Abstract
BACKGROUND:
This study aimed to evaluate emergency medicine doctors’ accuracy in predicting the need of film printing in a simulated setting of computed radiography and assess whether this can facilitate optimal patient care.
METHODS:
Cross sectional study was conducted from 20 March 2009 to 3 April 2009 in 1334 patients. After clinical assessment of those patients who needed X-ray examination, doctors in the emergency department would indicate whether film printing was necessary for subsequent patient care in a simulated computed radiography setting. The final discharge plan was then retrieved from each patient record. Accuracy of doctors’ prediction was calculated by comparing the initial request for radiographic film printing and the final need of film. Doctors with different level of emergency medicine experience would also be analyzed and compared.
RESULTS:
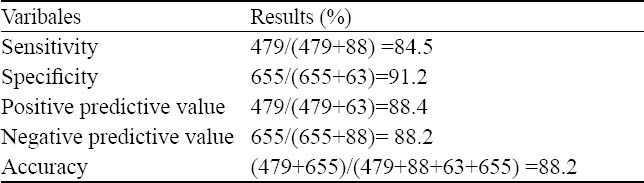
The sensitivity of predicting film printing was 84.5% and the specificity of predicting no film printing was 91.2%. Positive predictive value was 88.4% while negative predictive value was 88.2%. The overall accuracy was 88.2%. The accuracy of doctors stratified into groups of fellows, higher trainees and basic trainees were 85.4%, 90.5% and 88.5% respectively (P=0.073).
CONCLUSIONS:
Our study showed that doctors can reliably predict whether film printing is needed after clinical assessment of patients, before actual image viewing. Advanced indication for film printing at the time of imaging request for selected patients can save time for all parties with minimal wastage.
KEY WORDS: Computed tomography X-ray, Emergencies, Radiographic image enhancement, Forecasting
INTRODUCTION
In 1895, Wilhelm Roentgen, a German professor of experimental physics, discovered X-ray. For more than a hundred years thereafter, radiography is an important diagnostic tool frequently employed by medical professionals because of its low cost, being non-invasive and easy availability. However, conventional screen-film radiography (SFR) has certain shortcomings as follows: (1) limited information that can be captured on
film because of fixed dose latitude; (2) fixed non-linear grey scale response; and (3) limited potential for varying radiation dose to the patient. The contrast of images cannot be changed once they have been processed. Besides, film is expensive and uses hazardous materials for processing. The long term storage and retrieval of film is also difficult and labor intensive.™
In order to overcome these problems, scientists developed new technology in the form of computed or digital radiography (CR or DR). The new technology digitalizes radiographic images so that images can be viewed through electronic screen and the data can be stored in the computer server. When compared with SFR, CR or DR has the advantages of being lower cost, easier access, lower radiation dose and faster speed.[1] It can lead to a reduction in cost in the long run due to lower film cost, reduced requirement for storage space, and lesser staff required to run the imaging and archiving services. The images produced by CR or DR can easily be accessed because they are instantly available for distribution to clinical services without the time and physical effort required to retrieve film packets. A lower radiation dose can produce a comparable image quality because of the use of higher sensitivity plates to produce images with good resolution and sharpness. Last but not the least, it is faster because fewer steps are required in the operation and the use of radiology information system allows patient demographic data to be downloaded automatically into the computer.[2-5]
In order to improve the quality and efficiency of patient care, the radiography service stationed in the Emergency Department (ED) of Kwong Wah Hospital upgraded its system to CR in April 2009. By doing so, all radiographic images produced by the system could be viewed through electronic screen. However, the initial investment was substantial. We had to install high resolution display monitors in all workstations within our ED so that digital images viewed on the screen would be comparable to conventional film.[1,6] Besides, we also needed a Picture Archiving and Communication System (PACS) program to ensure minimal loss of data during transmission. Data would eventually be uploaded to the Clinical Management System (CMS) within the network of Hospital Authority. However, viewing the images via the CMS would suffer some loss in image quality. Filmless radiography within the hospital is our aim. Because of substantial initial investment together with limitations in pre-existing building structures, it will take years for our hospital to function as such. Therefore, we still need to produce hard copies of radiographic film in certain occasions such as for those patients who require admission or transfer, and patients who require referral to chest clinic and trauma clinic.
In order to strike a balance between smooth patient flow and effective use of resource, it would be ideal if doctors could request film printing (for those in need) before patients were sent to X-ray suite. A study was thus planned to find out the accuracy of doctors’ decision on advanced film printing.
METHODS
The research incorporated a cross sectional study. Participants included all doctors working in the ED of Kwong Wah Hospital. The study period was from 20 March 2009 to 3 April 2009 (before the formal implementation of CR). Doctors working in the ED between 8 am to 12 midnight were invited to participate in the study. They were given a record form by designated nursing officer at the start of their shift. On the record form, there was a self explanatory paragraph listing those conditions that required printing of radiographic film. After each patient assessment, the doctor would decide whether radiographic imaging was necessary. For those patients who needed X-rays, the doctor would input the patients’ names and AE numbers onto the record sheet, followed by choosing “yes” or “no” for film printing. The conditions that required hard copy printing included: 1) patients who were managed in the resuscitation room; 2) patients who required admission after clinical assessment; 3) patients who required referral to chest clinic; and 4) patients who required follow-up at special orthopedic clinics such as trauma clinic or Colles’ fracture clinic. The forms were collected after each shift by designated nursing officer in charge.
The record forms collected were then assessed. The attendance records of individual patients were retrieved to find out the final discharge plan so as to determine whether they need a hard copy of film. We could then compare the initial prediction of the doctor with the final discharge plan to evaluate the accuracy of doctors in predicting the need of film printing. We also wanted to know whether doctors’ ED experience would affect the accuracy of prediction. Thus the doctors were stratified into groups of fellows, higher trainees (membership holder) and basic trainees and their accuracies were compared.
RESULTS
A total of 152 record forms were distributed and 121 record forms were completed and returned. Response rate was irrelevant as the record forms were used only as needed. These 121 record forms contained 1334 patients who were sent for radiography. Among these patients, 542 (40.6%) were indicated in advance to print radiographic films while 743 (55.7%) were indicated not to print radiographic films. There were 49 patients (3.7%) whose data could not be processed further because the patient discharged against medical advice, disappeared before formal disposal or the information entered was not clear.
After assessment of the clinical record, there were 567 (42.5%) patients who eventually required radiographic film printing and 718 (53.8%) patients who did not.
We obtained a 2×2 table (Table 1) from these results, which allows us to calculate the sensitivity and specificity of our doctors’ prediction on radiographic film printing (Table 2).
Table 1.
Result of doctors’ prediction vs. final requirement of film printing

Table 2.
Statistical analysis of pooled data
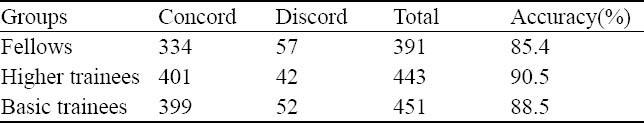
We further stratified the doctors into 3 groups according to their level of ED experience and accuracy was calculated for different groups (Table 3). It was shown that the accuracy for fellows, higher trainees and basic trainees were 85.4%, 90.5% and 88.5% respectively (P=0.073).
Table 3.
Accuracy of doctors’ prediction stratified according to their ED experience
DISCUSSION
The results showed that our doctors had a high accuracy (88.2%) in predicting the necessity of film printing before they actually viewed the radiographic image. The rates of inappropriate film printing (63 patients, 4.7%) and failure to identify those who required film printing (88 patients, 6.6%) were low. The former showed that there would be a low level of wastage of resources and the latter would mean that the disruption in patient flow arising from delayed request for film printing (after image viewing) would also be low. Six hundred and fifty-five patients were saved from printing unnecessary radiographic films through our doctors’ prediction. We could do a cost-reduction calculation from this as well. Within a two-week period, unnecessary radiographic films were saved from printing for 655 (-50%) patients. That was almost 16 000 patients in one year. If we assumed there was only one radiographic film for each patient and each film cost HK$10 (data from senior radiographer, Mr. Apollo Wong of Radiology Department of Kwong Wah Hospital), CR could save at least HK$160 000 per year.
It is irrational to print film for every radiographic image taken via CR. The reason behind is obvious: there will be many unnecessary films produced. On the other hand, we can achieve zero wastage if we only print radiographic films after images are available and discharge plans are finalized by doctors. However, this will create two problems.
Firstly, this will generate another queue of patients waiting for film printing before disposal or admission. The waiting hall of our ED, like EDs in other hospitals of Hong Kong, is relatively small. Therefore, the flow of patients has to be efficient and fast enough so as to avoid overcrowding and chaotic conditions. Once management plan has been made, the subsequent actions e.g. admission into the ward, need to be carried out promptly. We cannot accommodate another group of patients in our ED solely for the waiting of radiographic film printing as the delay in management can be substantial and situation can be chaotic (past experience of one of the authors in the ED of another local hospital, which started CR at the ED lately).
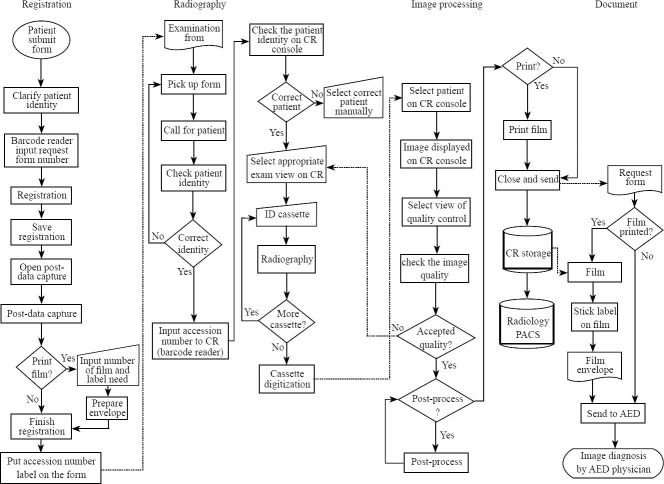
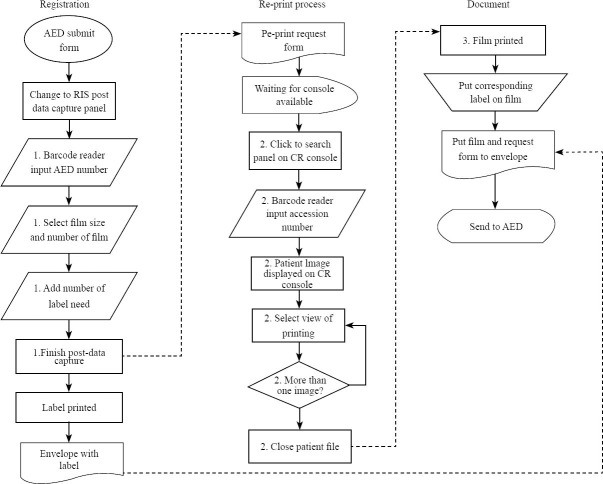
Secondly, this will interrupt the workflow of our radiographer, causing delay in patient flow. We learn from our radiographer colleagues that their workflow will be similar whether they just capture the computed image into the server without printing film or print radiographic films for the patient regardless of final decision plan (Figure 1). However, if film printing request is made after images are viewed by doctors; the workflow of our radiographer will be interrupted: they need to switch the computer away from its work on new examinations to retrieve the images from the database and direct the printing of radiographic films (Figure 2). According to the estimation from our radiographer colleagues, this extra time needed to do the re-print process will take minutes, which can be tremendous if applied to all 567 patients (-45%) who required printing of radiographic films.
Figure 1.
The detailed working flowchart of a computed radiography examination
Figure 2.
The additional work-steps required when film printing is requested after image is available to emergency physicians
Therefore, we have to find a cost effective way of deciding on film-printing. We should neither print film for every patient without using our judgment; nor should we decide only after images are available to doctors. The present study showed that advanced request of radiographic film printing by doctors can be a cost effective measure which can facilitate patient care and smooth patient flow at the expense of a small potential “wastage”. Although further calculation of accuracies showed varying results, with higher trainees attaining a slightly higher accuracy, the difference was not statistically significant. Based on our findings, the departmental administration agreed on our suggestion and prepared chops labeled “PRINT FILM” to direct the radiographers to capture the computed image and print the film in one goal (in selected patients) so as to save the time for all parties. For indeterminate cases, the decision of film printing can be made after viewing the actual image and consolidation of the disposal plan.
There were some aspects that might affect our study results. Firstly, doctors were informed of the study in advance. Although they were informed that the accuracy calculation would not be done for individuals, this might affect their willingness to participate in the decision on film printing request. Secondly, not all patients who were sent for radiographic examination were entered into the record form. This might be due to omission by the doctors to put down the patient particulars as a result of busy work, or they could not decide at that juncture. Thirdly, there was a minority of data that could not be processed because of wrong labeling, discharged against medical advice, or disappeared before formal disposal. However, even if we assumed that all these cases were incorrectly predicted, the accuracy was still as high as about 85.0%.
Our study showed that doctors can reliably predict whether film printing is needed after clinical assessment of patients, before actual image viewing. Advanced indication for film printing at the time of imaging request for selected patients can save time for all parties with minimal wastage. Certainly, filmless networking with lossless transmission within the healthcare corporate is our future direction.
Acknowledgement
The researchers would like to thank Mr. Apollo Wong (Senior Radiographer) and Mr. Lyman Lee Ho Yin (Radiographer II) from the Radiology Department of Kwong Wah Hospital for their valuable input to this study.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there are not any financial interests or potential conflicts of interest relating to the manuscript.
Contributors: The manuscript has been read and approved by Yang SM and Lo CM.
REFERENCES
- 1.Bansal GJ. Digital radiography. A comparison with modern conventional imaging. Postgrad Med J. 2006;82:425–428. doi: 10.1136/pgmj.2005.038448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.May GA, Deer DD, Dackiewicz D. Impact of digital radiography on clinical workflow. J Digit Imaging. 2000;13:76–78. doi: 10.1007/BF03167630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andriole KP. Productivity and cost assessment of computed radiography, digital radiography, and screen-film for outpatient chest examinations. J Digit Imaging. 2002;15:161–169. doi: 10.1007/s10278-002-0026-3. Epub 2003 Jan 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reiner BI, Siegel EL. Technologists’ productivity when using PACS: comparison of film-based versus filmless radiography. AJR Am J Roentgenol. 2002;179:33–37. doi: 10.2214/ajr.179.1.1790033. [DOI] [PubMed] [Google Scholar]
- 5.Mariani C, Tronchi A, Oncini L, Pirani O, Murri R. Analysis of the X-ray work flow in two diagnostic imaging departments with and without a RIS/PACS system. J Digit Imaging. 2006;19(Suppl 1):18–28. doi: 10.1007/s10278-006-0858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aldrich JE, Rutledge JD. Assessment of PACS display systems. J Digit Imaging. 2005;18:287–295. doi: 10.1007/s10278-005-6974-7. [DOI] [PMC free article] [PubMed] [Google Scholar]