Abstract
Objective:
To report a rare case of basal encephalocele (spheno-orbital encephalocele), managed successfully in our institute. This is one of the rarest type of encephaloceles with very little literature available. In this case, sphenoid dysplasia was not associated with type 1 Neurofibromatosis.
Settings:
Grant Medical College and Sir J.J Group of Hospitals, Byculla, Mumbai, Maharashtra, India.
Methods:
A 22 year old male presented with a history of protrusion of right eye since the age of 7 years followed by progressive diminution of vision in the same eye for 5 months. MRI scan was suggestive of sphenoid dysplasia with herniation of right fronto-temporal lobe. The patient was operated upon with right frontal craniotomy with excision of encephalocele and repair of skull base. Subsequently, the patient underwent plastic surgery for facial skin remodeling.
Results:
Patient's encephalocele reduced completely after excision and repair with good cosmetic results and no neurological deficits. There is no evidence of recurrence till recent follow-up.
Conclusion:
Basal encephaloceles are very rare. Complete excision of encephalocele with repair of the defect should be the aim to achieve cure.
Keywords: Basal encephalocele, sphenoid dysplasia, Spheno-Orbital encephalocele
Introduction
Encephaloceles are one of the rare congenital lesions consisting of herniation of intracranial contents from the cranial cavity. They may consist of meninges alone (meningoceles), may contain brain tissue in addition (meningoencephalocele or encephalocele), and may even include a ventricle (hydroencephalomeningocele).
Basal encephaloceles are the least common (1.5%) of all encephaloceles. The incidence is 1 in 35,000 live births. It is much higher in Southeast Asian countries, including some parts of India. (It is as high as 1:5,000 live births in Thailand.) These rare encephaloceles are classified into five anatomic types: Spheno-ethmodial, transsphenoidal, spheno-orbital, transethmoidal, and spheno-maxillary. Trans-sphenoidal is the rarest of all. We report a rare case of such basal encephalocele (spheno-orbital type) managed successfully in our institute.
Case Report
A 22 year old, second-born issue of non-consanguineous marriage with full term normal delivery was admitted with swelling behind upper eye lid and protrusion of the right eye since the age of 7 years. The patient noticed rapid increase in the size of swelling for last 6 months. There was history of progressive diminution of vision during the same time.
The swelling had pushed the eyeball medially and downwards. This was associated with diminution of vision, pain, watering, and redness of the right eye.
On general examination, there was a single 10 cm x 5 cm ill defined hyper pigmented patch with hypertrichosis over the back on the left side suggestive of “Becker's Nevus”. There was no evidence of café-au- lait spots, hypertelorism, broad nasal root, cleft lip, or cleft palate.
On neurological examination, higher mental functions were normal. The right eyeball was deviated medially and inferiorly. Visual acuity was reduced to finger counting at 1 feet in right eye and was normal in the left eye. External ocular movements were restricted in all directions in right eye. Pupils were 3.00 mm equally reacting in both eyes. Fundus examination was normal in both eyes and remaining cranial nerves were normal. Power was 5/5 in all limbs. Sensory examination did not reveal any abnormality. Reflexes and gait were normal.
On local examination [Figure 1], there was a soft, compressible, nonpulsatile swelling behind the right eyeball causing severe proptosis. However, there was no impulse on coughing.
Figure 1.

Pre-operative view of the encephalocele with the globe being displaced inferiorly and medially
The right eyeball which was pushed medially and inferiorly was almost touching the ala of the right nostril. This was associated with swelling of the right eyelid with conjunctival chemosis.
No evidence of lisch nodules or other stigmata of neurofibromatosis was present.
An irregular bony defect of 6 cm x 4 cm in size was present over the right occipital region with no evidence of encephalocele.
Plain radiograph of the skull showed a defect in the sphenoid wing and occipital region with widening of the right orbital fissure.
USG of the right eye showed a large retro-ocular mass with solid and cystic areas within with internal septations possibly representing herniated neural tissue.
CT [Figures 2 and 3] and MRI scans [Figures 4 and 5] were suggestive of dysplastic greater wing of sphenoid on the right side with herniation of temporal lobe and CSF in to right orbital space causing displacement of right eyeball anteriorly. Diffuse atrophy of right cerebral hemisphere was seen. Multiple sutural defects were also seen in the right occipital bone and lambda. Right-sided extra ocular muscles and optic nerve were displaced and appeared indistinct.
Figure 2.

CT scan (3D reconstruction) showing dysplastic greater wing of sphenoid on right side with herniation of temporal lobe and CSF in right orbital space causing displacement of right eye globe anteriorly
Figure 3.
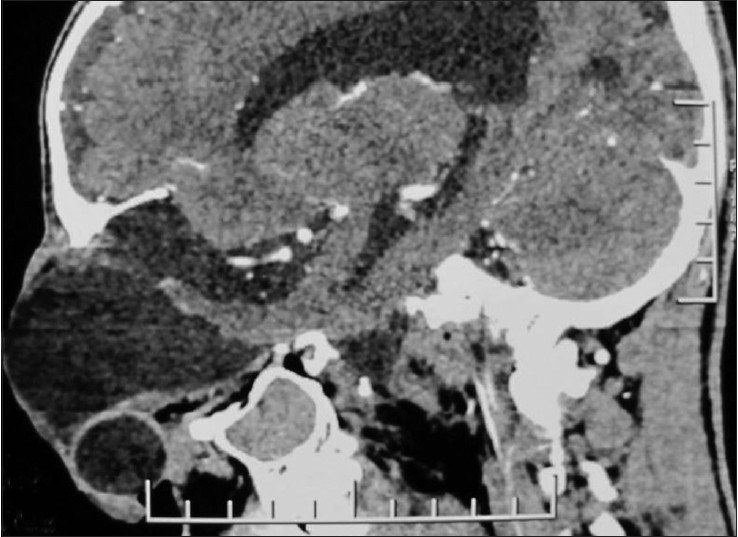
CT scan (3D reconstruction) showing herniation of temporal lobe and CSF in right orbital space causing displacement of right eye globe anteriorly through the defect
Figure 4.
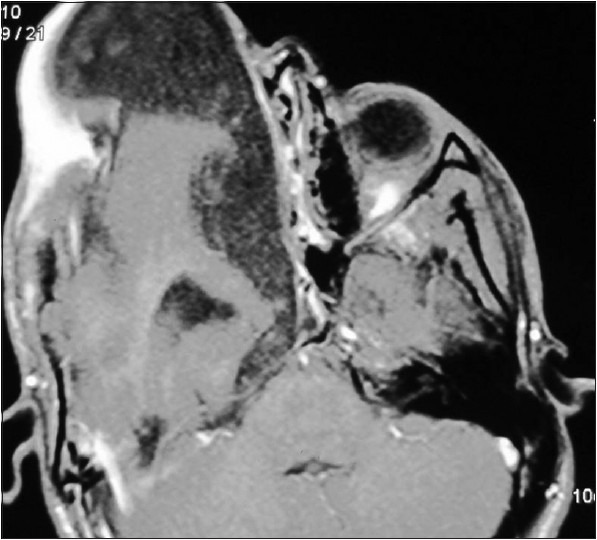
MRI scan (axial view) was suggestive of sphenoid wing dysplasia on right side with herniation of right fronto-temporal lobe, temporal horn of right ventricle and CSF though the defect. Hemiatrophy of right cerebral hemisphere
Figure 5.
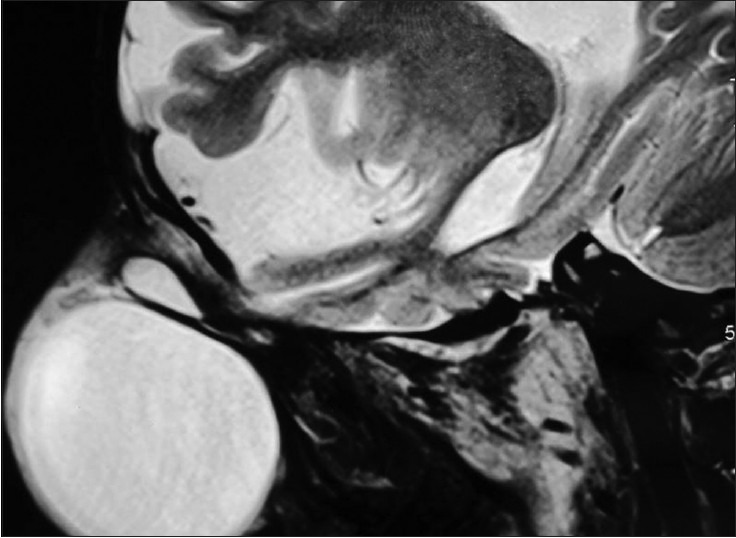
MRI scan (sagittal view) was suggestive of sphenoid wing dysplasia on right side with herniation of right fronto-temporal lobe, temporal horn of right ventricle and CSF through the defect. Hemiatrophy of right cerebral hemisphere
The patient was operated wherein Bicoronal incision taken and right frontal craniotomy was done. The dysplastic brain tissue was excised after opening the sac with primary suturing of the dural defect. The repair of the skull base defect was done using a pericranial flap.
Intra-operatively, bony defect was present on the roof of the right orbit (frontal and sphenoid bone) extending posteriorly up to the petrous temporal bone. Encephalocele sac was identified, opened, and CSF was drained. Gliosed brain entering into the sac was sucked to define the posterior limit of dural defect. Dural edges were sutured primarily after defining the edges all around.
Patient's enecephalocele reduced completely after surgery with good cosmetic result and without any neurological deficits [Figure 6].
Figure 6.
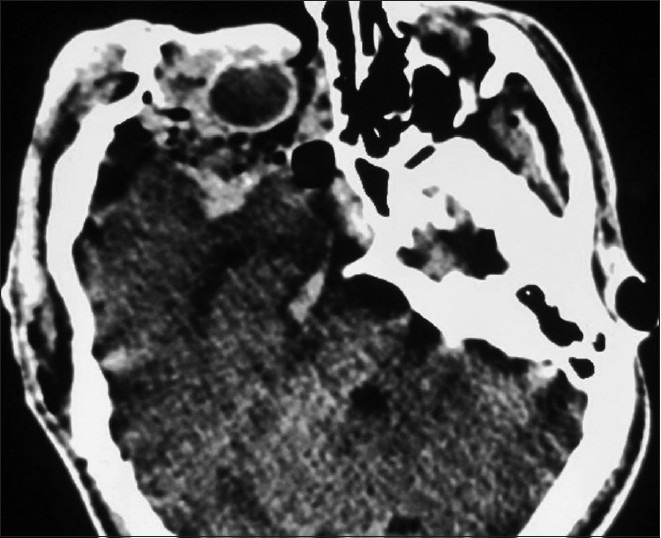
Post-operative CT scan (axial view) showing complete excision of encephalocele
Post-operatively [Figure 7], there was ptosis in the right eye. Patient's visual acuity had improved to finger counting at 4 feet. However, there was no change in the range of movement and field. Pupils were 3.00 mm equally reacting in both eyes. Conjunctival congestion had decreased. Fundus examination was showing attenuated blood vessels with hyperemic disc in the right eye.
Figure 7.

Post-operative pic of the patient showing complete excision of encephalocele with redundant eyelid
The patient has been following up regularly with no evidence of recurrence.
Discussion
An encephalocele is a protrusion of cranial contents beyond the normal confines of the skull due to a disturbance in the separation of surface ectoderm and neuroectoderm mostly in the midline after closure of the neural folds.[1]
The primary abnormality in the development of encephalocele is a mesodermal defect resulting in a defect in the bone and dura through which cranial contents herniate.
Encephaloceles are classified as anterior (frontal, sincipital, basal) and posterior (infra and supratorcular).[2]
Posterior encephaloceles are most common (75%) and basal ones are least frequent (1.5%).[3]
Encephaloceles occur most commonly in females than in males.[3] They are often associated with midline craniofacial dysraphism,[3] which is not seen in the present case. When it protrudes into the nasal cavity, it can lead to upper airway obstruction.
Some particularly, sphenoid encepahloceles are often clinically occult and usually become apparent at the end of first decade of life.[4] In our case also, the patient presented with the proptosis since the age of 8 years and not since birth.
Basal encephaloceles are very rare, found in 1:35,000 live births, and classified based on the anatomical site of defect in to sphenoethmoidal, sphenoorbital, trans-sphenoidal, and trans-ethmoidal types.[2]
Trans-sphenoidal is the rarest of all, constituting 5% of all basal encephaloceles and is associated with visual and hormonal disturbances.[3]
The most widely accepted theory to explain basal encephalocele lies in defective ossification of the body of the sphenoid bone with persistence of the craniofacial canal. Herniation through the floor of the sella turcica occurs before the 10th week of gestation.[5]
Basal encephaloceles are often associated with other midline anomalies such as hypertelorism, broad nasal root, cleft lip, and cleft palate. Optic disc anomalies such as pallor, dysplasia, optic pit, coloboma, and megalopapilla have been reported to occur in patients with basal encephalocele,[6] which was conspicuous by absence in our case.
Encephaloceles are definitively diagnosed by radiological examination. Computed tomography (CT) with three-dimensional reconstruction and MRI provide precise information about the position of cranial bony defect and the content of the cystic mass. They are valuable in determining the need for and planning the extent of craniofacial reconstruction.[7]
Angiography may be helpful to establish the relationship between major branches of circle of Willis and the internal orifice.
After thorough evaluation, the definite management of encephalocele is surgical intervention which includes excision of encephaloceles and repair of the defect.
The goal of treatment is to achieve a watertight closure of the dura following amputation of the mass or its relocation into the cranial cavity. These lesions are difficult to treat, given the propensity for vital structures (hypothalamus, chiasma, optic nerve, third ventricle, anterior cerebral arteries) to herniate.[8]
Extra-cranial approaches to these lesions are associated with many problems including incomplete resection and post-operative CSF leaks. The intracranial approach is the preferred method for treatment of these lesions.[8]
As in our case, we have done excision of encephalocele via the intracranial approach with repair of the defect.
Most authors agree that encephalocele should be managed in the first few months of life. This makes the identification of the intracranial connection technically easier and allows more complete repair of the dural defect.[9]
Attempts at surgical reconstruction of the sphenoid defect, to separate the orbit from the middle cranial fossa, have met with only limited success due to the resorption of bone grafts.[10] However, there are rare chances of recurrence due to the formation of fibrous tissue which prevent recurrent prolapses.
The prognosis is inversely related to the amount of neural tissue found in the sac and the severity of associated anomalies. The prognosis for both survival and intellectual development is better for anteriorly placed than for posteriorly placed encephaloceles.
Conclusion
Basal encephaloceles are very rare. They are associated with midline facial deformities such as oral cleft. Sphenoid dysplasias are associated with NF-1; therefore, extensive work-up to rule out NF-1 should be carried out. Complete excision or relocation of encephalocele with repair of the defect should be the aim to achieve cure.
Long-term follow-up is required to ensure that the satisfactory cosmetic result is achieved.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Aubry MC, Aubry JP, Dommergues M. Sonographic prenatal diagnosis of central nervous system abnormalities. Childs Nerv Syst. 2003;19:391–402. doi: 10.1007/s00381-003-0768-3. [DOI] [PubMed] [Google Scholar]
- 2.HUMPREYS RP. Encephalocele and dermal sinus. In: Cheek WS, editor. Pediatric Neurosurgery. Philadelphia: WB Saunders, Co; 1994. p. 4. [Google Scholar]
- 3.Vidaèiæ A, Matovinoviæ M, Mariæ A, Herman D, Murgiæ J, Peæina HI, Èerina V, Vrkljan M. Transsphenoidal encephalocele case report. Acta Clin Croat. 2005;44:373. [Google Scholar]
- 4.Winniger SJ, Donnenfeld AE. Syndrome identified in fetus with prenatal diagnosis of cephaloceles. Prenat Diagn. 1994;14:839–43. doi: 10.1002/pd.1970140912. [DOI] [PubMed] [Google Scholar]
- 5.Teng E, Heller J, Lazareff J, Kawamoto H, Wasson K, Garri JI, et al. Caution in treating transsphenoidal encephalocelewith concomitant moyamoya disease. J Craniofac Surg. 2006;17:1004–9. doi: 10.1097/01.scs.0000224988.40280.4a. [DOI] [PubMed] [Google Scholar]
- 6.Caprioli J, Lesser RL. Basal encephalocele and morning glory syndrome. Br J Ophthalmol. 1983;67:349–51. doi: 10.1136/bjo.67.6.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shimizu T, Kitamura S, Kinouchi K, Fukumitsu K. A rare case of upper airway obstruction in an infant caused by basal encephalocele complicating facial midline deformity. Paediatr Anaesth. 1999;9:73–6. [PubMed] [Google Scholar]
- 8.Albright AL, Adelson PD, Pollack IF. Principles and practice of pediatric neurosurgery. 2nd ed. New York: Thieme Medical Publishers, Inc.; 2008. p. 246. [Google Scholar]
- 9.Charles WC. Flint P, editor. Congenital malformation of nose. Cummings otolaryngology Head and Neck Surgery. 2005;4:4099–109. [Google Scholar]
- 10.Havlik RJ, Boaz J. Cranio-orbital-temporal neurofibromatosis; are we treating the whole problem? J Craniofac Surg. 1998;9:529–35. doi: 10.1097/00001665-199811000-00007. [DOI] [PubMed] [Google Scholar]


