Abstract
Objectives: To assess the clinical evidence of auriculotherapy for constipation treatment and to identify the efficacy of groups using Semen vaccariae or magnetic pellets as taped objects in managing constipation.
Methods: Databases were searched, including five English-language databases (the Cochrane Library, PubMed, Embase, CINAHL, and AMED) and four Chinese medical databases. Only randomized controlled trials were included in the review process. Critical appraisal was conducted using the Cochrane risk of bias tool.
Results: Seventeen randomized, controlled trials (RCTs) met the inclusion criteria, of which 2 had low risk of bias. The primary outcome measures were the improvement rate and total effective rate. A meta-analysis of 15 RCTs showed a moderate, significant effect of auriculotherapy in managing constipation compared with controls (relative risk [RR], 2.06; 95% confidence interval [CI], 1.52– 2.79; p<0.00001). The 15 RCTs also showed a moderate, significant effect of auriculotherapy in relieving constipation (RR, 1.28; 95% CI, 1.13–1.44; p<0.0001). For other symptoms associated with constipation, such as abdominal distension or anorexia, results of the meta-analyses showed no statistical significance. Subgroup analysis revealed that use of S. vaccariae and use of magnetic pellets were both statistically favored over the control in relieving constipation.
Conclusions: Current evidence illustrated that auriculotherapy, a relatively safe strategy, is probably beneficial in managing constipation. However, most of the eligible RCTs had a high risk of bias, and all were conducted in China. No definitive conclusion can be made because of cultural and geographic differences. Further rigorous RCTs from around the world are warranted to confirm the effect and safety of auriculotherapy for constipation.
Introduction
Chronic constipation in adults is now a common health care issue. This disorder of gastrointestinal motility is characterized by sustained and difficult defecation, infrequent bowel movements, or incomplete evacuation,1 which can be attributed to such factors as a change in diet or daily routine, medication, and acute emotional stress. The prevalence of the condition ranges from 0.7% to 79% on a global scale, with an average rate of 16%.2 On the mainland of China, about 6% of population experience constipation, of which women and the elderly are the largest group.3Although non–life-threatening, long-term constipation can cause serious complications, such as diverticulosis of the colon, crissum diseases, and melanosis coli.4 As Rogers concluded, chronic constipation not only can bring about discomfort but also affects a person's physical and psychological well-being, with further consequences of reduced quality of life and high costs for both families and society.5
For these reasons, it is of vital importance to manage chronic constipation with effective, safe, and inexpensive approaches. Auriculotherapy (AT), which has been widely used to treat diseases for thousands of years in China, may play some role.6 As defined by Oleson, AT refers to “a healthcare modality by stimulating the external surface of the auricle to alleviate pathological conditions in other parts of the body.”7 Ear points stimulation used to be considered an adjuvant treatment combined with body acupuncture, moxibustion, or other traditional Chinese practices but has been gradually developed into a treatment system of its own.8 Performing a treatment upon the external surface of ear with reliable quantity of stimulus and duration can relieve symptoms of distant pathology through the reticular formation and the regulation of the sympathetic or parasympathetic nervous systems.9 Forms of AT are multitudinous. Ear points can be stimulated with different materials, such as Semen vaccariae,10 magnetic pellets,11 or small acupuncture needles,12 by direct contact with the skin, as with subcutaneous electrical stimulation.13 It's worth noting that, without any invasive procedure, auricular pressing therapy seems to be accepted by patients more easily.
Recently, AT has been used for both preventing and managing constipation. Several clinical trials have been conducted,14–16 but findings have been conflicting. Only one published systematic review has addressed clinical trials on auricular pressing therapy as the primary modality in managing constipation.17 However, this review included only nonrandomized clinical trials and reached no conclusion about effectiveness because of the substantial methodologic flaws. Reviews of randomized, controlled trials (RCTs), which are considered the gold standard in the hierarchy of scientific evidence, are highly valued and are used to support practice, guideline, and policy recommendations.17 Several RCTs with good study design and methods have recently been published; they suggest that AT alone can have encouraging results in managing constipation and offer the potential for meta-analysis of RCTs.
The objective here was to quantitatively and precisely assess the effects of AT for the management of constipation in adults as reported in RCTs by using systematic review and, if possible, meta-analysis.
Methods
Selection strategy
The literature was searched using the following databases from their inception through April 22, 2013: the Cochrane Library, PubMed, Embase, CINAHL, AMED, and four Chinese Medical Databases (CBMdisc, CNKI, VIP Information, and WanFang Data). These databases were searched by using the following Medical Subject Heading terms and text words: (“constipation” OR “astriction” OR “colonic inertia” OR “dyschezia”) AND (“auriculotherapy” OR “auricular point sticking” OR “auriculotherapies” OR “auricular point therapy” OR “auricular plaster therapy” OR “ear acupressure” OR “ear point” OR “auricular pressing therapy”). Finally, a snowball search was done, in which reference lists of selected articles were screened and checked for additional relevant clinical studies. Non–English-language publications satisfying the inclusion criteria were translated into English and then appraised.
Selection of studies
Only RCTs were selected as eligible studies. Further, these studies had to satisfy the following inclusion criteria:
Population: Studies that examined adults (≥18 years old) with constipation, which was defined explicitly according to the Rome II/III criteria18 or other consensus criteria, were all considered for review. Studies that recruited patients with any underlying abnormality (i.e., adult Hirschsprung disease or thyroid abnormalities) were ineligible.
Intervention: Clinical studies on the use of auricular pressing therapy (i.e., using S. vaccariae or magnetic pellets as the taped objects) in managing constipation were included. Studies that used AT as the primary modality in managing constipation were also considered for inclusion. In particular, AT in managing constipation studies, which involve invasive procedure, such as auricular acupuncture and erjian bloodletting method, were not included.
Comparison: Studies had to compare AT with no treatment, placebo, conventional medicine, or other Traditional Chinese Medicine modalities.
Outcome: Studies must have used dichotomous data on total effective rate or continuous data on frequency of defecation or symptom scores as primary outcomes.
Study outline
First, databases were searched for relevant articles. After identifying and deleting the duplicates, one reviewer read titles/abstracts of the remaining studies for potential relevance and a second reviewer retrieved a random sampling independently. Then, these two reviewers separately assessed the eligibility of all trials that met the inclusion criteria by reading the full texts of related studies. Finally, a snowball technique was used to find more eligible papers. During the processes above, disagreement among two reviewers was discussed and agreement was reached by consensus.
Quality critical appraisal
Two reviewers independently conducted a critical appraisal by using the Cochrane risk of bias tool for RCTs, which was recommended by the Cochrane Handbook for Systematic Reviews of Interventions.19 The Cochrane risk of bias tool is a six-item list designed to assess sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other potential sources of bias. Each item was rated as “met,” “unmet,” or “unclear.” Auricular point sticking may not be double-blinded, so we considered single-blinding of outcome assessors as “met” for blinding.
According to the Cochrane handbook, quality of clinical trials can be divided into three levels. If the study design fully met the preceding six criteria, it is considered A level, signifying the low risk of bias. B level, representing moderate risk of bias, would be assigned when one or more criteria were partly met. If one or more criteria were not met, the study would be defined as C level, implying high risk of bias. Given that the high risk of bias would substantially reduce the credibility of the results, studies rated as C level would be eliminated.
Any disagreements were resolved by consensus; when study contents were not sufficient to determine the risk of bias, study authors were contacted for further information.
Data extraction
Two reviewers independently extracted and recorded data on a standardized data form. Information about participant characteristics, intervention protocol, and therapeutic outcomes (including effective rate, adverse events, and withdrawals) were recorded. Extracted participant characteristics included age, sex, specific medical conditions, and diagnostic criteria for constipation. Data on intervention protocol included selected acupoints, detailed instructions for manual pressing, daily activity, duration of therapy, follow-up, and comparison group. Study authors were contacted to supply missing data. Any disagreements between two independent reviewers were resolved by consensus.
Quantitative synthesis of data
Meta-analysis was performed by using software RevMan 5 (http://www.cc-ims.net/revman/download). Statistical heterogeneity among studies was measured by using the chi-square and I2 tests. If I2<50% and p>0.1, a fixed-effect model was used. Additionally, a random-effects model was applied if the trials had sufficient clinical homogeneity. Otherwise, they would be synthesized with descriptive statistics rather than quantitative assessment. For continuous data, mean differences and 95% confidence intervals (95% CIs) were calculated. For dichotomous data, relative risks (RRs) and corresponding 95% CIs were calculated. Whether S. vaccariae has a therapeutic effect is controversial,6,20 so subgroup analysis should be used for further study.
Results
Search process
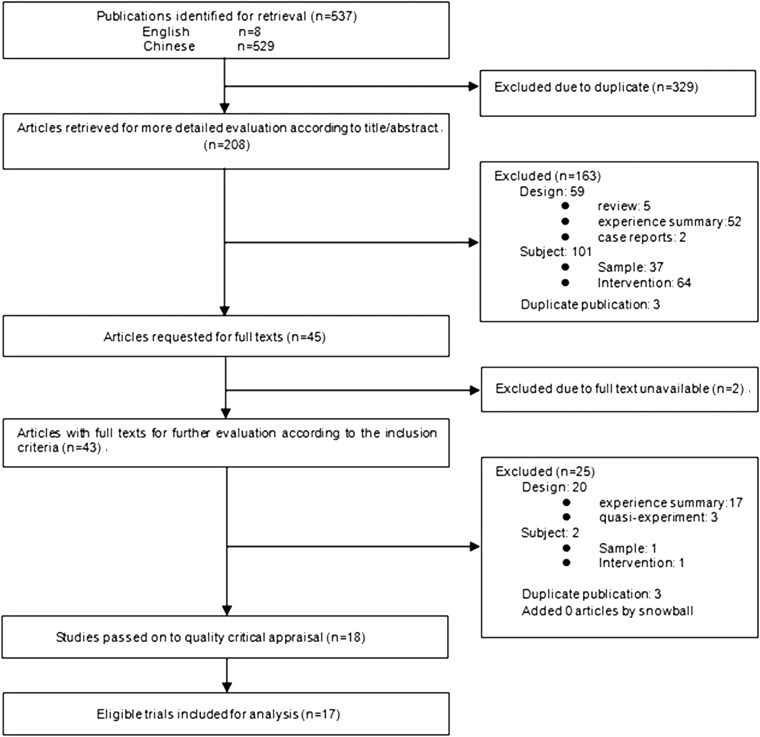
The database identified 537 potentially relevant records. After duplicates were removed, 208 records were retrieved for evaluation according to title/abstract. Of these, 45 records were identified for more detailed evaluation after acquisition of the full text. With 2 studies unavailable, 43 records with full texts were subsequently used for further evaluation according to the criteria set in advance. Twenty-five records were excluded for various reasons illustrated in Figure 1. Moreover, no articles were found by snowball search. Finally, 18 studies were screened for critical appraisal of quality.
FIG. 1.
Study flow diagram.
Critical appraisal of quality
Judgments on each methodologic quality item for all included studies are described in Table 1. Of 18 studies, 2 studies were quality level A; 15, quality level B; 1, quality level C. According to the Cochrane risk of bias tool, studies labeled as level C should be excluded. As a result, 17 studies were included for analysis (the level C article21 was excluded).
Table 1.
Methodologic Quality of All Included Studies
| Study, year | Random allocation | Allocation concealment | Blinding | Incomplete outcome | Selective reporting | Other bias | Quality level |
|---|---|---|---|---|---|---|---|
| Cai et al., 2011 | ? | − | − | − | + | + | B |
| Chen et al., 2012 | ? | − | − | + | + | + | B |
| Chen et al., 2011 | ? | − | − | + | + | + | B |
| He and Pei, 2012 | ? | − | − | + | − | + | B |
| Hong and Shen., 2013 | ? | − | − | + | + | + | B |
| Ji et al., 2010 | ? | − | + | + | + | + | B |
| Li et al., 2012 | + | + | + | + | + | + | A |
| Liu et al., 2011 | ? | − | − | + | − | − | C |
| Liu et al., 2009 | ? | − | − | + | + | + | B |
| Meng et al., 2011 | + | − | − | + | + | + | B |
| Qian et al., 2012 | ? | − | − | + | + | + | B |
| Wang et al., 2011 | ? | − | − | + | + | + | B |
| Yin and Qin., 2012 | ? | − | − | + | + | + | B |
| Zeng et al., 2012 | + | − | − | + | − | + | B |
| Zhang et al., 2009 | ? | − | − | + | + | + | B |
| Zhang and Yang, 2009 | + | − | − | + | + | + | B |
| Zhong and Zhang, 2007 | + | − | − | + | + | + | B |
| Zhou et al., 2012 | + | + | − | + | + | + | A |
+, criteria met; ?, criteria not met/unclear whether criteria were met.
Characteristics of eligible RCTs included for analysis
Table 2 lists the characteristics of the 17 included studies. All RCTs were from mainland China or Hong Kong. Sixteen22–37 were reported in Chinese, and 1 was published in English.38 Fourteen RCTs focused on specific groups: chronic renal disease,35 subarachnoid hemorrhage,30 diabetes mellitus,31 coronary heart disease,25 threatened abortion,33 cancer,26 stroke,32 female college students,29 and elderly people.24,27,28,34,37,38 In addition, 3 studies involved participants with specific syndromes.24,32,36
Table 2.
Data Extraction of Randomized, Controlled Trials on Auriculotherapy for Constipation
| Study, year, location | Participants | Diagnostic criteria for constipation/syndrome differentiation | Control intervention |
|---|---|---|---|
| Cai et al., 2011, China/Shanghai | Community groups with predisposition toward constipation (n=250); E: n=119, MA: 59.95±16.38 y; C: n=131, MA: 61.51±12.10 y | Rome III diagnostic criteria/NM | Laxatives or glycerol enema if necessary |
| Chen et al., 2012, China/Fujian | Inpatients in geriatrics department (n=68 patients with constipation of qi deficiency); E: n=35 (20 M, 15 F), MA: 79.6±6.5 y; C: n=33 (14 M, 19 F), MA: 79.2±5.8 y | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/deficiency of qi | Routine care, laxatives or glycerol enema if necessary |
| Chen et al., 2011, China/Shanghai | Outpatients in community health center (n=122); E: n=60 (17 M, 43 F), MA: 63±10 y; C: n=62 (24 M, 38 F), MA: 61±14 y | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/deficiency syndrome, excess syndrome | Blank control |
| He and Pei, 2012, China/Zhejiang | Patients with coronary heart disease (n=88); E: n=46 (26 M, 20 F), MA: ? y (range, 51–83 y); C: n=42 (25 M, 17 F), MA: ? y (range, 51–86 y) | Rome II diagnostic criteria/deficiency syndrome, excess syndrome | Rhubarb soda tablets orally, 2 pills/time 3 times daily, glycerol enema if necessary |
| Hong and Shen, 2013, China/Zhejiang | Inpatients in oncology department (n=60 patients) (32 M, 28 F), MA: 61 y (range, 43–78); E: n=30; C: n=30 | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/NM | Phenolphthalein orally, 100 mg/piece, 3 pieces/time, 3 times daily |
| Ji et al., 2010, China/Shanghai | Inpatients with senile functional constipation (n=73); E: n=37 (19 M, 18 F), MA: 72.30±1.07 y (range, 60–87 y); C: n=36 (18 M, 18 F), MA: 69.81±1.04 y (range, 61–85 y) | Rome II diagnostic criteria/deficiency syndrome, excess syndrome | Conventional instructions, glycerol enema if necessary |
| Li et al., 2012, China/HongKong | Residents in elderly residential care home (n=39) E: 21 (5 M, 16 F), MA: 81±7.43 y (65–96) C: 18 (5 M, 13 F), MA: 81.4±7.17 y (68–91) | Rome III diagnostic criteria/excess syndrome, deficiency syndrome | AT with Semen vaccariae applied to each of the 7 selected auricular acupoints |
| Liu et al., 2009, China/Henan | Patients with senile habitual constipation (n=88) E: n=44 (16 M, 28 F), MA: 71±10.6 y C: n=44 (18 M, 26 F), MA: 70±10.5 y | <3 bowel movements per week, failed >3 mo/NM | Conventional instructions |
| Meng et al., 2011, China/Jiangxi | Female college students (n=26 patients); E: n=12, MA: 21.4±3.6 y; C: n=14 MA: 20.3±3.3 y | Rome III diagnostic criteria/NM | Guodao Pian (phenolphthalein) orally, 100 mg/time, once before sleep |
| Qian, 2012, China/Zhejiang | Inpatients in department of neurology (n=84 patients); E: n=42 (35 M, 7 F), MA: 37.1 y (range, 29–51 y); C: n=42 (36 M, 6 F), MA: 31.1 y (range, 26–47 y) | Rome III diagnostic criteria/NM | Conventional instructions |
| Wang et al., 2011 China/Heilongjiang | Inpatients in department of endocrinology (n=95 patients; 51 M, 44 F), MA: 56.66±8.84 y (range, 39–75); E: n=48; C: n=47 | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/NM | Conventional instructions |
| Yin and Qin, 2012, China/Anhui | Patients with stroke (n=120); E: n=60 (38 M, 22 F); C: n=60 (41 M, 19 F) | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/NM | Conventional instructions |
| Zeng et al., 2012, China/Hunan | Patients with threatened abortion (n=60); E: n=30, MA: 31.5±3.6 y (range, 26–41 y); C: n=30, MA: 31.8±4.1 y (range, 24–42 y) | No bowel movement for 18 h beyond normal bowel movement time AND bowel movement with straining and hard stool/NM | Abdominal massage, 5 min/session, 3–4 times/d, massage whenever abdominal distension occurs, 30 min/session |
| Zhang et al., 2009, China/Shanghai | Inpatients with chronic renal disease (n=120) (excess: 60, deficient: 60); E: n=60 (excess: 30, deficient: 30); C: n=60 (excess: 30, deficient: 30) | No bowel movement for 2 d OR bowel movement with straining and hard stool/deficiency syndrome, excess syndrome | Laxatives or glycerol enema if necessary |
| Zhang and Yang, 2009, China/Shandong | Outpatients in hospital and volunteers in community (n=60); E: n=30 (15 M, 15 F), MA: 69.77 y (range, 61–78 y); C: n=30 (14 M, 16 F), MA: 68.20 y (range, 63–75 y) | Rome II diagnostic criteria/deficiency syndrome, excess syndrome | Phenolphthalein orally, 2 pieces/time 3 times daily |
| Zhong and Zhang, 2007, China/Beijing | Outpatients in anorectal department (n=60); E: n=30 (12 M, 18 F), MA: 45.13±15.51 y (range, 19–65 y); C: n=30 (10 M, 20 F), MA: 45.90±16.03 y (range, 19–65 y) | Rome II diagnostic criteria/qi deficiency of lung and spleen | Tegaserod orally, 6 mg/time twice daily |
| Zhou et al., 2012, China/Guangxi | Outpatients or inpatients with senile habitual constipation in gastrointestinal department (n=200); E: n=100 (45 M, 55 F), MA: 69±12 y (range, 56–82 y); C: n=100 (42 M, 58 F), MA: 70±11 y (range, 57–87 y) | Standardized diagnostic criteria for constipation developed by Chinese Medical Society/excessive heat in the stomach and intestine, blockage of lung qi, deficiency of spleen and kidney | Routine AT without syndrome differentiation, with the same treatment course as E |
E, experimental group; C, control group; M, male; F, female; MA, mean age; AT, auriculotherapy; NM, not mentioned.
All eligible RCTs, with sample sizes ranging from 26 to 274, allocated a total of 1637 adult patients with chronic constipation. Of these RCTs, 6 compared AT with usual care and health education;24,27,28,30–32 6 studies compared AT with conventional medicine;22,26,29,34–36 and the other 5 compared AT with abdominal massage,33 Traditional Chinese Medicine modalities,25,37,38 and blank control.23
Content and implementation of AT
Selection and number of ear points in AT
As shown in Table 3, ear points were divided into two types: the main part and the adjunct. Main ear points were selected in quantities ranging from 2 to 8; the adjunct was chosen according to syndrome differentiation. Of 17 RCTs, 8 were based on differentiation of syndrome.23–25,27,34,35,37,38 The number of adjunct ear points selected ranged from 1 to 3 according to the corresponding type of syndrome. Among the 8 RCTs based on syndrome differentiation, 6 adopted deficiency and excess syndrome differentiation as the theoretical basis.23,25,27,34,25,38 The other 2 added syndrome differentiation of qi and blood or of zang-fu viscera based on deficiency and excess syndrome differentiation. Six RCTs claimed that adjunct ear points were selected according to differentiation of syndrome22,30–33,36 but did not further describe patterns of syndrome. One RCT reported specific type of syndrome38 but had no adjunct ear points to be chosen. In particular, 1 study adopted AT in both the experimental and control group; however, the experimental group was given treatment based on syndrome differentiation and the control group was not.37 In all eligible studies but 1,26 both ears were be used alternately.
Table 3.
Implementation of Randomized Controlled Trials on Auriculotherapy for Constipation
| Study, year | Taped objects | No. of selected ear points | Acupoint detection | Manual pressing | Using ears alternately | Health care | Duration/follow-up |
|---|---|---|---|---|---|---|---|
| Cai et al., 2011 | Magnetic pellet | M (6): large intestine, small intestine, rectum, Shenmen, lung; stomach A (4): spleen, kidney, endocrine, San Jiao | Probe | 3 times/d for 3 min/time per acupoints until de qi | Yes | Yes | 30 d (5 d/session)/30 d |
| Chen et al., 2012 | SV | M (5): large intestine, San Jiao, lung, spleen, stomach | NM | 3 times/d for a total of 1 min/time until de qi | Yes | Yes | 40 d (2 d/session)/NM |
| Chen et al., 2011 | Magnetic pellet | Excess: rectum, large intestine, lung, San Jiao, constipation spot; deficient: rectum, large intestine, lung, San Jiao, constipation spot, spleen, kidney | NM | Excess: strong force, 5–6 times/d for a total of 3–5 min/time; deficient: light force, 3–4 times/d for a total of 1–3 min/time | Yes | NM | 30 d, 60 d (excess: 5 d/session; deficient: 7 d/session)/NM |
| He and Pei, 2012 | SV | M (2): large intestine, rectum; A (4): subcortex, San Jiao, spleen, lung | NM | 3–5 times/d for a total of 1–2 min/time until de qi; excess: strong force; deficient: light force | Yes | NM | 14 sessions (2–3 d/session)/NM |
| Hong and Shen, 2013 | SV | M (5): large intestine, rectum, sympathesis, constipation spot, subcortex | Probe | 2–3 times/d for 2 min/time per acupoints until de qi | NM | NM | 3 d/NM |
| Ji et al., 2010 | Excess: Liu shen pills; deficient: magnetic pellets | M (3): Large intestine, small intestine, rectum; A: excess (3), lung, San Jiao, stomach/deficient (3), spleen, kidney, endocrine | NM | Excess: 3 times/d for 1 min/time per acupoints; deficient: 3 times/d for 3 min/time per acupoints until de qi | Yes | Yes | 30 d (excess: 2 d /session; deficient: 3 d /session)/NM |
| Li et al., 2012 | E: magnetic pellet C: SV | M (7): large intestine, rectum, San Jiao, spleen, lung, sympathesis, subcortex | Acupoint detector | Not exerting manual pressure | Yes | Yes | 21 d (3–4 d/session) for 1 mo |
| Liu et al., 2009 | SV | M (6): large intestine, small intestine, sympathesis, lung, spleen, subcortex | NM | 3–5 times/d for a total of 3–5 min/time until de qi | Yes | Yes | 20 sessions (3–5 d/session)/NM |
| Meng et al., 2011 | SV | M (6): constipation spot, lower portion of rectum, large intestine, spleen, subcortex, San Jiao | NM | 4 times/d for a total of 3–5 min/time with pressing intensity that patients could tolerate | Yes | NM | 4 sessions (2 sessions/week) at 1, 3, and 6 mo |
| Qian, 2012 | SV | M (5): large intestine, San Jiao, spleen, abdomen, subcortex; A (2): lung, sigmoid colon | NM | 2–3 times/d for a total of 3–5 min/time until de qi | Yes | Yes | 14 d (2–3 d/session)/NM |
| Wang et al., 2011 | SV | M (5): large intestine, constipation spot, spleen, rectum, San Jiao; A (2): lung, subcortex | NM | 2–3 times/d for a total of 3–5 min/time until and 2–3 times/acupoint at 15 min before defecation | Yes | Yes | 5 sessions (2–3 d/session)/NM |
| Yin and Qin, 2012 | SV | M (4): large intestine, small intestine, rectum, San Jiao; A (4): endocrine, lung, spleen, kidney | Probe | 3–5 times/d for a total of 1 min/time until de qi | Yes | Yes | 20 sessions (3 d/session)/NM |
| Zeng et al., 2012 | SV | M (3): constipation spot, lower portion of rectum, sympathesis; A (5): San Jiao, lung, small intestine, spleen, stomach | Acupoint detector | 4–5 times/d for a total of 3–5 min/time until de qi | Yes | Yes | 6 d (2 d/session)/NM |
| Zhang et al., 2009 | Excess: Liu shen pills; deficient: magnetic pellets | M (3): large intestine, small intestine, rectum; A: excess (3), lung, San Jiao, stomach/deficient (3), spleen, kidney, endocrine | NM | Excess: 3–5 times/d for 1 min/time per acupoints with strong force; deficient: 3–5 times/d for 3 min/time per acupoints with light force | Yes | NM | 30 d (excess: 2 d/session; deficient: 3 d/session)/NM |
| Zhang and Yang, 2009 | SV | M (5): lower portion of rectum, large intestine, constipation spot, subcortex, lung; A: excess (3), stomach, San Jiao, abdomen; Deficient(2), spleen, kidney | Acupoint detector | ≥4 times/d for a total of 5 min/time until de qi | Yes | NM | 8 wk (3–5 d/session)/NM |
| Zhong and Zhang, 2007 | SV | M (6): lung, spleen, large intestine, rectum, subcortex, constipation spot; A (3): stomach, abdomen, San Jiao | NM | 3–5 times/d for a total of 27 cycle/time per acupoints until de qi | Yes | NM | 20 d (2 d/session)/NM |
| Zhou et al., 2012 | SV | M (8): brain stem, occiput, subcortex, large intestine, San Jiao, abdomen, endocrine, constipation spot; A: excessive heat in the stomach and intestine (2), stomach, small intestine/blockage of lung qi (1), lung/deficiency of spleen and kidney (2), spleen, kidney | NM | 4 times/d for 30 s/time per acupoints | Yes | NM | 16 sessions (3–4 d/session)/NM |
De qi refers to patient's subjective feelings of soreness, numbness, distention, heaviness or hotness. Health care mainly refers to dietary guidance, advice on exercise, established bowel habits, psychological care, and drug administration.
SV, Semen vaccariae; M, main ear points; A, adjunct ear points.
In all studies, 15 main ear points were commonly used for treating constipation: large intestine (94.1%), rectum (76.5%), subcortex (47.1%), San Jiao (47.1%), constipation spot (47.1%), spleen (41.2%), lung (41.2%), small intestine (29.4%), sympathesis (23.5%), stomach and abdomen (11.8%), brain stem, occiput, endocrine, and Shenmen (all 5.9%).
Use of taped objects and acupoint detection tools in AT
Twelve of the eligible studies described using S. vaccariae as the taped objects in AT,24–26,28–34,36,37 and 2 studies applied magnetic pellets.22,23 In addition, 2 studies used 2 types of taped objected: Liu shen pills in excess syndrome and magnetic pellets in deficiency syndrome.27,35 The remaining trial used AT in both groups, but intervention patients used magnetic pellets and the controls were given S. vaccariae.38
To find the most sensitive points, 3 RCTs used an acupoint detector33,34,38 and 2 applied a probe.26,32 Other studies did not report using detection tools to explore hypersensitive spots.
Instructions of manual pressing and health education on constipation
The most frequently used supplementary modality was instructions of manual pressing, with 16 of 17 (94.1%) of the RCTs adopting it.22–37 The remaining study reported that taped objects were left in situ for several days without exertion of manual pressure.38 Instructions of manual pressing mainly included four aspects: the frequency of daily pressing, duration of pressing, timing, and the required intensity. Sixteen studies with pressing implementations thoroughly described the frequency and duration of pressing. Of these studies, 3 claimed it should be done 3 times per day22,24,27 and 2 reported performing it 4 times per day.29,37 Others reported less specific instructions, such as “3–5 times per day”25,28,32,35,36 or “not less than 4 times per day,”34 Concerning the duration of pressing, 1 study considered that each of the selected acupoints should be lightly kneaded in 27 circles every time;36 5 studies described different duration of pressing each acupoint each time, ranging from 30 seconds to 3 minutes;22,26,27,35,37 and 10 studies reported that all of the selected acupoints should be pressed for some time, varying from 60 seconds to 5 minutes.23–25,28–34 Among 17 RCTs, only 1 mentioned the timing for manual pressing, claiming that it should be done 15 minutes before defecation.31 As for intensity, 3 of the eligible studies emphasized that in patients with excess syndrome pressing should be done with strong force.23,25,35 Inversely, mild force was used for patients with a deficiency syndrome. Of these 3 RCTs, 1 explained in detail how to implement manual pressing.35 Thirteen RCTs considered a patient's subjective feelings of de qi, in which soreness, numbness, distention, heaviness, or hotness represented suitable intensity.22,24–28,30–36 Additionally, 1 RCT used the pressing force that the patients could tolerate as the criteria.29
Health education on constipation during the intervention mainly referred to dietary guidance, advice on exercise, established bowel habits, psychological care, and drug administration. Eight of the 17 studies did not elaborate,23,25,26,29,34–37 whereas the others had provided at least 1 of those proposals to the patients.
Duration and follow-up of AT
All RCTs gave explicit information on the intervention periods. Duration was described in terms of number of days sessions. Eleven RCTs stated the duration of AT as number of days, which ranged from 3 to 60 days.22–24,26,27,29,30,33–35,38 However, 81.8% (9 of 11) had interventions that lasted longer than 2 weeks.22–24,27,29,30,34,35,38 Six RCTs described the group intervention as number of sessions as well as days per session.25,28,31,32,36,37 The number of sessions ranged from 4 to 20. Of these 6 studies, 4 (66.7%) reported interventions lasting for more than 14 sessions.25,28,32,37
Fourteen of the 17 RCTs did not report a plan for a follow-up visit,23–28,30–37 and the follow-up periods of the 3 RCTs ranged from 30 days to 6 months.22,29,38
Compliance and attrition rate
The therapeutic effect can be influenced by many factors; the quantity and quality of manual pressing applied play a decisive role under certain conditions. However, only 1 article reported on participants' adherence the instructions for manual pressing.38 Two RCTs mentioned the attrition of the participants after receiving AT,22,38 whereas the others did not explicitly report this. Only 1 of those 2 RCTs reported a specific proportion; the overall dropout rate was 23.1%.38
Outcome analysis
Of 17 RCTs, the most frequently used therapeutic outcome criteria for constipation were the “Standards for Diagnosis and Curative Effect of Chinese Medical Symptoms,” developed by the State Administration of Traditional Chinese Medicine of PRC,39 or the “Clinical Guideline of New Drugs for Traditional Chinese Medicine,” published by Medicine Science and Technology Press of China.40 For both of them, criteria for improvement consisted of having a bowel movement without straining within 2 days, accompanied by relief of constipation symptoms or return to normal defecation. “No effect” was defined as no improvement in or worsening of constipation or symptoms associated with constipation. A final time-point meta-analysis was performed because of the inconsistent appraisal times of the 17 RCTs. The therapeutic outcomes of all eligible RCTs are summarized in Table 4.
Table 4.
Therapeutic Outcomes of Randomized Controlled Trials on Auriculotherapy for Constipation
| Study, year | Outcome measure | Main results | Adverse events |
|---|---|---|---|
| Cai et al., 2011 | 1. Scores of constipation symptoms 2. Score of lifestyle 3. Use of laxatives | 1. Significant improvement, p<0.05 E: pre-AT 16.10±3.24, post-AT 14.03±3.82 (p<0.05); C: pre-Rx 15.89±2.74, post-Rx 15.50±2.38 (p>0.05); E group had significant difference between follow-up period and pre-Rx (p<0.05) | None |
| 2. No difference between E and C (p>0.05) but significant improvement in E and C within groups E: pre-Rx 15.35±2.16, post-Rx17.65±2.09 (p<0.05); C: pre-Rx 15.10±3.57, post-Rx 17.25±3.77 (p<0.05) | |||
| 3. Significant difference, p<0.05; E: pre-Rx 48, post-Rx 22; C: pre-Rx 53 post-Rx 48 | |||
| Chen et al., 2012 | Total effective rate | No significant difference, p>0.05; E: 88.57% vs.; C: 75.76% | NM |
| Chen et al., 2011 | 1. Effective rate 2. Defecation habit score: ease of defecation, feeling of incomplete bowel evacuation, straining, duration of defecation | 1. E (excess: 42.0%, deficient: 31.0%) vs.; C: 0.0% at 30 d; E (excess: 74.2%, deficient: 79.3%) vs.; C: 0.0% at 60 d 2. Significant improvement at 60 d, p<0.001; E: 8.55±2.25 vs. C: 11.49±1.96; significant improvement within E group (p<0.001) | NM |
| He and Pei, 2012 | Total effective rate | Significant difference, p<0.01; E: 95.65% vs. C: 69.05% | NM |
| Hong and Shen, 2013 | Total effective rate | Significant difference, p<0.05; E: 93.3% vs. C: 70.0% | NM |
| Ji et al., 2010 | 1. Total effective rate 2. Symptom score: defecation interval, stool consistency, straining, duration of defecation, abdominal distension condition, loss of appetite 3. Occurrence of adverse effects 4. Use of other auxiliary defecation method | 1. Significant difference, p=0.00; E: 91.89% vs. C: 30.56% 2. Significant improvement in each symptom, p<0.05; significant improvement in E and C within groups (p<0.05) 3. No difference 4. E: None; C: 58. 3% (21/36) using other auxiliary defecation method | E: 1 patient with excess syndrome had slight localized redness and damage of skin (cured in 2 d after sterilizing with Anerdian) |
| Li et al., 2012 | 1. Symptoms of constipation: PAC-SYM 2. Quality of life: PAC-QOL 3. Physical Activity Questionnaire 4. Bowel movement per week 5. Stool consistency | 1. No significant group effects; time effects were significant in E group but not in C group 2. No significant group effects; time effects were significant in C group but not in E group 3. No mediating effects on outcome variables 4. Increased in E group but decreased in C group 5. 13 patients had softer stools after the intervention; E:6; C:7 | 7 patients with mild, tolerable, and short-term itchiness of the ears after adopting AT (n=7) E: 2 C: 5 |
| Liu et al., 2009 | Total effective rate | Significant difference, p<0.01; E: 97.7% vs. C: 68.2% | NM |
| Meng et al., 2011 | 1. Total effective rate | 1. No difference (p>0.05); E: 100% vs. C: 100% | NM |
| 2. Recurrence rate | 2. At 1-mo follow-up, E: 100% vs. C: 92.9%; at 3-mo follow-up, E: 91.7% vs. C: 85.7%; at 6-mo follow-up, E: 91.7% vs. C: 71.4% | ||
| Qian, 2012 | Total effective rate | Significant difference, p<0.05; E: 95.2% vs. C: 85.7% | None |
| Wang et al., 2011 | Total effective rate | Significant difference, p<0.05’ E: 93.7% vs. C: 78.7% | NM |
| Yin and Qin, 2012 | Total effective rate | Significant difference, p<0.01; E: 98.3% vs. C: 75.0% | None |
| Zeng et al., 2012 | 1. Total effective rate 2. Number of bowel sounds/min 3. Frequency of defecation per week 4. Symptom score | 1. No difference (p>0.05); E: 80.0% vs. C: 63.3% 2. Significant improvement, p=0.000; E: 4.37±0.67 vs. C: 3.33±0.66 3. E: 2.25±0.49 vs. C: 2.39±0.71; difference not reported 4. Difference between E and C not reported, significant improvement in E group; E: pre-AT 1.87±0.73 vs. post-AT 1.31±0.43 (p<0.05) | None |
| Zhang et al., 2009 | 1. Total effective rate 2. Condition of abdominal distension and loss of appetite 3. Effects on renal function: BUN, creatinine and BUA | 1. Significant difference, p<0.01; deficient: E: 96.7% vs. C: 70.0% (p<0.01); excess: E: 93.3% vs. C: 60.0% (p<0.01) 2. Significant difference in the symptom of anorexia, p<0.01; E: 64.3% vs. C: 40.4%; no difference in the symptom of abdominal distension (p>0.05); significant improvement in both symptoms in E and C within groups (p<0.01) 3. Excess: significant difference in BUN, p<0.05; E: 12.99±6.73 vs. C:17.55±8.91; no difference in BUA, creatinine, p>0.05; deficient: no difference in BUN, BUA, creatinine, p>0.05 | E: 2 patients with excess type had slight skin redness and soreness in the ear points (cured after sterilizing with Anerdian) |
| Zhang and Yang, 2009 | 1. Total effective rate 2. First defecation time 3. Scores of constipation symptoms: first defecation time, defecation interval, duration of defecation, stool consistency, ease of defecation, awareness of defecation, concomitant symptoms 4. Effect of individual symptoms | 1. No difference (p>0.05); E: 90% vs. C: 83.33% 2. Significant difference, p<0.05; E: 6.68±5.48 vs. C: 11.80±7.23 3. Significant improvement, p<0.01; E: 5.45±2.71 vs. C: 8.68±3.57; significant improvement in E and C within groups (p<0.01) 4. Significant difference between E and C in duration of defecation, stool consistency, awareness of defecation, ease of defecation (p<0.05); significant improvement in defecation interval, duration of defecation, stool consistency, ease of defecation, awareness of defecation in E and C within groups (p<0.01) | None |
| Zhong and Zhang, 2007 | 1. Total effective rate 2. Effective rate after one treatment course 3. Defecation in 24 h 4. CTT 5. Scores of constipation symptoms: defecation interval, duration of defecation, stool consistency, ease of defecation, concomitant symptoms | 1. Significant difference, p<0.05; E: 90% vs. C: 80% 2. No difference (p>0.05); E: 63.33% vs. C: 50% 3. No difference (p>0.05); E: 73.3% vs. C: 76.7% 4. No difference (p>0.05); E: 86.67% vs. C: 83.33% 5. Significant improvement in defecation interval, p<0.05; E: 0.3667±0.7184 vs. C: 0.7667±0.7739; significant improvement in concomitant symptoms, p<0.05; E: 0.4000±0.4624 vs. C: 0.7167±0.6783; no difference in duration of defecation, stool consistency, ease of defecation (p>0.05) | None |
| Zhou et al., 2012 | 1. Total effective rate | 1. Significant difference, p<0.05; E: 92.0% vs. C: 76.0% | None |
| 2. Quality of life: PAC-QOL | 2. Significant improvement, p<0.05; E: 56.3±17.8 vs. C: 70.1±19.0; significant improvement in E and C within groups (p<0.05) |
E, experimental group; C, control group; Rx, treatment; NM, not mentioned; PAC-SYM, Patient Assessment of Constipation–Symptom questionnaire; PAC-QOL, Patient Assessment of Constipation Quality of Life questionnaire; BUN, blood urea nitrogen; BUA, blood uric acid; CTT, colonic transit time.
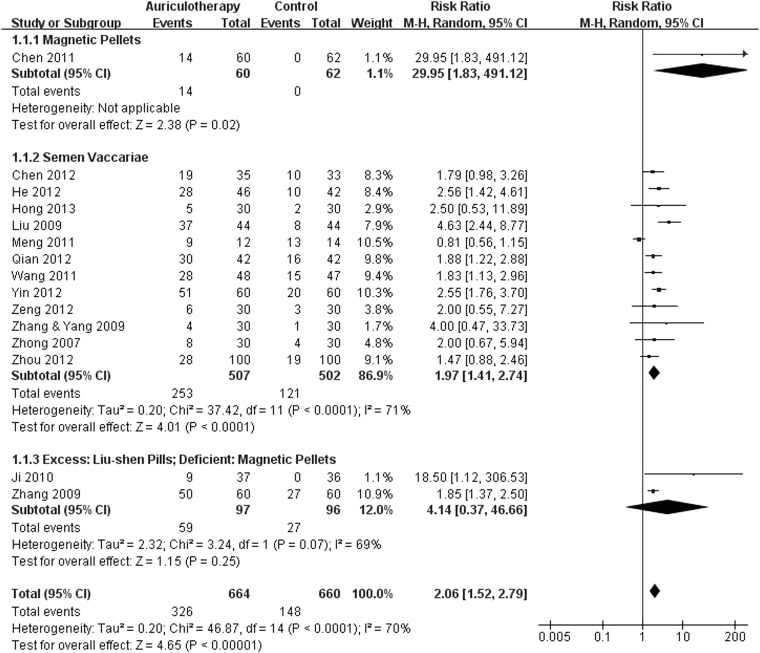
Improvement rate of AT for constipation
Fifteen RCTs used the improved criteria for constipation23–37 reported the number of improved cases. Meta-analysis revealed that, compared with control, AT had a moderate, significant effect on managing constipation (RR, 2.06; 95% CI, 1.52–2.79; p<0.00001) (Fig. 2). Subgroup analysis revealed that groups that used S. vaccariae were statistically favored over the controls (RR, 1.97; 95% CI, 1.41–2.74; p<0.0001), while the group that used magnetic pellets in deficiency syndrome and Liu shen pills in excess syndrome was not statistically favored (p=0.25). Only 1 RCT used magnetic pellets solely for AT, and this group showed more efficacy than the control group (p=0.02).
FIG. 2.
Forest plot of comparison: 1 auriculotherapy versus controls, outcome: 1.1 the improvement rate. CI, confidence interval; MH, Mantel Haenzel.
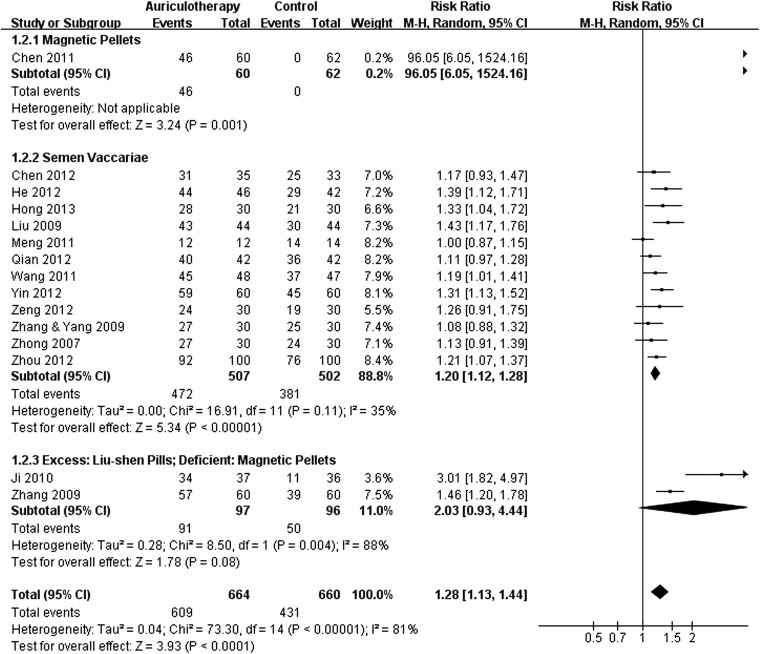
Total effective rate of AT for constipation
Fifteen RCTs used the criteria of “no effect” for constipation.23–37 According to the criteria, it was possible to calculate the total effective rate. Meta-analysis revealed that, compared with control, AT had a moderate, significant effect in relieving constipation (RR, 1.28; 95% CI, 1.13–1.44; p<0.0001) (Fig. 3). Subgroup analysis revealed that groups that used S. vaccariae were statistically favored over controls (RR, 1.20; 95% CI, 1.12–1.28; p<0.00001), whereas the group that used magnetic pellets in deficiency syndrome and Liu shen pills in excess syndrome was not statistically favored (p=0.08). Only 1 RCT used magnetic pellets solely for AT, and that group showed more efficacy than the control group (p=0.001).
FIG. 3.
Forest plot of comparison: 1 auriculotherapy versus controls, outcome: 1.2 total effective rate.
Abdominal distension
Two RCTs used the condition of abdominal distension as an outcome measure;27,35 the data were available or were calculated. Meta-analysis showed that, compared with control, AT had no statistically significant effect in relieving abdominal distension at the final time point (RR, 1.65; 95% CI, 0.51–5.35; p=0.40) (Fig. 4).
FIG. 4.
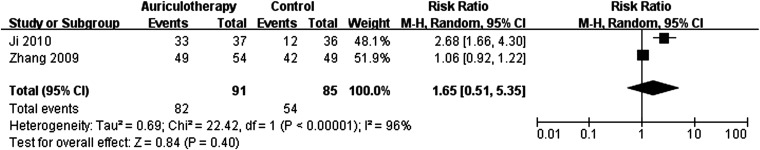
Forest plot of comparison: 1 auriculotherapy versus controls, outcome: 1.3 abdominal distension.
Anorexia
Two RCTs used the condition of anorexia as an outcome measure;27,35 the data were available or calculated. Meta-analysis showed that, compared with control, AT had no statistically significant effect on improving anorexia (RR, 2.56; 95% CI, 0.91–7.25; p=0.08) (Fig. 5).
FIG. 5.
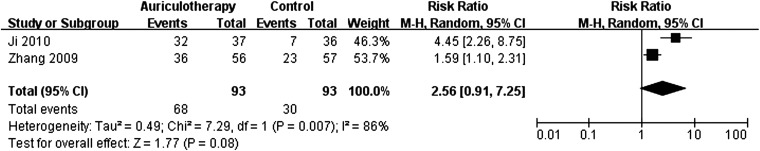
Forest plot of comparison: 1 auriculotherapy versus controls, outcome: 1.4 anorexia.
Other outcomes
Of the remaining 2 studies that were not included in the meta-analysis, 1 showed that AT had a significant positive effect on relieving constipation symptoms, including ease of defecation, feeling of incomplete bowel evacuation, straining, and duration of defecation.22 The other study, which adopted AT in both the experimental and control groups, showed no significant difference between groups.38 In that study, however, for the Patient Assessment of Constipation–Symptoms instrument, time effects were significant in the experimental group but not the control group, while for Patient Assessment of Constipation–Quality of Life instrument, time effects were significant in the control group but not in the experimental group.
Adverse effects of AT
Ji and colleagues27 reported that only 1 of 37 patients in their experimental group had slight localized and redness and damage on the skin. Zhang et al.35 reported that 2 of 60 patients with excess syndrome in the experimental group experienced adverse events: 1 with slight skin redness and breakdown and 1 with soreness of the ear points. Li et al.38 adopted AT in both the experimental and control groups and reported that 7 of 39 patients in the two groups had mild, tolerable, and short-term itchiness of the ears after the intervention. No other adverse events were recorded.
Discussion
On the whole, this review found that for adults, AT probably has favorable effects on chronic constipation compared with other agents. For other symptoms associated with constipation, such as abdominal distension or anorexia, results of meta-analyses did not show any statistical significance. Subgroup analysis revealed that groups using S. vaccariae or magnetic pellets were both statistically favored over the controls in managing or relieving constipation, while the group using magnetic pellets in deficiency syndrome and Liu shen pills in excess syndrome were not significantly favored.
A previous systematic review17 assessed the role of AT in managing constipation but made no conclusion about its effectiveness. All the studies included in that review appear to have been of a clinical nature, not RCTs. Indeed, if non-RCTs are included in a review that addresses an area of scientific uncertainty, the objective is to give insights for the development of future RCTs by combining all available evidence. Reviews of RCTs are considered the gold standard in the hierarchy of scientific evidence. The recent publication of several RCTs with good study design and methods offers the potential for meta-analysis of RCTs.
The current review included only RCTs to assess the effects of AT for the management of constipation. As illustrated earlier, this approach provides a more concrete picture of the role of AT in managing constipation than has been available.
Few reports have addressed the adverse effects of AT for managing constipation. Two of the 17 included studies reported that 1 of 37 patients and 2 of 60 patients had slight localized redness and damage to the skin, and 1 RCT reported that 7 of 39 patients had mild, tolerable, and short-term itchiness of the ear points. There is not enough evidence to show that AT is unsafe for patients with constipation.
As mentioned earlier, AT is a complementary strategy that stimulates the external surface of the auricle to alleviate pathologic conditions in other parts of the body. How does AT benefit patients with constipation? Currently, the research on AT has two main lines on a global scale: one is the French AT of Nogier, and the other is the Chinese. In the former line, the auricular microsystem is considered reflexology of a neurologic action.41 Perforation of a reflex point in the ear probably works because groups of pluripotent cells contain information from the whole organism and attempt to create regional organization centers representing different parts of the body. In the Chinese line of AT, ear points are selected according to the principles of Traditional Chinese Medicine.42 On the basis of Traditional Chinese Medicine, the vital energy (qi) of the body circulates in the channels and collaterals and works on other areas in the interconnection between the internal and external, the viscera and organs. Continuously stimulating with proper intensity a particular area of the ear can adjust the rise or fall of qi and blood in the meridians and channels; at the same time it can have regulative effects on the corresponding zang-fu function. A Chinese scholar, Yun, discovered that placing pressure on the stomach area of auricular cartilage could induce obvious changes in gastrointestinal peristalsis.43 She reported that upper gastrointestinal radiography showed adopting AT could make the original strong peristaltic wave weakened, and vice versa. All these factors may explain the positive role of AT in managing constipation.
In 1998, the National Center for Complementary and Alternative Medicine was established by the U.S. Congress in response to the public's continuing interest in complementary and alternative medicine (CAM).44 The aim is to explore CAM practices and, furthermore, to facilitate the integration of CAM and conventional medicine.45 Better yet, Traditional Chinese Medicine, as one of the whole medical systems, has full support of NCCAM.44 AT, as a TCM external therapy, has become one of the most popular Eastern practices worldwide. Previously, AT was considered an adjunct and complement to other practices; it has been developed into a distinct treatment system of its own. According to the studies reported in China in the past 20 years, AT clearly has great efficiency in managing constipation.46,47 Moreover, a study by Kurebayashi et al. showed that AT considers humans to be an integrated whole, with no barriers between the mind, body, and spirit, which conforms to the modern integrated biological-psychological-social medical model.48
As mentioned earlier, all the eligible RCTs were published from 2007 to 2013. The standardized research in effectiveness of AT in managing constipation has just started, so searching for powerful original evidence is not easy. In general, no eligible RCTs were fully free of risk of bias or were methodologically rigorous in terms of random sequence generation, allocation concealment, blinding, and record of incomplete outcome data. Given these concerns, caution must be exercised in drawing a definitive conclusion. To make the findings more convincing, some special individualized approaches, such as excluding studies labeled as level C by conducting critical appraisal and narrowing down the inclusion criteria, were adopted in this study. These identified methodologic flaws will have to be considered as empirical evidence in future randomized controlled trials on the topic.
This review has some limitations. First, because of the paucity of evidence at one particular time point, this review involved meta-analyses at a final time point, which cannot describe the effectiveness of AT for constipation over time. In the future, as more rigorous RCTs are performed, summary estimates from primary studies can be calculated by using an all-time-points meta-analysis, which can capture the trend of effectiveness over the time. This has more important practical significance for the management of chronic constipation. Another limitation of this review is that the original evidence is not powerful on the whole considering the small sample sizes in some included trials. Third, all eligible studies were produced by authors in mainland China or Hong Kong. Considering cultural and geographical differences, the appropriateness of using AT as a complementary strategy for constipation in Western countries and other regions is uncertain.
In conclusion, the 17 eligible RCTs used AT as a complementary strategy to treat constipation. Meta-analysis illustrated that because AT is a relatively safe strategy for treating disease, it is probably more beneficial than other agents in managing constipation. However, all eligible studies were conducted in China. No definitive conclusion can be made because of cultural and geographic differences. Further rigorous RCTs are warranted worldwide to confirm the effect and safety of AT for constipation.
Acknowledgments
Our work was financed by Grant-in-aid for scientific research from the Summit of six categories of talents in Jiangsu Provincial Human Resources and Social Security Office of China (No. 2013-WSN-046).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Andrews CN, Storr M. The pathophysiology of chronic constipation. Can J Gastroenterol 2011;25(Suppl B):16B–21B [PMC free article] [PubMed] [Google Scholar]
- 2.Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol 2011;25:3–18 [DOI] [PubMed] [Google Scholar]
- 3.Zhao YF, Ma XQ, Wang R, et al. . Epidemiology of functional constipation and comparison with constipation-predominant irritable bowel syndrome: the Systematic Investigation of Gastrointestinal Diseases in China (SILC). Aliment Pharmacol Ther 2011;34:1020–1029 [DOI] [PubMed] [Google Scholar]
- 4.Stark ME. Challenging problems presenting as constipation. Am J Gastroenterol 1999;94:567–574 [DOI] [PubMed] [Google Scholar]
- 5.Rogers J. How to manage chronic constipation in adults. Nurs Times 2012; 108:12, 14, 16 passim [PubMed] [Google Scholar]
- 6.Chen HY, Shi Y, Ng CS, et al. . Auricular acupuncture treatment for insomnia: a systematic review. J Altern Complement Med 2007;13:669–676 [DOI] [PubMed] [Google Scholar]
- 7.Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. 3rd ed. Edinburgh: Churchill Livingstone, 2003 [Google Scholar]
- 8.Asher GN, Jonas DE, Coeytaux RR, et al. . Auriculotherapy for pain management: a systematic review and meta-analysis of randomized controlled trials. J Altern Complement Med 2010;16:1097–1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soliman N, Frank BL. Auricular acupuncture and auricular medicine. Phys Med Rehabil Clin N Am 1999;10:547–554 [PubMed] [Google Scholar]
- 10.Hsieh CH, Su TJ, Fang YW, Chou PH. Efficacy of two different materials used in auricular acupressure on weight reduction and abdominal obesity. Am J Chin Med 2012;40:713–720 [DOI] [PubMed] [Google Scholar]
- 11.Suen LK, Wong EM. Auriculotherapy with magnetic pellets produces longitudinal changes in sleep patterns of elderly patients with insomnia. J Altern Complement Med 2007;13:306–307 [DOI] [PubMed] [Google Scholar]
- 12.do Prado JM, Kurebayashi LF, da Silva MJ. Auriculotherapy effectiveness in the reduction of anxiety in nursing students. Rev Esc Enferm USP 2012;46:1200–1206 [DOI] [PubMed] [Google Scholar]
- 13.Vera-Portocarrero L, Cordero T, Billstrom T, et al. . Differential effects of transcutaneous electrical stimulation (TENS) and subcutaneous electrical stimulation (SQS) on inflammatory and neuropathic pain. J Pain 2012;13:S69. [DOI] [PubMed] [Google Scholar]
- 14.Carmelo G, Dolores P, Iacopo B, et al. . Acupuncture and auriculotherapy for chemotherapy adverse effects. Eur J Integr Med 2012;4:128 [Google Scholar]
- 15.Lai HM, Cheng W, Li P, et al. . Wangbuliuxing therapy for constipation in fractured patients [in Chinese]. Nurs J Chin Peoples Liberation Army 2000;17:9–10 [Google Scholar]
- 16.Xiao AH. Influence of ear point pressing and abdominal massage on constipation in tumor patients treated with chemotherapy. Chin J Mod Nurs 2008;14:2947–2949 [Google Scholar]
- 17.Li MK, Lee TF, Suen KP. A review on the complementary effects of auriculotherapy in managing constipation. J Altern Complement Med 2010;16:435–447 [DOI] [PubMed] [Google Scholar]
- 18.Longstreth GF, Thompson WG, Chey WD, et al. . Functional bowel disorders. Gastroenterology 2006;130:1480–1491 [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011] ed: The Cochrane Collaboration, 2011 [Google Scholar]
- 20.Suen LK, Wong TK, Chung JW, Yip VY. Auriculotherapy on low back pain in the elderly. Complement Ther Clin Pract 2007;13:63–69 [DOI] [PubMed] [Google Scholar]
- 21.Liu SY, Lin F, Wang LL. Clinical observation on treatment of functional constipation with auricular point plaster therapy [in Chinese]. Chin Gen Pract Nurs 2011;9:210–211 [Google Scholar]
- 22.Cai JP, Zhang YL, Zhu KM. Observation on effect of applying magnet beads sticking and pressing auricular acupoints for community groups with predisposition of constipation [in Chinese]. Chin Nurs Res 2011;25:2059–2061 [Google Scholar]
- 23.Chen SL, Chen ZY, Lv Y, Cheng JL. Analysis of the effect of auricular point plaster therapy on chronic constipation [in Chinese]. Shanghai J Acu-mox 2011;30:540–541 [Google Scholar]
- 24.Chen YF, Zhan XF, Chen XH. Observation on the effect of applying auricular point plaster therapy for senile constipation of Qi-deficiency [in Chinese]. Fujian J Trad Chin Med 2012;43:62 [Google Scholar]
- 25.He LH, Pei JB. Treatment of 46 cases of constipation in patients with coronary heart disease using auricular taping therapy [in Chinese]. Zhejiang J Trad Chin Med 2012;47:120 [Google Scholar]
- 26.Hong JN, Shen Q. Clinical observation on the effect of auricular taping therapy combined with oral phenolphthalein for constipation in patients with cancer [in Chinese]. Chin J Trad Med Sci Technol. 2013;20:29 [Google Scholar]
- 27.Ji XP, Zhang YL, Cai JP, Chen FL. Clinical observation on treatment of senile functional constipation with auricular taping therapy [in Chinese]. Shanghai J Trad Chin Med 2010;44:85–87 [Google Scholar]
- 28.Liu SX, Liu F, Sun HX. Clinical observation on treatment of senile habitual constipation with auricular point plaster therapy. Chin J Misdiagnostics 2009;9:5594–5595 [Google Scholar]
- 29.Meng P, Wang J, Cao YX, et al. . Clinical observation on the effect of auricular taping combined with cognitive-behavioral therapy for college girl students with slow transit constipation [in Chinese]. Int J Trad Chin Med 2011;33:1036–1038 [Google Scholar]
- 30.Qian AP. Treatment of 42 cases of constipation associated with subarachnoid hemorrhage by using auricular taping therapy [in Chinese]. Chin J Trad Med Sci Technol 2012;19:469–470 [Google Scholar]
- 31.Wang LQ, Zhu HB, Tong Y. Clinical observation on the effect of auricular taping therapy for constipation in patients with diabetes [in Chinese]. J Chin Trad Chin Med Inf 2011;3:230 [Google Scholar]
- 32.Yin H, Qin LH. Clinical observation on the effect of auricular taping therapy for constipation in stroke patients with qi deficiency and blood stasis syndrome [in Chinese]. Clin J Trad Chin Med 2012;24:504–505 [Google Scholar]
- 33.Zeng J, Tan ZY, Zou ZX. Clinical observation on treatment of constipation in pregnant women using auricular taping therapy [in Chinese]. Chin J Inf Trad Chin Med 2012;19:62–63 [Google Scholar]
- 34.Zhang Y. Clinical observation on treatment of senile habitual constipation with auricular taping therapy [in Chinese], Shandong University of Traditional Chinese Medicine; 2009 [Google Scholar]
- 35.Zhang YL, Cai JP, Qin XF, et al. . Effect of auricular-plaster therapy with syndrome-differentiation on constipation in patients with chronic renal disease [in Chinese]. Shanghai Nurs 2009;9:5–8 [Google Scholar]
- 36.Zhong X. Observation on the effect of auricular taping therapy for slow transit constipation in type of Qi-deficiency syndrome of lung and spleen [in Chinese]. Beijing: Beijing University of Chinese Medicine, 2007 [Google Scholar]
- 37.Zhou XX, Zhong Y, Teng J. Senile habitual constipation treated with auricular therapy based on the pattern/syndrome differentiation: a randomized controlled trial [in Chinese]. Chin Acu-mox 2012;32:1090–1092 [PubMed] [Google Scholar]
- 38.Li M, Lee D, Suen L. A randomised placebo-controlled trial evaluating the complementary effects of auriculotherapy in relieving constipation symptoms among elderly residential care home residents. Intern J Nurs Pract 2012;18(Suppl 1):59 [Google Scholar]
- 39.The State Administration of Traditional Chinese Medicine of PRC. Diagnostic and Curative Criteria: TCM Internal Medicine (ZY 1001, 1-94), 1994 [Google Scholar]
- 40.Zheng XY. Clinical Guideline of New Drugs for Traditional Chinese Medicine. Beijing: Medicine Science and Technology Press of China, 1993 [Google Scholar]
- 41.Nogier P. Auricolotherapy to Auricolomedicine. Sainte-Ruffine, France: Maisonneuve, 1983 [Google Scholar]
- 42.Huang LC. The Diagnosis of Auricular Points. Beijing: Science and Technology Literature Publishing House, 2004 [Google Scholar]
- 43.Yun M, Ding CQ. Research of effects on gastric function by pressing ear points with fingers [in Chinese]. Shanghai J Acu-mox 1987;2:4–5 [Google Scholar]
- 44.Pearson NJ, Chesney MA. The National Center for Complementary and Alternative Medicine. Acad Med 2007;82:967. [DOI] [PubMed] [Google Scholar]
- 45.Pearson NJ, Chesney MA. The CAM Education Program of the National Center for Complementary and Alternative Medicine: an overview. Acad Med 2007;82:921–926 [DOI] [PubMed] [Google Scholar]
- 46.Cai JP, Qin XF, Zhang YL. Development on treatment of different types of constipation in auricular taping therapy [in Chinese]. Shanghai Nurs 2006;6:59–60 [Google Scholar]
- 47.Zhong Y, Jiang GH. Development on clinical treatment of constipation with auriculotherapy [in Chinese]. J Clin Acu-mox 2008;24:53–56 [Google Scholar]
- 48.Kurebayashi LF, Gnatta JR, Borges TP, et al. . The applicability of auriculotherapy with needles or seeds to reduce stress in nursing professionals. Rev Esc Enferm USP 2012;46:89–95 [DOI] [PubMed] [Google Scholar]