Abstract
Objective
To examine reciprocal associations between substance use (cigarette smoking, use of alcohol, marijuana, and other illegal drugs) and suicidal ideation among adolescents and young adults (aged 11–21 at wave 1; aged 24–32 at wave 4).
Methods
Four waves public-use Add Health data were used in the analysis (N= 3,342). Respondents were surveyed in 1995, 1996, 2001–2002, and 2008–2009. Current regular smoking, past-year alcohol use, past-year marijuana use, and ever use of other illegal drugs as well as past-year suicidal ideation were measured at the four waves (1995, 1996, 2001–2002, and 2008–2009). Fixed effects models with lagged dependent variables were modeled to test unidirectional associations between substance use and suicidal ideation, and nonrecursive models with feedback loops combining correlated fixed factors were conducted to examine reciprocal relations between each substance use and suicidal ideation, respectively.
Results
After adjusting for the latent time-invariant effects and lagged effects of dependent variables, the unidirectional associations from substance use to suicidal ideation were consistently significant, and vice versa. Nonrecursive model results showed that use of cigarette or alcohol increased risk of suicidal ideation, while suicidal ideation was not associated with cigarette or alcohol use. Reversely, drug use (marijuana and other drugs) did not increase risk of suicidal ideation, but suicidal ideation increased risk of illicit drug use.
Conclusion
The results suggest that relations between substance use and suicidal ideation are unidirectional, with cigarette or alcohol use increasing risk of suicidal ideation and suicidal ideation increasing risk of illicit drug use.
Keywords: suicidal ideation, regular smoking, alcohol use, drug use, adolescents, young adults
1. INTRODUCTION
Suicidal ideation is defined as thoughts of harming or killing oneself (Institute of Medicine, 2002), and it is prevalent among adolescents and young adults. National survey data from high school students in grades 9–12 in 2011 showed that 15.8% of students reported past-year suicidal ideation (Center for Disease Control and Prevention [CDC], 2012). Another national survey data in 2012 indicated that 7.2% of young adults aged 18–25 reported past-year suicidal thoughts, which was highest across adult age groups (Substance Abuse and Mental Health Services Administration [SAMHSA], 2013a). Further, persons having serious suicidal thoughts are more likely to make an actual suicidal attempt than those without, and suicidal attempt is one of the strongest predictors of completed suicide (Bridge et al., 2006). Suicidal ideation also serves as an important marker of psychopathology and behavioral problems among youths (Thompson et al., 2012). Thus, it is important to investigate suicidal ideation and related problems.
Substance use, including use of cigarette, alcohol, marijuana, and other illegal drugs, is another type of risky behaviors among adolescents and young adults. Data from a US national sample of youths aged 12–17 showed that 37% of the youths used alcohol or drugs in the past year, with 32% alcohol, 19% any illicit or nonmedical drugs, and 13% marijuana (Wu et al., 2011). Past-month substance use data from the 2012 National Survey on Drug Use and Health (NSDUH; SAMHSA, 2013b) indicated that 6.6% of youths aged 12–17 were cigarette users, 12.9% alcohol users, 9.5% illicit or nonmedical drug users, and 7.2% marijuana users. Across age groups, young adults aged 21–25 tended to have the highest past-month prevalence of cigarette use (34.1%) and alcohol use (69.2%), and then those aged 26–29 (33.4% cigarette use; 67.0% alcohol use). Among young adults aged 18–25, 21.3% were past-month illicit or nonmedical drug users, and 18.7% marijuana users. In addition, substance use and suicidal ideation often co-exist, with higher rates of suicidal ideation among substance users than nonusers. In a sample of youths from 2001–2009 Youth Risk Behavior Survey (YRBS), Wong et al. (2013) found that 54.4% of youths reported ever smoking regularly, with 20.9% having suicidal ideation in smokers vs. 10.3% in nonsmokers; 74.7% reported lifetime alcohol use, with 19.1% having suicidal ideation in users vs. 8.1% in nonusers. Further, young drug users reported even much higher suicidal ideation than nonusers, e.g., 47.1% in lifetime heroin users vs. 15.3% in nonusers (Wong et al., 2013). Adolescents and young adults constitute a high-risk group for both suicidal ideation and substance use problems, while it is far from conclusive about how the two are related in the literature.
Research findings suggest four possible relations between substance use and suicide ideation by directionality. First, substance use may increase risk of suicide ideation because substance use may induce depressed feelings, decrease abilities of cognitive processing and problem solving, and influence important relationships and school/work performance (Bagge and Sher, 2008). Cross-sectional findings have documented associations between substance use and suicidal ideation (e.g., Wong et al., 2013). Wong et al. (2013) found that each substance use (lifetime use of heroin, inhalant, methamphetamine, steroid, hallucinogen, ecstasy, cocaine, marijuana, alcohol, and ever smoking regularly) was associated with increased odds of suicidal ideation. Findings were mixed from longitudinal studies (Rasic et al., 2013; Pedersen, 2008; Boden et al., 2008; McGee et al., 2005). Rasic et al. (2013) found that current illicit drug use with or without marijuana use was associated with later suicidal ideation over a two-year period, whereas only current marijuana use was not. No significant longitudinal associations were found in other studies after adjusting for confounders (Boden et al., 2008; McGee et al., 2005). The mixed findings may be due to differences in measurement of substance use, selected control variables and samples from different cultural contexts across studies.
Second, although less considered, suicidal ideation may increase risk of substance use (Bagge and Sher, 2008). Individuals with suicidal ideation may use substances as self-medicate methods to escape or relieve suicidal feelings (Bagge and Sher, 2008). To date, little is known about longitudinal relations between prior suicidal ideation and later substance use.
Third, the relation between suicidal ideation and substance use may be bidirectional. That is, suicidal ideation and substance use may affect each other (Dawes et al., 2008). Findings from three longitudinal studies found earlier substance use predicting later suicidal ideation, but did not support the reverse relations (van Ours et al., 2013; Pederson and von Soest, 2008; Bronisch et al., 2008). Van Ours et al. (2013) found that using marijuana several times a week increased the likelihood of suicidal ideation in males, whereas suicidal ideation was not associated with the uptake of marijuana use. The other two studies found that cigarette use (non-dependent and dependent regular smoking in Bronisch et al., 2008; nicotine dependent in Pedersen and von Soest, 2008) was associated with later suicidal ideation, whereas early suicidal ideation was not associated with later initiation of smoking. The three studies analyzed the outcomes as the first episode of suicidal ideation and substance use. This study does not limit to examine the outcomes of the initiation of suicidal ideation and substance use, but tests the reciprocal associations between substance use and suicidal ideation using a nonrecursive model with feedback loops where the two sets of variables are specified as causes and effects of each other concurrently (Fergusson et al., 2011; Kline, 2013).
Finally, the relations between substance use and suicidal ideation may be spurious and explained by third variables (Bagge and Sher, 2008; Dawes et al., 2008). For example, some common factors like impulse control may influence both (Dawes et al., 2008). However, current research provides limited information about the directionality and mechanisms between them. This study employed structural equation modeling (SEM), i.e., incorporating both nonrecursive models and correlated latent time-invariant factors (Fergusson et al., 2011), to address this gap using a national representative sample of adolescents and young adults from the National Longitudinal Study for Adolescent Health (Harris and Udry, 1994–2008). Because of the difficulty of measuring the exact time lag between two effects, the nonrecursive model is a viable alternative to the cross-lagged model for determining reciprocal relations of two conditions (Wong and Law, 1999). We also controlled for the time-invariant unmeasured effects for both suicidal ideation and substance use and permitted them to be correlated (Fergusson et al., 2011). This advanced modeling method can not only estimate whether the relations between substance use and suicidal ideation are reciprocal, but also examine whether parts of the relations are explained by some common fixed factors. Our hypothesis was that the relations between the two were reciprocal and some common fixed factors might account for parts of the relations. We first examined unidirectional associations from substance use to suicidal ideation and vice versa using fixed effects models (FEM) with lagged dependent variables (Bollen and Brand, 2010). This method incorporated classic FEM into a SEM framework. Compared to classic FEM (Allision, 1994), SEM allows the analysis to add lagged effects of dependent variables and generates a variety of model fit indexes (Bollen and Brand, 2010). Finally, the nonrecursive models with correlated latent time-invariant factors were conducted to examine reciprocal relations and the potential existence of some common fixed factors.
2. METHODS
2.1 Data Source
Add Health is a longitudinal study of a nationally representative sample of adolescents in grades 7–12 during 1994–1995 academic years (Harris and Udry, 1994–2008). It includes four waves of in-home interview data, with Wave I data (N=20,745, age=11–21) collected between April and December, 1995, Wave 2 data (N=14,738, age=11–21) collected between April and August in 1996, Wave 3 data (N=15,170, age=18–28) collected between August 2001 and April, 2002, and Wave 4 data (N=15,701, age=24–32) collected in 2008 and 2009. In this paper, we analyzed data from 3,342 respondents who were included in all the four waves’ of public-use dataset.
2.2 Data Collection and Study Variables
Most of the interviews at Wave 1–4 were conducted at respondents’ home. Each interview lasted 1–2 hours depending on their age and experiences. To protect privacy, the audio-computer assisted self-interview technology (ACASI) was used for sensitive health status and behavioral health-related questions (Harris, 2013). The survey contents at Wave 1 and 2 included topics related to adolescents’ health and risk behaviors. At Wave 3 and 4, the contents have expanded to adult roles and responsibilities. The detailed information can be found in Harris, 2013.
Regular smoking at each wave was based on the two variables, including “Have you smoked cigarettes regularly, that is, at least one cigarette every day for 30 days?” and “During the past 30 days, on how many days did you smoke cigarettes?” Respondents who ever smoked regularly and smoked at least one day in the past 30 days were defined as “current regular smokers”.
Alcohol use at each wave was assessed by the item “Over the past 12 months, on how many days did you drink alcohol?” It was originally coded in a 7-point scale, with “1=every day/almost every day” to “7=never”. We recoded it into three mutually exclusive categories. “Weekly use” referred to using alcohol “every day/almost every day” or “3–5 days/week”, or “1 or 2 days/week”; “≤monthly use” referred to using alcohol “2 or 3 days/month”, or “once a month or less (3–12 times in the past 12 months)”, or “1 or 2 days in the past 12 months”. “No use” referred to not using alcohol in the past 12 months.
Marijuana use referred to “ever use” at Wave 1. At Wave 2, 3, and 4, it referred to “use in the past year”. Other drug use referred to “ever use” at Wave 1 and 4; for Wave 2, it referred to “ever use since last interview”; for Wave 3, it referred to “ever use since June 1995.” The other drugs included cocaine, inhalants, crystal meth, LSD, PCP, ecstasy, mushrooms, ice, heroin, or prescription medicines not prescribed to respondents (see additional information in Table 1).
Table 1.
Prevalence and 95% Confidence Interval (CI) of substance use and suicidal ideation a
| Weighted results | Wave 1 | Wave 2 | Wave 3 | Wave 4 |
|---|---|---|---|---|
|
| ||||
| Year of Survey | 1995 | 1996 | 2001–2002 | 2008–2009 |
|
| ||||
| Prevalence % (95% CI) | % (95% CI) | % (95% CI) | % (95%CI) | % (95%CI) |
|
| ||||
| Regular Smoking | ||||
| Yes | 16.0 (13.6–18.4) | 19.7 (17.4–22.1) | 35.1 (32.6–37.6) | 34.4 (32.0–36.9) |
|
| ||||
| Alcohol Use | ||||
| No use | 56.65 (53.1–59.8) | 53.6 (50.7–56.4) | 26.7 (23.7–29.6) | 25.8 (23.4–28.1) |
| ≤ Monthly use | 35.8 (32.9–38.6) | 35.4 (33.1–37.6) | 41.6 (39.2–44.0) | 41.4 (39.1–43.6) |
| Weekly use | 7.6 (6.4–8.7) | 10.9 (9.3–12.4) | 31.4 (28.3–34.6) | 32.8 (29.9–35.6) |
|
| ||||
| b Marijuana Use | ||||
| Yes | 24.2 (21.2–27.2) | 25.4 (22.7–28.0) | 35.2 (32.8–37.6) | 23.5 (21.2–25.8) |
|
| ||||
| c Other Illegal Drugs Use | ||||
| Yes | 11.5 (9.8–13.1) | 8.0 (6.8–9.2) | 33.5 (31.1–35.9) | 36.5 (33.6–39.4) |
|
| ||||
| Suicidal Ideation | ||||
| Yes | 13.4 (11.9–14.8) | 11.6 (10.3–12.8) | 7.2 (6.0–8.3) | 6.4 (5.4–7.4) |
The percentages of missing data on all the studied variables ranged from 0.1–1.8%.
Marijuana use: The variable referred to “ever use” at Wave 1, and it referred to “use in the past year” at Wave 2–4. At Wave 2, respondents were asked “Since last interview, have you tried or used marijuana?” Because the interview gap between Wave 1 and 2 was about one year, marijuana use at Wave 2 was defined as “use in the past year”. At Wave 3, respondents were asked “In the past year, have you used marijuana?” At Wave 4, respondents were asked “during the past 12 months, on how many days did you use marijuana?” It was coded from “0=never” to “6=every day or almost every day”. Respondents who answered “1= 1 or 2 days” to “6=every day or almost every day” were coded as “users”.
Other illegal drug use: At Wave 1, the variable refereed to “ever use”. It was based on three questions, including “How old were you when you tried any kind of cocaine”, “How old were you when you tried inhalants, such as glue or solvents”, and “How old were you when you first tried any other type of illegal drugs, such as LSD, PCP, ecstasy, mushrooms, speed, ice, heroin, or pills, without a doctor’s prescription”. If respondents never tried the above drugs, they were coded as “no users”, otherwise were coded as “users”. At Wave 2, the variable refereed to “since last interview, ever using other illegal drug”. It was based on three questions, including whether respondents having ever tried or used any kind of “cocaine”, “inhalants”, and “any other types of illegal drugs”. Respondents who answered “yes” on any of the three were coded as “users”. At Wave 3, the variable refereed to “since June 1995, ever using other illegal drugs”. It was based on seven questions, including whether using five types of drugs without a doctor’s permission, i.e., “sedatives”, “tranquilizers”, “stimulants”, “pain killers”, “steroids”, and whether using “cocaine”, “crystal meth”, and “other types of illegal drugs”. Respondents who answered “yes” on any of the seven questions were coded as “users”. At Wave 4, it referred to “ever using other types of illegal drugs”. It was based on five questions, including whether using “prescription drugs which are not prescribed”, “steroids”, “cocaine”, “crystal meth”, and “other types of illegal drugs.” Those who answered “yes” on any of the five were coded as “users”.
Suicidal ideation at each wave was assessed by a question “During the past 12 months, did you ever seriously think about committing suicide? (no/yes)”
2.3 Data Analysis
Add Health employed a complex survey design. All analyses considered cluster and sampling weights. Stata 11.0 was used to calculate the prevalences of substance use and suicidal ideation. Logistic regression analyses were conducted to attain unadjusted associations between each substance use and suicidal ideation using the survey options. Mplus 7.1 (Muthén and Muthén, 1998–2012) was used to conduct FEM with lagged dependent variables and nonrecursive models. In the FEM with lagged dependent variables, the effect of unmeasured variables on dependent variables (ŋ) was held constant over time, and it was allowed to correlate with the time-varying covariates. The effects of time-varying variables on dependent variables were held constant over time, that is, the values of path coefficients across waves were assumed equal (Bollen and Brand, 2010). Lagged effects of dependent variables were added in the model to permit previous substance use to predict later substance use, or prior suicidal ideation to predict later suicidal ideation. In the nonrecursive models, the variances of substance use and suicidal ideation were divided into two components: the time-invariant source of variation (ŋ) and the time-varying source of variation (Fergusson et al., 2011). The two time-invariant sources of variations of substance use and suicidal ideation were permitted to correlate. Nonrecursive models with feedback loops have two assumptions: 1) the values of the estimates of the direct effects do not depend upon a particular time point of data collection (equilibrium); and 2) the underlying causal structure does not change over time (stationarity; Kline, 2013). Thus, the estimates of the pathways from substance use to suicidal ideation were assumed equal across waves, so do those from suicidal ideation to substance use.
A robust weighted least squares estimator using a diagonal weight matrix (WLSMV) was specified as an estimator (Muthén and Muthén, 1998–2012). Chi-square, Comparative Fit Index (CFI, Bentler, 1990), and Root Mean Square Error of Approximation (RMSEA, Browne and Cudeck, 1993) were reported as model fit indexes. A CFI greater than 0.95 and RMSEA less than 0.05 indicates good model fit (Hu and Bentler, 1999). We reported unstandardized parameter estimates and standard errors.
3. RESULTS
3.1 Prevalence of Substance Use and Suicidal Ideation (Table 1)
Table 1 summarizes prevalences of substance use and suicidal ideation. In 1995 and 1996, less than 20% of youths were regular smokers, and its prevalence increased to more than 30% in 2001–2002 and 2008–2009. Approximately 10% were weekly alcohol users in 1995 and 1996, while the prevalence increased to 31.4% in 2001–2002 and 32.8% in 2008–2009. Almost 25% of youths had tried marijuana in 1995, and the prevalence of past-year use was 25.4% in 1996; 35.2% in 2001–2002 and 23.5% in 2008–2009. Approximately 12% of youths had tried other drugs in 1995, and the prevalence increased to 36.5% in 2008–2009. Prevalence of suicidal ideation was 13.4% in 1995 and 11.6% in 1996, and it decreased to 6.4% in 2008–2009.
3.2 Unadjusted Associations between Substance Use and Suicidal Ideation (Tables 2–3)
Table 2.
Unadjusted odds ratios (OR) and 95% Confidence Intervals (CI) of suicidal ideation (dependent variable) in relation to substance use status.
| Suicidal Ideation-W1 | Suicidal Ideation-W2 | Suicidal Ideation–W3 | Suicidal Ideation-W4 | |
|---|---|---|---|---|
|
| ||||
| Regular Smoking-Wave 1 | 2.89 (2.25–3.70) *** | 2.41 (1.90–3.06) *** | 1.55 (1.07–2.23) * | ns. |
| Regular Smoking-Wave 2 | 2.83 (2.15–3.71) *** | ns. | 1.48 (1.01–2.18) * | |
| Regular Smoking-Wave 3 | 1.69(1.26–2.28) ** | 1.72 (1.22–2.42) ** | ||
| Regular Smoking-Wave 4 | 1.74 (1.25–2.42) ** | |||
|
| ||||
| Alcohol Use-Wave 1 | ||||
| ≤Monthly Use: No Use | 2.36 (1.81–3.07) *** | 1.76 (1.39–2.23) *** | ns. | ns. |
| Weekly Use: No Use | 3.02 (2.06–4.42) *** | 2.37 (1.60–3.53) *** | ns. | ns. |
|
| ||||
| Alcohol Use–Wave 2 | ||||
| ≤Monthly Use: No Use | 1.99 (1.53–2.58) *** | ns. | ns. | |
| Weekly Use: No Use | 2.40 (1.61–3.57) *** | ns. | ns. | |
|
| ||||
| Alcohol Use-Wave 3 | ||||
| ≤Monthly Use: No Use | 2.35 (1.41–3.92) ** | ns. | ||
| Weekly Use: No Use | 2.57 (1.58–4.16) *** | ns. | ||
| Alcohol Use-Wave 4 | ||||
| ≤Monthly Use: No Use | ns. | |||
| Weekly Use: No Use | ns. | |||
|
| ||||
| Marijuana Use-Wave 1 | 3.09 (2.44–3.91) *** | 2.03 (1.56–2.63) *** | 1.56 (1.08–2.26) * | 1.83 (1.27–2.65) ** |
| Marijuana Use-Wave 2 | 2.59 (2.01–3.32) *** | 1.52 (1.10–2.11) * | ns. | |
| Marijuana Use-Wave 3 | 2.89 (2.05–4.07) *** | 1.46 (1.01–2.09) * | ||
| Marijuana Use-Wave 4 | 1.98 (1.34–2.93) ** | |||
|
| ||||
| Other Illegal Drugs-Wave 1 | 4.57 (3.52–5.94) *** | 3.02 (2.24–4.08) *** | 1.94 (1.29–2.92) ** | 2.17 (1.41–3.35) *** |
| Other Illegal Drugs-Wave 2 | 4.39 (3.19–6.03) *** | 1.66 (1.03–2.66) * | ns. | |
| Other Illegal Drugs-Wave 3 | 3.48 (2.53–4.79) *** | 1.59 (1.17–2.17) ** | ||
| Other Illegal Drugs-Wave 4 | 2.16 (1.53–3.05) *** | |||
Note.
p≤.05,
p<.01,
p<.001. ns., insignificant.
Table 3.
Unadjusted odds ratios (OR) and 95% Confidence Intervals (CI) of substance use (dependent variable) in relation to suicidal ideation status.
| Suicidal Ideation-Wave 1 | Suicidal Ideation-Wave 2 | Suicidal Ideation–Wave 3 | Suicidal Ideation-Wave 4 | |
|---|---|---|---|---|
|
| ||||
| Regular Smoking-Wave 1 | 2.89 (2.25–3.70) *** | |||
| Regular Smoking-Wave 2 | 2.68 (2.14–3.36) *** | 2.82 (2.15–3.71) *** | ||
| Regular Smoking-Wave 3 | 1.58 (1.24–2.03) *** | 1.59 (1.26–2.01) *** | 1.69 (1.26–2.28) ** | |
| Regular Smoking-Wave 4 | 1.86 (1.50–2.30) *** | 1.68 (1.30–2.16) *** | 1.53 (1.16–2.02) ** | 1.74 (1.25–2.42) ** |
|
| ||||
| Alcohol Use-Wave 1 | ||||
| ≤Monthly Use vs. No Use | 2.36 (1.80–3.08) *** | |||
| Weekly Use vs. No Use | 3.02 (2.05–4.43) *** | |||
|
| ||||
| Alcohol Use-Wave 2 | ||||
| ≤Monthly Use vs. No Use | 1.74 (1.36–2.23) *** | 1.99 (1.53–2.58) *** | ||
| Weekly Use vs. No Use | 1.93 (1.34–2.79) ** | 2.40 (1.60–3.59) *** | ||
|
| ||||
| Alcohol Use-Wave 3 | ||||
| ≤Monthly Use vs. No Use | ns. | ns. | 2.35 (1.41–3.94) ** | |
| Weekly Use vs. No Use | ns. | ns. | 2.57 (1.58–4.18) *** | |
|
| ||||
| Alcohol Use-Wave 4 | ||||
| ≤Monthly Use vs. No Use | ns. | ns. | ns. | ns. |
| Weekly Use vs. No Use | ns. | ns. | 1.67 (1.11–2.51) * | ns. |
|
| ||||
| Marijuana Use-Wave 1 | 3.09 (2.44–3.91) *** | |||
| Marijuana Use-Wave 2 | 2.61 (2.04–3.34) *** | 2.59 (2.01–3.32) *** | ||
| Marijuana Use-Wave 3 | 1.57 (1.23–2.00) *** | 1.61 (1.22–2.13) ** | 2.89 (2.05–4.07) *** | |
| Marijuana Use-Wave 4 | 1.63 (1.24–2.15) ** | 1.65 (1.24–2.19) *** | 2.44 (1.70–3.49) *** | 1.98 (1.34–2.93) ** |
|
| ||||
| Other Illegal Drugs-Wave 1 | 4.57 (3.52–5.94) *** | |||
| Other Illegal Drugs-Wave 2 | 3.55 (2.67–4.72) *** | 4.39 (3.19–6.03) *** | ||
| Other Illegal Drugs-Wave 3 | 1.82 (1.44–2.31) *** | 1.92 (1.48–2.50) *** | 3.48 (2.53–4.79) *** | |
| Other Illegal Drugs-Wave 4 | 2.19 (1.71–2.80) *** | 2.29 (1.77–2.97) *** | 2.96 (2.15–4.09) *** | 2.16 (1.53–3.05) *** |
Note.
p≤.05,
p<.01,
p<.001. ns., insignificant.
Table 2 summarizes unadjusted associations from substance use to suicidal ideation. Regular smoking was associated with increased odds of concurrent and subsequent suicidal ideation, except for insignificant associations between regular smoking at Wave 2 and suicidal ideation at Wave 3. Compared to “no use”, “≤monthly use” and “weekly use” alcohol at Wave 1 increased odds of suicidal ideation at Wave 2. No significant associations were found in other subsequent associations between alcohol use and suicidal ideation. The concurrent and sequential associations between drug use (marijuana, other drugs) and suicidal ideation were all significant.
Table 3 summarizes unadjusted associations from suicidal ideation to substance use. The overall findings indicated that suicidal ideation consistently increased odds of concurrent and later substance use, except for alcohol. Suicidal ideation at Wave 1–2 was not associated with alcohol use at Wave 3–4.
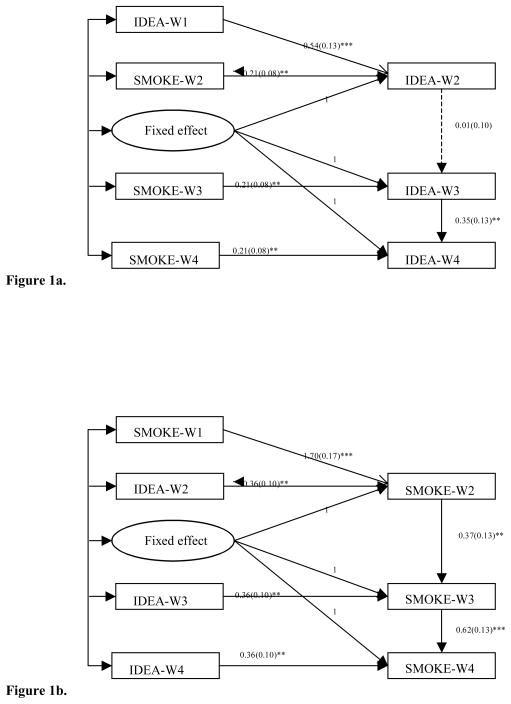
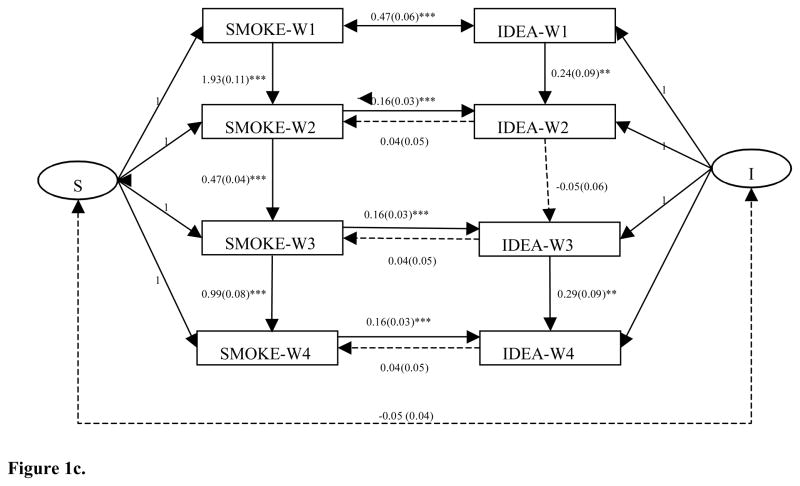
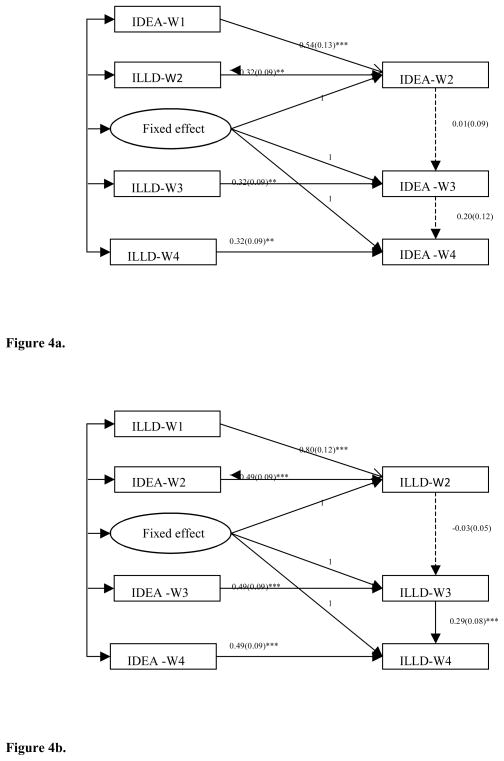
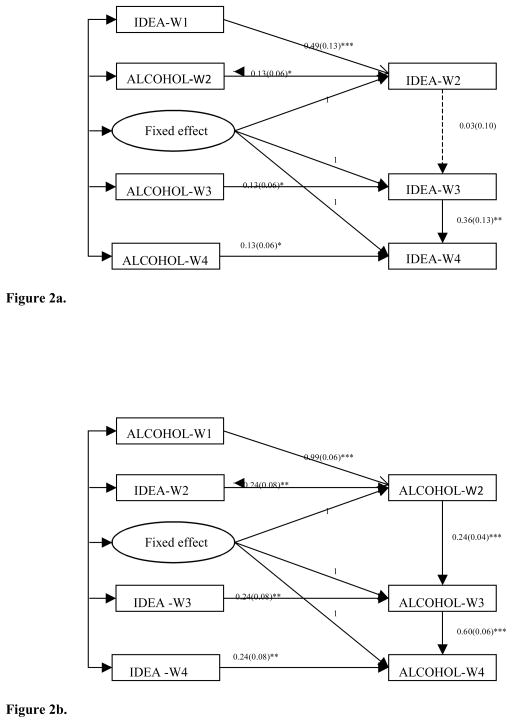
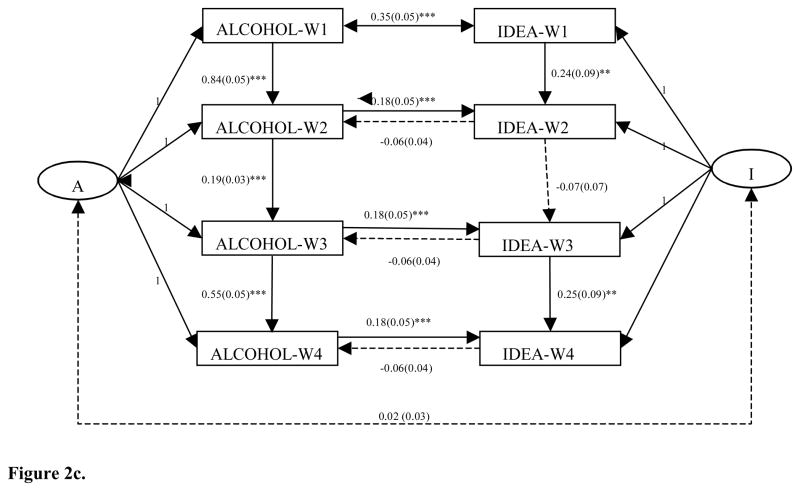
3.3 FEM with Lagged Dependent Variables: Testing Unidirectional Associations from Substance Use to Suicidal Ideation (Figure 1a–4a)
Figure 1.
Figure 1a. Fixed effects model with lagged dependent variables-unidirectional association from current regular smoking to suicidal ideation.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, while not all of them were statistically significant larger than 0. The covariances between fixed effect with current regular smoking at wave 3 and 4 were not significant. IDEA, Suicidal Ideation; SMOKE, Current Regular Smoking.
Figure 1b. Fixed effects model with lagged dependent variables-unidirectional association from suicidal ideation to current regular smoking.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, while not all of them were statistically significant larger than 0. The covariances between fixed effect with suicidal ideaiton at each wave and the covariance between suicidal ideaiton at wave 4 and current regular smoking at wave 1 were not significant. IDEA, Suicidal Ideation; SMOKE, Current Regular Smoking.
Figure 1c. A nonrecursive model: the reciprocal relations between current regular smoking and suicidal ideation.
Note. * p<.05, ** p<.01, *** p<.001. IDEA, Suicidal Ideation; SMOKE, Current Regular Smoking; I, Fixed Effect of Suicidal Ideation; S, Fixed Effect of Current Regular Smoking.
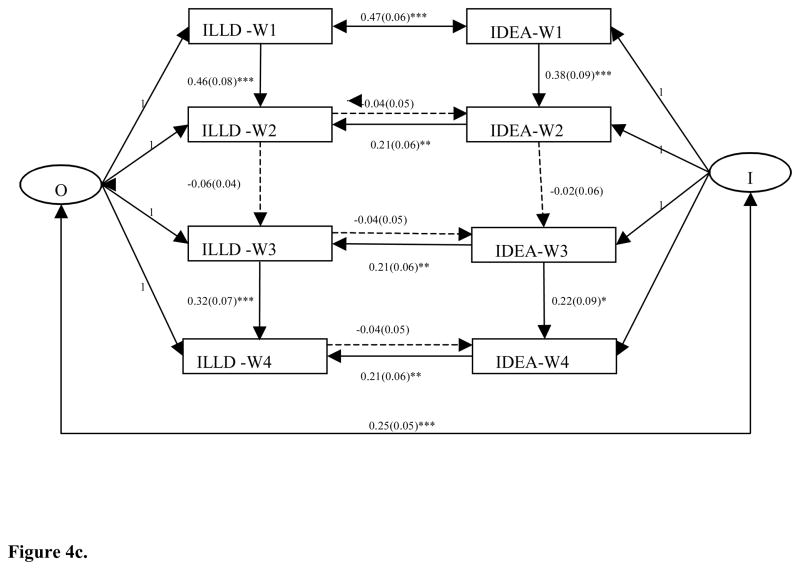
Figure 4.
Figure 4a. Fixed effects model with lagged dependent variables-unidirectional association from ever other illegal drug use to suicidal ideaiton.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, all of them were statistically sifnificant larger than 0. IDEA, Suicidal Ideation; ILLD, Ever Other Illegal Drug Use
Figure 4b. Fixed effects model with lagged dependent variables-unidirectional association from suicidal ideation to other illegal drug use.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, all of them were statistically sifnificant larger than 0, except for the covariance between fixed effect and suicidal ideation at wave 4. IDEA, Suicidal Ideation; ILLD, Ever Other Illegal Drug Use.
Figure 4c. A nonrecursive model: the reciprocal relations between ever other illegal drug use and suicidal ideation.
Note. * p<.05, ** p<.01, *** p<.001. IDEA, Suicidal Ideation; ILLD, Ever Other Illegal Drug Use; I, Fixed Effect of Suicial Ideation; O, Fixed Effect of Other Illegal Drug Use.
All models showed good model fit (regular smoking: χ2=13.10, df=6, p<.05, CFI=0.996, RMSEA=0.019; alcohol use: χ2=19.78, df=6, p<.01, CFI=0.976, RMSEA=0.026; marijuana use: χ2=16.65, df=6, p<.05, CFI=0.991, RMSEA=0.023; other drug use: χ2=45.23, df=6, p<.001, CFI=0.964, RMSEA=0.044. See Supplementary Materials1.). The findings indicated that substance use were associated with increased risk of suicidal ideation after controlling for the fixed effects and lagged effects of suicidal ideation (regular smoking: B=0.21, SE=0.08, p<.01; alcohol use: B= 0.13, SE=0.06, p<.05; marijuana use: B=0.41, SE=0.09, p<.001; other drug use: B=0.32, SE=0.09, p<.01, see Figure 1a–4a). The fixed effects of suicidal ideation were significant larger than 0 (p<.05), except for that in the model of marijuana use and suicidal ideation. Compared to the results of classic FEM without lagged effects of suicidal ideation, the fixed effects reduced when adding lagged effects (classic FEM: ŋ =0.74–0.78, SE=0.07–0.08, p<.001; FEM with lagged effects: ŋ =0.28–0.36, SE=0.14–0.15, p<.05. see Supplementary Material2).
3.4 FEM with Lagged Dependent Variables: Testing Unidirectional Associations from Suicidal Ideation to Substance Use (Figure 1b–4b)
All models indicated good model fit (regular smoking: χ2=6.60, df=6, p>.05, CFI=1.000, RMSEA=0.005; alcohol use: χ2=2.81, df=6, p>.05, CFI=1.000, RMSEA=0.000; marijuana use: χ2=2,97, df=6, p>.05, CFI=1.000, RMSEA=0.000; other drug use: χ2=9.52, df=6, p>.05, CFI=0.997, RMSEA=0.013). Suicidal ideation was significantly associated with increased risk of substance use after controlling for the fixed effects and lagged effects of substance use (regular smoking: B=0.36, SE=0.10, p<.01; alcohol use: B= 0.24, SE=0.08, p<.01; marijuana use: B=0.46, SE=0.10, p<.001; other drug use: B=0.49, SE=0.09, p<.001, see Figure 1b–4b). The impact of fixed effects on substance use reduced with the lagged effects included compared with those of classic FEM.
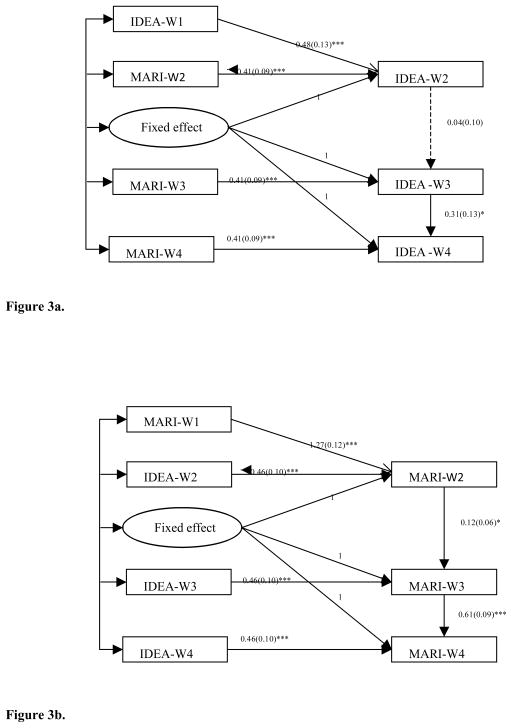
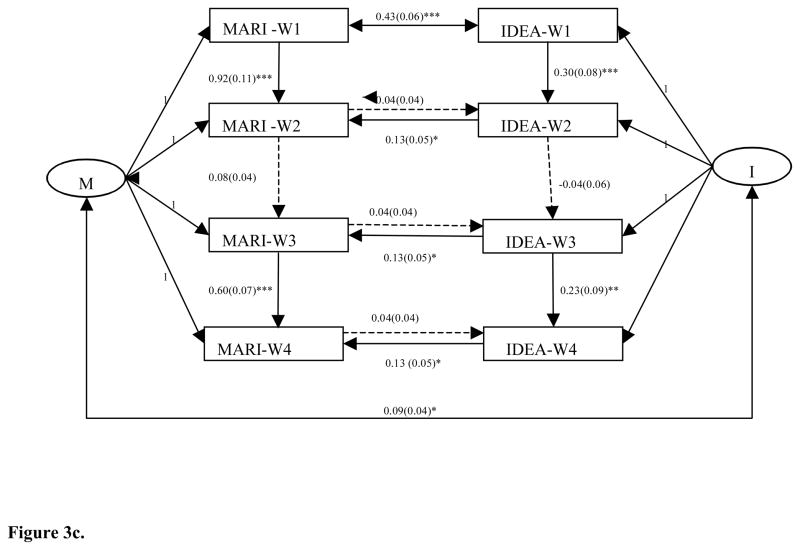
3.5 Nonrecursive Models: Testing Reciprocal Relations between Substance Use and Suicidal Ideation (Figure 1c–4c)
The nonrecursive models also showed good model fit (regular smoking: χ2=28.31, df=17, p<.05, CFI=0.998, RMSEA=0.014; alcohol use: χ2=39.09, df=16, p<.01, CFI=0.990, RMSEA=0.021; marijuana use: χ2=35.15, df=16, p<.01, CFI=0.992, RMSEA=0.019; other drug use: χ2=50.33, df=6, p<.001, CFI=0.982, RMSEA=0.025). The results showed that cigarette/alcohol use increased risk of suicidal ideation (regular smoking: B=0.16, SE=0.03, p<.001; alcohol use: B=0.18, SE=0.05, p<.001), while suicidal ideation was not be a significant determinant of regular smoking (B=0.04, SE=0.05, p>.05) and alcohol use (B=−0.06, SE=0.04, p>.05). Reversely, drug use did not increase risk of suicidal ideation (marijuana use: B=0.04, SE=0.04, p>.05; other drug use: B=−0.04, SE=0.05, p>.05), while suicidal ideation increased risk of drug use (marijuana use: B=0.13, SE=0.05, p<.05; other drug use: B=0.21, SE=0.06, p<.01). In addition, correlations between the fixed effects of cigarette/alcohol use and suicidal ideation were not significant (regular smoking: ŋ1 with ŋ2=−0.05, SE=0.04, p>.05; alcohol use: ŋ1 with ŋ2=0.02, SE=0.03, p>.05), while the fixed effects of drug use and suicidal ideation were significantly correlated (marijuana use: ŋ1 with ŋ2=0.09, SE=0.04, p<.05; other drug use: ŋ1 with ŋ2=0.25, SE=0.05, p<.001).
4. DISCUSSION
This study employed SEM methods to incorporate both correlated fixed factors and reciprocal causal pathways to examine the relations between substance use and suicidal ideation. The overall findings indicate that the relations between the two are unidirectional, while the directions depend on the types of substances used. Specifically, regular smoking/alcohol use increases odds of suicidal ideation, whereas suicidal ideation may not increase regular smoking and alcohol use. Reversely, drug use (marijuana and other drugs) may not lead to increased risk of suicidal ideation, but suicidal ideation increases odds of illicit drug use. In addition, the fixed effects between regular smoking/alcohol use and suicidal ideation are not significantly correlated after controlling for lagged effects and reciprocal causal pathways, which suggests that the correlations between smoking/alcohol use and suicidal ideation may not be partly accounted by some common time-invariant factors (e.g., family and personal characteristics). The significant correlated fixed factors between drug use and suicidal ideation suggest that the correlations between the two are partly explained by some common fixed factors. The findings are discussed below.
In agreement with some of previous findings (Breslau et al., 2005), we find that regular smoking is associated with increased risk of suicidal ideation. This finding is not consistent with those in Boden et al. (2008) and McGee et al. (2005). Boden et al. (2008) found non-significant relations between frequency of cigarette smoking and suicidal ideation after controlling for unmeasured fixed effects in a sample of youths in New Zealand. They concluded that unmeasured background factors might explain the correlation between smoking and suicidal ideation. This is not the case in the present study. After controlling for unmeasured fixed effects and lagged effects, regular smoking remains significant in predicting suicidal ideation (Figure 1a). Additionally, the correlation between the two unmeasured fixed effects is not significant (Figure 1c). Thus, the present data suggest that the relations of the two may be explained by pathways from smoking to suicidal ideation. The differences in measurement of smoking (6 levels in Boden et al., 2008) and culture context (Goldston, 2004) may account for the discrepant findings. Several possible mechanisms could explain the link from smoking to suicidal ideation, including worsened behavioral problems (e.g., negative affect, impulsivity, and aggression), reduced levels of serotonin and monoamine oxidase-A and -B, and physical illness (Hughes, 2008).
As for the relations from suicidal ideation to regular smoking, although we find significant path coefficients in the model of testing unidirectional associations (Figure 1b), we do not find those in the nonrecursive model (Figure 1c). The latter model is more comprehensive, thus the present data suggest that suicidal ideation may not lead to increased risk of regular smoking. It is consistent with previous findings using the first episodes of outcomes (e.g., Perdersen and von Soest, 2008).
Similar to prior findings about the relations between smoking and suicidal ideation, our data suggest that alcohol use increases risk for suicidal ideation, while the reverse relations are not supported. One explanation is that alcohol use may increase psychological distress, aggression, impulsivity and decrease cognitive processing and problem solving shortly (Bagge and Sher, 2008). Also, in the long run, alcohol use may increase changes in biology and have negative impacts on important relationships and work/school performance (Bagge and Sher, 2008).
In contrast to the relations between smoking/alcohol use and suicidal ideation, drug use (marijuana and other drugs), is not associated with suicidal ideation, whereas suicidal ideation increases use of illicit drugs. The results are in line with the pattern of the “self-medication” hypothesis (Goldston, 2004). Suicidal youths may encounter a series of problems, e.g., mental health illness, sexual abuse, family discord, or poor peer relationships (Evans et al., 2004), which may trigger youths to use drugs to cope. Additionally, the relations between drug use and suicidal ideation can partly be explained by some common fixed factors such as impulsivity (Goldston, 2004).
There are limitations in this study. First, we used self-report data on suicidal ideation and substance use. Although the sensitive information was entered privately by youths using the ACASI to enhance privacy and honest reporting, there was potential measurement error (e.g., underreporting), which might impact the estimates. Second, the measurements of other drug use were not current use status, and were inconsistent across the four waves, which might underestimate drug use. Third, we assumed that the relations between substance use and suicidal ideation were constant over time because of modeling methods. Future research needs to examine whether the relations change or are constant over the course of development. Fourth, we recognized that a small proportion of youth used multiple substances (SAMHSA, 2013b; Wu et al., 2011). Polysubstance use is associated with high rates of substance dependence problems in young adulthood (Moss et al., 2014). Thus, additional research is needed to delineate the reciprocal associations between polysubstance use and suicidal outcomes.
Nonetheless, to better understand associations of suicidal ideation and substance use, we examine the relations between suicidal ideation and each of the four substance classes (cigarettes, alcohol, marijuana, other drugs), respectively. This is the first of its kind to examine both reciprocal relations and common background factors between suicidal ideation and four groups of substance use, and these analyses suggest that the correlation between smoking/alcohol use and suicidal ideation may largely be explained by direct pathways, while the correlation between drug use and suicidal ideation is accounted by both direct pathways and correlated fixed factors. These results from longitudinal data analyses make unique contributions to the literature. In addition, we use a nationally representative sample of adolescents and young adults, thus the findings have some strength in generalizability.
Suicide is the third leading cause of death among youths aged 15–24, and second among those aged 25–34 (CDC, 2010). Substance use is another major public health threat, and increasingly plays a role for suicide (Center for Substance Abuse Treatment, 2008). Findings show that regular smoking/alcohol use increases risk of suicidal ideation, and suicidal ideation increases risk for drug use. Litts and Carr (2013) state that “substance abuse prevention is suicide prevention”, and they advocate stronger collaboration between the two prevention fields at all the levels (community, state, tribal, and national). Similarly, mental health care and substance abuse treatment providers should align their efforts to screen, identify, and treat youths with the co-occurring conditions. Estimates from the 2012 NSDUH showed that only 7.9% people with both mental illness and substance use problems received both services in the past year (SAMHSA, 2013a). Further, due to a lack of coordination between mental health and substance abuse treatment systems, many who are cross-referred fail to receive treatment; thus, there is a clear need for promoting an integrated approach to care (Hawkins, 2009). Finally, clinical trials often target either suicidal conditions or substance abuse, and exclude youths with both problems (Goldston, 2004). Available data showed that the integrated treatment was associated with significant improvement in both substance use and suicidal behaviors (Esposito-Smythers et al., 2011). All the above speaks to the ongoing need to intervene and prevent both suicidal and substance use problems among youths.
Supplementary Material
Figure 2.
Figure 2a. Fixed effects model with lagged dependent variables-unidirectonal associaton from past-year alcohol use to suicidal ideaiton.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, while not all of them were statistically sifnificant larger than 0. The covariances between fixed effect with past-year alcohol at each wave, and the covariances between suicidal ideation at wave 1 with past-year alcohol use at wave 3 and 4 were not sginificant. IDEA, Suicidal Ideation; ALCOHOL, Past-year Alcohol Use.
Figure 2b. Fixed effects model with lagged dependent variables-unidirectional association from suicidal ideation to past-year alcohol use.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, while not all of them were statistically sifnificant larger than 0. The covariances between fixed effect with suicidal ideaiton at each wave, and the covariances between suicidal ideaiton at wave 3 with past-year alcohol use at wave 1 were not significant. IDEA, Suicidal Ideation; ALCOHOL, Past-year Alcohol Use.
Figure 2c. A nonrecursive model: the reciprocal relations between past-year alcohol use and suicidal ideation.
Note. * p<.05, ** p<.01, *** p<.001. IDEA, Suicidal Ideation; Alcohol, Past-Year Alcohol Use; I, Fixed Effect of Suicial Ideation; A, Fixed Effect of Past-Year Alcohol Use.
Figure 3.
Figure 3a. Fixed effect model with lagged dependent variables-unidirectional assocication from past-year marijuana use to suicidal ideation.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, while not all of them were statistically sifnificant larger than 0. The covariances between fixed effect and past-year marijuana use at each wave were not statisitcally significant. IDEA, Suicidal Ideation; MARI, Past-year Marijuana Use
Figure 3b. Fixed effects model with lagged dependent variables-unidirectional association from suicidal ideation to past-year marijuana use.
Note. * p<.05, ** p<.01, *** p<.001. All the covariances among exogenous variables were specified in the model, and all of them were statistically sifnificant larger than 0, except for the covariance between fixed effect and suicidal ideation at wave 4. IDEA, Suicidal Ideation; MARI, Past-year Marijuana Use.
Figure 3c. A nonrecursive model: the reciprocal relations between past-year marijuana use and suicidal ideaton.
Note. * p<.05, ** p<.01, *** p<.001. IDEA, Suicidal Ideation; MARI, Past-Year Marijuana Use; I, Fixed Effect of Suicial Ideation; M, Fixed Effect of Past-Year Marijuana Use.
Acknowledgments
Role of the funding source: This work was made possible by research support from the U.S. National Institutes of Health (R01MD007658, R01DA019623, R01DA019901, R33DA027503 to Li-Tzy Wu) and by Duke University Department of Psychiatry and Behavioral Sciences. The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Contributors: Xiaoyun Zhang contributed to study designs, conducted data analyses, and drafted the manuscripts. Li-Tzy Wu contributed to study designs and analyses, drafted the manuscripts, and supervised the work.
Conflict of Interest: The other authors have no conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allison PD. Using panel data to estimate the effects of events. Sociol Method Res. 1994;23:179–199. [Google Scholar]
- Bagge CL, Sher KJ. Adolescent alcohol involvement and suicide attempts: toward the development of a conceptual framework. Clin Psychol Rev. 2008;28:1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Cigarette smoking and suicidal behavior: results from a 25-year longitudinal study. Psychol Med. 2008;38:433–439. doi: 10.1017/S0033291707001547. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Brand JE. A general panel model with random and fixed effects: a structural equations approach. Soc Forces. 2010;89:1–34. doi: 10.1353/sof.2010.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC. Smoking and the risk of suicidal behavior: a prospective study of a community sample. Arch Gen Psychiatry. 2005;62:328–334. doi: 10.1001/archpsyc.62.3.328. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Bronisch T, Höfler M, Lieb R. Smoking predicts suicidality: findings from a prospective community study. J Affect Disord. 2008;108:135–145. doi: 10.1016/j.jad.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage Publications; Thousand Oaks, CA: 1993. pp. 136–162. [Google Scholar]
- Center for Disease Control and Prevention. Youth risk behavior surveillance-United States, 2011. MMWR. 2012;61:1–45. [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance Abuse and Suicide Prevention: Evidence and Implications-A White Paper. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2008. DHHS Pub. No. SMA-08-4352. [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [online] National Center for Injury Prevention and Control; 2010. Retrieved on Jan 22, 2014 from www.cdc.gov/injury/wisqars/index.html. [Google Scholar]
- Dawes MA, Mathias CW, Richard DM, Hill-Kapturczak N, Dougherty DM. Adolescent suicidal behavior and substance use: developmental mechanisms. Subst Abuse. 2008;2:13–28. doi: 10.4137/sart.s1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Moti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. J Consult Clin Psychol. 2011;79:728–739. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clin Psychol Rev. 2004;24:957–979. doi: 10.1016/j.cpr.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2011;46:933–942. doi: 10.1007/s00127-010-0268-1. [DOI] [PubMed] [Google Scholar]
- Goldston DB. Conceptual issues in understanding the relationship between suicidal behavior and substance use during adolescence. Drug Alcohol Depend. 2004;76S:S79–S91. doi: 10.1016/j.drugalcdep.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Harris KM, Udry JR. National Longitudinal Study of Adolescent Health (Add Health), 1994–2008. ICPSR21600-v12. Inter-university Consortium for Political and Social Research [distributor]; 2013-03-08; Ann Arbor, MI. 1994–2008. [DOI] [Google Scholar]
- Harris KM. The Add Health Study: design and accomplishments. 2013 Retrieved on Jan. 22, 2014 from http://www.cpc.unc.edu/projects/addhealth/data/guides/DesignPaperWIIV.pdf.
- Hawkins EH. A tale of two systems: co-occurring mental health and substance abuse disorders treatment for adolescents. Annu Rev Psychol. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Hughes JR. Smoking and suicide: a brief overview. Drug Alcohol Depend. 2008;98:169–178. doi: 10.1016/j.drugalcdep.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Reducing Suicide: A National Imperative. The National Academies Press; Washtington, DC: 2002. [PubMed] [Google Scholar]
- Kline RB. Reverse arrow dynamics: feedback loops and formative measurement. In: Hancock GR, Mueller RO, editors. Structural Equation Modeling: A Second Course. 2. Information Age Publishing; Charlotte, NC: 2013. pp. 39–77. [Google Scholar]
- Litts DA, Carr C. Substance abuse prevention is suicide prevention. 2013 Retrieved on Jan. 30, 2013 from http://www.whitehouse.gov/blog/2013/09/10/substance-abuse-prevention-suicide-prevention.
- McGee R, Williams S, Nada-Raja S. Is cigarette smoking associated with suicidal ideation among young people? Am J Psychiatry. 2005;162:619–620. doi: 10.1176/appi.ajp.162.3.619. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi H-y. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Muthén & Muthén; Los Angeles, CA: 1998–2012. [Google Scholar]
- Pedersen W. Does cannabis use lead to depression and suicidal behaviors? A population-based longitudinal study. Acta Psychiatr Scand. 2008;118:395–403. doi: 10.1111/j.1600-0447.2008.01259.x. [DOI] [PubMed] [Google Scholar]
- Pedersen W, von Soest T. Smoking, nicotine dependence and mental health among young adults: a 13-year population-based longitudinal study. Addiction. 2008;104:129–137. doi: 10.1111/j.1360-0443.2008.02395.x. [DOI] [PubMed] [Google Scholar]
- Rasic D, Weerasinghe S, Asbridge M, Langille DB. Longitudinal associations of cannabis and illicit drug use with depression, suicidal ideation and suicidal attempts among Nova Scotia high school students. Drug Alcohol Depend. 2013;129:49–53. doi: 10.1016/j.drugalcdep.2012.09.009. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013a. NSDUH Series H-47, HHS Publication No. (SMA) 13-4805. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013b. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- Thompson R, Proctor LJ, English DJ, Dubowitz H, Narasimhan S, Everson MD. Suicidal ideation in adolescence: examining the role of recent adverse experiences. J Adolesc. 2012;35:175–186. doi: 10.1016/j.adolescence.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ours JC, Williams J, Fergusson D, Horwood LJ. Cannabis use and suicidal ideation. J Health Econ. 2013;32:524–537. doi: 10.1016/j.jhealeco.2013.02.002. [DOI] [PubMed] [Google Scholar]
- Wong CS, Law KS. Testing reciprocal relations by nonrecursive structural equation models using cross-sectional data. Organ Res Methods. 1999;2:69–87. [Google Scholar]
- Wong SS, Zhou B, Goebert D, Hishinuma ES. The risk of suicide across patterns of drug use: a nationally representative study of high school students in the United States from 1999 to 2009. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1611–20. doi: 10.1007/s00127-013-0721-z. [DOI] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/Ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.