Abstract
We report a rare case of an acute epidural hematoma (EDH) due to solitary skull metastasis in a 60-year-old patient treated earlier for ovarian carcinoma. The patient presented with head injury followed by unconsciousness and computerized tomography showed a large EDH in the right parietal region along with a contusion of left temporal-parietal lobe and subarachnoid hemorrhage in left sylvian fissure. Emergency craniotomy and evacuation of the EDH was performed and the hemorrhage was determined to be secondary to skull metastasis of ovarian carcinoma; the patient recovered and received whole brain radiation therapy.
Keywords: Epidural hematoma, ovarian carcinoma, skull metastases
Introduction
Skull and intracranial metastasis from ovarian carcinoma have been rarely reported. Epidural hematoma (EDH), subdural hematoma (SDH), and intracerebral hemorrhage from skull metastasis of ovarian carcinoma are also extremely rare.[1] Although EDH due to skull metastases has been described, almost all the cases have been associated with hepatocellular carcinoma.[2] We report a case of acute EDH with skull metastases in a 60-year-old female patient treated earlier for ovarian carcinoma, with a review of the pertinent literature. To our knowledge, this is the first and only such case reported in the literature.
Case Report
A 60-year-old housewife was brought to our emergency department following a fall from a two wheeler. On admission, she was found to be unconscious with a Glassgow Coma Score of 10/15 (E2 V3 M5), irritable, and without any motor deficits. Past history revealed a curative salpingo-opherectomy performed 3 years ago for ovarian carcinoma. Routine blood investigations were within normal limits. Computerized tomography of brain revealed a 4 × 3 cm epidural hematoma (EDH) in the right parietal region with a lytic lesion of parietal bone of skull overlying the EDH, a contusion of left temporal-parietal lobe and subarachnoid hemorrhage in left sylvian fissure [Figures 1 and 2]. The patient was immediately taken up for surgery. During the operation, no scalp mass or skull fracture was found; rather the parietal bone overlying the EDH was thinned out and was replaced by thick, firm, fibrous, yellowish-brown, hypervascular mass suggestive of tumor tissue. No gross invasion or thickening of the dura was observed. No active bleeding was seen from the dura or its overlying vessels. Hence, it was assumed that the bleeding focus was the destroyed diploic space of the parietal bone and the tumor mass itself. The hematoma, tumor tissue, and a ring of normal looking parietal bone around the lesion were completely removed [Figure 3].
Figure 1.
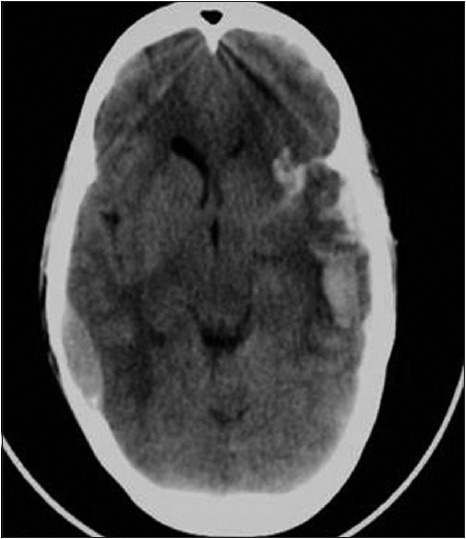
Non-contrast computerized tomography of the brain showing epidural hematoma in the right parietal region, a contusion of left temporal-parietal lobe and subarachnoid hemorrhage in left sylvian fissure
Figure 2.
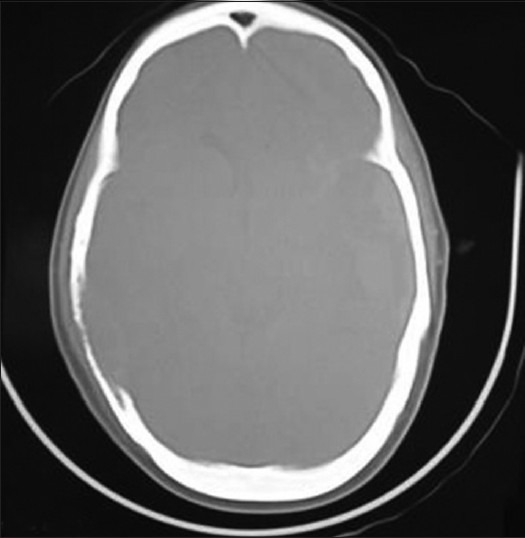
Bone window of the scan showing a lytic lesion of right parietal bone of skull
Figure 3.
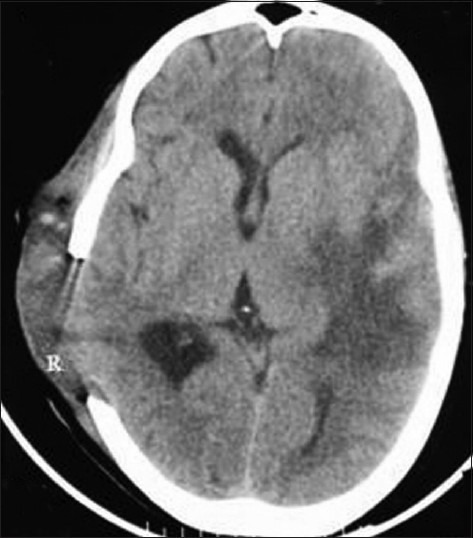
Postoperative scan showing evacuated hematoma and excised skull tumor
Microscopically, the tumor revealed round to oval cells with clear cytoplasm, indistinct cytoplasmic margins, vesicular nuclei, and prominent nucleoli. Cells were arranged in nests and sheets showing focal comedo necrosis [Figure 4]. These findings were compatible with the diagnosis of metastatic ovarian adenocarcinoma.
Figure 4.
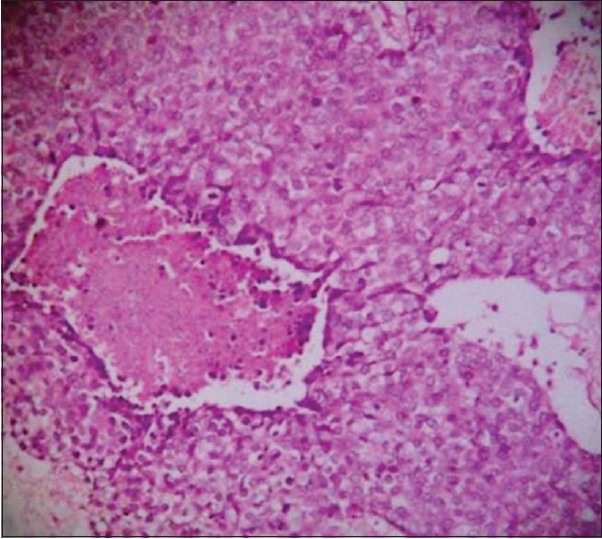
Photomicrograph showing tumor with comedo necrosis (Hematoxylin and eosin, ×400)
Postoperatively, the patient recovered well, became conscious, and received whole brain radiation therapy.
Discussion
Brain metastases are the most common intracranial tumor in adults, comprising about 40% of all intracranial neoplasms. Any primary systemic tumor can metastasize to the brain, but the most common neoplasms producing brain metastases are in order of decreasing frequency lung cancer, breast cancer, melanoma, colorectal cancer, and urogenital cancer.[3,4,5] Location of brain metastasis may be intra-axial or extra-axial. The latter may involve either the skull or dura.
The skull metastasis may involve either the calvarium or skull base, with the former being more common. Calvarial metastases are usually asymptomatic and discovered incidentally on radiographic studies. Incidence of calvarial metastasis diagnosed during trauma evaluation is less than 0.8%.[6] The time interval reported between treatment of primary and involvement of skull due to metastasis is around 3-4 years. The most common presenting symptom is a visible, localized swelling of the skull produced by a growing tumor that erodes the outer table. Tumors can also expand through inner skull table and apply direct pressure on adjacent brain parenchyma or on dural venous sinuses. Focal sensorimotor deficits and seizures occasionally result from progressive inward growth of a calvarial metastatic lesion. Rarely, they may be associated with either subdural or epidural hematomas.
Intracranial hemorrhage from distant metastasis of primary cancer is rare and its incidence accounts for 0.9-11%.[7] The location is usually intracerebral and very rarely epidural. Epidural hematoma (EDH) has been associated with skull tumors both primary and secondary. Several primary skull tumors, such as Ewing's sarcoma, epidermoid, and hemangioendothelioma, have been found to be associated with epidural hematomas. Several authors have reported skull metastases associated with chronic epidural hematomas but their association with acute epidural hematomas is rarely seen.[8]
Only six cases of acute EDH associated with metastatic tumors have been reported in the literature. Hepatocellular carcinoma has been the primary in five such cases[2,9,10,11] and ovarian carcinoma[1] in one case. In the five cases of EDH reported to be caused by hepatocellular carcinoma, four were due to skull metastasis and one was due to dural metastasis. The one case of EDH caused by ovarian carcinoma was due to dural metastasis. Hepatocellular carcinoma has been the primary in all cases of EDH due to skull metastasis. Our is the only reported case of EDH caused by skull metastasis from ovarian carcinoma.
EDH is usually a consequence of head injury. In-bending of skull at the time of traumatic impact on the head makes the skull fracture which can cause epidural bleeding from lacerated meningeal vessels, fractured edges, torn venous sinuses, or diploic veins. But spontaneous or non-traumatic intracranial EDHs are very rare. Main possible causes of this unusual phenomenon are infection from frontal sinusitis, maxillary sinusitis, otitis media, craniofacial infections, coagulation disorders, vascular malformation of dura, and malignancy.[12]
Epidural hematoma associated with skull metastasis has been spontaneous in all but one of the cases reported so far. Even in the one case associated with trauma, the history was suggestive of a minor trauma preceding the onset of symptoms by two weeks.[9] Our case has been an exception as the onset of EDH associated with the metastatic lesion was precipitated by severe degree of trauma. The patient had an asymptomatic course till the event of trauma.
This presentation other than reporting a rare case suggests two important points. A patient may harbor a significant metastatic tumor of skull with a potential to cause EDH and yet may not show any symptoms. Any hematoma following trauma in a patient treated for primary systemic carcinoma has to be carefully scrutinized and treated.
Conclusion
We emphasize that acute epidural hematoma associated with skull metastasis from ovarian carcinoma should always be considered in the differential diagnosis when the patient treated for the same presents with headache or unconsciousness with or without trauma. Only early diagnosis and emergent treatment can prevent mortality and morbidity in these patients. Since a significant skull lesion may be silent, this makes a case for periodical screening through CT scan especially from third year onwards following the treatment for the primary.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Anegawa S, Hirohata S, Tokutomi T, Kuramoto S. Spontaneous epidural hematoma secondary to dural metastasis from an ovarian carcinoma: Case report. Neurol Med Chir (Tokyo) 1989;29:854–6. doi: 10.2176/nmc.29.854. [DOI] [PubMed] [Google Scholar]
- 2.Woo KM, Kim BC, Cho KT, Kim EJ. Spontaneous epidural hematoma from skull base metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc. 2010;47:461–3. doi: 10.3340/jkns.2010.47.6.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Endo M, Hamano M, Watanabe K, Wakai S. Combined chronic subdural and acute epidural hematoma secondary to metastatic hepatocellular cancer: Case report. No Shinkei Geka. 1999;27:331–4. [PubMed] [Google Scholar]
- 4.Hayashi K, Matsuo T, Kurihara M, Daikoku M, Kitange G, Shibata S. Skull metastasis of hepatocellular carcinoma associated with acute epidural hematoma: A case report. Surg Neurol. 2000;53:379–82. doi: 10.1016/s0090-3019(00)00208-1. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh CT, Sun JM, Tsai WC, Tsai TH, Chiang YH, Liu MY. Skull metastasis from hepatocellular carcinoma. Acta Neurochir (Wien) 2007;149:185–90. doi: 10.1007/s00701-006-1071-3. [DOI] [PubMed] [Google Scholar]
- 6.Stark AM, Eichmann T, Mehdorn HM. Skull metastases: Clinical features, differential diagnosis, and review of the literature. Surg Neurol. 2003;60:219–25. doi: 10.1016/s0090-3019(03)00269-6. [DOI] [PubMed] [Google Scholar]
- 7.Wakai S, Yamakawa K, Manaka S, Takakura K. Spontaneous intracranial hemorrhage caused by brain tumor: Its incidence and clinical significance. Neurosurgery. 1982;10:437–44. doi: 10.1227/00006123-198204000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Nakao N, Kubo K, Moriwaki H. Cranial metastasis of hepatocellular carcinoma associated with chronic epidural hematoma: Case report. Neurol Med Chir (Tokyo) 1992;32:100–3. doi: 10.2176/nmc.32.100. [DOI] [PubMed] [Google Scholar]
- 9.McIver JI, Scheithauer BW, Rydberg CH, Atkinson JL. Metastatic hepatocellular carcinoma presenting as epidural hematoma: Case report. Neurosurgery. 2001;49:447–9. doi: 10.1097/00006123-200108000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Kanair R, Kubota H, Tenda T, Hate T, Tawaraya E, Fujii K. Spontaneous epidural hematoma due to skull metastasis of hepatocellular carcinoma. J Clin Neurosci. 2009;16:137–40. doi: 10.1016/j.jocn.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Kim BG, Yoon SM, Bac HG, Yun IG. Spontaneous intracranial epidural hematoma originating from dural metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc. 2010;48:166–9. doi: 10.3340/jkns.2010.48.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng FX, Chan Y. Spontaneous intracranial extradural hematoma: Case report and literature review. Neurol India. 2009;57:324–6. doi: 10.4103/0028-3886.53288. [DOI] [PubMed] [Google Scholar]


