Abstract
Background: Low-fat and low-carbohydrate weight-loss diets can have a beneficial effect on longitudinal measures of blood pressure and blood lipids. We aimed to assess longitudinal changes in blood pressure and blood lipids in a population of premenopausal women. We hypothesized that results may differ by level of adherence to the respective diet protocol and baseline presence of hypertension or hyperlipidemia.
Methods: Overweight or obese premenopausal women were randomized to a low-fat (n=41) or low-carbohydrate (n=38) diet. As part of the 52-week Lifestyle Eating and Fitness (LEAF) intervention trial, we fit linear mixed models to determine whether a change in outcome differed by treatment arm.
Results: Within-group trends in blood pressure and blood lipids did not differ (p>0.30). Across study arms, there was a significant decrease in systolic blood pressure (SBP, 3 mm Hg, p=0.01) over time, but diastolic blood pressure (DBP) did not change significantly over the course of the study. Blood lipids (total cholesterol [TC], low-density lipoproteins [LDL], and high-density lipoproteins [HDL]) all exhibited nonlinear trends over time (p<0.01); each decreased initially but returned to levels comparable to baseline by study conclusion (p>0.20). We observed a decline in SBP among women who were hypertensive at baseline (p<0.01), but hypercholesterolemia at baseline did not affect trends in blood lipids (p>0.40).
Conclusions: Our results support that dietary interventions may be efficacious for lowering blood pressure and blood lipids among overweight or obese premenopausal women. However, a decrease in SBP was the only favorable change that was sustained in this study population. These changes can be maintained over the course of a 1-year intervention, yet changes in blood lipids may be less sustainable.
Introduction
Hypercholesterolemia and hypertension are established risk factors for cardiovascular disease (CVD).1 Observational data indicate that a healthy diet and regular physical activity are associated with attainment of optimal levels of both blood lipids and blood pressure.2 Highly processed diets of low nutrient density, as well as physical inactivity, have been shown to contribute to overweight and obesity, which are also important risk factors for CVD.3 Indeed, the most recent diet and lifestyle recommendations from the American Heart Association encourage a healthy diet, body weight, optimal lipid and blood pressure levels, and physical activity in order to lower risk for CVD.4
In the context of randomized controlled trial (RCT) data, both hypertensive and prehypertensive participants showed improvements in blood pressure and blood lipids with adoption of the low-sodium and low-fat Dietary Approaches to Stop Hypertension (DASH) diet.5–7 In addition, regular physical activity has been shown to lower both systolic blood pressure (SBP) and diastolic blood pressure (DBP) among hypertensive and prehypertensive exercise-program participants.8 Extant data from RCTs comparing low-fat to low-carbohydrate diets vary in the type of diet, such as very low carbohydrate9,10 or Atkins,11 and composition of the study population, such as nondiabetic11,12 men and women.9–12
A recent meta-analysis of RCTs comparing low-fat and low-carbohydrate diets found that both types of diets decreased weight, yet the results favored low-carbohydrate diets for more beneficial changes in total cholesterol (TC), low-density lipoproteins (LDL), and high-density lipoproteins (HDL).13 An earlier meta-analysis of RCTs comparing low-fat and low-carbohydrate diets concluded that TC and LDL changed more favorably among participants assigned to low-fat diets, yet participants in the low-carbohydrate arms of the trials tended to experience more weight loss and more healthy HDL values.14 These measures showed a greater improvement in the first 6 months but not at 12 months.14 Differences in blood pressure were not observed between participants enrolled in the low-fat and low-carbohydrate diet arms of the 28 trials comprising the two meta-analyses.13,14
The overarching aim of the current study was to investigate dietary interventions—in the context of increased physical activity—that could prevent breast cancer in women. The study population was chosen because little information was known about breast cancer prevention in younger (premenopausal) overweight women. In the context of this parent study, we evaluated the effects of low-fat and low-carbohydrate weight-loss diets on longitudinal measures of blood pressure and blood lipids among overweight or obese premenopausal women who were also advised to increase their level of physical activity. We hypothesized that we would observe favorable changes over time in blood pressure and blood lipids in both diet groups but that results would differ by level of adherence to the respective diet protocol and baseline presence of hypertension or hyperlipidemia.
Materials and Methods
Study design and participants
The Lifestyle Eating and Fitness (LEAF) study was a 52-week randomized intervention pilot trial of low-fat and low-carbohydrate weight-loss diets. The primary aim of the LEAF study was to investigate changes in body weight in each arm of the trial, as dietary interventions to prevent breast cancer had not yet been undertaken in younger (premenopausal) overweight women. The aim of this secondary analysis was to investigate changes in blood pressure and blood lipids in both diet groups. Women were recruited from physician offices in Columbus, Ohio, and through media advertisements. Interested women called a designated phone number and spoke to an Ohio State University (OSU) Comprehensive Cancer Center staff member who was trained to provide general study information and to screen eligible subjects. Women deemed eligible following the screening were scheduled for an enrollment visit at which the study was explained in more detail and informed consent was obtained. This study was approved by the OSU Institutional Review Board.
Eligible participants were overweight and obese premenopausal women aged 30 or older with a body mass index (BMI) in the overweight and obese range of 25–34 kg/m2. Women were included if they had no prior diagnosis of cancer (except nonmelanoma skin cancer); planned to live in the Columbus, Ohio, area during the 18-month follow-up; and obtained a letter of medical clearance from their primary physician to participate. Women were considered ineligible for the study if they were pregnant or planning to become pregnant during the study period; were currently participating in a weight-loss program, such as Weight Watchers; had medical conditions that precluded dietary adherence; or lacked management or control of existing medical problems.
Of the 82 eligible women who consented to participate in the study, 3 withdrew prior to the baseline visit, resulting in a sample size of 79 women. Forty-one women were randomized to the low-fat diet and 38 to the low-carbohydrate diet (Supplementary Fig. S1; Supplementary Data are available online at www.liebertpub.com/jwh). The randomization strategy, based on BMI (kg/m2), ensured an equitable distribution of overweight and obese subjects to each diet.
Diet intervention
The low-fat diet recommended 20% of total calories from fat, 20% from protein, and 60% from carbohydrates; the low-carbohydrate diet, 40% of total calories from carbohydrates, 30% from protein, and 30% from fat. All women received counseling regarding their respective calorie-restricted diet, along with an individualized physical-activity prescription to promote weight loss.
Registered dietitians (RDs) provided each participant with a calorie goal based on the Harris-Benedict equation.15 The diet education was based on the American Dietetic Association's Exchange System plan.16,17 Each participant met with an RD at OSU's General Clinical Research Center (GCRC) once per week for the first month of the study, then every 3 weeks through the fourth month of the study, and then every 6 weeks through the remainder of the study, except for the scheduled in-person clinic visits during weeks 34 and 52. The participants met with the same RD throughout the study. If the participant could not come to the GCRC, the counseling sessions were conducted by phone. All women were asked to complete, and bring to their next appointment, a 7-day diet record at the beginning of each of 12 study months. Diet records were analyzed by Food Processor software (ESHA Research, Salem, OR), which established the level of adherence to the assigned diet and helped direct individual nutrition counseling. Adherence to the diet protocol was defined for each participant as being within 20% of her caloric goal (80%–120% attainment) for carbohydrates or fats, in keeping with the study arm, according to her final diet record.
Physical-activity advice
Participants monitored their physical activity by wearing a Digiwalker™ pedometer (Yamax-Digiwalker, Warminster, PA) and recording their total steps walked per day. Each participant was advised to walk 10,000 steps per day, which roughly equates to 3 miles of walking. Adherence to physical-activity advice was defined for each participant as attaining 80% or more of her goal of 10,000 steps per day. We averaged steps per day over the course of the study to determine physical-activity adherence.
Clinic measurements
Each participant was scheduled to complete five in-person visits to the GCRC. The visits included screening, baseline, week 12, week 34, and week 52 (within 4 weeks of the scheduled close-out date). Demographic and health behavior data were assessed via baseline questionnaire; quality-of-life factors were assessed at all visits. At each GCRC visit, a blood draw and anthropometric measurements were completed. Anthropometric tests included blood pressure, body weight, body composition, skinfold, and waist-to-hip ratio measurements. Blood lipids (TC, LDL, and HDL), as well as SBP and DBP, were measured at each in-person clinic visit.
Blood pressure was measured according to GCRC protocol. The participant was seated with her legs uncrossed and her feet flat on the floor. SBP and DBP were measured via sphygmomanometer and documented to the nearest 2 mm Hg. Fasting TC was analyzed using Beckman Coulter LX20 (Indianapolis, IN) instrumentation and the timed-endpoint method.
Statistical analyses
Longitudinal measures of blood pressure and blood lipids were analyzed using linear mixed models. In studies with incomplete follow-up (such as LEAF), mixed models provide unbiased estimates of treatment effects under the assumption of missing at random (MAR).18 In the first step of the model-building process, we evaluated the functional form of time for each outcome of interest (TC, LDL, HDL, SBP, and DBP). We compared linear, quadratic, and cubic trends and selected the model with the smallest Bayesian Information Criterion.
The final model included the following fixed effects: diet, the appropriate polynomial terms for time, and diet-by-time interactions. The models for SBP and DBP contained a random intercept and linear time slope. Random time slopes could not be estimated for the blood lipids data, owing to the fewer number of measurements per subject; instead, we assumed a power correlation structure for the residual errors, which allowed within-subject correlations to depend on distance in time: TYPE=SP (POW) in REPEATED statement of PROC MIXED (SAS Institute, Cary, NC).
In separate mixed models, we examined the effects of a baseline presence of hypertension or hyperlipidemia, along with adherence to diet protocols on the longitudinal trends. We used the Kenward-Rogers method19 to calculate degrees of freedom for all hypothesis tests and included all measurements obtained by week 56 of the study in the analysis to allow for flexibility in the timing of the final follow-up and study close-out. We performed all analyses using SAS version 9.2 (SAS Institute, Cary, NC).
Results
The LEAF study participants were 75% white (n=54) and had an average age of 41.4 years and an average BMI of 30.3 kg/m2 (Table 1). At baseline, only 11% of the women (n=8) were hypertensive (blood pressure ≥140/90 mm Hg, Table 1), and 10% had high cholesterol (TC ≥200 mg/dL, Table 1). Despite low adherence to diet in each group (data not shown: 22% for low-fat diet, 29% for low-carbohydrate diet, p=0.47), more than half of the participants were adherent to the prescribed physical-activity level (66% among women assigned to the low-fat diet and 61% among women assigned to the low-carbohydrate diet, for an average adherence rate of 63%).
Table 1.
Baseline Characteristics (Mean [Standard Deviation]) of Lifestyle Eating and Fitness Study Participants (n=79)
| Overall | Low-fat diet (n=41) | Low-carbohydrate diet (n=38) | |
|---|---|---|---|
| Age, years | 41.4 (5.3) | 40.9 (5.1) | 41.9 (5.4) |
| Nonwhite race (n, %) | 25 (32) | 12 (29) | 13 (34) |
| BMI, kg/m2 | 30.3 (2.8) | 30.5 (2.9) | 30.1 (2.6) |
| SBPa, mm Hg | 121.8 (13.0) | 122.4 (14.7) | 121.3 (11.0) |
| DBPa, mm Hg | 74.5 (8.9) | 75.1 (9.0) | 74.0 (8.7) |
| Hypertensiona (n, %) | 8 (11) | 6 (15) | 2 (6) |
| LDL, mg/dL | 123.1 (30.8) | 126.6 (32.3) | 119.4 (29.1) |
| HDL, mg/dL | 53.0 (13.8) | 51.2 (11.3) | 54.9 (15.9) |
| TC, mg/dL | 194.2 (34.7) | 197.5 (35.8) | 190.5 (33.7) |
| Hypercholesterolemiab (n, %) | 10 (13) | 6 (15) | 4 (11) |
n=40 for low-fat diet; n=36 for low-carbohydrate diet.
n=40 for low-fat diet (invalid triglycerides level).
BMI, body mass index; DBP, diastolic blood pressure; HDL, high-density lipoproteins; LDL, low-density lipoproteins; SBP, systolic blood pressure; TC, total cholesterol.
Trends in each outcome (SBP, DBP, TC, LDL, and HDL) did not differ by treatment group (p-value for each outcome >0.30, Table 2). Across study arms, there was a significant linear decrease in SBP of 3 mm Hg (p=0.01) over time, but DBP (p=0.67) did not change significantly over the course of the study (0.3 mm Hg, Table 2). In contrast, there were quadratic trends in TC, HDL, and LDL during the study (ptime2<0.01 for each model, Table 2).
Table 2.
Mixed-Model Means of Outcome Measures
| Baseline | Week 34 | Week 52 | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Diet | Mean | SE | Mean | SE | Mean | SE |
| SBP (mm Hg) | Low fat | 124.7 | 1.8 | 122.0 | 1.6 | 120.5 | 1.7 |
| Low carbohydrate | 120.8 | 1.9 | 119.5 | 1.7 | 118.8 | 1.8 | |
| Overalla | 122.7 | 1.3 | 120.7 | 1.2 | 119.6 | 1.3 | |
| DBP (mm Hg) | Low fat | 74.8 | 1.2 | 74.1 | 1.2 | 73.7 | 1.3 |
| Low carbohydrate | 72.7 | 1.3 | 73.0 | 1.3 | 73.2 | 1.4 | |
| Overall | 73.8 | 0.9 | 73.6 | 0.9 | 73.5 | 1.0 | |
| TC (mg/dL) | Low fat | 197.5 | 5.2 | 180.4 | 5.7 | 191.0 | 8.0 |
| Low carbohydrate | 190.5 | 5.4 | 172.7 | 6.0 | 188.5 | 7.8 | |
| Overalla | 194.0 | 3.8 | 176.6 | 4.1 | 189.8 | 5.6 | |
| HDL (mg/dL) | Low fat | 51.2 | 2.1 | 47.7 | 2.2 | 49.1 | 3.0 |
| Low carbohydrate | 54.9 | 2.2 | 48.5 | 2.3 | 51.5 | 3.0 | |
| Overalla | 53.0 | 1.5 | 48.1 | 1.6 | 50.7 | 2.1 | |
| LDL (mg/dL) | Low fat | 126.5 | 4.7 | 118.0 | 5.1 | 126.9 | 7.3 |
| Low carbohydrate | 119.4 | 4.9 | 110.9 | 5.3 | 123.2 | 7.1 | |
| Overalla | 123.0 | 3.4 | 114.5 | 3.7 | 125.1 | 5.1 | |
Overall estimates of means are averages across the two diets. Estimates for TC and LDL assume a quadratic trend in time. All other estimates assume a linear trend in time.
Changed significantly during the study period (p≤0.01).
SE, standard error.
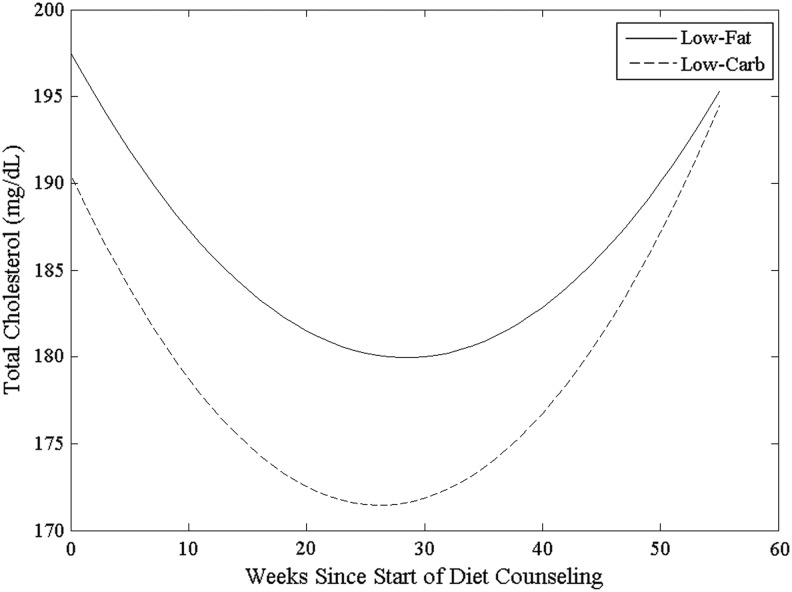
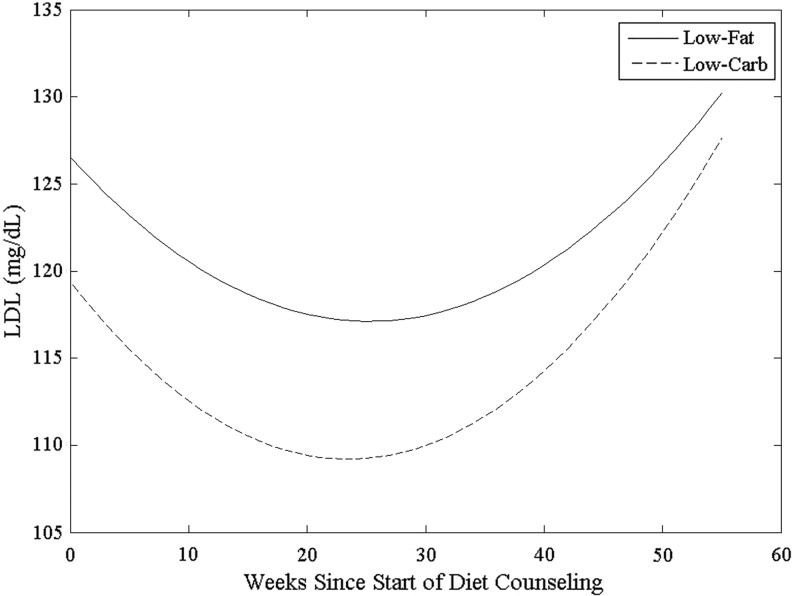
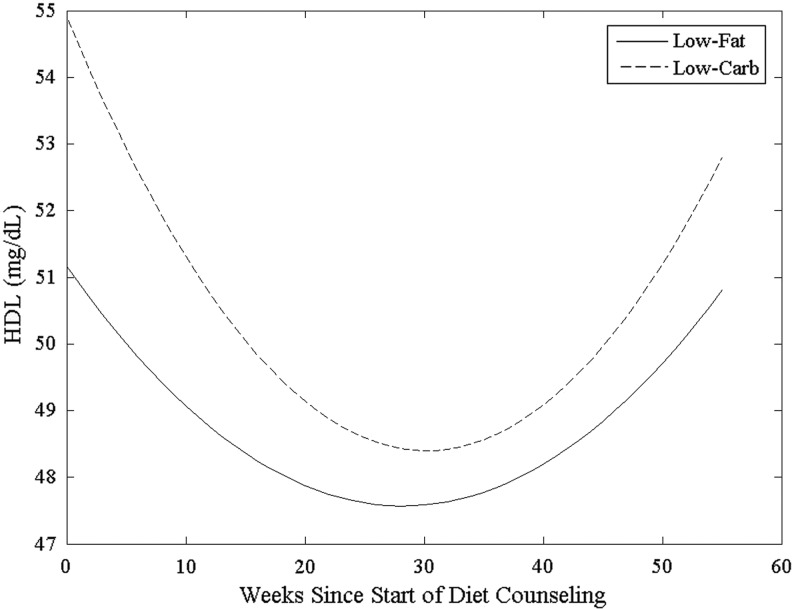
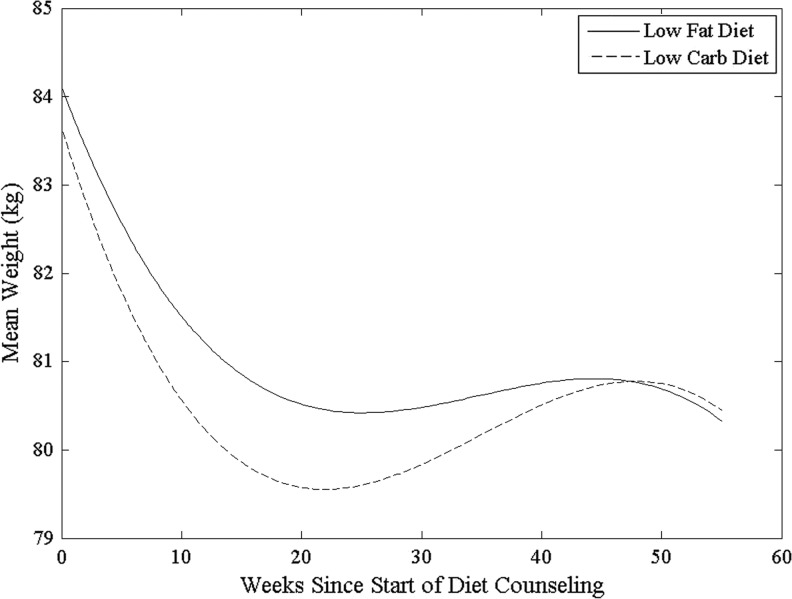
Figure 1 shows that TC initially decreased but rebounded at approximately 30 weeks. A similar trend was observed for LDL (Fig. 2) and HDL (Fig. 3). Figure 4 shows the change in body weight over the same time period and demonstrates a common inflection point with Figures 1–3 around 30 weeks. We did not observe a statistically significant change in TC (p=0.45), HDL (p=0.25), or LDL (p=0.68) from baseline to study close.
FIG. 1.
Trend over time in mean total cholesterol (mg/dL) by study arm.
FIG. 2.
Trend over time in mean low-density lipoproteins (LDL) (mg/dL) by study arm.
FIG. 3.
Trend over time in mean high-density lipoproteins (HDL) (mg/dL) by study arm.
FIG. 4.
Trend over time in mean body weight (kg) by study arm.
Owing to the similarity in trends across treatment groups, we pooled the data across groups in examining the effects of adherence to diet or physical activity, baseline hypertension, and baseline hypercholesterolemia. Trends in each outcome did not differ significantly by dietary or physical-activity adherence (p-values>0.25). Given the low adherence to the respective diets, we likely did not have sufficient power to detect a difference. However, we likely did have enough power to detect a difference by physical-activity adherence. Hypertension at baseline did not affect the trend in DBP (p=0.17) but did affect SBP trends (p<0.01); hypertensive women (11%) experienced a decline in SBP (slope=−0.35 mm Hg/week, p<0.01), but normotensive women did not (slope=−0.03 mm Hg/week, p=0.20). Hypercholesterolemia (n=10) at baseline did not significantly affect changes in blood lipid values across time (p>0.4 for TC, LDL, and HDL).
Discussion
We aimed to assess longitudinal changes in blood pressure and blood lipids in a population of premenopausal women. In this secondary analysis, we hypothesized that results might differ by level of adherence to the respective diet protocol and baseline presence of hypertension or hyperlipidemia. At the time of this study, no data existed on the effect of type of diet on breast cancer prevention among premenopausal women. In this 52-week randomized intervention trial of low-fat and low-carbohydrate weight-loss diets, a reduction in SBP was seen in both study arms. This finding is consistent with another 1-year RCT, which reported no differences between diet groups in blood pressure or cholesterol.10 In our study, levels of blood lipids decreased during the first half of the trial and mirrored both the reduction and subsequent rebound in body weight in the second half of the trial. A similar yet shorter-term (6-month) RCT demonstrated an improvement in blood pressure and cholesterol levels from baseline to follow-up regardless of dietary arm.9 However, a longer-term (2-year) trial provided evidence of the weight-rebound effect at 1 year, and there were no statistically significant differences between groups in blood pressure or cholesterol at any time point.12
We hypothesized that favorable changes would be seen in blood lipids and blood cholesterol values over the 52-week dietary intervention trial. Over time, we observed a decrease in SBP but not DBP in both arms of the trial. A lack of effect by diet type is supported by meta-analyses comprising 28 trials comparing the effect of low-fat and low-carbohydrate dietary interventions, with no differences in blood pressure levels seen over a follow-up of at least 6 months.13,14
Meanwhile, being hypertensive at baseline led to a larger decline in SBP. This finding is consistent with the DASH trial, in which larger decreases in both SBP and DBP were seen among persons who were hypertensive at baseline (11 mm Hg and 6 mm Hg, respectively) compared to those with normal blood pressure at baseline (6 mm Hg and 3 mm Hg, respectively).20 The small improvements in SBP that we observed in the LEAF population are consistent with those observed in the DASH trial.20 Since these women were close to normotensive at baseline, it is important to note that large changes in SBP may have had the adverse clinical effect of making them hypotensive.
Favorable changes in TC were not observed in either study arm when comparing baseline to study close-out. TC initially decreased but then returned to near-baseline levels by the end of the trial. This pattern was consistent with weight loss in this study. However, our findings are not supported by extant literature, which indicates that favorable changes in TC are more often seen among participants assigned to low-fat diets compared to low-carbohydrate diets.21
A decrease in HDL was observed among participants in both arms of the trial, which is a finding consistent with another study of weight-loss diets,21 and may not be surprising given the modest level of adherence (63%) to physical activity in our study. We hypothesized that HDL would remain the same or increase, particularly with physical-activity advice; however, some evidence suggests that exercise typically induces a modest elevation of HDL among women, and the intensity of exercise is an important factor, which was not measured in this study.22,23 Importantly, we were not able to separate the effects of the diet versus that of increased physical activity. During the study-design process, LEAF investigators acknowledged that both weight loss and maintenance of weight loss require physical activity in addition to changes in diet. Thus, both dietary interventions comprised a physical-activity component.
This study assessed the effect of long-term dietary interventions on changes in blood pressure and blood lipids. Strengths of this study included repeat measurements of TC, LDL, HDL, SBP, and DBP at five in-person clinic visits, and monthly 7-day diet records from which to assess adherence. Although the characteristics of our study population indicated that the study participants were, on average, in good cardiovascular health, our study included women who were hypertensive, hyperlipidemic, and diabetic at baseline. As a result, our findings may be more generalizable to overweight and obese premenopausal women, as these medical conditions are common exclusion criteria for other RCTs comparing low-fat to low-carbohydrate diets.11,12 However, as a result of our small sample size, we were unable to consider all factors (study arm, dietary adherence, physical-activity adherence, and presence of hypertension or hyperlipidemia at baseline) simultaneously in order to assess changes over time in blood pressure and blood lipids in this study population. Key limitations of studies of behavior change are the low percentage of screened participants who ultimately enroll in the study, along with low adherence rates. These factors influence the study's real-world applications to lifestyle coaching and generalizability to clinical outcomes. We do not believe that these considerations are unique to this population of overweight and obese premenopausal women.
It should be noted that the LEAF study was powered to detect differences between diet arms in terms of weight loss, the primary outcome of the study. Although we may not have had enough subjects to address the effects of between-subject variability on power, we did have rich longitudinal data on each subject, which minimized the effects of within-subject variability on power.
A limitation of defining diet adherence solely via attainment of a participant's caloric goal is that it does not take into account whether the participant was adherent to the low-fat or the low-carbohydrate composition of the diet. An additional limitation of these data is that 34% of the women enrolled in the low-fat dietary arm and 50% of the women enrolled in the low-carbohydrate dietary arm did not complete the last study visit. Although this rate of attrition affected the precision of our study estimates, losses to follow-up in long-term dietary trials are common. This speaks to the need for further investigation into diet approaches that are easier to implement and adhere to. It should be noted that there was no difference in the proportion of women who completed the last study visit according to study arm. In a recent meta-analysis of low-fat and low-carbohydrate dietary interventions lasting 6 months or longer, half of the eligible trials had attrition rates of more than 30%.13
Conclusions
Our results support that dietary interventions are efficacious for lowering blood pressure and blood lipids. Specifically, favorable changes in SBP were seen across study arms, although decreases in TC and LDL were limited to the first half of follow-up. We recommend that future investigations pay careful attention to issues of adherence in terms of caloric goal, macronutrients, and dietary pattern, as it will be critical to distinguish whether adherence to caloric restriction for the improvement of CVD risk factors is more important than type of diet consumed.
Supplementary Material
Acknowledgments
The study—Clinical Trial Registration Number: NCT01559194—was supported by grants from the Breast Cancer Research Foundation and the National Center for Advancing Translational Sciences (8UL1TR000090-05). The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the Breast Cancer Research Foundation, the National Center for Advancing Translational Sciences, or the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Marmot M, Elliott P, eds. Coronary heart disease epidemiology: From aetiology to public health, 2nd ed. Oxford, UK: Oxford University Press, 2005 [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: A report from the American Heart Assoiation. Circulation 2011;123:e18–e209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Labarthe D. Epidemiology and prevention of cardiovascular diseases: A global challenge, 2nd ed. Sudbury, MA: Jones and Bartlett Publishers, 2011 [Google Scholar]
- 4.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82–96 [DOI] [PubMed] [Google Scholar]
- 5.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–1124 [DOI] [PubMed] [Google Scholar]
- 6.Obarzanek E, Proschan MA, Vollmer WM, et al. Individual blood pressure responses to changes in salt intake. Hypertension 2003;42:459–467 [DOI] [PubMed] [Google Scholar]
- 7.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension. Hypertension 2006;47:296–308 [DOI] [PubMed] [Google Scholar]
- 8.Kokkinos P. Physical activity and cardiovascular disease prevention: Current recommendations. Angiology 2008;59(2 suppl):26S–29S [DOI] [PubMed] [Google Scholar]
- 9.Brehm BJ, Seeley RJ, Daniels SR, D'Alessio DA. A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. J Clin Endocrinol Metab 2003;88:1617–1623 [DOI] [PubMed] [Google Scholar]
- 10.Lim SS, Noakes M, Keogh JB, Clifton PM. Long-term effects of a low carbohydrate, low fat or high unsaturated fat diet compared to a no-intervention control. Nutr Metab Cardiovasc Dis 2010;20:599–607 [DOI] [PubMed] [Google Scholar]
- 11.Gardner CD, Kiazand A, Alhassan S, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: The A to Z Weight Loss Study: A randomized trial. JAMA 2007;297:969–977 [DOI] [PubMed] [Google Scholar]
- 12.Foster GD, Wyatt HR, Hill JO, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: A randomized trial. Ann Intern Med 2010;153:147–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu T, Mills KT, Yao L, et al. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: A meta-analysis of randomized controlled clinical trials. Am J Epidemiol 2012;176Suppl 7:S44–S54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nordmann AJ, Nordmann A, Briel M, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: A meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:285–293 [DOI] [PubMed] [Google Scholar]
- 15.McCarron DA, Oparil S, Chait A, et al. Nutritional management of cardiovascular risk factors: A randomized clinical trial. Arch Intern Med 1997;157:169–177 [PubMed] [Google Scholar]
- 16.Benezra LM, Nieman DC, Nieman CM, et al. Intakes of most nutrients remain at acceptable levels during a weight management program using the food exchange system. J Am Diet Assoc 2001;101:554–561 [DOI] [PubMed] [Google Scholar]
- 17.Franz M, Barr P, Holler H, Powers M, Wheeler M, Wylie-Rosett J. Exchange lists: Revised 1986. J Am Diet Assoc 1987;87:28–34 [PubMed] [Google Scholar]
- 18.Fitzmaurice G, Laird N, Ware J. Applied longitudinal analysis, 2nd ed. Hoboken, NJ: John Wiley & Sons, 2011 [Google Scholar]
- 19.Kenward M, Roger J. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 1997;53:983–997 [PubMed] [Google Scholar]
- 20.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: Subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med 1999;159:285–293 [DOI] [PubMed] [Google Scholar]
- 21.Malik VS, Hu FB. Popular weight-loss diets: From evidence to practice. Nat Clin Pract Cardiovasc Med 2007;4:34–41 [DOI] [PubMed] [Google Scholar]
- 22.Eapen D, Kalra G, Rifai L, Eapen C, Merchant N, Khan B. Raising HDL cholesterol in women. Int J Womens Health 2009;1:181–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haskell W. Exercise-induced changes in plasma lipids and lipoproteins. Prev Med 1984;13:23–36 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.