Abstract
BACKGROUND:
The purpose of triage is to identify patients needing immediate resuscitation, to assign patients to a pre-designed patient care area, and to initiate diagnostic/therapeutic measures as appropriate. This study aimed to use emergency severity index (ESI) in a pediatric emergency room.
METHODS:
From July 2006 to August 2010, a total of 21 904 patients visited the International Department of Beijing Children’s Hospital. The ESI was measured by nurses and physicians, and compared using SPSS.
RESULTS:
Nurses of the hospital took approximately 2 minutes for triage. The results of triage made by nurses were similar to those made by doctors for ESI in levels 1-3 patients. This finding indicated that the nurses are able to identify severe pediatric cases.
CONCLUSION:
In pediatric emergency rooms, ESI is a suitable tool for identifying severe cases and then immediate interventions can be performed accordingly.
KEY WORDS: Pediatrics, Emergency Department, Triage, Emergency severity index
INTRODUCTION
Emergency department (ED) is a vital component in our health care safety network. There has been a steady increase in the volume and acuity of patient visits to EDs, now with well over 100 million Americans (30 million children) receiving emergency care annually. This rise in ED utilization has effectively saturated the capacity of EDs and emergency medical services in many communities. The resulting phenomenon, commonly referred to as ED overcrowding, now threatens access to emergency services for those who need them the most.[1-4] ED overcrowding can lead to delays in time-sensitive diagnostic decisions, leaving of patients without completion of care, dissatisfaction of both patients and care providers, poor treatment and health-related outcomes. The fact is that not all of the patients visiting ED are in life-threatening situations, therefore an effective and accurate triage system can reduce ED delays and ED overcrowding.[5-8]
Triage is the prioritization of patient care (or victims during a disaster) based on illness/injury, severity, prognosis, and resource availability. The purpose of triage is to identify patients needing immediate resuscitation, to assign patients to a pre-designed patient care area, and to initiate diagnostic/therapeutic measures as appropriate.[9-11] It has been using in hospitals since the 1990s, and has become more and more important especially in ED. There are various triage systems ranging from two to five levels. In the United States, a three-level triage system is most commonly used (69%), with 12% of EDs using a four-level system, 3% using a five-level model, and 16% using no acuity system according to an ENA survey in 2001.[12-15]
Children change with growth and development. The triage of children is more complicated and time-consuming than that of adults.[16] Emergency severity index (ESI) is a five-level triage system developed in the United States using a flowchart-based triage algorithm.[17-19] The ESI uses patient acuity (stability of vital signs, degree of distress) as well as expected resource intensity and timeliness (expected staff response, time to disposition) to define five levels from level 1 (most urgent) to level 5 (least urgent). ESI is one of the international triages in pediatric EDs as AST, CAST and the Manchester Triage Scale.[20-25] The present study aimed to describe the application of the ESI system from July 2006 to August 2010 in the ED of Beijing Children’s Hospital.
METHODS
Data
The data were from children who had been admitted to the ED of International Department, Beijing Children’s Hospital from July 2006 to August 2010.
Methods
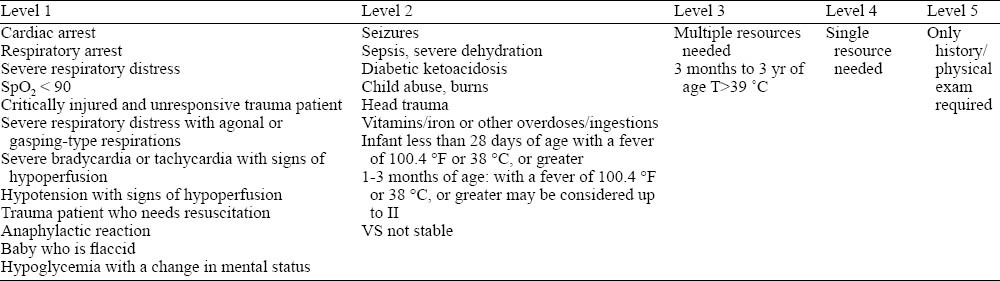
ESI is a five-level ED triage algorithm that provides clinically relevant stratification of patients into groups 1 (most urgent) to 5 (least urgent) on the basis of acuity and resource needed. Level 1: unresponsive, apneic, intubated, etc; level 2: confused or lethargic, severe pain, respiratory distress, unstable vital signs; levels 3-5: stable vital signs; level 3: multiple resources needed (X-ray exam, laboratory exam, etc.); level 4: single resource needed (X-ray exam, consultation, etc.); level 5: history/ physical exam only. ESI for children is listed in Table 1.
Table 1.
Definition of ESI for children
Nurses and doctors in ED are trained to complete the ESI (version 4) triage for all children visiting the ED. The nurses are in charge of measuring vital signs (pulse, blood pressure, oxygen saturation) using Welch Allyn 300 (USA), body temperature with an electronic thermometer, pain level with the Wong Faces Scale, and breathing frequency. Based on these data, the children were classified into ESI levels 1-5. Level 1 children were allocated on rescue beds, and doctors were asked to provide immediate medical treatments. Level 2 children were directly sent to treatment rooms and waited for doctors within 5 minutes. Level 3 children were arranged to have interviews within 10 minutes before level 4 and 5 children. Level 4 and 5 children waited for interviews based on levels and time of registrations. Triage nurses carried out the general treatment when level 4 and 5 children were waiting. All triage results were verified by doctors.
RESULTS
Demographic characteristics
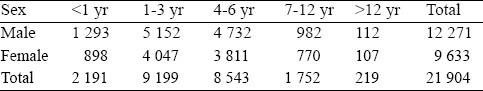
Altogether 21 904 children visited ED. Among them, 20 558 (93.85%) children visited department of internal medicine, 852 (3.98%) visited department of surgery, 397 (1.82%) visited otorhinolaryngology department, 97 (0.44%) visited other departments (dental, ophthalmology, dermatology). The top three causes for internal medicine visits were upper respiratory infections (54.5%), lower respiratory infections (25%), and digestive system illnesses (13.1%). The top three causes for surgery visits were injuries (61.85%), radius displacement and acute abdomen (7.51%). The top three causes for otorhinolaryngology visits were otitis, rhinitis and foreign body. The age distribution of the patients is listed in Table 2.
Table 2.
Distribution of age and sex
Severity triage
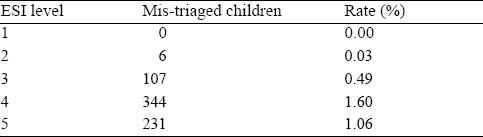
Triage designations were initially made by one of triage nurses who performed triage duties during the study period. Each of these triage nurses had worked full time as a nurse in the ED, and each had formal training in the use of ESI criteria. Whether a patient received an immediate intervention was determined by a review of the entire nursing and physician record for each patient. Triage results were compared between nurses and physicians, and a statistical difference was seen in the total triage results between the nurses and doctors (P<0.05) (Table 3), but there was no difference in results from level 1-3 children (P>0.05). If the determinations of physicians were used as final results, the triage nurses made 588 false decisions (2.68%). However, there were no false determinations in level 1 children. According to the triage results of physicians, 6 children were triaged to level 2 from level 3, 113 children to level 5 from level 4, and 231 children to level 5 from level 4 (Table 4).
Table 3.
The comparison of triage between nurses and doctors
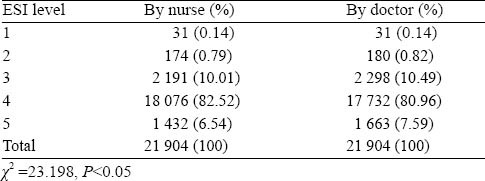
Table 4.
Mis-triaged children
Distribution of diseases
Traumatic brain injury, brain hernia, tracheal foreign body, septic shock, volvulus, congenital genetic metabolic diseases combined with respiratory failure, sepsis with meningitis were found in each of level 1 children, respectively. Besides, there were two children with large intracranial hemorrhage, four with arrhythmia, and four with apnea. In level 2 children, there were 3 newborns with temperature above 38 ˚C, 5 with poisoning, 5 with intussusceptions, 8 with sepsis, 13 with acute appendicitis, 26 with unstable vital signs, 32 with aching, 36 1-3-month infants with temperature over 38 ˚C, and 52 with convulsions. The level 3 to 5 children were found to have upper respiratory infections, lower respiratory infections and digestive system illnesses.
Mis–triaged children
Six level 3 children were mis-triaged in level 2; among them, 2 children had severe asthma complicated with dyspnea and decreased breathing sound, 4 1-3-month infants with a body temperature over 38 °C. Totally 113 level 4 children were mis-triaged in level 3; among them, 52 3-month to 3-year children had a body temperature over 39 °C, 61 needed more than one clinical resource and most of them had respiratory infections requiring CBC and chest X-ray examination (two clinical resources). Totally 231 level 5 children were mis-triaged as level 4; these children had upper respiratory infections, and didn’t need clinical resources.
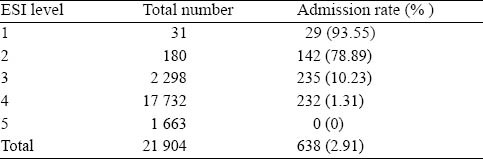
Triage and admission rate
Among the 21 904 children, 638 (2.91%) were hospitalized. The 31 level 1 children were all hospitalized, except one child died from septic shock and the other from tracheal foreign body. The admission rate for level 1 children was 93.55%. Table 5 shows the admission rates of children with different ESI levels.
Table 5.
The admission rates for children with different ESI levels
DISCUSSION
ESI is a tool using in ED triage. The ESI triage algorithm yields rapid, reproducible, and clinically relevant stratification of patients into five groups, from level 1 (most urgent) to level 5 (least urgent). The ESI provides a method for categorizing ED patients by both acuity and resource needed.[17-19] Other triage systems require triage nurses to collect clinical history, measure vital signs, evaluate ABCs, or even perform basic physical examinations. These triage systems need more time than ESI.[26] The international standard for triage is usually 2-5 minutes. However, research[27] indicated that only 22% of all emergency services in the USA can reach this standard. In our hospital triage nurses take approximately 2 minutes in performing triage.
Triage nurses can instantly and accurately triage ESI level 1 and 2 children, and the aforementioned data show that in ESI level 1-3 children the triage results of nurses were similar to those of doctors. This finding indicated that the nurses are able to identify severe pediatric cases, such as cases of brain hernia, cranium hemorrhage, respiratory failure, circular failure in ED. The successful triage of level 1 and level 2 children are extremely important in terms of providing immediate interventions.
The results of this study showed that there were differences in triage of level 3 to 5 patients made by nurses and doctors. Altogether 119 children were low-triaged, while 231 were up-triaged. Notably, 6 level 2 patients were mis-triaged in level 3. Low-triage indicates that patients may not receive timely treatments, and up-triage means possible waste of clinical resources. The mis-triage was due to nurses’ inadequent understanding of body temperature in age groups or sufficient forecast of clinical resources. Hence triage nurse training in the application of ESI criteria or revision of the ESI criteria may help to improve the triage.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: Wang L proposed and wrote the study. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics, Committee on Pediatric Emergency Medicine. Overcrowding crisis in our nation`s emergency departments: is our safety net unraveling? Pediatrics. 2004;114:878–888. doi: 10.1542/peds.2004-1287. [DOI] [PubMed] [Google Scholar]
- 3.Rost K, Hsieh YP, Xu S, Harman J. Gender Differences in Hospitalization After Emergency Room Visits for Depressive Symptoms. J Womens Health (Larchmt) 2011 Mar 21; doi: 10.1089/jwh.2010.2396. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Nanth RH. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hohenhaus SM, Travers D, Mecham N. Pediatric triage: a review of emergency education literature. J Emerg Nurs. 2008;34:308–313. doi: 10.1016/j.jen.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 6.Funderburke P. Exploring best practice for triage. J Emerg Nurs. 2008;34:180–182. doi: 10.1016/j.jen.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Lyons M. Factors that affect the flow of patients through triage. Emerg Med J. 2007;24:78–85. doi: 10.1136/emj.2006.036764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moll HA. Challenges in the validation of triage systems at emergency departments. J Clin Epidemiol. 2010;63:384. doi: 10.1016/j.jclinepi.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Kriengsoontornkij W, Homcheon B, Chomchai C, Neamsomboon W. Accuracy of pediatric triage at Siriraj Hospital, Bangkok, Thailand. J Med Assoc Thai. 2010;93:1172–1176. [PubMed] [Google Scholar]
- 10.Montejano AC, Visser LS. What is a triage nurse? J Emerg Nurs. 2010;36:85–86. doi: 10.1016/j.jen.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Seefeld AW. Triage. J Emerg Nurs. 2008;34:9–10. doi: 10.1016/j.jen.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Casey RP, Bensadigh BM, Lake MT, Thaller SR. Dentoalveolar trauma in the pediatric population. J Craniofac Surg. 2010;21:1305–1309. doi: 10.1097/SCS.0b013e3181e206c1. [DOI] [PubMed] [Google Scholar]
- 13.Holt K. Developing a triage tool for paediatric care. Emerg Nurse. 2009;17:12–17. doi: 10.7748/en2009.06.17.3.12.c7087. [DOI] [PubMed] [Google Scholar]
- 14.Parenti N. Reliability and validity of two four-level emergency triage systems. Eur J Emerg Med. 2009;16:115–120. doi: 10.1097/MEJ.0b013e328310b594. [DOI] [PubMed] [Google Scholar]
- 15.Chiu HY, Chen LC, Lin XZ, Sang YY, Kang QJ, Chao YF. Current trends in emergency triage in Taiwan: the five-level triage system. Hu Li Za Zhi. 2008;55:87–91. [PubMed] [Google Scholar]
- 16.Thompson T. Triage assessment in pediatric emergency departments: a national survey. Pediatric Emerg Care. 2010;26:554–558. doi: 10.1097/PEC.0b013e3181ea718e. [DOI] [PubMed] [Google Scholar]
- 17.Durani Y. The emergency severity index version 4: reliability in pediatric patients. Pediatric Emerg Care. 2009;154:A1109. [PubMed] [Google Scholar]
- 18.Innes GD, Stenstrom R, Grafstein E, Christenson JM. Prospective time study derivation of emergency physician workload predictors. CJEM. 2005;7:299–308. doi: 10.1017/s1481803500014482. [DOI] [PubMed] [Google Scholar]
- 19.Shelton R. The emergency severity index 5-level triage system. Dimens Crit Care Nurs. 2009;28:9–12. doi: 10.1097/01.DCC.0000325106.28851.89. [DOI] [PubMed] [Google Scholar]
- 20.Murray M, Bullard M, Grafstein E CTAS Natioanal Working Group; CEDIS National Working Group. Revisions to the Canadian Emergency Department Triage and Acuity Scale implementation guidelines. CJEM. 2004;6:421–427. [PubMed] [Google Scholar]
- 21.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Mechanism of injury and special consideration criteria still matter: an evaluation of the National Trauma Triage Protocol. J Trauma. 2011;70:38–44. doi: 10.1097/TA.0b013e3182077ea8. [DOI] [PubMed] [Google Scholar]
- 22.Van Veen M, Steyerberg EW, Ruige M, van Meurs AH, Roukema J, van der Lei J, et al. Manchester triage system in pediatric emergency care prospective observational study. BMJ. 2008;337:1501. doi: 10.1136/bmj.a1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warren M. Correlation of the Canadian Pediatric Emergency triage and acuity scale to ED resource utilization. Am J Emerg Med. 2008;26:893–897. doi: 10.1016/j.ajem.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 24.Olofsson P, Gellerstedt M, Carlström ED. Manchester Triage in Sweden -interrater reliability and accuracy. Int Emerg Nur. 2009;17:143–148. doi: 10.1016/j.ienj.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Gravel J, Manzano S, Arsenault M. Safety of a modification of the triage level for febrile children 6 to 36 months old using the Paediatric Canadian Triage and Acuity Scale. CJEM. 2008;10:32–37. doi: 10.1017/s1481803500009982. [DOI] [PubMed] [Google Scholar]
- 26.Hamm JR. How to overcome triage barriers. J Emerg Nurs. 2008;34:241–242. doi: 10.1016/j.jen.2008.02.023. [DOI] [PubMed] [Google Scholar]
- 27.Gonzalez C, Brunstein A. Training for emergencies. J Trauma. 2009;67:S100–105. doi: 10.1097/TA.0b013e3181adc0d5. [DOI] [PubMed] [Google Scholar]


