Abstract
Background
Buprenorphine is a promising treatment for heroin addiction. However, little is known regarding its provision to pre-release prisoners with heroin dependence histories who were not opioid-tolerant, the relative effectiveness of the post-release setting in which it is provided, and gender differences in treatment outcome in this population.
Methods
This is the first randomized clinical trial of prison-initiated buprenorphine provided to male and female inmates in the US who were previously heroin-dependent prior to incarceration. A total of 211 participants with 3–9 months remaining in prison were randomized to one of four conditions formed by crossing In-Prison Treatment Condition (received buprenorphine vs. counseling only) and Post-release Service Setting (at an opioid treatment center vs. a community health center). Outcome measures were: entered prison treatment; completed prison treatment; and entered community treatment 10 days post-release.
Results
There was a significant main effect (p=.006) for entering prison treatment favoring the In-Prison buprenorphine Treatment Condition (99.0% vs. 80.4%). Regarding completing prison treatment, the only significant effect was Gender, with women significantly (p<.001) more likely to complete than men (85.7% vs. 52.7%). There was a significant main effect (p=.012) for community treatment entry, favoring the In-Prison buprenorphine Treatment Condition (47.5% vs. 33.7%).
Conclusions
Buprenorphine appears feasible and acceptable to prisoners who were not opioid-tolerant and can facilitate community treatment entry. However, concerns remain with in-prison treatment termination due to attempted diversion of medication.
Keywords: Heroin, Buprenorphine, Prison, Opioid Dependence, Opioid Use Disorder, Correctional Settings
1. INTRODUCTION
Incarcerated individuals in the United States (US), Australia, and in many European and Asian nations have disproportionately higher rates of heroin addiction than the general population (Dolan et al., 2007; Fazel et al., 2006; Kinlock et al., 2011). In the US, an estimated 12–15% of incarcerated individuals have pre-incarceration heroin addiction, compared to less than 1% of the general population (Mumola and Karberg, 2006). However, many inmates with heroin addiction histories remain untreated in prison (Kastelic et al., 2008; Stover and Michels, 2010; Taxman et al., 2007). As a consequence, heroin addiction continues or resumes rapidly following release from incarceration (Dolan et al., 2007; Kinlock et al., 2011; Strang et al., 2006) and it contributes to high rates of HIV and hepatitis infection (Dolan et al., 2007; Kanato, 2008), overdose death among newly released inmates (Binswanger et al., 2011, 2012; Krinsky et al., 2009; Merral et al., 2010), increased criminal activity (Kinlock et al., 2003; Inciardi, 2008), and re-incarceration (Dolan et al., 2005; Metz et al., 2010). Thus, increased access to effective treatment interventions that begin during incarceration and continue in the community are needed for inmates with heroin addiction histories (Chandler et al., 2009; Dolan et al., 2007; Kinlock et al., 2011).
1.1. Buprenorphine for general populations
Buprenorphine, approved for the treatment of opioid dependence in the US in 2002, has several advantages over methadone: less associated stigma; lower risk of overdose (Mattick et al., 2009); and fewer regulations, which allow its use outside opioid treatment programs (Dasgupta et al., 2010). Although buprenorphine, as a partial agonist that has a longer duration to peak effect compared to morphine, which is useful for treating opioid dependence, as an opioid drug, it has potential for abuse (Tompkins and Strain, 2011). The buprenorphine/naloxone combination lowers the likelihood of intravenous abuse because injected naloxone can precipitate opioid withdrawal (Tompkins and Strain, 2011). Buprenorphine has been safely and effectively implemented in various community settings: opioid treatment programs, non-methadone outpatient programs, community health centers, and medical practices (Miotto et al., 2012; Mitchell et al., 2012). In community settings, it has been effective in reducing heroin use and retaining patients in treatment (Alford et al., 2011; Mattick et al., 2009; Miotto et al., 2012; Mitchell et al, 2012).
1.2. Buprenorphine in correctional settings
Observational examinations of buprenorphine in correctional settings in France (buprenorphine mono product; Levasseur et al., 2002) and Puerto Rico and New York City (buprenorphine/naloxone; Garcia et al., 2007, Lee et al., 2012) respectively found that it was feasible and facilitated community-based treatment entry. Garcia et al. (2007) reported that of 50 inmates eligible for study participation, 5 refused; all 45 consenting participants initiated buprenorphine treatment in prison; 42 of 45 (93.3%) completed treatment until release, with 35 (77.8%) entering community treatment. Garcia et al. further reported that buprenorphine treatment reduced heroin use at 1-month post-release; Lee et al. (2012) reported that jail-initiated buprenorphine patients had similar rates of treatment retention and opioid-positive urine test results to community-initiated patients at 48 weeks. A randomized clinical trial comparing buprenorphine and methadone among male, heroin-dependent newly-admitted jail inmates in New York City found that while treatment completion rates in jail were similar, buprenorphine patients were significantly more likely to enter community-based treatment (Magura et al., 2009). However, buprenorphine patients were significantly more likely than methadone patients to be terminated from treatment in prison for attempted diversion of medication. Finally, Zaller et al. (2013) conducted a small-scale (n=44) feasibility study with buprenorphine/naloxone for Rhode Island prisoners who were previously, but not currently opioid-tolerant, with the intention to initiate medication up to two weeks before anticipated release. Because 32 inmates were released earlier than expected, Zaller and colleagues compared community-treatment entry and retention for these 32 who did not receive buprenorphine/naloxone in prison to 12 who began induction while incarcerated. Both outcomes number of days to first treatment post release (Mean=3.9 vs. Mean=9.2) and remained in care for the entire six-months (83% vs. 34%) favored the group that initiated buprenorphine/naloxone in prison.
1.3. Need for further research with incarcerated populations
Although Magura et al. (2009) noted that their results were encouraging, they emphasized that “a larger clinical trial of buprenorphine in a different setting with both genders would be a useful avenue for further research” (p. 228). Setting is important also because, unlike newly-incarcerated jail inmates in the US and longer-term prisoners in some other countries, most prisoners with pre-incarceration heroin dependence in the United States may not be regularly using heroin in prison (Kinlock et al., 2011); nearly all participants in studies cited in Section 1.2 except for Zaller et al. (2013) were opioid-tolerant when medication began. Consequently, it is important to examine whether buprenorphine provided to non-opioid tolerant male and female prison inmates with heroin dependence histories would be feasible and would facilitate community-based substance abuse treatment entry. It is also critical to examine whether the setting in which community-based buprenorphine treatment is delivered to newly released inmates facilitates treatment entry (Lee et al., 2012; Stallwitz and Stover, 2007).
2. METHODS
The study was approved by the Friends Research Institute Institutional Review Board (IRB) on February 7, 2008, the Maryland Department of Public Safety and Correctional Services (DPSCS) research committee, and the US Office for Human Research Protections. The ClinicalTrials.gov identifier is NCT00574067. Buprenorphine-naloxone was donated by Reckitt-Benckiser Pharmaceuticals, Inc.
2.1. Rationale and Design
The present analyses were developed to address three unexplored issues that emerged from the review of the opioid agonist treatment literature for prisoners with heroin addiction histories: (1) the relative importance of providing buprenorphine/naloxone treatment prophylactically to previously-addicted prison inmates who are nearing release, compared to providing buprenorphine/naloxone after release; (2) the relative effectiveness of the setting in which post-release buprenorphine/naloxone treatment is provided; and, 3) gender differences regarding the effectiveness of the combination of the two treatment components. The emphases on the present analyses involve the extent to which there are treatment condition and gender differences in the earlier phases of the study (e.g., prison treatment entry, prison treatment completion, and community treatment entry within 10 days of release).
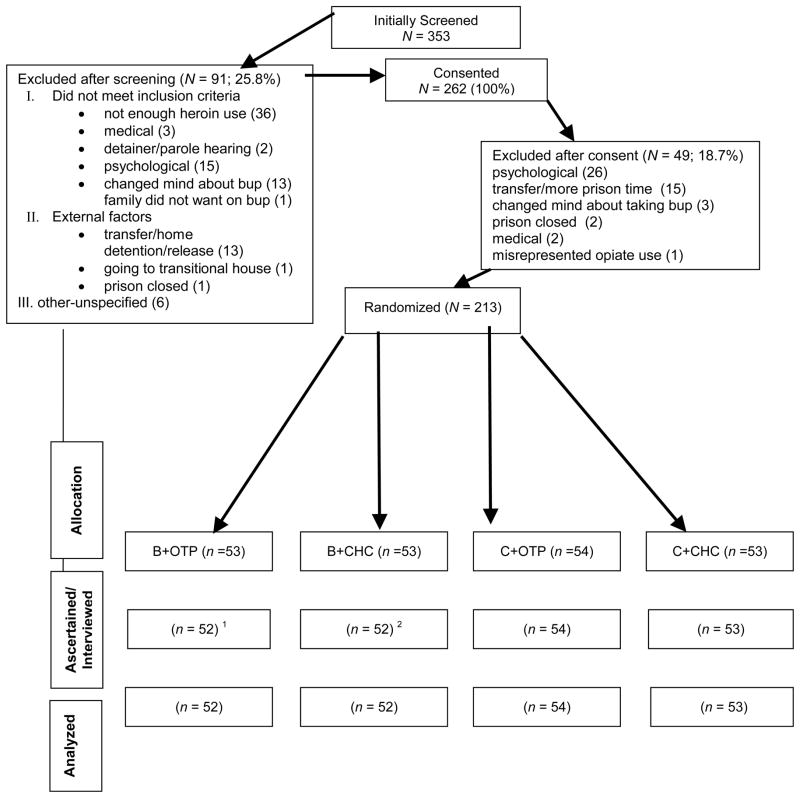
The design can be conceptualized as a 2 (In-Prison Treatment Condition: Buprenorphine treatment vs. counseling only) X 2 [Post-Release Service Setting: Opioid agonist maintenance treatment program (OTP) vs. community health center (CHC)] X 2 (Gender) factorial design. Imprisoned men and women with pre-incarceration heroin use disorders who were within 3–9 months of release and met criteria for buprenorphine treatment were randomly assigned by block randomization within gender to one of the four treatment conditions formed by crossing In-Prison Treatment Condition and Post-Release Service Setting (see Figure 1, Consort Diagram).
Figure 1.
Consort Diagram.
B+OTP: Buprenorphine in prison and continued at an Opioid Treatment Program (OTP)
B+CHC: Buprenorphine in prison and continued an a Community Health Center (CHC)
C+OTP: Counseling only in prison and initiation of buprenorphine at an OTP
C+CHC: Counseling only in prison and initiation of buprenorphine at a CHC
1 participant was randomized prior to the prison closure
2 participant mispresented opiate use
2.2. Participants
Study methods were described in detail previously (Kinlock et al., 2010). In summary, participants were recruited between September 2008 and July 2012 from Maryland prisons. Eligibility criteria were: 1) 3–9 months remaining in prison before anticipated release; 2) meeting Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria of heroin dependence at time of incarceration, being physiologically dependent during the year before incarceration; 3) suitable for buprenorphine/naloxone treatment, determined by medical examination; 4) willing to receive buprenorphine/naloxone treatment; and 5) residing in Baltimore City following release. Individuals who did not meet the heroin dependence criterion were eligible if they were enrolled in an OTP in the year before incarceration. Individuals with one or more of the following conditions were excluded from study participation: 1) kidney failure; 2) liver failure; 3) history of psychosis; 4) pending or unadjudicated charges that could have resulted in transfer to another correctional facility and/or additional prison time; 5) pending parole hearing; and 6) pregnancy.
Inmates were recruited by group orientation sessions and word-of-mouth. Inmates interested in enrolling were individually screened for participation by trained research assistants (RAs). RAs then met with individuals remaining eligible to review the study’s informed consent document; following consent, assessments, described below, were administered. Finally, it was determined whether each potential participant was medically eligible for buprenorphine/naloxone treatment based on results of a medical history, physical examination, and laboratory tests conducted under the direction of a study physician, the Medical Director of a Baltimore community-based OTP (Figure 1). As shown in Figure 1, of 353 inmates initially screened, 91 (25.8%) were excluded after screening; all of the remaining 262 (100%) consented; 49 of 262 (18.7%) were excluded after consent and 213 randomized. Of the 213 randomized, two were excluded from analysis, leaving a total of 211 participants.
2.3. Interventions in Prison
All participants received an individual intake assessment at study entry and a medical examination. Participants were also scheduled to receive 12 weekly group sessions provided by the study’s addiction counselor that involved relapse prevention, overdose prevention, overcoming barriers to community treatment entry, and obtaining post-release employment and housing, with participants receiving buprenorphine/naloxone in prison meeting separately from participants not receiving buprenorphine/naloxone in prison. Immediately before release, participants still in prison treatment were scheduled to meet with the study’s counselor individually to discuss re-entry plans. Study RAs met with each participant within two weeks of his/her release from prison to give the participant an appointment card with the address of the designated program (the OTP or CHC that he/she had to report to) and to reiterate that they had 10 days to attend.
2.3.1. Buprenorphine/naloxone Dosing
In-prison buprenorphine/naloxone treatment was provided by a community-based opioid treatment program physician and nursing staff. Daily dosing was scheduled to be administered by study nurses for the first 49 days (1 mg, days 1–7; 2 mg, days 8–14; 3 mg, days 15–21; 4 mg, days 22–28; 6 mg, days 29–35, 8 mg; days 36–49). Days 50 through 63 dosing was scheduled every other day at 16 mg (or twice the daily dose). From day 64 onward until release from incarceration, participants were scheduled to receive 16 mg (or twice the daily dose) on Mondays and Wednesdays and 20 mg (or 2.5 times the daily dose) on Fridays. Allowance was made to increase the Friday dose to 3 times the daily dose if needed. The every other day and three times weekly dosing schedules follow the demonstration that this is safe and effective among tolerant patients [Center for Substance Abuse Treatment (CSAT), 2004], and would be more convenient for participants, the correctional staff, and the medical staff. It should be noted that actual dosing was individualized according to participant needs. Dosage started low and increased slowly because nearly all participants were not tolerant to opioids (they were not using heroin or other opioids regularly) at study entry.
2.3.2. Diversion and Attempted Diversion of Buprenorphine
At the outset of treatment and consistently thereafter, the study’s medical staff informed participants in the buprenorphine In-Prison Treatment Condition that they would be terminated from treatment if they diverted or attempted to divert buprenorphine/naloxone. Throughout the study, we attempted various additional strategies to minimize the problem with attempted diversion including: a warning about treatment termination in the informed consent document; dividing the buprenorphine/naloxone tablets in quarters before administration to effect faster tablet dissolution; and subsequently, to switch the formulation from tablets to strips. Throughout most of this study buprenorphine/naloxone tablets were administered; however, because of incidents of attempted diversion of the tablets, the medication formulation was switched to the faster-dissolving buprenorphine/naloxone film strips (after their FDA-approval which was obtained while the study was ongoing) for the last 23 participants medicated in prison.
2.3.3. Release from prison
Upon anticipated release from incarceration, participants were advised by treatment staff and study RAs to report to their designated OTP or CHC as soon as possible. Participants were informed at study entry and immediately prior to their anticipated release by treatment staff that they would be guaranteed admission to the designated facility if they arrived within 10 business days of release from prison, and if they arrived at the particular OTP or CHC afterward, they would be subjected to the facility’s standard admission procedures, including possibly being placed on a waiting list. Participants designated to continue or begin buprenorphine/naloxone treatment at a CHC (which was not open on weekends) who were released on Fridays had the opportunity to be guest-dosed at the OTP over that weekend. No medication was dispensed to participants upon their release from prison.
2.4. Assessments/procedures
Assessments included demographic information and histories of drug abuse, drug abuse treatment, criminal activity, and criminal justice system involvement. Immediately following informed consent, measures administered included the Addiction Severity Index (ASI; McLellan et al., 1992). More detailed historical information about criminality, criminal justice sanctions, drug abuse, and drug abuse treatment than provided by the ASI were obtained from a supplemental self-report questionnaire similar to the UCLA Natural History Interview (NHI; see Murphy et al., 2010) based on previous research on heroin-dependent adults (Gordon et al., 2008; Nurco, 1998) and, like the NHI, modified from an instrument originally developed by Nurco et al (1975). [The essential validity and reliability of the ASI and NHI was summarized by Murphy et al., (2010).] In-prison treatment data including dosing days, doses administered, and counseling sessions attended were gathered from treatment records. Data from the one-month post-release follow-up version of this supplemental questionnaire relevant to this manuscript included whether participants entered any treatment program within 10 days of release other than the designated OTP or CHC.
2.5. Outcome measures
Three outcome measures (all yes v. no), defined as follows, were employed: 1) Entered prison treatment. This outcome was defined as, for the buprenorphine In-Prison Treatment Condition, whether or not the participant received at least one dose of buprenorphine/naloxone. For participants in counseling only In-Prison Treatment Condition, whether or not the participant met at least once with the study’s counselor. These data were recorded by treatment staff. 2) Completed prison treatment. This outcome was defined as, for the buprenorphine In-Prison Treatment Condition, whether or not the participant was receiving buprenorphine/naloxone treatment at the time of his/her release from prison; for participants in the counseling only In-Prison Treatment Condition, whether or not the participant was receiving weekly counseling or had completed 12 sessions of weekly counseling at the time of his/her release from prison. These data were recorded by treatment staff. 3) Entered community treatment. This outcome was defined as whether or not the participant entered treatment at his/her designated OTP or CHC (discussed above) as well as whether or not the participant entered treatment at any other substance abuse treatment program within 10 business days of release from prison. These data were obtained from the OTP and CHC; data on entry into any other substance abuse treatment programs were obtained from a one-month post-release follow-up version of the supplemental questionnaire mentioned earlier.
2.6. Hypothesis
Based on research evidence regarding the effectiveness of opioid agonist maintenance treatment in other settings, described above, our hypothesis is that the buprenorphine In-Prison Treatment Condition will have more favorable outcomes, regardless of post-release service setting, than will the counseling only In-Prison Treatment Condition.
2.7. Statistical analysis
The 211 participants were compared by treatment condition with regard to each outcome variable listed above using logistic regression analysis (Agresti, 1990; Hosmer and Lemeshow, 1989). Because the outcome entered prison treatment had few participants failing to enter such treatment, it was necessary to use bias correction to estimate parameters and conduct tests of significance. First bias correction is considered an ideal approach for the case in which there is complete or quasi-complete separation of data points (Heinze and Schemper, 2002). The explanatory variables in the model were: In-Prison Treatment Condition (buprenorphine treatment vs. counseling only), Post-Release Service Setting [opioid treatment program (OTP) vs. community health center (CHC)], Gender, and their interactions. Gender was included as a predictor variable in view of the need to examine differences in responsiveness to treatment by men and women. An alpha level of .05 was chosen to determine statistical significance.
3. RESULTS
3.1. Participant characteristics
Selected background characteristics by treatment condition are shown in Table 1. Most participants were male, African American, between 35 and 45 years of age, and completed less than 12 years of education. Whereas all participants had at least one prior incarceration, over four-fifths had at least one substance abuse treatment episode. However, fewer than one-third reported having undergone MMT; less than one in six participants reported having received buprenorphine/naloxone treatment. Participants, on average, initiated heroin use in their late teens, roughly five to seven years after their onset of criminal activity. During the 30 days before the index incarceration, participants reportedly used heroin and committed crime almost every day. Using chi-square tests of independence for categorical variables and t-tests for continuous variables, there were no significant (p<.05) differences between groups on the variables reported in Table 1. Participants, independent of treatment condition, were also compared by gender on the variables reported in Table 1. Women were significantly (p<.05) more likely to have undergone prior drug treatment than men (X2=10.7; 95.2 % vs. 76.4%); methadone maintenance treatment (X2 =37.7; 61.9% vs. 18.9%) and buprenorphine treatment (X2 =12.5; 28.6 vs. 9.5%). Men had significantly (p<.05) younger mean ages at first crime (t = 2.3; 13.1 vs. 15.2); first use of heroin (t = 2.3; 18.7 vs. 20.7); first arrest (t = 4.3; 17.1 vs. 22.6); and first incarceration (t = 4.4; 19.6 vs. 24.3). Women were also significantly younger (p<.05) than men at baseline assessment (t = −2.3; Mean ages = 37.0 vs. 40.0, respectively). Finally, men and women differed significantly (X2 = 9.7; p<.05) with regard to ethnicity, as 55.6% of the women were African American and 39.7% were white; for men, 76.4% were African American and 19.6% were white.
Table 1.
Selected background characteristics by treatment condition (N=211)
| B+OTP (n=52) | B+CHC (n=52) | C+OTP (n=54) | C+CHC (n=53) | Total Sample (N=211) | |
|---|---|---|---|---|---|
| Categorical Variables, n (%) | |||||
| Gender | |||||
| Female | 15 (28.9) | 17 (32.7) | 16 (29.6) | 15 (28.3) | 63 (29.9) |
| Male | 37 (71.2) | 35 (67.3) | 38 (70.4) | 38 (71.7) | 148 (70.1) |
| Race | |||||
| African American | 41 (78.9) | 30 (57.7) | 42 (77.8) | 35 (66.0) | 148(70.1) |
| Caucasian | 9 (17.3) | 20 (38.5) | 11 (20.4) | 14 (26.4) | 54(25.6) |
| Other | 2 (3.8) | 2 (3.9) | 1 (1.9) | 4(7.6) | 9(4.3) |
| Prior drug treatment | 40 (76.9) | 44 (84.6) | 46 (85.2) | 43 (81.1) | 173 (81.9) |
| Prior methadone treatment | 16 (30.8) | 22 (42.3) | 15 (27.8) | 14 (26.4) | 67(31.8) |
| Prior buprenorphine treatment | 7 (13.5) | 7 (13.5) | 6 (11.11) | 12 (22.6) | 32(15.2) |
|
| |||||
| Continuous Variables, M (SD)
| |||||
| Age | 39.15 (7.5) | 39.18 (8.7) | 39.55 (10.0) | 38.42 (9.1) | 39.08 (8.8) |
| Education | 11.06 (1.6) | 11.19 (1.7) | 10.96 (1.7) | 11.49 (1.7) | 11.18 (1.7) |
| Age first marijuana use | 14.33 (2.4) | 13.74 (3.1) | 16.12 (12.0) | 13.59 (2.5) | 14.45 (6.6) |
| Age first cocaine use | 21.02 (7.4) | 20.76 (7.6) | 21.37 (5.0) | 23.65 (13.2) | 21.70 (8.8) |
| Age first heroin use | 18.08 (5.9) | 20.08 (6.1) | 20.17 (6.2) | 18.85 (5.4) | 19.30 (5.9) |
| Age first crime | 13.59 (6.4) | 14.81 (8.5) | 13.04 (4.7) | 13.43 (4.4) | 13.71 (6.2) |
| Age first arrested | 19.58 (12.4) | 18.78 (6.9) | 18.72 (8.6) | 18.0 (5.6) | 18.77 (8.7) |
| Age first incarcerated | 20.37 (6.6) | 21.49 (7.2) | 21.72 (9.2) | 20.51 (6.9) | 21.02 (7.5) |
| Number of Prior incarcerations | 8.06 (6.4) | 8.86 (12.1) | 6.24 (3.7) | 6.34 (3.4) | 7.35 (7.2) |
| Heroin use daysa | 24.13 (10.0) | 24.21 (10.2) | 23.83 (11.0) | 25.60 (9.3) | 24.45 (10.1) |
| Cocaine use daysa | 9.69 (12.8) | 12.65 (12.9) | 13.50 (13.5) | 11.53 (13.2) | 11.86 (13.1) |
| Crime daysa | 19.85 (12.9) | 18.35 (12.8) | 19.48 (12.9) | 24.36 (15.3) | 20.53 (13.6) |
Past 30 days in the community prior to the current incarceration.
3.2. Entered prison treatment
Of all 211 participants, 189 (89.6%) entered prison treatment (Table 2). There was a significant main effect for type of in-prison treatment [χ2(df=1)=7.6; p=.006; adjusted odds ratio (AOR)=2.8; 95% CI=1.3, 5.7], with individuals in the buprenorphine In-Prison Treatment Condition significantly more likely than individuals in the counseling only In-Prison Treatment Condition to enter prison treatment. (99.0% v. 80.4%, respectively). No other effect in the model was significant (all ps > .05).
Table 2.
Number and Proportion of Participants Achieving Treatment Outcomes by Treatment Condition and Gender (N=211)
| Outcome | B+OTP | B+CHC | In-Prison Buprenorphine |
C+OTP | C+CHC | In-Prison Counseling |
All Conditions | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||||||||||||||
|
| |||||||||||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| Entered Prison Treatment | 36/37 (97.3) | 15/15 (100) | 51/52 (98.1) | 35/35 (100) | 17/17 (100) | 52/52 (100) | 71/72 (98.6) | 32/32 (100) | 103/104 (99.0) | 29/38 (76.3) | 14/16 (87.5) | 43/54 (79.6) | 29/38 (76.3) | 14/15 (93.3) | 43/53 (81.1) | 58/76 (76.3) | 28/31 (90.3) | 86/107 (80.4) | 129/148 (87.2) | 60/63 (95.2) | 189/211 (89.6) |
|
| |||||||||||||||||||||
| Completed Prison Treatment | 20/37 (54.1) | 12/15 (80.0) | 32/52 (61.5) | 17/35 (48.6) | 15/17 (88.2) | 32/52 (61.5) | 37/72 (51.4) | 27/32 (84.4) | 64/104 (61.5) | 23/38 (60.5) | 14/16 (87.5) | 37/54 (68.5) | 18/38 (47.4) | 13/15 (86.7) | 31/53 (58.5) | 41/76 (53.9) | 27/31 (87.1) | 68/107 (63.6) | 78/148 (52.7) | 54/63 (85.7) | 132/211 (62.6) |
|
| |||||||||||||||||||||
| Entered Community Treatment | 13/36 (36.1) | 9/14 (64.3) | 22/50 (44.0) | 16/35 (45.7) | 10/16 (62.5) | 26/51 (51.0) | 29/71 (40.8) | 19/30 (63.3) | 48/101 (47.5) | 17/36 (47.2) | 6/16 (37.5) | 23/52 (44.2) | 7/35 (20.0) | 4/14 (28.6) | 11/49 (22.4) | 24/71 (33.8) | 10/30 (33.3) | 34/101 (33.7) | 53/142 (37.3) | 29/60 (48.3) | 82/202 (40.6) |
Notes:
M=Male; F=Female, T=Total
B+OTP: Buprenorphine in prison and continued at an Opioid Treatment Program (OTP)
B+CHC: Buprenorphine in prison and continued an a Community Health Center (CHC)
C+OTP: Counseling only in prison and initiation of buprenorphine at an OTP
C+CHC: Counseling only in prison and initiation of buprenorphine at a CHC
Data for Entered Community Treatment were obtained on 202 participants; of the 211 participants, 2 received additional prison time and are still incarcerated, and we were unable to locate an additional 7 participants, so one-month post-release data were obtained on 202 of the remaining 209 participants (96.7%).
N= 202 for the analysis regarding Entered Community Treatment because two participants received additional prison time beyond the study period and seven others were not located at the one-month follow-up point.
3.3. Completed prison treatment
Of all 211 participants, 132 (62.6%) completed prison treatment (Table 2). The only significant effect in the model was Gender [χ2 (df=1)=17.9; p<.001; AOR=2.3 95% CI=1.6, 3.5], with women [54/63 (85.7%)] significantly [X2 =18.2] more likely to complete prison treatment than men [78/148 (52.7%)].
3.4. Entered community treatment
Of the 202 participants who were contacted following release from incarceration (Table 2), 82 (40.6%) entered community treatment [men=53 (37.3%) vs. women=29 (48.3%); X2=1.4.] As with results for entering prison treatment, there was a statistically significant main effect for In-Prison Treatment, again favoring buprenorphine over counseling only in prison [χ2(df=1)=6.3; p=01; AOR=1.5 95% CI=1.1, 2.1]. For the buprenorphine In-Prison Treatment condition 48/101 (47.5%) participants entered community treatment, while for the counseling only In-Prison Treatment condition, 34/101 (33.7%) participants entered community treatment. Of note, 8.5% (7/82 who entered community treatment) entered community treatment at facilities other than their designated OTP or CHC. No other effect in the model was significant (all ps > .05).
3.5. Reasons for Failure to Enter/Complete Prison Treatment
As reported in Table 3, only 1 of 104 participants (1.0%) randomized to the buprenorphine In-Prison Treatment Condition did not enter prison treatment, compared to 21 of 107 participants (19.6%) in the counseling only In-Prison Treatment Condition. The main reasons given by the participants in the counseling only Condition for not entering prison treatment included not wanting to receive counseling without buprenorphine (n=10), transfers resulting from rule violations (n=6), and early release (n=5).
Table 3.
Reasons failed to enter or complete prison treatment (N=211)
| Reason failed to enter prison treatment | B+OTP (n = 1) | B+CHC (n = 0) | Total Buprenorphine (n = 1) | C+OTP (n = 11) | C+CHC (n = 10) | Total Counseling (n = 21) |
|---|---|---|---|---|---|---|
| Changed mind after consent | 1 | 1 | ||||
| Did not want counseling without buprenorphine1 | 5 | 5 | 10 | |||
| Released from prison prior to first counseling intake/buprehorphine dose | 4 | 1 | 5 | |||
| Violated institutional rules, transferred to other prison | 2 | 4 | 6 | |||
| Reason failed to continue prison treatment | (n = 20) | (n = 20) | (n = 40) | (n = 6) | (n = 12) | (n = 20) |
| Attempted diversion/diversion of buprenorphine | 9 | 10 | 19 | - | - | - |
| Did not like effects of buprenorphine2 | 6 | 3 | 9 | - | - | - |
| Violated institutional rules, transferred to other prison | 5 | 6 | 11 | 4 | 7 | 11 |
| Transfer to another prison (no rule violation) | 1 | 1 | ||||
| Warrant for arrest | 1 | 1 | ||||
| Did not want counseling without buprenorphine | - | - | - | 2 | 4 | 6 |
Notes:
B+OTP: Buprenorphine in prison and continued at an Opioid Treatment Program (OTP)
B+CHC: Buprenorphine in prison and continued an a Community Health Center (CHC)
C+OTP: Counseling only in prison and initiation of buprenorphine at an OTP
C+CHC: Counseling only in prison and initiation of buprenorphine at a CHC
2 participants in the C+OTP condition and 1 participant in the C+CHC condition specifically noted that they did not want to receive counseling because they wanted to receive buprenorphine in prison.
Of the 6 participants in the B+OTP condition that ended prison treatment because they did not like the effects of the medication, the main symptoms that reportedly caused them to drop out were: 2 reported constipation; 2 reported feeling ill-not further specified; 1 reported feeling sluggish and losing appetite; and 1 said that other inmates noticed that he was “high”. One of the above six participants also reported experiencing drowsiness.
Of the 3 participants that dropped out of buprenorphine treatment in prison because they did not like the effects of the medication, the main symptoms that reportedly caused them to drop out were: one reportedly experienced headache; another reported erectile dysfunction and a rash; and a third reported itching and constipation. One of the above three participants also reported experiencing drowsiness.
Twice as many participants receiving buprenorphine/naloxone in prison discontinued treatment in prison compared to those in the counseling only condition (40 v. 20). Attempted diversion of buprenorphine/naloxone was the most frequent reason why members of the buprenorphine In-Prison Treatment condition discontinued prison treatment (n=19), followed by rule violations (n=11) and reportedly experiencing unpleasant side effects of buprenorphine/naloxone (n=9). (No participants experienced any serious adverse events during the prison and early community phase of the study). All participants who were terminated from treatment in prison for attempted diversion of medication received a medically supervised dose reduction. The main reason for discontinuing treatment in the counseling only condition involved rule violations (n=11).
4. DISCUSSION
4.1. Outcomes
4.1.1. Entering Prison Treatment
This is the first randomized clinical trial conducted in the US to report on buprenorphine/naloxone treatment administered to both male and female prisoners with pre-incarceration histories of heroin dependence. Results for entering prison treatment were encouraging for individuals assigned to treatment conditions receiving buprenorphine in prison. The observation that 99% of participants randomized to buprenorphine treatment in prison started treatment resembles or exceeds somewhat the comparable rates observed by Garcia et al. (2007; 100%) in an open-label trial in a pre-release prison in Puerto Rico and Magura et al. (2009; 78%) in a randomized trial of buprenorphine vs. methadone treatment conducted in a New York City jail, respectively. Further, in contrast to the studies by Garcia et al. (2007) and Magura et al. (2009), nearly all participants in the current study were not opioid-tolerant at study entry.
4.1.2. Completing Prison Treatment
Unlike the findings for entering prison treatment, results for completing prison treatment showed no significant differences by In-Prison Treatment condition. The percentage of participants randomized to receive buprenorphine/naloxone treatment in prison who completed prison treatment was 62%, compared to 64% in the Magura et al. (2009) study and 93% reported by Garcia et al. (2007). However, in the present study there was a significant effect for gender, with significantly more women than men completing prison treatment. This finding may be attributable to the fact that the women in the sample had more treatment episodes, both in general, and with both methadone and buprenorphine, than men; furthermore, as Greenfield et al. (2010) reported, women are more likely than men to initially enter treatment earlier in their substance use careers. In addition, among heroin-dependent prisoners, men typically engage in crime at earlier ages than women. Early onset of crime is related to a greater variety, severity, and persistence of deviant offenses (Inciardi, 2008). Consistent with this observation, the men in the present sample had begun offending earlier than women, and had been first arrested and incarcerated at younger ages. A challenge to retaining buprenorphine-initiated participants in prison treatment was the observation that 19/40 individuals (47.5%) who discontinued buprenorphine treatment were terminated for attempted diversion of medication (17.5% of those who initiated buprenorphine treatment). Of these 19 individuals, 16 (84.2%) were men. Magura et al. (2009) reported that 10% of their buprenorphine patients inducted in jail were removed from treatment for attempted diversion of medication.
A limitation with the use of buprenorphine/naloxone in tablet form is its potential for diversion, both in prison (Kinlock et al., 2010; Magura et al., 2009) and community (Johanson et al. 2012; Monte et al., 2009; Stimmel, 2007) settings. Our experiences with attempted diversion of medication resemble that of Magura et al. (2009) in that they are more frequent with buprenorphine/naloxone than with methadone; in our previously conducted randomized clinical trial of prison-initiated methadone (Kinlock et al., 2009), there were no identified instances of attempted methadone diversion. Diversion attempts are particularly common in prison, possibly because drugs may have more value in prison than in the community (Inciardi, 2008).
Another 9 of the 40 (22.5%) participants randomized to buprenorphine treatment initiated in prison ended treatment because they did not like the effects of the medication. All 9 were on relatively low doses (1–3 mg) when they discontinued. In the study by Zaller et al. (2013), 12 non-tolerant participants with pre-incarceration opioid dependence were on buprenorphine for, on average, one week until release from incarceration; of these, 11 continued buprenorphine treatment in the community; one participant (8.3 %) did not like the effects of the medication and entered drug-free treatment. Garcia et al. (2007) reported that of the 45 participants (most of whom were opioid-tolerant) who began buprenorphine treatment in prison, two (4.4%) withdrew because of side effects attributed to the medication. Magura et al. (2009) indicated that, of 60 opioid-tolerant participants who entered buprenorphine treatment in jail (mean days remaining in jail=23.2), one (1.7%) discontinued because of adverse effects attributed to the medication. Unlike incarcerated individuals in other nations (Dolan et al., 2005, 2007; Strang et al., 2006), Baltimore prisoners may not have as ready access to heroin and thus may be less likely to be opioid-tolerant during the later stages of their incarceration sentence. Thus, it is necessary to begin induction at a low dose and increase slowly to minimize adverse effects. For the most part, the dosing schedule was well tolerated. More details regarding the induction scheme and adverse events will be reported in a separate manuscript.
4.1.3. Entering Community Treatment
Similar to results for Entering Prison Treatment, there was a significant main effect for type of prison treatment, favoring members of the two In-Prison Buprenorphine Conditions. These results are comparable to those reported by Zaller et al. (2013) in their small-scale feasibility study. It is noteworthy that rates of post-release treatment entry were similar for the In-Prison Buprenorphine Conditions and the Condition in which participants did not start buprenorphine in prison and were referred to the OTP in the community, (44%, 51%, and 44%, respectively) as the Condition involving counseling only in prison and referral to the CHC had by far the lowest rate of community treatment entry (22%). However, the 48% community treatment entry rate for the two In-Prison Buprenorphine Conditions was considerably lower than the 92% reported by Zaller et al. (2013) and the 85% found by Garcia et al. (2007). In the study by Magura et al. (2009), 48% of participants who began buprenorphine treatment in jail entered community treatment.
It should be noted that in the authors’ prior randomized clinical trial of prison-initiated methadone, 66% of participants scheduled to begin MMT in prison entered MMT in the community within 10 days of release. The higher rate of treatment entry in the methadone study compared with the present study may be attributable to differences in medications and/or because the methadone study used the same treatment provider in prison and the community. Similarly, community-based treatment providers may not be receptive to newly released inmates as clients, as Magura and colleagues (2009) emphasized.
4.1.4. Limitations
A cautious interpretation of results is recommended because of several limitations in the current study. First, the study only involved inmates from Baltimore, so the findings are not necessarily generalizable to other geographic locations. Another factor limiting generalizability to prisoners was that a number of potential participants were excluded because of psychosis and/or suicidal ideation; these individuals may have been treated with buprenorphine in community settings. Second, although we desired to have relatively equal numbers of male and female participants, this did not occur; 70% of participants were male. As emphasized by Messina et al. (2009), recruiting female participants in prison studies is challenging because approximately 90% of US inmates are male, and female inmates are often offered other, competing, treatment options. Also, it was possible to continue providing buprenorphine/naloxone to some of the female participants (but not male participants) who were transferred from the institution for prison rule violations. Furthermore, because of state budgetary issues, the pre-release facility for women closed abruptly and unexpectedly shortly after the first year of recruitment. Because US Drug Enforcement Agency (DEA), DPSCS, and IRB approval was required to enlist the only other Maryland prison for women, there was a 10-month period in which no female participants were recruited. Finally, the issue of geographic barriers to the attendance of community treatment was not addressed. As emphasized by Rosenblum et al. (2011), among substance-dependent individuals, lower probability of treatment entry is associated with longer travel distances.
4.1.5. Implications
Results suggest that in-prison initiation of buprenorphine/naloxone pharmacotherapy among male and female prisoners is feasible. Apparently it was acceptable to all but one of the inmates randomized to begin buprenorphine/naloxone in prison, in contrast to 21 participants in the counseling only condition who failed to enter treatment in prison.
Results also indicated that buprenorphine treatment can be effective for a considerable proportion of inmates in terms of facilitating post-release treatment entry. However, major challenges remain, particularly concerning in-prison treatment terminations for attempted diversion of medication, as noted by others, cited above. Perhaps injectable or implantable formulations of buprenorphine may be more effective in reducing diversion attempts. Future publications from the present study will examine post-release treatment retention, heroin use, cocaine use, criminal activity, arrests, and re-incarceration.
Acknowledgments
Role of Funding Source
This study was supported by the National Institute on Drug Abuse (NIDA), Buprenorphine for Prisoners (PI: Kinlock; R01DA021579). NIDA staff had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of this manuscript and the decision to submit it for publication.
We would like to thank the Maryland Department of Public Safety and Correctional Services (DPSCS) and the three Baltimore City substance abuse treatment clinics for their collaboration and support. We also wish to thank all of the participants in this study.
Footnotes
Contributors
All authors contributed to and approved the final manuscript. The manuscript is the work of the authors alone. Authors Kinlock, Gordon, Schwartz, and O’Grady designed the study and wrote the protocol. All authors contributed to summaries of previous work. Author Kinlock and Gordon wrote the first draft of the manuscript. Authors Gordon and Kinlock wrote the first draft of the tables and figures. Author O’Grady made the primary contribution to the statistical analyses.
Conflict of Interest
Authors Gordon, Kinlock, Schwartz, and Fitzgerald report no conflicts of interest. Drs. Vocci and O’Grady have, in the past, received reimbursement for their time from Reckitt-Benckiser, one of the manufacturers of buprenorphine. This study was supported by an unrestricted, unsolicited investigator initiated request from Reckitt Benckiser Pharmaceuticals, Inc. who had no role in study design; collection, analysis and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication. The authors alone are responsible for the content and writing of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A. Categorical Data Analysis. Wiley; New York: 1990. [Google Scholar]
- Alford DP, LaBelle CT, Kretsch N, Bergeron A, Winter M, Boticelli M, Samet JH. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171:425–431. doi: 10.1001/archinternmed.2010.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Blatchford PJ, Lindsay RG, Stern MF. Risk factors for all-cause, overdose and early deaths after release from prison in Washington state. Drug Alcohol Depend. 2011;117:1–6. doi: 10.1016/j.drugalcdep.2010.11.029. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Nowels C, Corsi KF, Glanz J, Long J, Booth RE, Steiner JF. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clin Pract. 2012;7:3. doi: 10.1186/1940-0640-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment (CSAT) Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction, TIP 40. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2004. [PubMed] [Google Scholar]
- Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009;301:183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N, Bailey EJ, Cicero T, Inciardi J, Parrino M, Rosenblum A, Dart RC. Post-marketing surveillance of methadone and buprenorphine in the United States. Pain Med. 2010;11:1078–1091. doi: 10.1111/j.1526-4637.2010.00877.x. [DOI] [PubMed] [Google Scholar]
- Dolan K, Khoei EM, Brentari C, Stevens A. Prisons and Drugs: A Global Review of Incarceration, Drug Use and Drug Services. Beckley Foundation; Oxford: 2007. [Google Scholar]
- Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak AD. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, re-incarceration and hepatitis C infection. Addiction. 2005;100:820–828. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- Fazel S, Bains P, Doll H. Substance abuse and dependence in prisoners: a systematic review. Addiction. 2006;101:181–191. doi: 10.1111/j.1360-0443.2006.01316.x. [DOI] [PubMed] [Google Scholar]
- Garcia CA, Correa GC, Hernandez Viver AD, Kinlock TW, Gordon MS, Avila CA, Reyes CI, Schwartz RP. Buprenorphine-naloxone treatment for pre-release opioid-dependent inmate in Puerto Rico. J Addict Med. 2007;1:126–132. doi: 10.1097/ADM.0b013e31814b8880. [DOI] [PubMed] [Google Scholar]
- Gordon MS, Kinlock TW, Schwartz RP. A Randomized Clinical Trial of Methadone Maintenance for Prisoners: Findings at 12 Months Post Release. Presented as part of a symposium: Incarceration and Opioid Dependence: Impact, Interventions, and Implications Addiction Health Services Research Conference; Boston, MA. 2008. [Google Scholar]
- Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33:339–355. doi: 10.1016/j.psc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21:2409–2419. doi: 10.1002/sim.1047. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemshow S. Applied Logistic Regression. Wiley; New York: 1989. [Google Scholar]
- Inciardi JA. The War on Drugs IV. Prentice Hall; Upper Saddle River, NJ: 2008. [Google Scholar]
- Johanson C, Arfken C, diMenza S, Schuster CR. Diversion and abuse of buprenorphine: findings from national surveys of treatment patients and physicians. Drug Alcohol Depend. 2012;120:190–195. doi: 10.1016/j.drugalcdep.2011.07.019. [DOI] [PubMed] [Google Scholar]
- Kanato M. Drug use and health among prison inmates. Curr Opin Psychiatry. 2008;21:252–254. doi: 10.1097/YCO.0b013e3282fc985c. [DOI] [PubMed] [Google Scholar]
- Kastelic A, Pont J, Stöver H. A Practical Guide. Oldenburg: BIS-Verlag; 2008. Opioid Substitution Treatment in Custodial Settings. [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP. Incarcerated populations. In: Ruiz P, Strain E, editors. Lowinson & Ruiz’s Substance Abuse: A Comprehensive Textbook. Lippincott Williams & Wilkins; Philadelphia, PA: 2011. pp. 881–891. [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT. Developing and implementing a new prison-based buprenorphine treatment program. J Offender Rehabil. 2010;49:91–109. doi: 10.1080/10509670903534951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months post-release. J Subst Abuse Treat. 2009;37:277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, O’Grady KE, Hanlon TE. Prediction of the criminal activity of incarcerated drug-abusing offenders. J Drug Issues. 2003;33:897–920. [Google Scholar]
- Krinsky CS, Lathrop SL, Brown P, Nolte KB. Drugs, detention, and death: a study of the mortality of recently released prisoners. Am J Forensic Med Pathol. 2009;30:6–9. doi: 10.1097/PAF.0b013e3181873784. [DOI] [PubMed] [Google Scholar]
- Lee JD, Grossman E, Truncall A, Rotrosen J, Rosenblum A, Magura S, Gourevitch M. Buprenorphine-naloxone maintenance following release from jail. Subst Abuse. 2012;33:40–47. doi: 10.1080/08897077.2011.620475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levasseur L, Marzo JN, Ross N, Blatier C. Frequency of re-incarcerations in the same detention center: role of substitution therapy. A preliminary retrospective analysis. Ann Med Interne (Paris) 2002;153:1S14-19. [PubMed] [Google Scholar]
- Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 2009;99:222–230. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009:CD002209. doi: 10.1002/14651858.CD002209. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, Hutchinson SJ, Bird SM. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105:1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N. Implications for Criminal Justice Involved Women with Co-Occurring Substance Abuse and Mental and Physical Health Problems. White Paper prepared for the Co-Occurring Joint Action Council (COJAC), the Department of Alcohol and Drug Programs (ADP), and Department of Mental Health (DMH) 2009 http//www.aodpolicy.org/COD.htm.
- Metz V, Matzenauer C, Kammerer K, Winklbaur B, Ebner N, Radler D, Fischer G. Evaluation of opioid-dependent prisoners in oral opioid maintenance therapy. Heroin Addiction and Related Clinical Problems. 2010;12:5–16. [Google Scholar]
- Miotto K, Hillhouse M, Ling W. Comparison of buprenorphine treatment for opioid dependence in three settings. J Addict Med. 2012;6:68–76. doi: 10.1097/ADM.0b013e318233d621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SG, Kelly SM, Gryczynski J, Myers CP, Jaffe JH, O’Grady KE, Olsen YK, Schwartz RP. African American patients seeking treatment in the public sector: characteristics of buprenorphine vs. methadone patients. Drug Alcohol Depend. 2012;122:55–60. doi: 10.1016/j.drugalcdep.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monte AA, Mandell T, Wilford BB, Tennyson J, Boyer EW. Diversion of buprenorphine/naloxone coformulated tablets in a region with high prescribing prevalence. J Addict Dis. 2009;28:226–231. doi: 10.1080/10550880903014767. [DOI] [PubMed] [Google Scholar]
- Mumola CJ, Karberg JC. Drug Use and Dependence, State and Federal Prisoners, 2004. U.S. Department of Justice, Office of Justice Programs; 2006. NCJ 213530. [Google Scholar]
- Murphy DA, Hser Y, Huand D, Brecht ML, Herbeck DM. Self-report of longitduinal substance use: a comparison of the UCLA natrual history interview and the addiction severity index. J Drug Issues. 2010;40(2):495–515. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurco DN. A long-term program of research on drug use and crime. Subst Use Misuse. 1998;33:1817–1837. doi: 10.3109/10826089809059323. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Bonito AJ, Lerner M, Balter MB. Studying addicts over time: methodology and preliminary findings. Am J Drug Alcohol Abuse. 1975;2:183–196. doi: 10.3109/00952997509002733. [DOI] [PubMed] [Google Scholar]
- Rosenblum A, Cleland CM, Fong C, Kayman DJ, Tempalski B, Parrino M. Distance traveled and cross-state commuting to opioid treatment programs in the United States. J Environ Public Health. 2011 doi: 10.1155/2011/948789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallwitz A, Stover H. The impact of substitution treatment in prisons--a literature review. Int J Drug Policy. 2007;18:464–474. doi: 10.1016/j.drugpo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Stimmel B. Buprenorphine misuse, abuse, and diversion: when will we ever learn? J Addict Dis. 2007;26:1–3. doi: 10.1300/J069v26n03_01. [DOI] [PubMed] [Google Scholar]
- Stover H, Michels Drug use and opioid substitution treatment for prisoners. Harm Reduct J. 2010;7:17. doi: 10.1186/1477-7517-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, Gossop M, Heuston J, Green J, Whiteley C, Maden A. Persistence of drug use during imprisonment: relationship of drug type, recency of use and severity of dependence to use of heroin, cocaine and amphetamine in prison. Addiction. 2006;101:1125–1132. doi: 10.1111/j.1360-0443.2006.01475.x. [DOI] [PubMed] [Google Scholar]
- Taxman FS, Perdoni ML, Harrison LD. Drug treatment services for adult offenders: the state of the state. J Subst Abuse Treat. 2007;32:239–254. doi: 10.1016/j.jsat.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tompkins AD, Strain EC. Buprenorphine in the treatment of opioid dependence. In: Ruiz P, Strain E, editors. Lowinson & Ruiz’s Substance Abuse: A Comprehensive Textbook. Lippincott Williams & Wilkins; Philadelphia, PA: 2011. pp. 437–446. [Google Scholar]
- Zaller N, McKenzie M, Friedmann PD, Green TC, McGowan S, Rich JD. Initiation of buprenorphine during incarceration and retention in treatment upon release. J Subst Abuse Treat. 2013;45:222–226. doi: 10.1016/j.jsat.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]