 (0.988, 1.020) | 7.0–11.0† | 13.8–18.8† | 0.28–0.73 |
| Host et al. 2008 | 6 French cities, France | 2000–2003* | Time-Series | 15–64 years | 57,589 | 1.026 (0.995, 1.058) | 1.008 (0.993, 1.023) | 7.0–11.0† | 13.8–18.8† | 0.28–0.73 |
| Host et al. 2008 | 6 French cities, France | 2000–2003* | Time-Series | >65 years | 56,267 | 1.019 (0.981, 1.059) | 1.005 (0.980, 1.030) | 7.0–11.0† | 13.8–18.8† | 0.28–0.73 |
| Peng et al. 2008 | 108 Counties, United States | 1999–2005 | Time-Series | >65 years | 1.4 M | 0.999 (0.994, 1.005) | 1.004 (1.001, 1.008) | 13.5 | 9.8 | 0.12 |
| Qiu et al. 2012 | Hong Kong, Special Administrative Region of China | 2000–2005 | Time-Series | 518,864 | 1.009 (1.004, 1.014) | 14.5 | 34.8 | 0.68 | ||
| Stafoggia et al. 2013 | 6 metropolitan areas, European Mediterranean | 2001–2010 | Time-Series | >15 years | 459,261 | 1.012 (0.989, 1.036) | 1.011 (1.000, 1.021) | 9.3–17.5† | 17.2–34.4† | 0– > 0.5 |
| Yang et al. 2004 | Vancouver, Canada | 1995–1999 | Case-Control | <3 years | 1,610 | 1.048 (0.885, 1.255) | 4.8 | 7 | 0.39 | |
| Short-Term Associations With Cardiovascular Hospitalizations | ||||||||||
| Atkinson et al. 2010 | London, United Kingdom | 2000–2005 | Time-Series | 293,913 | 1.002 (0.990, 1.014) | 1.004 (0.999, 1.008) | 7.0 | 15 | 0.22 | |
| Halonen et al. 2009 | Helsinki metropolitan area, Finland | 1998–2004 | Time-Series | 61,571 | 1.010 (0.998, 1.021) | 0.997 (0.985, 1.009) | 7.5 | 9.5 | 0.25 | |
| Host et al. 2008 | 6 French cities, France | 2000–2003* | Time-Series | 251,397 | 1.005 (0.988, 1.023) | 1.009 (1.001, 1.018) | 7.0–11.0† | 13.8–18.8† | 0.28–0.73 | |
| Peng et al. 2008 | 108 Counties, United States | 1999–2005 | Time-Series | >65 years | 3.7 M | 1.004 (1.001, 1.007) | 1.007 (1.005, 1.010) | 13.5 | 9.8 | 0.12 |
| Qiu et al. 2013 | Hong Kong, Special Administrative Region of China | 2000–2005 | Time-Series | 338,123 | 1.007 (1.000, 1.013) | 1.006 (1.003, 1.009) | 14.5 | 34.8 | 0.68 | |
| Stafoggia et al. 2013 | 6 metropolitan areas, European Mediterranean | 2001–2010 | Time-Series | >15 years | 727,579 | 1.007 (1.002, 1.013) | 1.005 (1.001, 1.009) | 9.3–17.5† | 17.2–34.4† | 0– > 0.5 |
* Years differed by city, ** PM1 reported instead of PM2.5, † Mean, †† Dust day, dust-free day
Associations Between Short-Term PM10-2.5 Exposures, Mortality, and Hospital Admissions
The vast majority of short-term studies linked higher mortality and morbidity with higher PM10-2.5 concentrations (Fig. 1). Mortality and hospital admissions due to respiratory causes had the largest associations with random-effects summary estimates of 1.4 % (95 % CI: 0.5–2.4 %) and 1.0 % (95 % CI: 0.1–1.8 %) higher rates per 10 μg/m3, respectively (Table 2). These estimates were approximately two to three times higher than the observed associations for total mortality, cardiovascular mortality, and cardiovascular hospital admissions, although the confidence intervals were also much wider. Sensitivity analyses of cause-specific hospital visits (including estimates from emergency department studies) provided consistent evidence of increased rates with increasing levels of PM10-2.5 for outcomes including asthma, chronic obstructive pulmonary disease, and ischemic heart disease (results not presented). In general, the inclusion of emergency department visits resulted in a slight weakening of the respiratory but not cardiovascular summary estimates, though the results were qualitatively the same. Exclusion of childhood respiratory admissions also did not substantially alter our findings (results not presented).
Fig. 1.
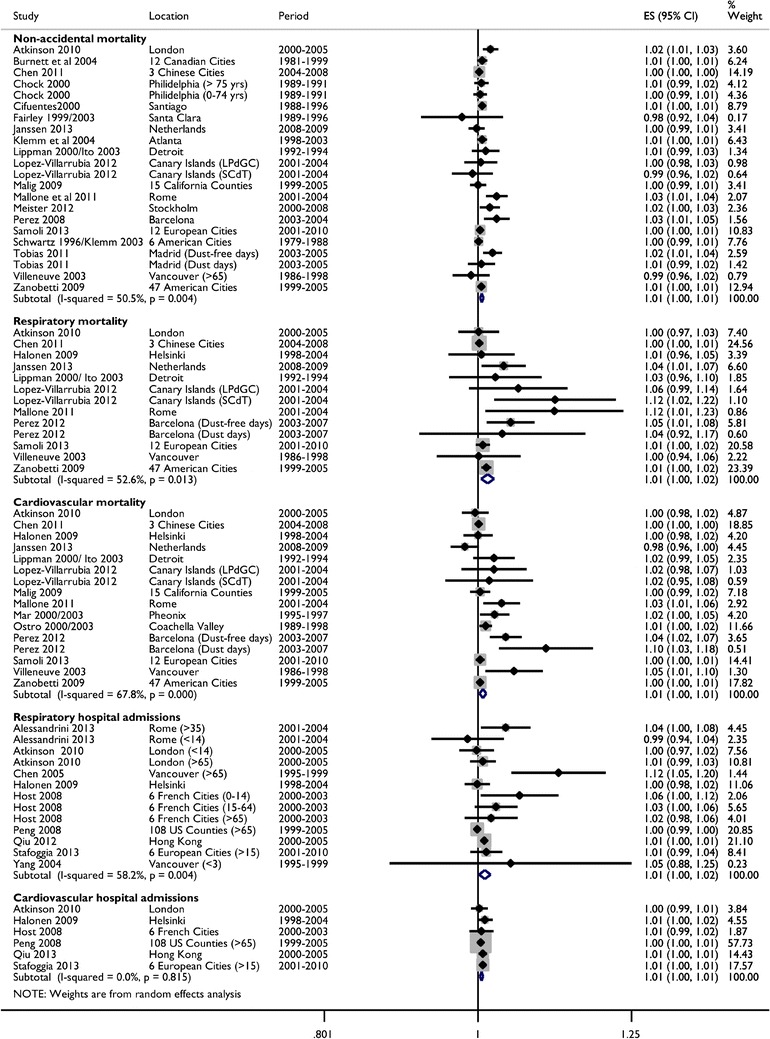
Forest plot of incidence rate ratios for mortality and hospital admissions per 10 μg/m3 of short-term exposure to PM10-2.5. Note: Overall estimates are from random-effects models without adjustment for possible publication bias
Table 2.
Summary rate ratios (RR) for mortality and hospital admissions per 10 μg/m3 of PM10–2.5 and PM2.5 concentrations
| Short-Term Exposures | Long-Term Exposures | |||||
|---|---|---|---|---|---|---|
| Total Mortality | Respiratory Mortality | Cardiovascular Mortality | Respiratory Hospitalizations | Cardiovascular Hospitalizations | Total Mortality | |
| Coarse Particulate Matter | ||||||
| Number of studies | 19 | 11 | 14 | 9 | 6 | 6 |
| Number of estimatesa | 22 | 13 | 16 | 13 | 6 | 6 |
| Pooled RR (95 % CI)b | 1.006 (1.003–1.008) | 1.014 (1.005–1.024) | 1.007 (1.002–1.012) | 1.010 (1.001–1.018) | 1.005 (1.003–1.008) | 1.021(0.984–1.058) |
| Heterogeneity | ||||||
| I2 | 51 % | 53 % | 68 % | 58 % | 0 % | 38 % |
| p-value | 0.004 | 0.013 | <0.001 | 0.004 | 0.82 | 0.15 |
| Publication bias | ||||||
| Adjusted RR (95 % CI)c | 1.004 (1.001–1.007) | 1.007 (0.996–1.018) | 1.002 (0.997–1.008) | 1.006 (0.996–1.016) | 1.005 (1.003–1.007) | 0.994 (0.956–1.035) |
| Egger regression test, p-value | 0.05 | 0.01 | 0.01 | 0.07 | 0.45 | 0.66 |
| Fine Particulate Matter | ||||||
| Number of studies | 18 | 11 | 14 | 9 | 7 | 6 |
| Number of estimatesa | 21 | 13 | 15 | 11 | 7 | 6 |
| Pooled RR (95 % CI)b | 1.007 (1.004–1.009) | 1.012 (1.005–1.020) | 1.006 (1.004–1.008) | 1.009 (1.005–1.013) | 1.006 (1.004–1.007) | 1.092 (1.009–1.182) |
| Heterogeneity | ||||||
| I2 | 75 % | 62 % | 17 % | 27 % | 0 % | 76 % |
| p-value | <0.001 | 0.002 | 0.26 | 0.19 | 0.51 | 0.001 |
| Publication bias | ||||||
| Adjusted RR (95 % CI)c | 1.005 (1.002–1.008) | 1.006 (0.998–1.013) | 1.006 (1.004–1.008) | 1.009 (1.005–1.013) | 1.006 (1.004–1.007) | 1.061 (0.984–1.143) |
| Egger regression test, p-value | 0.08 | 0.06 | 0.20 | 0.39 | 0.28 | 0.32 |
Notes: a The number of estimates can differ from the number of studies due to reports stratified by age group and/or Saharan dust days
b Overall estimates are from random-effects models
c Models are adjusted for possible publication bias using a trim and fill approach
Single pollutant associations for PM10-2.5 were generally similar to those reported for PM2.5 in studies with paired single pollutant estimates (Table 2). Estimates for PM10-2.5, however, showed more evidence of possible publication bias as shown by statistically significant findings of asymmetry using Egger’s regression test. Adjustment for asymmetry using a “trim and fill” approach resulted in a weakening, though not elimination, of most associations with PM10-2.5. Associations for PM2.5 were generally more robust to adjustment for possible publication bias.
All outcomes except cardiovascular disease hospital admissions showed moderate (I2 = 51–68 %) and statistically significant heterogeneity in the point estimates for PM10-2.5 (Table 2). As shown in Figs. 2 and 3, location appeared to be an important explanatory factor for this heterogeneity with stratified analyses indicating that European cities consistently had larger PM10-2.5 associations than North America for all outcomes except for cardiovascular mortality. Although there was no clear evidence of heterogeneity by PM2.5 concentrations, there was some evidence of lower rate ratios with higher PM10-2.5 concentrations for both mortality and hospital admissions. Lower rate ratios were also found when PM10-2.5 was more than half of the reported PM10 concentrations for hospital admissions but not mortality (meta-regression p-value: 0.06). There was also a suggestion of weaker associations with total mortality among studies using TEOMs and stronger associations among studies using dichotomous samplers but the sample size was small and the differences were not large (results not shown). There were insufficient numbers to examine these relationships with outcomes other than cardiovascular and respiratory mortality and admissions.
Fig. 2.
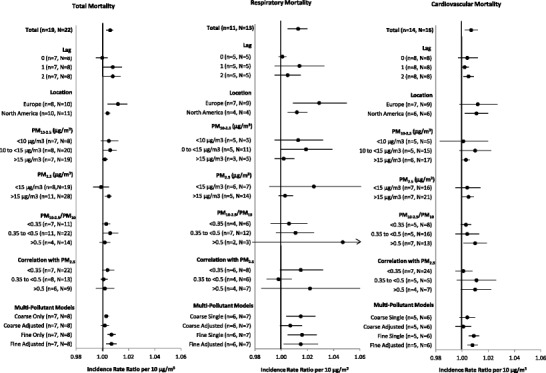
Summary incidence rate ratios for short-term exposures to PM10-2.5 with mortality by study characteristics. Note: Estimates stratified by concentrations include city-specific data from Malig and Ostro [35] and Chock et al. [45] provided via personal correspondence. Estimates were also provided by Zanobetti and Schwartz [33••] but ultimately not included because the use of shrunken Bayes estimates could have undue influence on our results
Fig. 3.
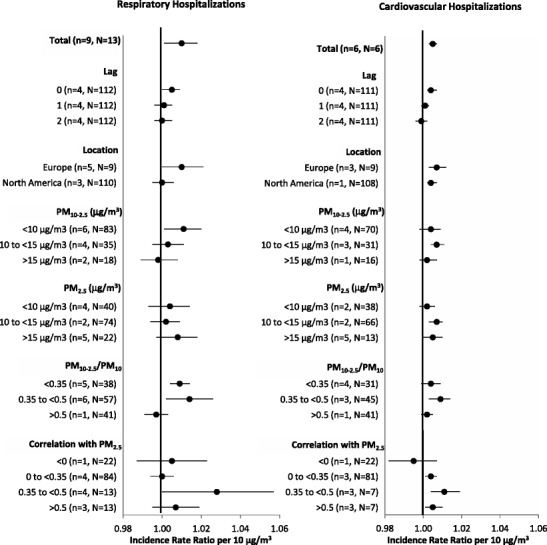
Summary incidence rate ratios for short-term exposures to PM10-2.5 with hospital admissions by study characteristics. Note: Estimates stratified by PM concentrations and correlations include city-specific estimates provided by Peng et al. [62••] and Host et al. [61] in personal communications
As shown in Fig. 2, associations between short-term PM10-2.5 concentrations and mortality were sensitive to control for PM2.5 in two-pollutant models, with a weakening of associations that resulted in a loss of statistical significance in all scenarios. This was especially true for cardiovascular mortality, for which the PM10-2.5 association was fully eliminated by control for PM2.5 (results not shown). Although there were too few hospital admission studies with multi-pollutant estimates for a formal meta-analysis, these results appeared to be generally less sensitive to control for PM2.5. In spite of the observed sensitivity in PM10-2.5 associations to control for PM2.5, we did not observe a consistent pattern of increasing associations with PM10-2.5 with increasing correlations between PM2.5 and PM10-2.5 concentrations when PM2.5 was associated with adverse health (Fig. 4). Nor did we find consistent evidence of smaller associations with PM10-2.5 with increasing correlations between PM10-2.5 and PM2.5 concentrations when PM2.5 concentrations were associated with improved health. Associations with PM2.5 were less sensitive to control for PM10-2.5 concentrations (Fig. 2)
Fig. 4.
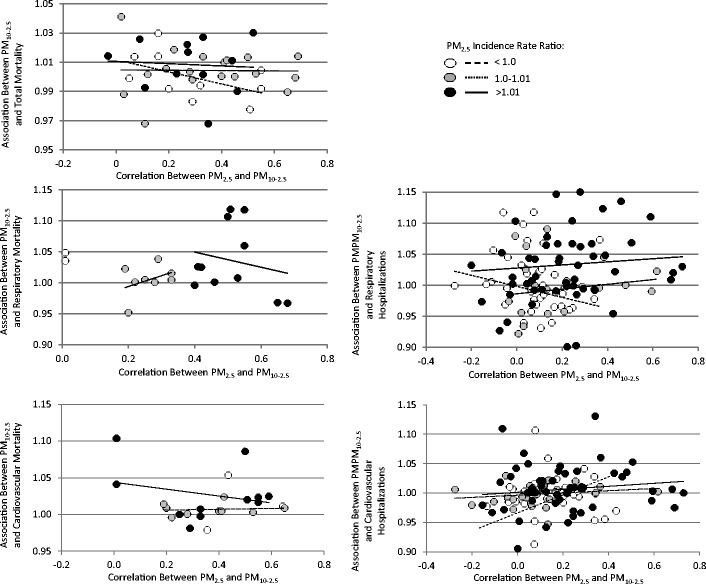
Incidence rate ratios (RR) for PM10-2.5 as a function of the correlation between short-term PM10-2.5 and PM2.5 concentrations stratified by PM2.5 associations. Note: Data include city-specific estimates provided by Peng et al. [62••] and Host et al. [61] from personal communications
Papers Identified with Long-Term Exposures to PM10-2.5
Estimates of associations between long-term PM10-2.5 concentrations and all-cause mortality were available from five American cohort studies [78••, 79, 80••, 81••, 82] and one multicenter study in Europe that combined data from 19 study populations (Table 3) [83]. Additional studies on infant mortality[84] and fatal coronary heart disease [85] were identified but ultimately not included because the number of studies was insufficient to support a meta-analysis. As summarized in Tables 3, these cohort studies collectively followed approximately 780,000 participants over a range of PM10-2.5 (4.0 to 27.3 μg/m3) and PM2.5 concentrations (6.6 to 31.9 μg/m3).
Table 3.
Descriptive information for long-term exposure studies included in the meta-analysis
| Study | Location | Time Period | Study Design | Restrictions | Reported or Estimated # of Events (Short-Term) or # of Participants (Long-Term) | Estimated Incidence Rate Ratios (95 % CI) per 10 μg/m3 of PM10–2.5 | Estimated Incidence Rate Ratios (95 % CI) per 10 μg/m3 of PM2.5 | Median or Mean† PM10–2.5 | Median or Mean† PM2.5 | Correlation of PM10–2.5 and PM2.5 |
|---|---|---|---|---|---|---|---|---|---|---|
| Long-Term Associations With Non-Accidental Mortality | ||||||||||
| Beelen et al. 2013 | 19 Cohorts from 12 European Countries | 1985–2007 | Cohort Studies | 327,780 | 1.08 (0.96, 1.21) | 1.14 (1.04, 1.28) | 4.0–20.7† | 6.6–31.0† | 0.11–0.90 | |
| Lipfert et al. 2006 | 32 Veterans Hospitals, United States | 1989–1996 | Cohort Study | All-Cause | 24,642 | 1.06 (1.01, 1.11) | 1.15 (1.05, 1.26) | 16† | 14.3† | |
| McDonnell et al. 2000 | California, United States | 1977–1992 | Cohort Study | 1,266 | 1.05 (0.92, 1.20) | 1.22 (0.95, 1.58) | 27.3† | 31.9† | 0.5 | |
| Pope et al. 2002 | 50 States, United States | 1982–1998 | Cohort Study | 359,000 | 1.01 (0.97, 1.05) | 1.06 (1.02, 1.11) | 19.2†˜ | 17.7† | ||
| Puett et al. 2009 | 13 Northeast and Midwest States, United States | 1992–2002 | Cohort Study | 66,250 | 1.03 (0.89, 1.18) | 1.26 (1.02, 1.54) | 7.7† | 13.9† | ||
| Puett et al. 2011 | 13 Northeast and Midwest States, United States | 1989–2003 | Cohort Study | 17,545 | 0.96 (0.91, 1.02) | 0.94 (0.87, 1.00) | 10.1† | 17.8† | ||
˜ PM15 reported instead of PM10
Associations Between Long-Term PM10-2.5 Exposures and Mortality
Pooled random-effects analyses resulted in a summary estimate of a 2.1 % (95 % CI: -1.6 % to 5.8 %) increased mortality rates per 10 μg/m3 higher long-term PM10-2.5 concentration (Table 2, Fig. 5). There was limited evidence of heterogeneity among these point estimates (I2 = 38 %, p = 0.15) and no finding of publication bias among these five studies. A meta-analysis of multi-pollutant estimates from five studies [79, 80••, 81••, 82, 83] indicated no associations with PM10-2.5 after adjustment for PM2.5 (-1.2 %, 95 % CI: -5.1 to 2.8 % per 10 μg/m3). In contrast, PM2.5 associations were weakened after adjustment for PM10-2.5 (3.7 %, 95 % CI: 0 to 7.6 % per 10 μg/m3) but remained positive and statistically significant. Because there were only six studies identified, we did not investigate stratified analyses by study characteristics.
Fig. 5.
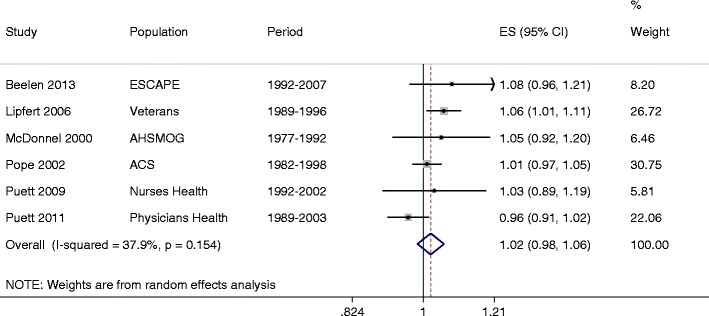
Summary of rate ratios between long-term exposure to PM10-2.5 and death per 10 μg/m3
Discussion
Although the health implications of PM10-2.5 remain far less characterized than those for PM2.5, there is a growing epidemiological literature for PM10-2.5. In this meta-analysis we identified 23 and 10 studies of short-term associations with mortality and hospitalizations, respectively, as well as 6 papers for long-term associations with mortality. Overall, we found suggestive evidence that higher short-term PM10-2.5 concentrations are associated with greater rates of mortality and hospitalizations, with the strongest relationships for respiratory endpoints. There was high heterogeneity in these estimates, however, with stronger associations suggested for European locations as compared to North America and weaker associations for locations with the highest PM10-2.5 levels. Adjustments for PM2.5 and asymmetry due to possible publication bias resulted in positive associations for PM10-2.5 that were weaker and less precise. Higher long-term exposures to PM10-2.5 were also associated with larger mortality in single pollutant models but these associations were eliminated by control for PM2.5. PM2.5 associations in these studies were less sensitive to control for PM10-2.5 and had less evidence of asymmetry.
PM10-2.5 may plausibly impact health given their deposition in the lungs, high biological content, and, in urban areas, high content of heavy metals.[86] Toxicological studies have provided evidence of the inflammatory effects of PM10-2.5, including some evidence that PM10-2.5 may be more inflammatory than PM2.5.[87–93] Controlled human exposure studies have similarly provided some evidence of acute alterations in markers of inflammation, coagulation, and autonomic tone although there was not consistent evidence of stronger associations with PM2.5.[94–99] Epidemiological data for subclinical endpoints with PM10-2.5 are still relatively sparse but there has been some evidence of biological activity including alterations in cytokines and coagulation factors, pulmonary function, respiratory symptoms, and cardiac function in some [96, 100–106] but not all studies.[104, 107–110] It should be noted, however, that even results from positive studies were often only suggestive and failed to meet statistical significance.
One possible explanation for the inconclusive nature of the literature pertains to the challenges of accurate exposure assessment for PM10-2.5. PM10-2.5 concentrations are often highly spatially and temporally variable as a consequence of higher deposition velocities as well as the intermittent nature of many PM10-2.5 sources.[2] For temporal trends, this has resulted in correlation coefficients between different sites that are generally lower than those reported for PM2.5 or PM10.[111] Concentrations have also been shown to vary across space based on proximity to different sources [112, 113], making long-term exposure assignment especially difficult given the limited numbers of monitoring stations with data to estimate PM10-2.5. In addition, most measurements of PM10-2.5 are indirect, estimated through subtraction of PM2.5 from PM10 concentrations measured at the same location. While past research has deemed this a reliable approach to estimating PM10-2.5 in urban areas [114], there are inherently errors due to the uncertainty of both filters. Even dichotomous samples for PM10-2.5, which are generally thought to have less error due to the use of a virtual impactor, may also have additional uncertainty due the small deposition of PM2.5 in the PM10-2.5 channel [115]. Similarly, continuous monitors such as the TEOM have been shown to be subject to measurement error if the losses of semi-volatile material are not properly accounted for [13]. Finally, infiltration rates for PM10-2.5 are quite low in comparison to PM2.5 and the presence of indoor sources are high, suggesting that ambient exposure may not accurately estimate personal exposure [116].
Although we only had limited data to investigate the impacts of measurement error on associations with health, we found some evidence of its importance with stronger associations among short-term concentrations measured using dichotomous samplers as compared to difference metrics, and weaker associations in studies using TEOMs as compared to other techniques. The three investigations using spatial prediction models to assess small-scale variability of long-term PM10-2.5 concentrations, however, did not consistently have stronger associations with mortality than other investigations relying only on central monitoring stations. Given these challenges for the measurement of PM10-2.5, we encourage researchers to be mindful of the methods used to assess exposure and report on the potential implications for their analyses. Epidemiological research is underway as part of the Colorado Course Rural Urban Sources and Health Study [117] for short-term exposures and the Multi-Ethnic Study of Atherosclerosis and Coarse Particulate Matter (MESA Coarse) [112] for long-term exposures that incorporates more accurate estimates of exposure, and thus should be subject to less measurement error.
Larger measurement error relative to PM2.5 may be a plausible explanation for the weakened associations for PM10-2.5 in two-pollutant models. First, the presence of greater classical measurement error is likely to result in a reduction of the point estimate towards the null. In addition, it has been hypothesized that a transfer of association from a variable with more measurement error to another with less error may occur in situations where there are substantial differences in the measurement error [118]. Another explanation is that confounding is present, although PM2.5 and PM10-2.5 concentrations only exhibited modest correlations in the incorporated studies (range: 0.0–0.7, median ~ 0.3). Furthermore, there was no consistent evidence of increasing associations for PM10-2.5 with increasing correlations between PM2.5 and PM10-2.5 concentrations when PM2.5 was associated with a worsening of health. Nor did we find consistent evidence of decreasing PM10-2.5 associations with increasing correlations between PM10-2.5 and PM2.5 concentrations when PM2.5 was found to be protective of health. Thus, while it may be compelling to assume that any observed associations with PM10-2.5 are due to PM2.5, our results do not support this as the sole explanation. Nevertheless, we encourage future investigations to continue exploring multi-pollutant models and reporting correlations between pollutants to better understand these complex relationships.
While it does not appear as though associations with PM10-2.5 are simply due to confounding by PM2.5, it remains possible that both PM2.5 and PM10-2.5 are acting as surrogates of a broader mixture of pollution. Thus, it may be that another unmeasured component or several components are the true causal factors. For example, in rural areas, gram-negative bacteria (as represented by bacterial-derived lipopolysaccharide or endotoxin) PM10-2.5 may be of special interest, especially for inflammatory mechanisms [87, 88, 97]. In urban areas, metals associated with roadway dust may be similarly important [89, 91, 119, 120]. The general lack of investigation of endotoxin levels, components of PM10-2.5, and multi-pollutant mixtures remains a weakness of the existing literature and an area for future development.
Along similar lines, it has been hypothesized that the toxicity of PM10-2.5 may be greater for particles originating in urban environments as compared to rural environments. Some evidence of such a relationship has been reported in 108 US counties [62••] and at least one toxicology study [88]. In this meta-analysis, we found evidence that PM10-2.5 associations with health were often weaker in regions with higher levels of PM10-2.5. This may suggest a non-linear dose response, as was reported in China [63••], or a difference in toxicity for more rural or arid regions. Weaker associations between PM10-2.5 and hospital admissions in regions with higher PM10-2.5/PM10 ratios may also support different toxicity by region, but the same pattern was not robust for morality. Interestingly, several investigators have attempted to distinguish toxicity of particulate matter from dust storms, but uncertainty remains around this question. Among those studies included in this meta-analysis, larger associations between short-term PM10-2.5 and health were reported on Saharan dust days in Rome [41, 59], whereas results with mortality in Madrid and Barcelona stratified by dust days were more mixed [31, 46]. While additional research may be needed from rural locations to inform this question, challenges will always remain unless speciated data is used, since anthropogenic and biological particles likely adhere to dust particles as they are transported through other airsheds.
Overall, this work adds to the literature by presenting the first meta-analysis results for PM10-2.5. With numerous new investigations in the literature, we also conducted stratified analyses to explore differences in associations with hospital admissions and mortality by various characteristics of the locations studied. As substantial heterogeneity was present among the associations presented, this represents an important area that requires further exploration in future investigations. In fact, it should be noted that the summary estimates reported in this analysis should be viewed with caution due to the presence of heterogeneity. Likewise, the observed heterogeneity suggests that the trim and fill method used to account for potential publication bias may be an overly conservative approach. While it may be challenging to fully characterize different personal characteristics that confer susceptibility, or components of the air pollution mixture that may lead to greater risk of morbidity and mortality in time-series studies, other designs not included in this investigation such as panel studies and controlled clinical studies have important contributions to make.
Conclusions
Suggestive evidence was observed for increased hospital admissions and mortality with higher levels of short-, but not long-term, PM10-2.5 concentrations. Relationships were generally stronger for respiratory endpoints, though associations with cardiovascular endpoints could not be excluded. Similarly, in spite of some sensitivity of the associations to control for PM2.5, our analysis suggests that associations with short-term exposures to PM10-2.5 cannot be fully explained by confounding by PM2.5. Additional research is still required to better understand sources of heterogeneity in associations, including co-exposure with other pollutants, sources, spatial variability, and composition of PM10-2.5, as well as individual susceptibilities.
Acknowledgments
This work was supported by supported by EPA STAR grants RD833741 and RD833744 as well as NIEHS P30ES017885. We also gratefully acknowledge Antonella Zanobetti, Brian Malig, Roger Peng, David Chock, and Leonardo Filigrana for their generosity with their data and/or time. We further thank Jason Sacks and Sung Kyun Park for sharing their insights on this work with us. Although supported in part by the EPA, this work has not been formally reviewed by the EPA, and the views in this document are solely those of the authors. The EPA does not endorse any products or commercial services mentioned.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Sara D. Adar, Paola A. Filigrana, Nicholas Clements, and Jennifer L. Peel declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Sara D. Adar, Phone: 734-615-9207, Email: sadar@umich.edu
Paola A. Filigrana, Phone: 734-730-4331, Email: paofilig@umich.edu
Nicholas Clements, Phone: (303)532-6546, Email: nsclements@gmail.com.
Jennifer L. Peel, Phone: 970-491-6391, Email: jennifer.peel@colostate.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manage Assoc. 2006;56:709–42. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 2.Lippmann M, Yeates DB, Albert RE. Deposition, retention, and clearance of inhaled particles. Br J Ind Med. 1980;37:337–62. doi: 10.1136/oem.37.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrison RM, Yin J. Particulate matter in the atmosphere: which particle properties are important for its effects on health? Sci Total Environ. 2000;249:85–101. doi: 10.1016/s0048-9697(99)00513-6. [DOI] [PubMed] [Google Scholar]
- 4.Pakkanen TA, Loukkola K, Korhonen CH, Aurela M, Mäkelä T, et al. Sources and chemical composition of atmospheric fine and coarse particles in the Helsinki area. Atmos Environ. 2001;35:5381–91. [Google Scholar]
- 5.USEPA . Integrated science assessment for particulate matter. Research Triangle Park: NCEA-RTP Office; 2009. [Google Scholar]
- 6.Brunekreef B, Forsberg B. Epidemiological evidence of effects of coarse airborne particles on health. Eur Respir J. 2005;26:309–18. doi: 10.1183/09031936.05.00001805. [DOI] [PubMed] [Google Scholar]
- 7.Lu Y, Zeger SL. On the equivalence of case-crossover and time series methods in environmental epidemiology. 2006. [DOI] [PubMed]
- 8.Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data - Referent selection strategies and their implications for bias. Epidemiology. 2005;16:717–26. doi: 10.1097/01.ede.0000181315.18836.9d. [DOI] [PubMed] [Google Scholar]
- 9.HEI. Revised analysis of selected time-series studies of air pollution and health. 2003. Spec Rep Health Eff Inst: 177–182.
- 10.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duval S, Tweedie R. Trim and fill: a simple funnel–plot–based method of testing and adjusting for publication bias in meta–analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 13.Clements N, Milford JB, Miller SL, Navidi W, Peel JL, et al. Errors in coarse particulate matter mass concentrations and spatiotemporal characteristics when using subtraction estimation methods. J Air Waste Manage Assoc. 2013;63:1386–98. doi: 10.1080/10962247.2013.816643. [DOI] [PubMed] [Google Scholar]
- 14.Lipfert FW, Morris SC, Wyzga RE. Daily mortality in the Philadelphia metropolitan area and size-classified particulate matter. J Air Waste Manag Assoc (Air Waste Manag Assoc) 2000;50:1501–13. doi: 10.1080/10473289.2000.10464185. [DOI] [PubMed] [Google Scholar]
- 15.Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, et al. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expo Anal Environ Epidemiol. 2005;15:153–9. doi: 10.1038/sj.jea.7500382. [DOI] [PubMed] [Google Scholar]
- 16.Jimenez E, Linares C, Martinez D, Diaz J. Particulate air pollution and short-term mortality due to specific causes among the elderly in Madrid (Spain): seasonal differences. Int J Environ Health Res. 2011;21:372–90. doi: 10.1080/09603123.2011.560251. [DOI] [PubMed] [Google Scholar]
- 17.Ostro BD, Broadwin R, Lipsett MJ. Coarse and fine particles and daily mortality in the Coachella Valley, California: a follow-up study. J Expo Anal Environ Epidemiol. 2000;10:412+. doi: 10.1038/sj.jea.7500094. [DOI] [PubMed] [Google Scholar]
- 18.Lippmann M, Ito K, Nadas A, Burnett R. Association of particulate matter components with daily mortality and morbidity in urban populations. 2000. Res Rep (Health Eff Inst): 5. [PubMed]
- 19.Klemm RJ, Mason RM, Jr, Heilig CM, Neas LM, Dockery DW. Is daily mortality associated specifically with fine particles? Data reconstruction and replication of analyses. J Air Waste Manag Assoc. 2000;50:1215–22. doi: 10.1080/10473289.2000.10464149. [DOI] [PubMed] [Google Scholar]
- 20.Fairley D. Daily mortality and air pollution in Santa Clara County, California: 1989-1996. Environ Health Perspect. 1999;107:637. doi: 10.1289/ehp.99107637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specifically with fine particles? J Air Waste Manage Assoc. 1996;46:927–39. [PubMed] [Google Scholar]
- 22.Burnett R, Brook J, Dann T, Delocla C, Philips O, et al. Association between particulate-and gas-phase components of urban air pollution and daily mortality in eight Canadian cities. Inhal Toxicol. 2000;12:15–39. doi: 10.1080/08958370050164851. [DOI] [PubMed] [Google Scholar]
- 23.Mar TF, Norris GA, Koenig JQ, Larson TV. Associations between air pollution and mortality in Phoenix, 1995-1997. Environ Health Perspect. 2000;108:347–53. doi: 10.1289/ehp.00108347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson HR, Bremner SA, Atkinson RW, Harrison RM, Walters S. Particulate matter and daily mortality and hospital admissions in the west midlands conurbation of the United Kingdom: associations with fine and coarse particles, black smoke and sulphate. Occup Environ Med. 2001;58:504–10. doi: 10.1136/oem.58.8.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castillejos VHB-A, Dockery DW, Gold DR, Loomis D, Margarita Airborne coarse particles and mortality. Inhal Toxicol. 2000;12:61–72. [Google Scholar]
- 26.Perez L, Medina-Ramón M, Kunzli N, Alastuey A, Pey J, et al. Size fractionate particulate matter, vehicle traffic, and case-specific daily mortality in Barcelona, Spain. Environ Sci Technol. 2009;43:4707–14. doi: 10.1021/es8031488. [DOI] [PubMed] [Google Scholar]
- 27.Kan H, London SJ, Chen G, Zhang Y, Song G, et al. Differentiating the effects of fine and coarse particles on daily mortality in Shanghai, China. Environ Int. 2007;33:376–84. doi: 10.1016/j.envint.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson WE, Mar TF, Koenig JQ. Influence of exposure error and effect modi. cation by socioeconomic status on the association of acute cardiovascular mortality with particulate matter in Phoenix. J Expo Sci Environ Epidemiol. 2007;17:S11–9. doi: 10.1038/sj.jes.7500620. [DOI] [PubMed] [Google Scholar]
- 29.Kettunen J, Lanki T, Tittanen P, Aalto PP, Koskentalo T, et al. Associations of fine and ultrafine particulate air pollution with stroke mortality in an area of low air pollution levels. Stroke. 2007;38:918–22. [DOI] [PubMed]
- 30.Perez L, Tobias A, Querol X, Kunzli N, Pey J, et al. Coarse particles from Saharan dust and daily mortality. Epidemiology. 2008;19:800–7. doi: 10.1097/ede.0b013e31818131cf. [DOI] [PubMed] [Google Scholar]
- 31.Tobias A, Perez L, Diaz J, Linares C, Pey J, et al. Short-term effects of particulate matter on total mortality during Saharan dust outbreaks: a case-crossover analysis in Madrid (Spain) Sci Total Environ. 2011;412:386–9. doi: 10.1016/j.scitotenv.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 32.Cifuentes LA, Vega J, Köpfer K, Lave LB. Effect of the fine fraction of particulate matter versus the coarse mass and other pollutants on daily mortality in Santiago, Chile. J Air Waste Manage Assoc. 2000;50:1287–98. doi: 10.1080/10473289.2000.10464167. [DOI] [PubMed] [Google Scholar]
- 32.••.Zanobetti A, Schwartz J. The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect. 2009;117:898–903. doi: 10.1289/ehp.0800108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Villeneuve PJ, Burnett RT, Shi Y, Krewski D, Goldberg MS, et al. A time-series study of air pollution, socioeconomic status, and mortality in Vancouver, Canada. J Expo Anal Environ Epidemiol. 2003;13:427. doi: 10.1038/sj.jea.7500292. [DOI] [PubMed] [Google Scholar]
- 35.Malig BJ, Ostro BD. Coarse particles and mortality: evidence from a multi-city study in California. Occup Environ Med. 2009;66:832–9. doi: 10.1136/oem.2008.045393. [DOI] [PubMed] [Google Scholar]
- 35.••.Chen R, Li Y, Ma Y, Pan G, Zeng G, et al. Coarse particles and mortality in three Chinese cities: the China Air Pollution and Health Effects Study (CAPES) Sci Total Environ. 2011;409:4934–8. doi: 10.1016/j.scitotenv.2011.08.058. [DOI] [PubMed] [Google Scholar]
- 37.López-Villarrubia E, Iñiguez C, Peral N, García MD, Ballester F. Characterizing mortality effects of particulate matter size fractions in the two capital cities of the Canary Islands. Environ Res. 2012;112:129–38. doi: 10.1016/j.envres.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 38.Janssen NAH, Fischer P, Marra M, Ameling C, Cassee FR. Short-term effects of PM2.5, PM10 and PM2.5–10 on daily mortality in the Netherlands. Sci Total Environ. 2013;463–464:20–6. doi: 10.1016/j.scitotenv.2013.05.062. [DOI] [PubMed] [Google Scholar]
- 38.••.Samoli E, Stafoggia M, Rodopoulou S, Ostro B, Declercq C, et al. Associations between fine and coarse particles and mortality in Mediterranean cities: results from the MED-PARTICLES Project. Environ Health Perspect. 2013;121:932–8. doi: 10.1289/ehp.1206124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meister K, Johansson C, Forsberg B. Estimated short-term effects of coarse particles on daily mortality in Stockholm, Sweden. Environ Health Perspect. 2012;120:431–6. doi: 10.1289/ehp.1103995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mallone S, Stafoggia M, Faustini A, Gobbi GP, Marconi A, et al. Saharan dust and associations between particulate matter and daily mortality in Rome, Italy. Environ Health Perspect. 2011;119:1409–14. doi: 10.12989/ehp.1003026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Atkinson RW, Fuller GW, Anderson HR, Harrison RM, Armstrong B. Urban ambient particle metrics and health: a time-series analysis. Epidemiology. 2010;21:501–11. doi: 10.1097/EDE.0b013e3181debc88. [DOI] [PubMed] [Google Scholar]
- 43.Burnett RT, Stieb D, Brook JR, Cakmak S, Dales R, et al. Associations between short-term changes in nitrogen dioxide and mortality in Canadian cities. Arch Environ Health Int J. 2004;59:228–36. doi: 10.3200/AEOH.59.5.228-236. [DOI] [PubMed] [Google Scholar]
- 44.Klemm R, Lipfert F, Wyzga R, Gust C. Daily mortality and air pollution in Atlanta: two years of data from ARIES. Inhal Toxicol. 2004;16:131–41. doi: 10.1080/08958370490443213. [DOI] [PubMed] [Google Scholar]
- 45.Chock DP, Winkler SL, Chen C. A study of the association between daily mortality and ambient air pollutant concentrations in Pittsburgh, Pennsylvania. J Air Waste Manage Assoc. 2000;50:1481–500. doi: 10.1080/10473289.2000.10464170. [DOI] [PubMed] [Google Scholar]
- 46.Perez L, Tobías A, Querol X, Pey J, Alastuey A, et al. Saharan dust, particulate matter and cause-specific mortality: a case–crossover study in Barcelona (Spain) Environ Int. 2012;48:150–5. doi: 10.1016/j.envint.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Halonen JI, Lanki T, Yli-Tuomi T, Tiittanen P, Kulmala M, et al. Particulate air pollution and acute cardiorespiratory hospital admissions and mortality among the elderly. Epidemiology. 2009;20:143–53. doi: 10.1097/EDE.0b013e31818c7237. [DOI] [PubMed] [Google Scholar]
- 48.Burnett RT, Cakmak S, Brook JR, Krewski D. The role of particulate size and chemistry in the association between summertime ambient air pollution and hospitalization for cardiorespiratory diseases. Environ Health Perspect. 1997;105:614–20. doi: 10.1289/ehp.97105614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health. 1999;54:130–9. doi: 10.1080/00039899909602248. [DOI] [PubMed] [Google Scholar]
- 50.Burnett RT, Smith-Doiron M, Stieb D, Raizenne ME, Brook JR, et al. Association between ozone and hospitalization for acute respiratory diseases in children less than 2 years of age. Am J Epidemiol. 2001;153:444–52. doi: 10.1093/aje/153.5.444. [DOI] [PubMed] [Google Scholar]
- 51.Lin M, Chen Y, Burnett RT, Villeneuve PJ, Krewski D. The influence of ambient coarse particulate matter on asthma hospitalization in children: case-crossover and time-series analyses. Environ Health Perspect. 2002;110:575–81. doi: 10.1289/ehp.02110575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tecer LH, Alagha O, Karaca F, Tuncel G, Eldes N. Particulate matter (PM2.5, p M10–2.5, and PM10) and children’s hospital admissions for asthma and respiratory diseases: a bidirectional case-crossover study. J Toxicol Environ Health A Curr Issues. 2008;71:512–20. doi: 10.1080/15287390801907459. [DOI] [PubMed] [Google Scholar]
- 53.Sheppard L, Levy D, Norris G, Larson TV, Koenig JQ. Effects of ambient air pollution on nonelderly asthma hospital admissions in Seattle, Washington, 1987-1994. Epidemiology. 1999;10:23–30. [PubMed] [Google Scholar]
- 54.Thurston GD, Ito K, Hayes CG, Bates DV, Lippmann M. Respiratory hospital admissions and summertime haze air pollution in Toronto, Ontario: consideration of the role of acid aerosols. Environ Res. 1994;65:271–90. doi: 10.1006/enrs.1994.1037. [DOI] [PubMed] [Google Scholar]
- 55.Fung KY, Khan S, Krewski D, Chen Y. Association between air pollution and multiple respiratory hospitalizations among the elderly in Vancouver, Canada. Inhal Toxicol. 2006;18:1005–11. doi: 10.1080/08958370600904538. [DOI] [PubMed] [Google Scholar]
- 56.Chang HH, Peng RD, Dominici F. Estimating the acute health effects of coarse particulate matter accounting for exposure measurement error. Biostatistics. 2011;12:637–52. doi: 10.1093/biostatistics/kxr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lin M, Stieb DM, Chen Y. Coarse particulate matter and hospitalization for respiratory infections in children younger than 15 years in Toronto: a case-crossover analysis. Pediatrics. 2005;116:E235–40. doi: 10.1542/peds.2004-2012. [DOI] [PubMed] [Google Scholar]
- 58.Chen Y, Yang Q, Krewski D, Shi Y, Burnett RT, et al. Influence of relatively low level of particulate air pollution on hospitalization for COPD in elderly people. Inhal Toxicol. 2004;16:21–5. doi: 10.1080/08958370490258129. [DOI] [PubMed] [Google Scholar]
- 59.Alessandrini ER, Stafoggia M, Faustini A, Gobbi GP, Forastiere F. Saharan dust and the association between particulate matter and daily hospitalisations in Rome, Italy. Occup Environ Med. 2013;70:432–4. doi: 10.1136/oemed-2012-101182. [DOI] [PubMed] [Google Scholar]
- 60.Chen Y, Yang Q, Krewski D, Burnett RT, Shi Y, et al. The effect of coarse ambient particulate matter on first, second, and overall hospital admissions for respiratory disease among the elderly. Inhal Toxicol. 2005;17:649–55. doi: 10.1080/08958370500189420. [DOI] [PubMed] [Google Scholar]
- 61.Host S, Larrieu S, Pascal L, Blanchard M, Declercq C, et al. Short-term associations between fine and coarse particles and hospital admissions for cardiorespiratory diseases in six French cities. Occup Environ Med. 2008;65:544–51. doi: 10.1136/oem.2007.036194. [DOI] [PubMed] [Google Scholar]
- 61.••.Peng RD, Chang HH, Bell ML, McDermott A, Zeger SL, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among medicare patients. JAMA J Am Med Assoc. 2008;299:2172–9. This analysis of Medicare patients across the United States was highly influential on the summary estimates for short-term associations between PM10-2.5 and hospital admissions for respiratory and cardiovascular causes. [DOI] [PMC free article] [PubMed]
- 62.••.Qiu H, Yu ITS, Tian LW, Wang XR, Tse LA, et al. Effects of coarse particulate matter on emergency hospital admissions for respiratory diseases: a time-series analysis in Hong Kong. Environ Health Perspect. 2012;120:572–6. This analysis of the from Hong Kong was highly influential on the summary estiamtes for short-term associations between PM10-2.5 and hosptial admissions for respiratory and cardiovascular causes. [DOI] [PMC free article] [PubMed]
- 64.Yang Q, Chen Y, Krewski D, Shi Y, Burnett RT, et al. Association between particulate air pollution and first hospital admission for childhood respiratory illness in Vancouver, Canada. Arch Environ Health Int J. 2004;59:14–21. doi: 10.3200/AEOH.59.1.14-21. [DOI] [PubMed] [Google Scholar]
- 64.•.Stafoggia M, Samoli E, Alessandrini E, Cadum E, Ostro B, et al. Short-term associations between fine and coarse particulate matter and hospitalizations in Southern Europe: results from the MED-PARTICLES Project. Environ Health Perspect. 2013;121:1026–33. This analysis from six European metropolitan areas was highly influential on the summary estimate for short-term associations between PM10-2.5 and CVD hospital admissions. [DOI] [PMC free article] [PubMed]
- 66.Qiu H, Yu IT-s, Wang X, Tian L, Tse LA, et al. Differential effects of fine and coarse particles on daily emergency cardiovascular hospitalizations in Hong Kong. Atmos Environ. 2013;64:296–302. [Google Scholar]
- 67.Tolbert PE, Klein M, Peel JL, Sarnat SE, Sarnat JA. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J Expo Sci Environ Epidemiol. 2007;17:S29–35. doi: 10.1038/sj.jes.7500625. [DOI] [PubMed] [Google Scholar]
- 68.Halonen JI, Lanki T, Yli-Tuomi T, Kulmala M, Tiittanen P, et al. Urban air pollution, and asthma and COPD hospital emergency room visits. Thorax. 2008;63:635–41. doi: 10.1136/thx.2007.091371. [DOI] [PubMed] [Google Scholar]
- 69.Ilabaca M, Olaeta I, Campos E, Villaire J, Tellez-Rojo MM, et al. Association between levels of fine particulate and emergency visits for pneumonia and other respiratory illnesses among children in Santiago, Chile. J Air Waste Manage Assoc. 1999;49:154–63. doi: 10.1080/10473289.1999.10463879. [DOI] [PubMed] [Google Scholar]
- 70.Malig BJ, Green S, Basu R, Broadwin R. Coarse particles and respiratory emergency department visits in California. Am J Epidemiol. 2013;178:58–69. doi: 10.1093/aje/kws451. [DOI] [PubMed] [Google Scholar]
- 71.Martinelli N, Girelli D, Cigolini D, Sandri M, Ricci G, et al. Access rate to the emergency department for venous thromboembolism in relationship with coarse and fine particulate matter air pollution. 2012. Plos One 7. [DOI] [PMC free article] [PubMed]
- 72.Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16:164–74. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- 73.Metzger KB, Tolbert PE, Klein M, Peel JL, Flanders WD, et al. Ambient air pollution and cardiovascular emergency department visits. Epidemiology. 2004;15:46–56. doi: 10.1097/01.EDE.0000101748.28283.97. [DOI] [PubMed] [Google Scholar]
- 74.Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med. 2010;182:307. doi: 10.1164/rccm.200908-1201OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang X, Chen R, Meng X, Geng F, Wang C, et al. Associations between fine particle, coarse particle, black carbon and hospital visits in a Chinese city. Sci Total Environ. 2013;458–460:1–6. doi: 10.1016/j.scitotenv.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 76.Tam WWS, Wong TW, Wong AHS. Effect of dust storm events on daily emergency admissions for cardiovascular diseases. Circ J. 2012;76:655–60. doi: 10.1253/circj.cj-11-0894. [DOI] [PubMed] [Google Scholar]
- 77.NYDoH. A study of ambient air contaminants and asthma in New York City: air contaminants and emergency department visits for asthma in the Bronx and Manhattan. http://purl.access.gpo.gov/GPO/LPS88357: New York Department of Health; 2006.
- 77.••.Pope 3rd CA, Burnett RT, Thun MJ, Calle EE, Krewski D, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287:1132–41. This analysis of the American Cancer Society Cancer Prevention Study II was highly influential on the summary estimate for long-term associations between PM10-2.5 and mortality. [DOI] [PMC free article] [PubMed]
- 79.Puett RC, Hart JE, Yanosky JD, Paciorek C, Schwartz J, et al. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the nurses’ health study. Environ Health Perspect. 2009;117:1697–701. doi: 10.1289/ehp.0900572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.••.Puett RC, Hart JE, Suh H, Mittleman M, Laden F. Particulate matter exposures, mortality, and cardiovascular disease in the health professionals follow-up study. Environ Health Perspect. 2011;119:1130. This analysis of the Physician’s Health Study was highly influential on the summary estimate for long-term associations between PM10-2.5 and mortality. [DOI] [PMC free article] [PubMed]
- 80.••.Lipfert F, Wyzga R, Baty J, Miller J. Traffic density as a surrogate measure of environmental exposures in studies of air pollution health effects: Long-term mortality in a cohort of US veterans. Atmos Environ. 2006;40:154–69. This cohort study of United States Veterans was highly influential on the summary estimate for long-term associations between PM10-2.5 and mortality.
- 82.McDonnell WF, Nishino-Ishikawa N, Petersen FF, Chen LH, Abbey DE. Relationships of mortality with the fine and coarse fractions of long-term ambient PM10 concentrations in nonsmokers. J Expo Anal Environ Epidemiol. 2000;10:427–36. doi: 10.1038/sj.jea.7500095. [DOI] [PubMed] [Google Scholar]
- 83.Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. [DOI] [PubMed]
- 84.Son J-Y, Bell ML, Lee J-T. Survival analysis of long-term exposure to different sizes of airborne particulate matter and risk of infant mortality using a birth cohort in Seoul, Korea. Environ Health Perspect. 2011;119:725–30. doi: 10.1289/ehp.1002364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen LH, Knutsen SF, Shavlik D, Beeson WL, Petersen F, et al. The association between fatal coronary heart disease and ambient particulate air pollution: are females at greater risk? Environ Health Perspect. 2005;113:1723–9. doi: 10.1289/ehp.8190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.U.S. Environmental Protection Agency. Integrated Science Assessment for Particulate Matter. In: Agency USEP, editor. Washington, DC.; 2009. [PubMed]
- 87.Monn C, Becker S. Cytotoxicity and induction of proinflammatory cytokines from human monocytes exposed to fine (PM2.5) and coarse particles (PM10-2.5) in outdoor and indoor air. Toxicol Appl Pharmacol. 1999;155:245–52. doi: 10.1006/taap.1998.8591. [DOI] [PubMed] [Google Scholar]
- 88.Schins RPF, Lightbody JH, Borm PJA, Shi TM, Donaldson K, et al. Inflammatory effects of coarse and fine particulate matter in relation to chemical and biological constituents. Toxicol Appl Pharmacol. 2004;195:1–11. doi: 10.1016/j.taap.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 89.Gerlofs-Nijland ME, Rummelhard M, Boere AJF, Leseman DLAC, Duffin R, et al. Particle induced toxicity in relation to transition metal and polycyclic aromatic hydrocarbon contents. Environ Sci Technol. 2009;43:4729–36. doi: 10.1021/es803176k. [DOI] [PubMed] [Google Scholar]
- 90.Becker S, Soukup JM, Sioutas C, Cassee FR. Response of human alveolar macrophages to ultrafine, fine, and coarse urban air pollution particles. Exp Lung Res. 2003;29:29–44. doi: 10.1080/01902140303762. [DOI] [PubMed] [Google Scholar]
- 91.Happo M, Salonen R, Hälinen A, Jalava P, Pennanen A, et al. Inflammation and tissue damage in mouse lung by single and repeated dosing of urban air coarse and fine particles collected from six European cities. Inhal Toxicol. 2010;22:402–16. doi: 10.3109/08958370903527908. [DOI] [PubMed] [Google Scholar]
- 92.Happo M, Salonen R, Hälinen A, Jalava P, Pennanen A, et al. Dose and time dependency of inflammatory responses in the mouse lung to urban air coarse, fine, and ultrafine particles from six European cities. Inhal Toxicol. 2007;19:227–46. doi: 10.1080/08958370601067897. [DOI] [PubMed] [Google Scholar]
- 93.Tong H, Cheng W-Y, Samet JM, Gilmour MI, Devlin RB. Differential cardiopulmonary effects of size-fractionated ambient particulate matter in mice. Cardiovasc Toxicol. 2010;10:259–67. doi: 10.1007/s12012-010-9082-y. [DOI] [PubMed] [Google Scholar]
- 94.Behbod B, Urch B, Speck M, Scott JA, Liu L, et al. Endotoxin in concentrated coarse and fine ambient particles induces acute systemic inflammation in controlled human exposures. Occup Environ Med. 2013;70:761–7. doi: 10.1136/oemed-2013-101498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bellavia A, Urch B, Speck M, Brook RD, Scott JA, et al. DNA hypomethylation, ambient particulate matter, and increased blood pressure: findings from controlled human exposure experiments. 2013. J Am Heart Assoc 2. [DOI] [PMC free article] [PubMed]
- 96.Graff DW, Cascio WE, Rappold A, Zhou HB, Huang YCT, et al. Exposure to concentrated coarse air pollution particles causes mild cardiopulmonary effects in healthy young adults. Environ Health Perspect. 2009;117:1089–94. doi: 10.1289/ehp0900558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Alexis NE, Lay JC, Zeman K, Bennett WE, Peden DB, et al. Biological material on inhaled coarse fraction particulate matter activates airway phagocytes in vivo in healthy volunteers. J Allergy Clin Immunol. 2006;117:1396–403. doi: 10.1016/j.jaci.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 98.Samet JM, Graff D, Berntsen J, Ghio AJ, Huang Y-CT, et al. A comparison of studies on the effects of controlled exposure to fine, coarse and ultrafine ambient particulate matter from a single location. Inhal Toxicol. 2007;19:29–32. doi: 10.1080/08958370701492706. [DOI] [PubMed] [Google Scholar]
- 99.Gong H, Jr, Linn WS, Terrell SL, Clark KW, Geller MD, et al. Altered heart-rate variability in asthmatic and healthy volunteers exposed to concentrated ambient coarse particles. Inhal Toxicol. 2004;16:335–43. doi: 10.1080/08958370490439470. [DOI] [PubMed] [Google Scholar]
- 100.Bonzini M, Tripodi A, Artoni A, Tarantini L, Marinelli B, et al. Effects of inhalable particulate matter on blood coagulation. J Thromb Haemost. 2010;8:662–8. doi: 10.1111/j.1538-7836.2009.03694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yeatts K, Svendsen E, Creason J, Alexis N, Herbst M, et al. Coarse particulate matter (PM2.5-10) affects heart rate variability, blood lipids, and circulating eosinophils in adults with asthma. Environ Health Perspect. 2007;115:709–14. doi: 10.1289/ehp.9499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Peters A, Greven S, Heid IM, Baldari F, Breitner S, et al. Fibrinogen genes modify the fibrinogen response to ambient particulate matter. Am J Respir Crit Care Med. 2009;179:484–91. doi: 10.1164/rccm.200805-751OC. [DOI] [PubMed] [Google Scholar]
- 103.Delfino RJ, Staimer N, Tjoa T, Polidori A, Arhami M, et al. Circulating biomarkers of inflammation, antioxidant activity, and platelet activation are associated with primary combustion aerosols in subjects with coronary artery disease. Environ Health Perspect. 2008;116:898. doi: 10.1289/ehp.11189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schwartz J, Neas LM. Fine particles are more strongly associated than coarse particles with acute respiratory health effects in schoolchildren. Epidemiology. 2000;11:6–10. doi: 10.1097/00001648-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 105.Metzger KB, Klein M, Flanders WD, Peel JL, Mulholland JA, et al. Ambient air pollution and cardiac arrhythmias in patients with implantable defibrillators. Epidemiology. 2007;18:585–92. doi: 10.1097/EDE.0b013e318124ff0e. [DOI] [PubMed] [Google Scholar]
- 106.Ebelt ST, Wilson WE, Brauer M. Exposure to ambient and nonambient components of particulate matter: a comparison of health effects. Epidemiology. 2005;16:396–405. doi: 10.1097/01.ede.0000158918.57071.3e. [DOI] [PubMed] [Google Scholar]
- 107.Gold DR, Litonjua A, Schwartz J, Lovett E, Larson A, et al. Ambient pollution and heart rate variability. Circulation. 2000;101:1267–73. doi: 10.1161/01.cir.101.11.1267. [DOI] [PubMed] [Google Scholar]
- 108.Liao D, Creason J, Shy C, Williams R, Watts R, et al. Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Environ Health Perspect. 1999;107:521–5. doi: 10.1289/ehp.99107521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Timonen KL, Vanninen E, De Hartog J, Ibald-Mulli A, Brunekreef B, et al. Effects of ultrafine and fine particulate and gaseous air pollution on cardiac autonomic control in subjects with coronary artery disease: the ULTRA study. J Expo Sci Environ Epidemiol. 2006;16:332–41. doi: 10.1038/sj.jea.7500460. [DOI] [PubMed] [Google Scholar]
- 110.Pekkanen J, Peters A, Hoek G, Tiittanen P, Brunekreef B, et al. Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: the Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air (ULTRA) study. Circulation. 2002;106:933–8. doi: 10.1161/01.cir.0000027561.41736.3c. [DOI] [PubMed] [Google Scholar]
- 111.Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manage Assoc. 1997;47:1238–49. doi: 10.1080/10473289.1997.10464074. [DOI] [PubMed] [Google Scholar]
- 112.Zhang K, Larson TV, Gassett A, Szpiro AA, Daviglus M, et al. Characterizing spatial patterns of airborne coarse particulate (PM10-2.5) mass and chemical components in three cities: the multi-ethnic study of atherosclerosis. 2014. Environ Health Perspect. 2014;122(7). doi:10.1289/ehp.1307287. [DOI] [PMC free article] [PubMed]
- 113.Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, et al. Development of land use regression models for PM2. 5, PM2. 5 absorbance, PM10 and PMcoarse in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46:11195–205. doi: 10.1021/es301948k. [DOI] [PubMed] [Google Scholar]
- 114.Vanderpool RW ET, Harmon MK, Hanley TD, Scheffe RD, Hunike ET, Solomon PA et al. Multi-site evaluations of candidate methodologies for determining coarse Pariculate Matter (PMc) Concentrations; 2004 April 13–16; Tampa, Florida.
- 115.Turner JR, Brown SG, Pasch AN, Roberts PT, Inc. ST. Interim Report on Data Analyses for the EPA Coarse PM Speciation Pilot Project. Draft. Interim Report STI-910203-4222-WEB. . Prepared for Joann Rice, U.S. Environmental Protection Agency, Office of Air Quality Planning and Standards. 2011.
- 116.Sarnat SE, Coull BA, Ruiz PA, Koutrakis P, Suh HH. The influences of ambient particle composition and size on particle infiltration in Los Angeles, CA, residences. J Air Waste Manage Assoc. 2006;56:186–96. doi: 10.1080/10473289.2006.10464449. [DOI] [PubMed] [Google Scholar]
- 117.Clements N, Piedrahita R, Ortega J, Peel JL, Hannigan M, et al. Characterization and nonparametric regression of rural and urban coarse particulate matter mass concentrations in Northeastern Colorado. Aerosol Sci Technol. 2012;46:108–23. [Google Scholar]
- 118.Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108:419. doi: 10.1289/ehp.00108419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lippmann M, Chen L-C. Health effects of concentrated ambient air particulate matter (CAPs) and its components. Crit Rev Toxicol. 2009;39:865–913. doi: 10.3109/10408440903300080. [DOI] [PubMed] [Google Scholar]
- 120.Gerlofs-Nijland ME, Dormans JA, Bloemen HJ, Leseman DL, Boere AJF, et al. Toxicity of coarse and fine particulate matter from sites with contrasting traffic profiles. Inhal Toxicol. 2007;19:1055–69. doi: 10.1080/08958370701626261. [DOI] [PubMed] [Google Scholar]


