Abstract
Aneurysmal bone cyst (ABC) is a rare benign tumor comprising 1.4% of all primary bone tumors. It commonly involves humerus, femur, tibia, and pelvic bones. Spinal involvement is rare. The pathological appearance of the lesion is one of the blown out distension with fluid filled cavities from which it gains the name aneurysmal bone cyst. The World Health Organization has defined it as an expanding lesion with blood filled cavities separated by septa of trabecular bone or fibrous tissue containing osteoclast giant cells. We describe the case of a 20-year-old Asian male who presented with backache and pain in right leg. Radiology was suggestive of an ABC involving the posterior elements of the lumbar vertebra. Excision was performed. We discuss this unusual case, reviewing the current literature on biological behavior and management of aneurysmal bone cyst.
Keywords: Aneurysmal bone cyst, aneurysmal bone cyst, back pain, primary bone tumor, spinal tumor
Introduction
Aneurysmal bone cysts (ABCs) were initially described as a distinct clinicopathological entity by Jaffe and Linchtenstein in 1942.[1] These are benign, thin walled, expansile tumors containing blood filled cystic cavities. Aneurysmal bone cysts primarily affect individuals between the ages 10-20 years of life with slight female preponderance.[2,3,4] ABCs comprise of approximately 1.4% of all bone tumors and 15% of all primary spine tumors.[5,6] Treatment modalities for aneurysmal bone cysts include surgical curettage with or without bone grafting, complete excision, embolization, radiation therapy or a combination of these modalities.[7,8,9]
We present a case of aneurysmal bone cyst of the lumbar spine. Clinical manifestations, pathogenesis, investigations, and management are discussed and reviewed along with pertinent literature.
Case Report
A 20-year-old Asian, young male was admitted to the Neurosurgery Department complaining of severe low back pain.
Local examination revealed an ill-defined, palpable, tender mass opposite the L2 vertebra. Neurological examination revealed no motor or sensory abnormality. The deep tendon reflexes were normal. Bowel and bladder functions were normal. X-ray of the spine revealed loss of posterior elements [Figure 1]. Magnetic resonance imaging (MRI) of the spine showed a well-defined expansile mass lesion involving L2 vertebra with bilateral laminar destruction , hypointense signal on T1 and hyperintense signal on T2 weighted images with multiple internal septations [Figure 2]. Heterogeneous contrast enhancement was also present.
Figure 1.
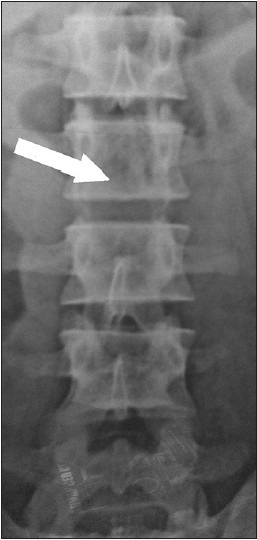
X-Ray Dorsolumbar spine AP view revealing loss of posterior elements (Arrow)
Figure 2.
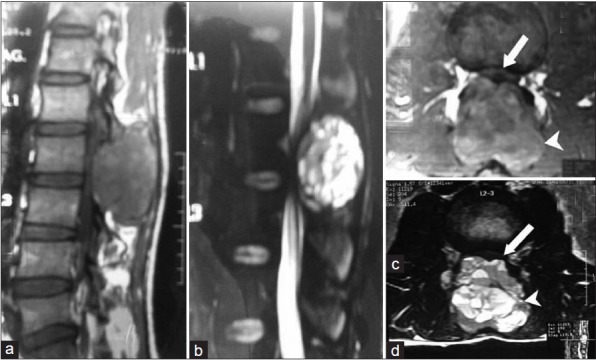
MRI spine showing well defined expansile mass lesion (arrow head) at L2 vertebra with bilateral laminar destruction and tecal sac compression (arrow). It displayed hypo intense signals on T1; (a and c) Hyper intense signals on T2 weighted images; (b and d) Multiple internal septations and heterogeneous contrast enhancement
The patient was operated through a midline longitudinal incision and meticulous muscle dissection was carried out. A dirty pinkish mass arising from the posterior bony elements was delivered which bled even on touching [Figure 3a]. The mass was removed piece-meal with bone roungers. It was filled with dirty-oily colored fluid. Complete excision was achieved and the thecal sac was decompressed [Figure 3b].
Figure 3.
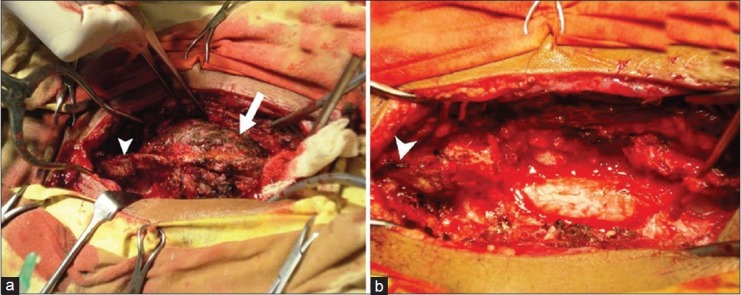
Preoperative (a) and Postoperative (b) Photographs depicating large dirty pinkish mass (arrow) which bleeds profusely on touching. Normal spinous process (arrow head) of rostral segment is also seen
Histopathology was consistent with ABC and revealed large blood filled spaces without any true endothelial lining ; intervening septa were crammed with multinucleated giant cells [Figure 4].
Figure 4.
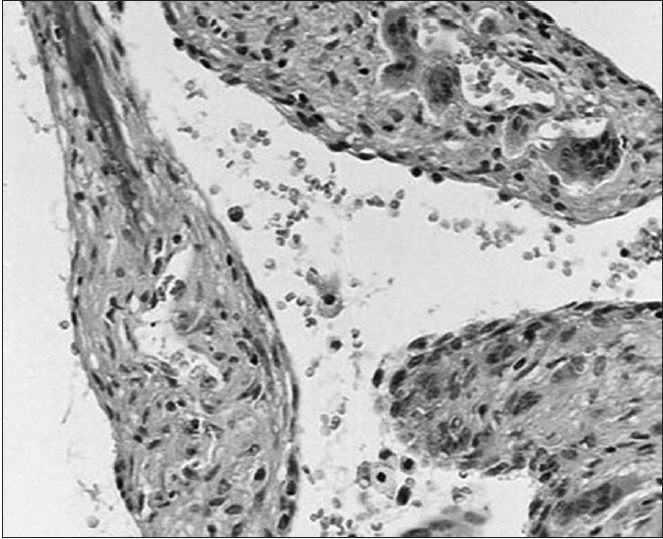
Aneurysmal bone cyst showing the characteristic pseudo-vascular spaces with intercening septa and giant cells (H and E, ×325)
The patient's post-operative course was uneventful and he was discharged in satisfactory, pain-free condition. No adjuvant therapy was given and there was no sign of recurrence at one year follow-up.
Discussion
The thoracic and lumbar (34%) vertebrae are the most common sites for spinal ABC.[2,3,5,10] The posterior elements and the pedicles are affected first. In approximately 25-35% patients, adjacent vertebrae are also affected through surrounding soft tissue extension, but never through an intervertebral disc.[2,11] Spinal deformities such as kyphosis or scoliosis can also be present in 10-15% cases.[4,8]
The etiology or exact pathogenesis of ABC remains obscure. These are generally thought to occur as a secondary vascular phenomenon superimposed on a preexisting lesion, which presumably initiates a periosteal or intraosseous arteriovenous malformation.[1,5,12] The resultant high pressure vascular channels erode the osseous trabeculae forming a cystic cavity . The associated reactive changes within endosteum and periosteum incite accelerated osteoblastic and osteoclastic activities, which then rapidly remodel the bone while conforming to hemodynamic forces giving the lesion a ballooned, thin shelled and multiseptated soap bubble appearance.[5,11,12]
Aneurysmal bone cysts are associated with an underlying skeletal lesion in 20 to 30% of cases consolidating the concept of secondary phenomenon.[3] The diagnosis of aneurysmal bone cyst should therefore be made when all other underlying lesions can be excluded.
The main presenting symptom is pain with duration of usually four through eight months.[11] There can be associated swelling or palpable mass which is tender to touch. Neurological symptoms can vary from mild paresthesias and radicular pains to complete paraplegia. Radiological and neurological deterioration is an indication for surgical intervention to prevent irreversible damage to the spinal cord and nerve roots.
Among the various treatment options, total enbloc excision, if possible, provides the highest rate of cure with excellent prognosis.[2,4,5,8] Excision must include the entire cyst wall because partial excision is associated with higher risk of recurrence.[2] If instability and deformity already exists or if the amount of bone resection is expected to result in instability , then simultaneous reconstruction and instrumented stabilization should be planned.[8,10,11]
The role of embolization in the management of aneurymal bone cyst is to decrease vascularity and reduce intra operative blood loss. Although successful treatment with this technique alone is reported in pelvic and long bones, its use as a sole mode of therapy is limited in spine , especially in a setting of pathological fractures and neurological involvement.[13] Radiation therapy has been advocated in case of partial excision, but has drawbacks of sarcomatous changes and irradiation myelopathy.[5,7]
Conclusion
ABC of spine is essentially a benign, vascular, expansile lesion, affecting a young age group and which can cause irreversible damage to the spinal cord if not treated early. For this reason, prompt diagnosis and timely intervention is required.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004–25. [Google Scholar]
- 2.Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, Biagini R, et al. Aneurysmal bone cyst of the mobile spine: Report on 41 cases. Spine (Phila Pa 1976) 2001;26:27–35. doi: 10.1097/00007632-200101010-00007. [DOI] [PubMed] [Google Scholar]
- 3.de Kleuver M, van der Heul RO, Veraart BE. Aneurysmal bone cyst of the spine: 31 cases and the importance of the surgical approach. J Pediatr Orthop B. 1998;7:286–92. doi: 10.1097/01202412-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Papagelopoulos PJ, Currier BL, Shaughnessy WJ, Sim FH, Ebsersold MJ, Bond JR, et al. Aneurysmal bone cyst of the spine. Management and outcome. Spine (Phila Pa 1976) 1998;23:621–8. doi: 10.1097/00007632-199803010-00018. [DOI] [PubMed] [Google Scholar]
- 5.Ameli NO, Abbassioun K, Saleh H, Eslamdoost A. Aneurysmal bone cyst of the spine. Report of 17 cases. J Neurosurg. 1985;63:685–90. doi: 10.3171/jns.1985.63.5.0685. [DOI] [PubMed] [Google Scholar]
- 6.Dahlin DC, McLeod RA. Aneurysmal bone cyst and other nonneoplastic conditions. Skeletal Radiol. 1982;8:243–50. doi: 10.1007/BF02219618. [DOI] [PubMed] [Google Scholar]
- 7.Clough JR, Price CH. Aneurysmal bone cyst: pathogenesis and long term results of treatment. Clin Orthop. 1973;97:52–63. doi: 10.1097/00003086-197311000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Turker RJ, Mardjetko S, Lubicky J. Aneurysmal bone cysts of the spine: Excision and stabilization. J Pediatr Orthop. 1998;18:209–13. [PubMed] [Google Scholar]
- 9.Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer. 1992;69:2921–31. doi: 10.1002/1097-0142(19920615)69:12<2921::aid-cncr2820691210>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 10.Capanna R, Albisinni U, Picci P, Campanacci M, Springfield DS. Aneurysmal bone cyst of the spine. J Bone Joint Surg Am. 1985;67:527–31. [PubMed] [Google Scholar]
- 11.Pang D, Tomita T, Byrd S, Conway JJ, Chou P, de Leon GA. A 14-year-old young woman with a five-week history of back pain. Pediatr Neurosurg. 2000;32:100–8. doi: 10.1159/000028908. [DOI] [PubMed] [Google Scholar]
- 12.Lichtenstein L. Aneurysmal bone cyst: observations on fifty cases. J Bone Joint Surg Am. 1957;39:873–82. [PubMed] [Google Scholar]
- 13.Wallace S, Granmayeh M, deSantos LA, Murray JA, Romsdahl MM, Bracken RB, et al. Arterial occlusion of pelvic bone tumours. Cancer. 1979;43:322–8. doi: 10.1002/1097-0142(197901)43:1<322::aid-cncr2820430147>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]


