Abstract
Two patients presented to us with very similar clinical and radiological presentation of huge hydatid cysts in the lung and liver. The first patient was an 11-year-old female child and the second one was a 9-year-old male child. The clinical features in both were breathlessness on exertion, pain abdomen, and abdominal distension. Chest Roentgenogram along with computed tomogram of the chest and abdomen revealed presence of thin-walled homogenous large cysts, one in the right lung and two in the liver, in both the cases. Although the liver cysts were of larger size and occupying most of the right lobe of the liver and part of the left lobe, liver function tests were normal. All three cysts were enucleated in the same sitting by a combined thoracic and abdominal approach (thoracotomy followed by laparotomy). After enucleation of the cyst, capitonnage of the cavity in the lung was done and the liver cavities were filled with omentum to prevent collection of fluid and abscess formation. Both patients recovered well, although the second patient required abdominal drain for a long period of 1 month for bile leakage which decreased gradually and eventually stopped.
Keywords: Huge hydatid cysts, laparotomy, single-stage management, thoracotomy
INTRODUCTION
There are many large series and reports available in the literature on hydatid disease.[1,2] Hydatid cyst has also been described in many unusual locations;[3,4] however, it is unusual to find huge cysts at multiple locations and organs in the pediatric age group as was seen in these two cases. This report also highlights that surgical intervention for hydatid cysts at multiple sites done in a single stage in the pediatric age group is safe, prevents the need of repeated surgeries, and lessens the financial burden, hospital stay, days of absence from school, and mental stress on the parents and family members of the patients.
Echinococcus granulosus is the pathogenic organism causing the disease and the disease is endemic in many parts of the world.[5,6] The disease is prevalent in a wide range of climatic conditions ranging from the cold climate of Russia to the hot climate of Africa and parts of Asia. The disease is more common in people of lower socioeconomic group due to poor hygiene and is usually transmitted by contaminated water, food, and vegetables. Common sites of involvement are liver, lungs, muscles, and pericardium.
Laboratory investigations useful in diagnosis include indirect hemagglutination tests and eosinophilia on peripheral blood film examination. Casoni's intradermal test is more or less obsolete nowadays. Radiological investigations, especially computed tomogram, play a major role in the diagnosis and further management of the disease, although chest Roentgenogram and ultrasonography of the abdomen are also suggestive of the diagnosis many times. There is usually a homogenous appearance of the cyst without any septae and the cyst wall is well defined with clear margins. Air fluid level or floating membranes may be seen in some cases giving the characteristic appearance of water lily sign, crescent sign,[7] serpent sign,[8] or air-bubble sign, which may be found in cases of ruptured hydatid cysts or complicated cysts with superadded infection.[9]
Surgery is the treatment of choice for the management of large cysts. Small cysts sometimes resolve with medical treatment with albendazole. Needle aspiration of the cyst and injection of scolicidal agents in the cyst cavity under ultrasonographic guidance has been described in the literature, but there is risk of anaphylaxis and its complications.
CASE REPORT
Two patients presented to us with very similar clinical and radiological presentation of large hydatid cysts in the lung and liver. The first patient was an 11-year-old female child and the second was a 9-year-old male child. As the presentation and treatment were similar, the first case is described in detail. The female patient presented with history of pain abdomen, abdominal distension, and breathlessness on exertion for 2 months. Ultrasonography of abdomen revealed multiple large cysts in the liver. Chest roentgenogram [Figure 1a] raised the suspicion of another cystic mass in the lung also. Computed tomogram of the chest and abdomen was done thereafter, which revealed the presence of large cysts in the lung and liver [Figure 1b]. Although the cysts in liver were larger and occupying most of the right lobe of the liver, liver function tests were normal. The liver cyst had pushed the right dome of the diaphragm up and the liver down. Patient was planned for single-stage surgery by combined thoracotomy and laparotomy using separate incisions (single thoracoabdominal incision using transdiaphragmatic approach was avoided to prevent incision in diaphragm, postoperative respiratory dysfunction, and cross contamination). General anesthesia was given using single-lumen endotracheal tube with invasive pressure monitoring. Lateral mini-thoracotomy was done through sixth intercostal space and the cyst was localized in the superior segment of the lower lobe. Cetrimide solution soaked sponges were packed around the cyst to prevent spillage. Pericyst was incised, and with gentle positive pressure ventilation, the cyst came out [Figure 1c]. Capitonnage of the remaining cavity was done using polypropylene sutures 4-0 and bronchial openings found in the cyst were also individually closed with the polypropylene sutures. Standard thoracotomy closure was done after inserting an intercostal tube. Patient was then turned to supine position. Right subcostal incision was used for exposure of the hepatic cysts [Figure 1d]. The liver was found to be grossly enlarged, and both liver cysts were enucleated after incising the cyst wall and packing the surrounding area with sponges soaked in scolicidal solution. We anticipated that approach to the superior liver cyst through the abdominal incision would be difficult and would require mobilization of the liver after division of its ligaments from the diaphragm. However, it was found that the large size of the cyst had made the approach relatively easier without any requirement for mobilization of the liver. Large liver cavities after enucleation were filled with omentum to prevent collection of fluid and abscess formation. Standard closure was done after inserting the drains.
Figure 1.
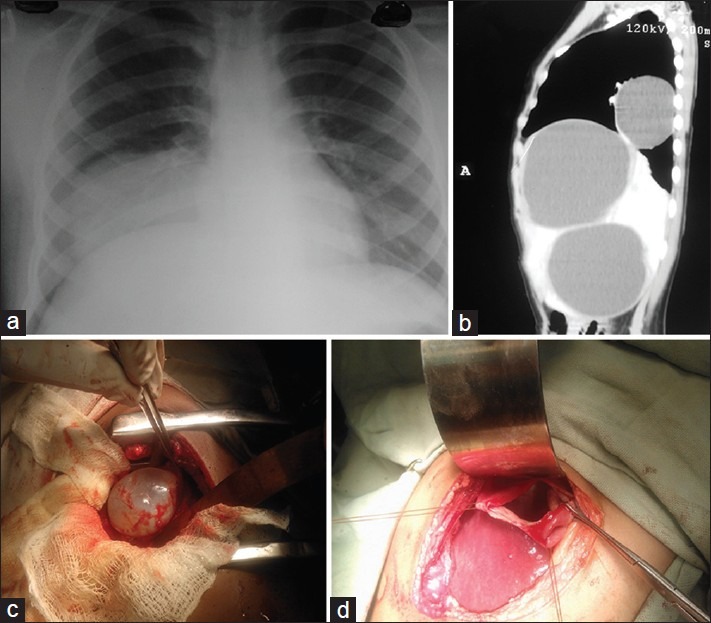
(a) Chest roentgenogram showing hydatid cyst in the lower lobe of the right lung. (b) Computed tomogram chest and abdomen (sagittal section) showing hydatid cyst in the right lung and the liver. (c) Intraoperative photograph showing gross appearance of the hydatid cyst coming out of the right lung with gentle positive pressure ventilation. (d) Intraoperative photograph showing residual cavity after enucleation of the hepatic cyst
In the second case, the cyst in the lung was occupying most of the right thoracic cavity, as seen on chest roentgenogram [Figure 2a] and computed tomogram [Figure 2b and c], and it was enucleated through anterolateral thoracotomy in the fifth intercostal space [Figure 2d] followed by right subcostal incision for the liver cysts. In the postoperative period, there was no air leak in the chest tubes. The chest tubes were removed on the fourth postoperative day after confirmation of the lung expansion on the chest roentgenogram. In the first case, the abdominal drains were removed after 1 week, although the second patient required abdominal drain for a longer period of 1 month for bile leakage which decreased gradually and eventually stopped.
Figure 2.
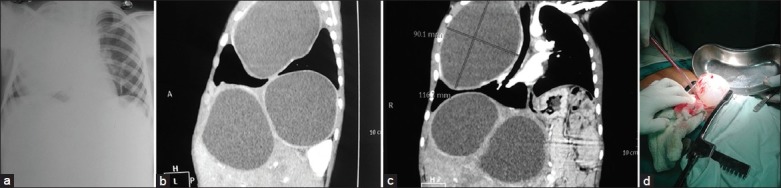
(a) Chest roentgenogram showing hydatid cyst occupying most of the right thoracic cavity. (b) Computed tomogram chest and abdomen (sagittal section) showing huge hydatid cyst in the right lung and the liver. (c) Computed tomogram chest and abdomen (coronal section) showing huge hydatid cyst in the right lung and the liver. (d) Intraoperative photograph showing gross appearance of the hydatid cyst coming out of the right lung with gentle positive pressure ventilation
DISCUSSION
Treatment of hydatid cyst has not changed much over the years, with surgery remaining the mainstay of therapy. Minimal invasive techniques (thoracoscopy and laparoscopy) are also being used, but the risk of rupture of the cyst may be increased as the cyst wall is usually very thin and spillage of contents cannot be easily minimized. Moreover, packing the surrounding area with sponges soaked in scolicidal solution is also not possible.
It is unusual to find such large cysts at multiple sites and organs (as in this case) at such a small age. There are chances of spontaneous rupture in large cysts which can sometimes be fatal or lead to serious morbidity. Surgical intervention is advocated in symptomatic patients with large cysts and in whom medical management has not been successful. There are reports in the literature of staged management[10,11] as well as simultaneous management of pulmonary and hepatic hydatid cysts.[12] In our experience, simultaneous management is a safe option even in the pediatric age group. Presence of large cysts in children can be more damaging than in adults as they tend to compress and destroy the parenchyma of the developing organ and can lead to long-term sequelae of that. Spontaneous cyst rupture can lead to bronchial and biliary fistula for pulmonary and hepatic cysts, respectively.
Reverse Trendelenburg position is helpful during enucleation of the pulmonary hydatid cyst to prevent spillage of contents in the trachea and the dependent lung in case of inadvertent rupture of the cyst while incising the pericyst and enucleation, especially in children in whom the airway is smaller in size and any spillage of contents into the contralateral lung can endanger the life of the patient or can increase the morbidity. Use of double-lumen endotracheal tube is advantageous to prevent spillage of contents in the trachea and the dependent lung in adults with pulmonary hydatid cyst; but in children, single-lumen tubes have to be used, although selective intubation of the contralateral main bronchus can also be successful many times.
Computed tomogram is the investigation of choice, and presence of hydatid cyst at one site should lead to search at other common sites of its occurrence. Treatment at an early stage can prevent the complete destruction of a lobe requiring lobectomy or major resection.
CONCLUSION
Surgical intervention done in a single stage in the pediatric age group for hydatid cysts at multiple sites is safe, prevents the need of repeated surgeries, and lessens the financial burden, hospital stay, days of absence from school, and mental stress on the parents and family members of the patients.
Separate incisions for pulmonary and hepatic cysts can be more beneficial than the transdiaphragmatic approach, as they preserve the diaphragmatic function and prevent the transdiaphragmatic spread of infection, bile leakage, and cross contamination. Reverse Trendelenburg position can be useful to prevent spillage of contents in the trachea and the dependent lung in case of inadvertent rupture during enucleation of the pulmonary hydatid cyst.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Djuricic SM, Grebeldinger S, Kafka DI, Djan I, Vukadin M, Vasiljevic ZV. Cystic echinococcosis in children - the seventeen-year experience of two large medical centers in Serbia. Parasitol Int. 2010;59:257–61. doi: 10.1016/j.parint.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Minaev SV, Gerasimenko IN, Bykov NI, Timofeev SV. Up-to-date approaches in treatment of hydatid disease of the liver in childhood. Vestn Khir Im I I Grek. 2013;172:71–4. [PubMed] [Google Scholar]
- 3.Iyigun O, Uysal S, Sancak R, Hokelek M, Uyar Y, Bernay F, et al. Multiple organ involvement hydatid cysts in a 2-year-old boy. J Trop Pediatr. 2004;50:374–6. doi: 10.1093/tropej/50.6.374. [DOI] [PubMed] [Google Scholar]
- 4.Slim MS, Akel SR. Hydatidosis in childhood. Prog Pediatr Surg. 1982;15:119–29. [PubMed] [Google Scholar]
- 5.Dopchiz MC, Elissondo MC, Andresiuk MV, Maiorini E, Gutiérrez AM, Muzulin PM, et al. Pediatric hydatidosis in the south-east of the Buenos Aires province, Argentina. Rev Argent Microbiol. 2009;41:105–11. [PubMed] [Google Scholar]
- 6.Elburjo M, Gani EA. Surgical management of pulmonary hydatid cysts in children. Thorax. 1995;50:396–8. doi: 10.1136/thx.50.4.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joshi JM. Hydatidothorax. Lung India. 2011;28:315–6. doi: 10.4103/0970-2113.85745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chawla RK, Madan A, Gupta S, Madoiya R, Chawla A, Chawla K. Mother with daughters. Lung India. 2012;29:388–9. doi: 10.4103/0970-2113.102843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biswas D, Dey A, Biswas S, Chakraborty M. It's easy to miss complicated hydatid cyst of lung. Lung India. 2010;27:164–6. doi: 10.4103/0970-2113.68328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chernousov AF, Musaev GK, Abarshalina MV. The surgical treatment of hydatid disease of liver and lungs: The state of art. Khirurgiia (Mosk) 2012:12–7. [PubMed] [Google Scholar]
- 11.Dzhafarov ChM, Rustam-Zade UCh. Surgical treatment of the combined hydatid disease of liver and lung. Khirurgiia (Mosk) 2009:37–40. [PubMed] [Google Scholar]
- 12.Jakob H, Grönniger J, Hürter T, Kohlhäufl M, Höhne U, Oelert H. Simultaneous resection of echinococcus cysts from the liver and lung. Prax Klin Pneumol. 1988;42:435–7. [PubMed] [Google Scholar]


