Abstract
Background:
The prevalence of water pipe (WP) smoking was studied using a standard questionnaire. Pulmonary function tests were also compared between WP smokers and non-smokers.
Materials and Methods:
The prevalence of WP smoking was studied using a standard questionnaire. Pulmonary function tests including forced vital capacity (FVC), forced expiratory volume in one second (FEV1), maximal mid-expiratory flow (MMEF), peak expiratory flow (PEF), maximal expiratory flow at 75%, 50%, and 25% of the FVC (MEF75,50,25) were compared between WP smokers and non-smokers.
Results:
A total of 673 individuals including 372 males and 301 females were interviewed. The number of WP smokers was 58 (8.6%) including 24 males (6.5%) and 34 females (11.3%). All pulmonary functional test (PFT) values in WP smokers were lower as compared to the non-smokers (P < 0.05 to P < 0.001). The prevalence and severity of respiratory symptoms (RS) in WP smokers were higher than non-smokers (P < 0.05 to P < 0.001). There were negative correlations between PFT values and positive correlation between RS and duration, rate, as well as total smoking (duration X rate) (P < 0.05 to P < 0.001).
Conclusion:
In this study the prevalence of WP smoking in Mashhad city was evaluated for the first time. The results also showed a significant effect of WP smoking on PFT values and respiratory symptoms.
Keywords: Prevalence, pulmonary function tests, respiratory symptoms, water pipe
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in the world.[1] The most important risk factor for COPD is tobacco smoking.[2]
Tobacco smoking using water pipe (WP) (narghile, hubble bubble or hookah) is a traditional way of smoking that is prevalent in Middle east and other parts of Asia.[3] Usually smokers use 10-20 g of tobacco during smoking of WP and the time of smoking is 40-50 minutes.[4] Most users and even physicians believe that water filters the toxic components considerably and is less harmful than cigarette smoking.[5,6,7] Previous studies on main stream smoke of WP showed that the nicotine content of WP tobacco is more than cigarettes (2% to 4%, in comparison with 1% to 3% for cigarettes)[8] and carbon mono oxide (CO) in WP is produced three times more than cigarette.[9] The amount of tar in smoke of WP is less than cigarette smoke,[10] but pyronsynthesized and polycyclic aromatic hydrocarbons are present in the “tar” despite the low temperatures characteristic of the tobacco in the WP.[11] Several studies reported the effect of WP smoke on pulmonary function tests,[8,12,13] small air way function[14] and tonicity of bronchial trees.[15]
Therefore, in the present study the prevalence of WP smoking in the city of Mashhad and the effect of quantity and duration of smoking on pulmonary functional tests (PFTs) and the respiratory symptoms were examined.
MATERIALS AND METHODS
Study area and population
Six hundred seventy-three (673) subjects (372 males aged 43.29 ± 13.23 and 301 females aged 41.84 ± 12.35) were interviewed from 10 randomly selected areas in the city of Mashhad using the cluster sampling method. The data of interviewed subjects regarding the prevalence of smoking of the WP were collected. The city of Mashhad is a holy city located in the north east of Iran with a population of two-million people, many of whom are immigrants from other parts of the country. Respiratory symptoms and PFT values of WP smokers (58 subjects including 24 males and 34 females aged 40.94 ± 11.97) were compared with 50 non-smokers (22 males and 28 females, aged 39.68 ± 12.73, control group) which were matched regarding age, job, race/ethnicity, place of living/working. The study was performed during the period of August-December 2008.
Protocol
A Farsi questionnaire was used to assess the prevalence of WP smoking among population of the city of Mashhad and the respiratory symptoms. The questionnaire had two different parts:
Part (a) questions on WP smoking, number of WP/week), duration of smoking and total amount of smoking (amount X duration)
Part (b) respiratory symptoms (wheezing, breathlessness, cough and sputum). In addition, a non-smoker (control) group from the same area of the city was also interviewed regarding the respiratory symptoms.
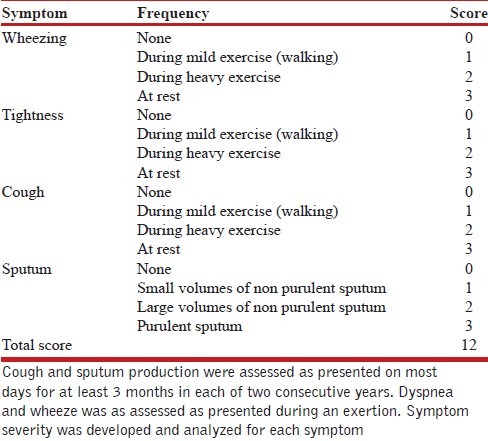
Questionnaire on respiratory symptoms was designed in accordance with several previous questionnaires of similar studies by expert groups [Table 1].[16,17,18,19]
Table 1.
The respiratory symptoms severity score
Pulmonary function tests of smokers and control groups were measured using a spirometer with a pneumotachograph sensor (Model ST90, Fukuda, Sangyo Co., Ltd, Japan). Prior to pulmonary function testing, the required maneuver was demonstrated by the operator, and subjects were encouraged and supervised throughout test performance. Pulmonary function testing was performed using the acceptability standards outlined by the American Thoracic Society (ATS) with subjects in a standing position and wearing nose clips.[20] All tests were carried out between 9:00 and 16:00 hours. Pulmonary function tests were performed three times in each subject with an acceptable technique. The highest level for forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak expiratory flow (PEF), maximal mid expiratory flow (MMEF) and maximal expiratory flow at 75%, 50%, and 25% of the FVC (MEF75, MEF50, and MEF25, respectively) were taken independently from the three curves. The study was approved by the ethical committee of Mashhad University of Medical Sciences.
Statistical analysis
The data of PFT values and age were expressed as mean ± SD and data of smoking and respiratory symptoms as percentage of each group having the corresponding symptom. Differences in the prevalence of symptoms between smokers and control groups were tested by the Chi-square test. PFT values between smokers and control groups were compared using the unpaired t test. The correlation between PFT values and respiratory symptoms with duration and quantity of smoking was assessed using least-square regression. A two-sided P value of 0.05 was the criterion for statistical significance. All analyses were performed with SPSS Software (version 11.5, SPSS In., USA).
RESULTS
Prevalence of water pipe smoking
The prevalence of WP smoking among studied subjects was 8.6% (58 out of 673 subjects) including 6.5% of males (24 out of 372 subjects) and 11.3% of females (34 out of 301 subjects).
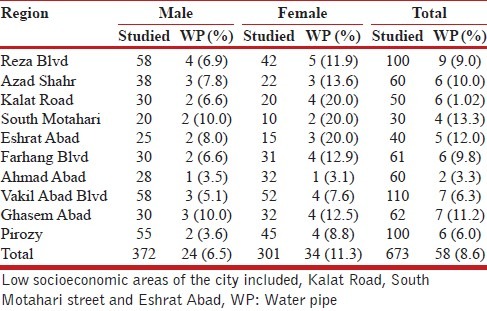
The prevalence of WP smoking was higher in the low socioeconomic areas of the city (Kalat Road, South Motahari street and Eshrat Abad) than the high socioeconomic areas (Ahmad Abad, Pirozi and Vakil Abad Blvd) [Table 2].
Table 2.
Total studied subjects and prevalence of water pipe smoking among different areas of Mashhad city
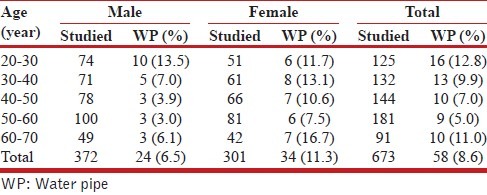
The prevalence of WP smoking was higher in younger individuals (20-40 years old) and lower among 50-60 years old population. The WP smoking was lower among women of 50-60 and 20-30 years aged and was higher in other age groups [Table 3].
Table 3.
Prevalence of water pipe smoking among different age groups in studied population
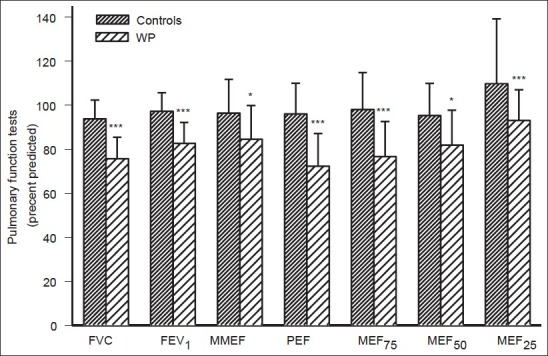
Respiratory symptoms
The most and least prevalent respiratory symptoms among WP smokers were chest tightness (37%) and sputum production (13%), respectively. The most and least prevalent respiratory symptoms among non-smokers were also chest tightness (6.6%) and cough (13%), respectively. The prevalence of all respiratory symptoms among WP smokers (except for the chronic sputum production), (P < 0.05 to P < 0.001), was higher as compared to the control group [Figure 1a]. In addition, the severity of respiratory symptoms among WP smokers (except for chronic sputum production), (P < 0.05 to P < 0.001), was also higher as compared to the control group [Figure 1b].
Figure 1.
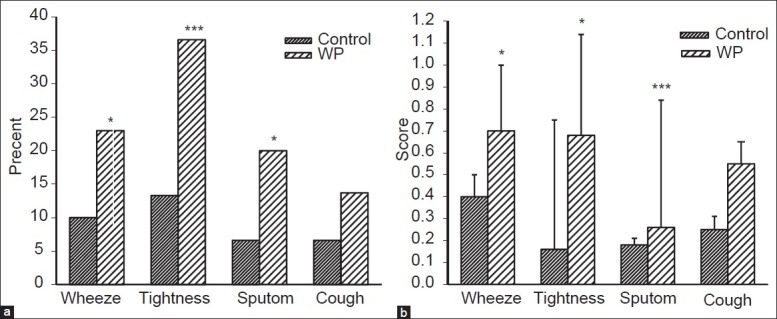
Comparison of prevalence (a) and severity (b) of respiratory symptoms between water pipe (WP) smokers and those of non-smokers. Amount of smoking was expressed in no. of WP/week and total amount of smoking is amount X duration. * = P < 0.05, *** = P < 0.001
Pulmonary function tests
All values of PFT in WP smokers were significantly lower than those of non-smokers (P < 0.05 to P < 0.001) [Figure 2].
Figure 2.
Comparison of pulmonary functional tests (PFT) between water pipe (WP) smokers and non smokers (controls) subjects. Values were presented as mean ± SD of percent predicted (for smokers and non smokers n = 58 and 50 respectively). FVC = Forced vital capacity, FEV1 = Forced expiratory volume in one second, MMEF = Maximal mid expiratory flow, PEF = Peak expiratory flow, MEF75, MEF50, and MEF25 = Maximal expiratory flow at 75%, 50%, and 25% of the FVC, respectively. * = P < 0.005, * = P < 0.001
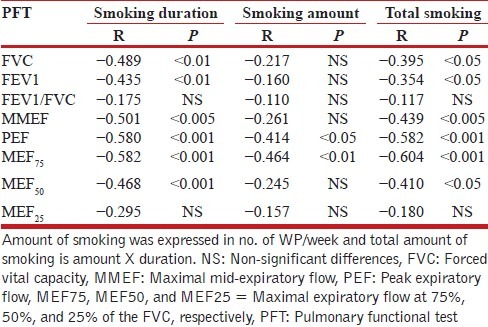
Correlation between smoking duration (year) and amount (pack/year) with pulmonary function tests and respiratory symptoms of smokers
There was no significant correlation between respiratory symptoms and duration or total amount of smoking in WP smokers [Table 4]. However, there was significant negative correlation between PFT values and duration as well as total amount of WP smoking except for MEF25 (P < 0.05 to P < 0.001). This was also true for the amount of smoking with only PEF and MEF75 (P < 0.05 for both cases) [Table 5].
Table 4.
Correlation between respiratory symptoms, smoking duration (year), amount and total smoking in water pipe smokers
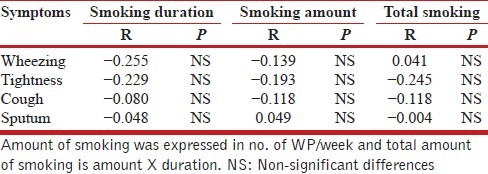
Table 5.
Correlation between PFT values, smoking duration (year), amount and total smoking of water pipe smokers
DISCUSION
In the present study, the prevalence of WP smoking in the city of Mashhad (north east Iran) was studied. The respiratory symptoms and PFT values of WP smokers were also compared with non-smoker subjects. The results showed that 8.6% of the population of the Mashhad city was WP smoker. The prevalence of smoking was lower in male (6.5%) than female (11.3%) subjects. The prevalence of WP smoking was higher in low socioeconomical regions (Kalat Road, South Motahari street and Eshrat Abad) compared to the high socioeconomical areas (Ahmad Abad, Pirozi and Vakil Abad Blvd). The prevalence of WP smoking was higher in younger aged groups (20-40 years old) and was lowest in the 50-60 years old population. The WP smoking was lower among women in studied subjects with 50-60 and 20-30 years old but was higher in other age groups.
Previous studies showed that the prevalence of WP in 13-15 years aged population of 5 different Arabic countries was 10%.[21] It was also shown that 25.5% of male and 4.9% of female students in Syria were WP smokers.[22] In addition, the prevalence of WP smoking in Arab young population was demonstrated to be 26.6%.[23] The prevalence of this type of smoking in Kuwait was 57% for male and 69% for female subjects.[24] The results of other studies showed that the prevalence of WP smoking in Middle East countries was 11-32%[25,26,27,28] which showed a progressive increase.[29] The present study, which is a population-based survey, showed that the prevalence of this type of smoking was lower in the Iranian population as compared to Arabic and other Middle East countries. In fact, the results of a study evaluating the prevalence of WP smoking in patients referred to two hospitals in Tehran showed 9.3% prevalence of WP smoking.[30] The prevalence of WP smoking in Shiraz providence of Iran was also 14%.[31] The results of these two later studies support the findings of our study regarding the prevalence of WP smoking in Iran. The prevalence of WP smoking among students of Birmingham city was also 8%[32] indicating the similar prevalence of this type of smoking in western countries as shown in the present study.
It was shown that the prevalence of WP smoking among Iranian university students was 18.7%[33] which was increased in 2005 compared with 2003.[34] It was also shown that 22% of the male and 8% of the female students had a history of at least one episode of smoking and the most important substance used was cigarette followed by WP.[35] The results of the present study also showed higher prevalence of WP smoking which was higher among male compared female subjects.
The prevalence of WP smoking among Iranian athletes was shown to be 10.5% which was very similar to the results of the present study.[36] The prevalence of WP smoking among Lor migrating tribes in Mamasani, southern Iran (age range, 21-80 years), was 79.9%.[37] The results of a comprehensive study among the population of all regions of Iran showed the prevalence of water pipe smoking of 2.7% (3.5% males and 1.9% females).[38] The prevalence of WP smoking among rural pregnant women in southern Iran was 8%,[39] and among general population in south Iran region (Bandar Abbas) was reported to be 10.4%.[40] Although the results of the later study regarding the prevalence of WP smoking is similar to the results of the present study, the results of three former studies[37,38,39] were different from the results of ours. The reason of these differences is most likely to be due to race/ethnicity differences among study participants.
Regarding the factors that promote use of WP smoking or cigarette smoking, a study on adult residents of Shiraz, Iran, showed that the prevalence of cigarette smoking was 9.7% and that of hookah smoking was 11.9%. A higher perceived level of stress, a non-manual occupation, and sedentary lifestyle were positively associated with cigarette smoking. Manual labor occupations, housewife/jobless status, and going frequently to restaurants were positive predictors of hookah smoking. Although cigarette smoking was 31 times more common in men, the prevalence of hookah smoking in women was the same as men.[41]
In a meta-analysis in an adult population of west of Iran in 25,990 subjects the prevalence smoking was 22.9 (20.6-25.2) and 0.6 (0.3-0.9) in men and women, respectively. Therefore, it was found that more than one-fifth of men from 15 year to 64-year-old of west of Iran smoked cigarette.[42] Our previous study also showed the prevalence of smoking of 12.7% (17.2% in male and 2.5 in female) in a study population of 1435 individuals in north east Iran.[43]
When we look at the data from India, a cross-sectional study in east Delhi showed that the prevalence of current smoking was 24.6%. A majority of current smokers smoked bidi exclusively, and on an average 13.5 bidi/cigarette were smoked per day. Multivariate analysis showed that the factors associated with current smoking were male sex, advancing age, illiteracy, skilled occupation, low socio- economic status, and low BMI (P < 0.001). Low educational status was associated with poor hazard awareness and quitting behavior.[44]
Since 1990, hookah use has increased markedly, spreading from Middle East to the other parts of the world, particularly among younger people, such as college and university students.[45] Studies suggest age, sex and socioeconomic status, as well as close relationship with smokers in family or friend group, emotional stress and history of alcohol and illicit drug use as predictors of smoking.[46,47] It was also shown that WP smoking was higher in younger age groups, female gender and in poor population. The reason of higher prevalence of WP smoking in younger age groups, females and unemployed population is perhaps because this type of smoking is a group smoking behavior.[46,47]
When we look at the data from different parts of world, a systematic review showed that the prevalence of current WP smoking among university students was high in the Persian Gulf region (6%), the United Kingdom (8%), the United States (10%), Syria (15%), Lebanon (28%), and Pakistan (33%). The prevalence of WP smoking among adults of different countries was as the follows: Pakistan (6%), Persian Gulf region (4%-12%), Australia (11% in Arab speaking adults), Syria (9%-12%), and Lebanon (15%)[48] which was similar to the results of our study. The water pip smoking among US population was reported as 29%,[49] among Turkey University students 32.7%[50] and among Jordan University students was also 36.8% (61.9% in male and 10.7% in female students).[51] The prevalence rate of WP smoking among Indian population was reported between 2.6% and 50%.[52] These data showed lower prevalence of WP smoking in the population of the Mashhad compared to the Arab countries but higher than some regions of India.
The results also showed an increased frequency of respiratory symptoms and reduction of all values of pulmonary function tests in WP smokers compared to those of non-smoker subjects. The increased respiratory symptoms and reduction of PFT values in WP smokers showed the effect of this type of smoking on the respiratory system. However, those PFT values indicating the diameter of smaller airways (MMEF, MEF50 and MEF25) were less affected in smokers. There was no significant relationship between quantity and duration of WP smoking and respiratory symptoms which was perhaps due to subjective notion of the data of respiratory symptoms. However, there was a significant and negative correlation between all PFT values and both quantity and duration of smoking. The relationship between respiratory symptoms and PFT values with quantity and duration of smoking are further confirmation of the significant effect of WP smoking on the respiratory system. It was also shown that WP smoking has a similar effect on respiratory symptoms and PFT values as deep inspiration cigarette smoking.[53]
Kiter et al.,[8] also evaluated the effect of WP smoking on PFT values. In addition, the study of Ehteshami Afshar et al., also showed reduction of FEV1 and MMEF in WP smokers in Iran.[30] A more rapid effect of WP smoking on PFT values as compared to cigarette smoking was also shown[54] which may be due to higher nicotine content of WP smoke.[55]
Confounding factors like age, job, race/ethnicity, place of living/working, active/passive smoking and other related variables (other than WP), chemical exposure, underlying diseases and medications may affect respiratory symptoms and PFT values. However, WP smokers and control groups were recruited from the same region of the city with similar age, job, race/ethnicity, place of living/working. Therefore, it seems that these factors have no or minor effect on respiratory symptoms and pulmonary function tests in two groups.
The limitation of the present study was relative small sample size. The comparison of prevalence of WP smoking among different socioeconomic populations, among people of different jobs and educational level and also rural versus urban population is important and needs to be evaluated further.
CONCLUSION
In conclusion, the results of the present study showed 8.6% prevalence of WP smoking among population of the city of Mashhad which was much higher in female as compared to male subjects. The results also demonstrated the profound effect of WP smoking on PFTs values. There were also increased respiratory symptoms among WP smokers.
ACKNOWLEDGEMENTS
This study was financially supported by the Tobacco Prevention and Control Research Centre and also supported by the Research Department of Mashhad University of Medical Sciences. The authors wish to thank Dr. Ramin Sadeghi for editing the manuscript. This paper was the results of a MD thesis.
Footnotes
Source of Support: This study was financially supported by the Tobacco Prevention and Control Research Centre and also supported by the Research Department of Mashhad University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization. World health report. Geneva: World Health Organization; 2000. [Google Scholar]
- 2.Auerbach O, Hammond EC, Garfinkel L, Benante C. Relation of smoking and age to emphysema. Whole-lung section study. N Engl J Med. 1972;286:853–7. doi: 10.1056/NEJM197204202861601. [DOI] [PubMed] [Google Scholar]
- 3.Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: A re-emerging strain in a global epidemic. Tob Control. 2004;13:327–33. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: An emerging health risk behavior. Pediater. 2005;116:e113–9. doi: 10.1542/peds.2004-2173. [DOI] [PubMed] [Google Scholar]
- 5.Varsano S, Ganz I, Eldor N, Garenkin M. Water-pipe tobacco smoking among school children in Israel: Frequencies, habits, and attitudes. Harefuah. 2003;142:736–41, 807. [PubMed] [Google Scholar]
- 6.Romero Palacios PJ. Asthma and tobacco smoke. Arch Bronconeumol. 2004;40:414–8. [PubMed] [Google Scholar]
- 7.Kandela P. Signs of trouble for hubble bubble. Lancet. 1997;349:1460. [Google Scholar]
- 8.Kiter G, Uçan ES, Ceylan E, Kilinç O. Water-pipe smoking and pulmonary functions. Respir Med. 2000;94:891–4. doi: 10.1053/rmed.2000.0859. [DOI] [PubMed] [Google Scholar]
- 9.Sajid KM, Akhter M, Malik GQ. Carbon monoxide fractions in cigarette and hookah (hubble bubble) smoke. J Pak Med Assoc. 1993;43:179–82. [PubMed] [Google Scholar]
- 10.Zahran FM, Ardawi MS, Al-Fayez SF. Carboxyhaemoglobin concentrations in smokers of sheesha and cigarettes in Saudi Arabia. Br Med J (Clin Res Ed) 1985;291:1768–70. doi: 10.1136/bmj.291.6511.1768-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43:655–61. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Al-Fayez SF, Salleh M, Ardawi M, Zahran FM. Effects of sheesha and cigarette smoking on pulmonary function of Saudi males and females. Trop Geogr Med. 1988;40:115–23. [PubMed] [Google Scholar]
- 13.Bayindir U, Ucan ES, Sercin B, Ikiz F. The effect of water-pipe smoking on the peak flow rate. Eur Respir J. 1993;6(Suppl 17):608–11. [Google Scholar]
- 14.Salem ES, El-Soroughi MK, Sharaf El Din M, Ali A. Small airways function among “Goza” versus cigarette smokers. Egypt J Chest Dis Tubercul. 1986;32:36–41. [Google Scholar]
- 15.El-Zahaby MM, Salem ES, Galeb H. Studies on the effect of Goza smoking sublimates on the tonicity of the bronchial tree. Egypt J Chest Dis Tubercul. 1980;23:23–6. [Google Scholar]
- 16.Boskabady MH, Fasihfar M, Maemoori GA. Correlation between symptom score, wheeze, reversibility of pulmonary function tests and treatment response in asthma. Iran J Allergy Asthma Immunol. 2003;2:61–7. [PubMed] [Google Scholar]
- 17.Boskabady MH, Kolahdoz GH. Prevalence of asthma symptoms among the adult population in the city of Mashhad (north-east of Iran) Respirology. 2002;7:267–72. doi: 10.1046/j.1440-1843.2002.00398.x. [DOI] [PubMed] [Google Scholar]
- 18.Bellia V, Pistelli F, Giannini D, Scichilone N, Catalano F, Spatafora M, et al. Questionnaires, spirometry and PEF monitoring in epidemiological studies on elderly respiratory patients. Eur Respir J Suppl. 2003;40:21s–7s. doi: 10.1183/09031936.03.00402303. [DOI] [PubMed] [Google Scholar]
- 19.National Institutes of Health. Global strategy for asthma management and prevention: NHBLI workshop report; Bethesda, MD. 2002. Jan, Publication No. 02-3659. [Google Scholar]
- 20.Standardization of spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Car Med. 1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 21.Global Youth Tobacco Survey Collaborative Group. Tobacco use among youth: A cross country comparison. Tob Control. 2002;11:252–70. doi: 10.1136/tc.11.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maziak W, Fouad FM, Asfar T, Hammal F, Bachir EM, Rastam S, et al. Prevalence and characteristics of narghile moking among uni versity students in Syria. Int J Tuberc Lung Dis. 2004;8:882–9. [PubMed] [Google Scholar]
- 23.Templin T, Rice VH, Gadelrab H, Weglicki L, Hammad A, Kulwicki A, et al. Trends in tobacco use among Arab/Arab-American adolescents: Preliminary findings. Ethn Dis. 2005;15(Suppl 1):S1. [PubMed] [Google Scholar]
- 24.Memon A, Moody PM, Sugathan TN, el-Gerges N, al-Bustan M, al-Shatti A, et al. Epidemiology of smoking among Kuwaiti adults: Prevalence, characteristics, and attitudes. Bull World Health Organ. 2000;78:1306–15. [PMC free article] [PubMed] [Google Scholar]
- 25.Varsano S, Ganz I, Eldor N, Garenkin M. Water-pipe tobacco smoking among school children in Israel: Frequencies, habits, and attitudes. Harefuah. 2003;142:736–41, 807. [PubMed] [Google Scholar]
- 26.Refaat A. Practice and awareness of health risk behaviour among Egyptian University students. East Mediterr Health J. 2004;10:72–81. [PubMed] [Google Scholar]
- 27.Zoughaib SS, Adib SM, Jabbour J. Prevalence and determinants of water pipe or narghile use among students in Beirut's southern suburbs. J Med Liban. 2004;52:142–8. [PubMed] [Google Scholar]
- 28.Tamim H, Terro A, Kassem H, Ghazi A, Khamis TA, Hay MM, et al. Tobacco use by university students, Lebanon, 2001. Addiction. 2003;98:933–9. doi: 10.1046/j.1360-0443.2003.00413.x. [DOI] [PubMed] [Google Scholar]
- 29.Chaaya M, El Roueiheb Z, Chemaitelly H, Azar G, Nasr J, Al-Sahab B. Argileh smoking among university students: A new tobacco epidemic. Nicotine Tob Res. 2004;6:457–63. doi: 10.1080/14622200410001696628. [DOI] [PubMed] [Google Scholar]
- 30.Ehteshami Afshar A, Naghshin R, Amidshahi AA, Fereshtehnejad SM, Naserbakht M. Evalution of the effects of hubble-bubble (waterpipe) smoking on pulmonary functional in patients with respiratory symptoms referred to Hazrat Rasoul and Haft-e-Tir Hospitals in Tehran. J Iran Univ Med Sci. 2006;13:49–57. [Google Scholar]
- 31.Ahmadi Zdeh AR, Tabatabee HR, Fraroei M, Kadivar MR. Prevalence of different type of smoking in Shiraz providence, Iran. Armaghan Danesh J. 2001;6:41–51. [Google Scholar]
- 32.Jackson D, Aveyard P. Waterpipe smoking in students: Prevalence, risk factors, symptoms of addiction, and smoke intake. Evidence from one British University. BMC Public Health. 2008;8:174. doi: 10.1186/1471-2458-8-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sabahy AR, Divsalar K, Bahreinifar S, Marzban M, Nakhaee N. Waterpipe tobacco use among Iranian University students: Correlates and perceived reasons for use. Int J Tuberc Lung Dis. 2011;15:844–7. doi: 10.5588/ijtld.10.0744. [DOI] [PubMed] [Google Scholar]
- 34.Momenan AA, Etemadi A, Ghanbarian A, Azizi F. The rising prevalence of waterpipe smoking among Iranian adolescents: Tehran lipid and glucose study. The 13th World Conference on Tobacco and Health; 2006. pp. 32–3. [Google Scholar]
- 35.Sahraian A, Sharifian M, Omidvar B, Javadpour A. Prevalence of substance abuse among the medical students in southern Iran. Shiraz E-Med J. 2010;11:198–202. [Google Scholar]
- 36.Nakhostin-Roohi B, Valizadeh S. Worrisome prevalence of waterpipe smoking among athletes. Medicina Dello Sport. 2011;64:63–9. [Google Scholar]
- 37.Aghasadeghi K, Zarei-Nezhad M, Keshavarzi A, Mehrabani D. The prevalence of coronary risk factors in Iranian lor migrating ribe. Arch Iran Med. 2008;11:322–5. [PubMed] [Google Scholar]
- 38.Meysamie A, Ghaletaki R, Haghazali M, Asgari F, Rashidi A, Khalilzadeh O, et al. Pattern of tobacco use among the Iranian adult population: Results of the national survey of risk factors of Non-Communicable diseases (SuRFNCD-2007) Tob Control. 2010;19:125–8. doi: 10.1136/tc.2009.030759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mirahmadizadeh A, Nakhaee N. Prevalence of waterpipe smoking among rural pregnant women in southern Iran. Med Princ Pract. 2008;17:435–9. doi: 10.1159/000151563. [DOI] [PubMed] [Google Scholar]
- 40.Tavafian SS, Aghamolaei T, Zare S. Water pipe smoking and health-related quality of life: A population-based study. Arch Iran Med. 2009;12:232–7. [PubMed] [Google Scholar]
- 41.Abdollahifard G, Vakili V, Danaei M, Askarian M, Romito L, Palenik CJ. Are the predictors of hookah smoking differ from those of cigarette smoking. Report of a population-based study in Shiraz, Iran, 2010? Int J Prev Med. 2013;4:459–66. [PMC free article] [PubMed] [Google Scholar]
- 42.Moosazadeh M. Meta-analysis of prevalence of smoking in 15-64-year-old population of west of Iran. Int J Prev Med. 2013;4:1108–14. [PMC free article] [PubMed] [Google Scholar]
- 43.Boskabady MH, Mahmoudinia M, Eslamizade MJ, Boskabady M, Shakeri MT, Heydari GR. The prevalence of smoking among the population in the city of Mashhad (north east of Iran) and pulmonary function tests among smokers. Pneumonol Alergol Pol. 2011;79:21–5. [PubMed] [Google Scholar]
- 44.Garg A, Singh MM, Gupta VK, Garg S, Daga MK, Saha R. Prevalence and correlates of tobacco smoking, awareness of hazards, and quitting behavior among persons aged 30 years or above in a resettlement colony of Delhi, India. Lung India. 2012;29:336–40. doi: 10.4103/0970-2113.102812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giovino GA. The tobacco epidemic in the United States. Am J Prev Med. 2007;33(Suppl 6):S318–26. doi: 10.1016/j.amepre.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 46.Mohammadpoorasl A, Fakhari A, Shamsipour M, Rostami F, Rashidian H. Transitions between the stages of smoking in Iranian adolescents. Prev Med. 2011;52:136–8. doi: 10.1016/j.ypmed.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 47.Maziak W. The waterpipe: Time for action. Addiction. 2008;103:1763–7. doi: 10.1111/j.1360-0443.2008.02327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akl EA, Gunukula SK, 1, Aleem S, 1, Obeid R, Jaoude PA, 1, Honeine R, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: A systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: Knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10:393–8. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Poyrazoğlu S, Sarli S, Genger Z, Günay O. Waterpipe (narghile) smoking among medical and non-medical university students in Turkey. Ups J Med Sci. 2010;115:210–6. doi: 10.3109/03009734.2010.487164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dar-Odeh NS, Bakri FG, Al-Omiri MK, Al-Mashni HM, Eimar HA, Khraisat AS, et al. Narghile (water pipe) smoking among university students in Jordan: Prevalence, pattern and beliefs. Harm Reduct J. 2010;7:10. doi: 10.1186/1477-7517-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ray CS. The hookah-the Indian waterpipe. Cur Sci. 2009;96:1319–23. [Google Scholar]
- 53.Boskabady MH, Farhang L, Mahmodinia M, Boskabady M, Heydari GR. Comparison of pulmonary function and respiratory symptoms in water pipe and cigarette smokers. Respirology. 2012;17:950–6. doi: 10.1111/j.1440-1843.2012.02194.x. [DOI] [PubMed] [Google Scholar]
- 54.White JR, Froeb HF. Small-airways dysfunction in nonsmokers chronically exposed to tobacco smoke. N Engl J Med. 1980;302:720–3. doi: 10.1056/NEJM198003273021304. [DOI] [PubMed] [Google Scholar]
- 55.Hadid Kamal A, Mohammad Faisal I. Nicotine content in tobacco used in hubble-bubble smoking. Saudi Med J. 2004;25:912–7. [PubMed] [Google Scholar]


