Abstract
BACKGROUND:
Previous studies depict low cardiac event and mortality rates in patients with angiographically normal coronary arteries. These studies, however, are limited by small sample sizes, short follow-up intervals, and selection biases. This study was undertaken to determine the natural five-year course of a diverse cohort of subjects with documented normal coronary arteries with respect to coronary heart disease development, revascularization need, and all-cause mortality.
METHODS:
Consecutive adult patients with angiographically normal coronary arteries were followed up for 5 years through medical record review. Patients with any degree of angiographic abnormality, including minimal luminal irregularity or non-critical stenosis, were excluded. Patients were not excluded based on age, co-morbidities (except cardiac transplant and structural heart disease), indication for angiogram, or initial hospitalization status.
RESULTS:
Normal coronary arteries were found in 182 (31.3%) of 582 patients; 129 met all inclusion criteria. The mean age was (49.1±12.5) years; 47 (36.7%) were male and 75 (58.1%) were caucasian. The most common indication for angiography was cumulative risk factors (60.5%). Within 5 years of a normal angiogram, 13 of 129 patients died (10.1%; 95 CI 5.7%-16.9%). Six (40%; 95 CI 19.8% to 64.3%) of 15 patients undergoing repeat angiogram within five years developed new coronary heart disease, with one requiring revascularization. Of traditional risk factors of coronary heart disease, only diabetes was associated with a higher risk of death.
CONCLUSION:
The natural five-year course of a diverse cohort of patients with documented normal coronary arteries suggests that there is significant risk for death and development of coronary heart disease.
KEY WORDS: Angiography, Coronary disease, Mortality, Prognosis
INTRODUCTION
Heart disease is the leading cause of death in the United States, and coronary angiography is the standard for detection of critical disease.[1,2] Many patients undergoing angiography are found to have normal coronary arteries.[3,4] Recently, however, the accuracy of angiography has been questioned. Investigations with intra-vascular ultrasound show high-risk lesions in many vessels with no apparent disease seen via standard angiography; these lesions are at risk of rupture and acute thrombus formation despite negligible luminal stenosis.[5,6] False-negative angiograms could lead to under-treatment of modifiable risk factors or failure to protect patients with coronary heart disease (CHD) from life-threatening cardiac events.
Emergency physicians frequently use reports of prior angiographic findings to risk-stratify patients complaining of chest pain or anginal equivalents because it is thought that angiograms provide important prognostic information. Previous studies suggest that patients with documented non-critical lesions on angiogram have progression of disease and higher mortality, while those with normal angiograms reportedly have excellent outcomes.[7-25] Unfortunately, selection bias, brief follow-up periods, and small sample sizes prevent the generalizability of these earlier findings.
This study was undertaken to track the development of coronary heart disease, need for revascularization, and all-cause mortality over 5 years in a diverse cohort of patients with documented normal coronary arteries. We hypothesized that outcomes in this broader population would be worse than those seen in previously selected study populations.
METHODS
Study design
This was a retrospective chart review of adult patients found to have normal coronary arteries during angiogram. Normal was defined, a priori, as absence of any angiographic abnormality, including minimal luminal irregularity and non-critical stenosis.
Setting
This study was conducted at an urban, academic tertiary referral center with diagnostic, interventional, and emergency cardiology services. Approximately 1400 coronary angiograms are performed annually. The study was approved by the local Institutional Review Board.
Selection of participants
Consecutive subjects were selected from among every patient undergoing cardiac catheterization between January and May, 2009. Reports of angiographic findings were reviewed to identify those with normal coronary arteries. Subjects were excluded if any abnormality, including minimal luminal irregularity or non-critical stenosis, was reported in the description of angiographic findings. Subjects who underwent angiogram for valvular heart disease or for pre- or post-cardiac transplant surveillance were also excluded. Subjects were included if they were older than 18 years and did not die during their initial hospitalization. Subjects were not excluded based on indication for angiogram (abnormal rest or stress testing, risk factors), age, co-morbidities, or initial hospitalization status (inpatient, transfer, outpatient).
Data collection and monitoring
Data were extracted to a standardized case report form by a study physician. The natural course of those with angiographically normal coronary arteries was followed through medical record review for 5 years after the date of the initial angiogram. Subjects were tracked through 2 electronic medical records systems containing documents from a six-hospital regional health system and hospital-based clinic visits. The Social Security Death Master File was searched for all subjects with unclear survival at 5 years; this query was performed at least 12 months after the end of the study period. In addition to the medical record review, records of all repeat angiogram-related visits for included subjects were reviewed to estimate the proportion developing coronary heart disease during the 5-year period.
Data elements were predefined according to standardized reporting guidelines for studies of chest pain patients.[26] While this study does not focus primarily on chest pain, these guidelines provide a framework for contextualizing the study sample and extrapolating these findings to chest pain patients with prior normal angiograms. Records from the index visit were used to obtain subject demographics, coronary heart disease risk factors, cardiovascular medication use, indication for angiography, symptoms at admission, initial electrocardiogram findings and ejection fraction.
Outcome measures
Outcomes after the index visit were defined as development of coronary heart disease based on repeat angiography, need for revascularization, and all-cause mortality. For each event, the type of event, date of event, and mortality status were abstracted. The full five year event history was obtained for patients surviving to 5 years; otherwise, observations ended at death. A repeat angiogram was defined as normal when there was no angiographic abnormality, whereas findings of minimal luminal irregularity, non-significant stenosis, or other lesions were considered abnormal.
Primary data analysis
Data are described using means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. Median survival, and 95% confidence intervals for survival, was estimated from Kaplan-Meier survival curves. Cox's proportional hazards model was used to estimate relative risk for death or adverse events. The data were managed in Microsoft Excel (Microsoft Corporation, Redmond, WA) and analyzed using SPSS v 15.0 (SPSS Inc. Chicago, IL).
RESULTS
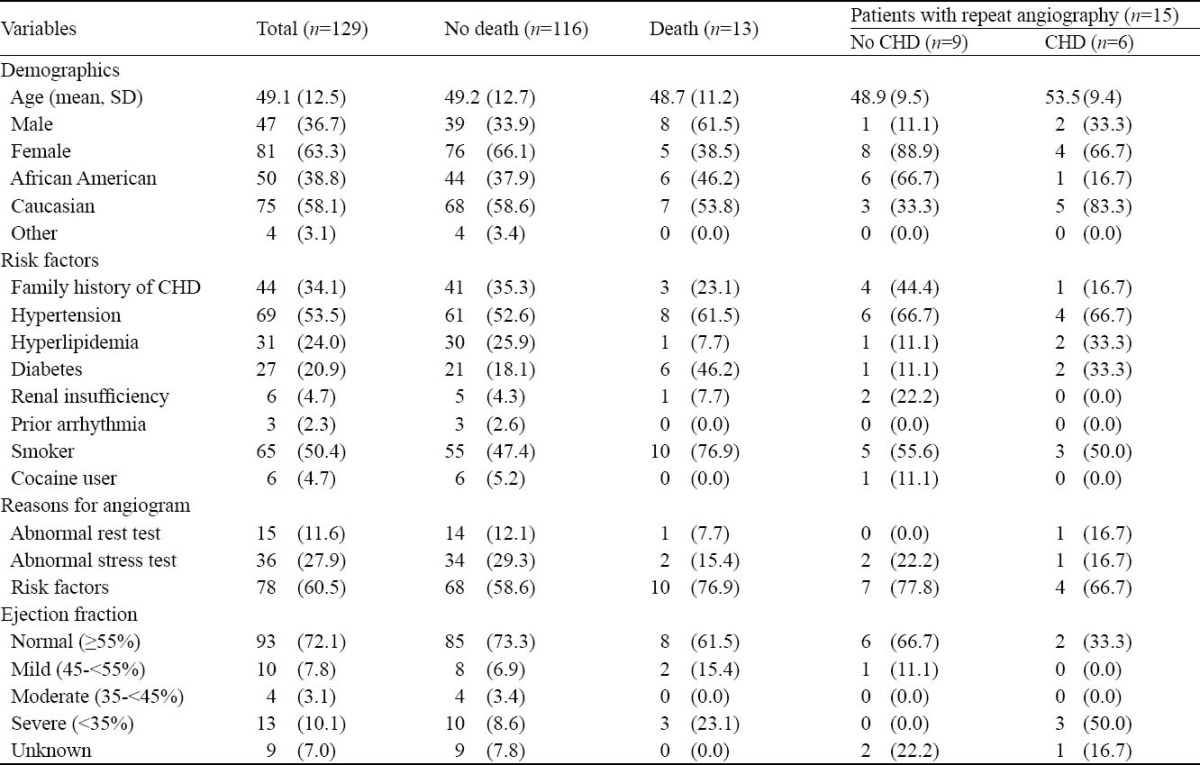
Of 582 patients undergoing coronary angiography without intervention between January and May 2009, 182 (31%) were found to be normal. After excluding angiograms performed for pre-transplant evaluation, post-cardiac transplant surveillance, and structural heart disease, there were 129 patients with an indication eligible for inclusion. Patient demographics, risk factors, and indications for initial normal angiogram are shown in Table 1.
Table 1.
Population characteristics (no.%)
Main results
Complete 5-year medical records were available for 70 of the 129 patients. Survival for the remaining 59 patients was determined by SSDI review.
Overall, there were 19 adverse events among the 129 patients. Survival and event-free survival are shown in Figure 1. Observed all-cause mortality was 10.1% (13/129, 95CI 5.7% to 16.9%). Among those who died, median survival was 106 weeks (0 to 246 weeks). Causes of death were cardiac in 3 patients, multi-organ system failure in 2, ischemic stroke in 1, malignancy in 1, and unknown in 6 (determined by SSDI review).
There were 15 patients who underwent repeat angiography. New angiographic lesions were found in 6 (40.0%; 95CI 19.8% to 64.3%). Patients developed coronary heart disease between 2 and 5 years after initial angiogram. One patient underwent percutaneous coronary intervention. Another patient, with normal initial angiogram who developed coronary heart disease on repeat angiogram but did not receive intervention, was resuscitated after an out-of-hospital cardiac arrest and survived through the 5-year observation period.
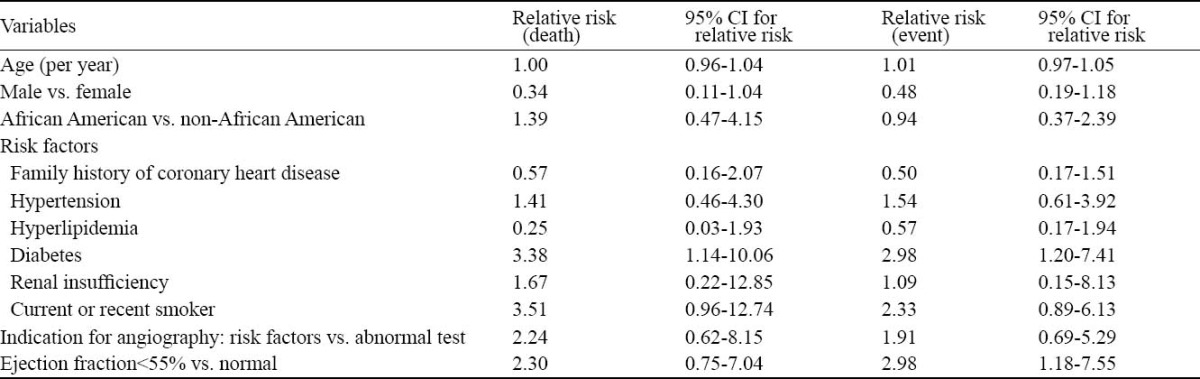
Univariable analysis (Table 2) showed that diabetes was associated with increased risk of death. Diabetes and an ejection fraction <55% were associated with increased risk of any event. The composite TIMI risk score and other individual traditional risk factors of coronary heart disease (smoking, hypertension, hyperlipidemia, family history) were not associated with an increased risk of death or event.[27]
Table 2.
Relative risk of death or event for demographic, risk factor, and angiogram data
DISCUSSION
Coronary angiography offers clinicians both diagnostic and therapeutic opportunities. Emergency physicians frequently rely on previous angiogram results to risk-stratify patients with complaints of angina or angina-equivalents. While angiography is often considered to be the standard for coronary heart disease assessment, it is not perfect. Many non-diseased segments on conventional angiogram are found to have disease on intra-vascular ultrasound.[5’6]
Compensatory enlargement may allow the left main coronary artery to appear normal, even in presence of disease, because the luminal area does not decrease until there is more than 40% obstruction.[28]
Documentation of coronary heart disease encourages more aggressive medical therapies for secondary prevention, even if direct intervention is not required.[29] Additional non-cardiac evaluation and treatment is often recommended for patients with normal angiograms.[30] Although few of these subjects required percutaneous intervention, the observed development of coronary heart disease might have been mitigated with risk-factor modification and initiation of drug therapies to prevent advancement of disease.
Traditionally, patients with a history of a prior normal angiogram are forecast to be at low risk for cardiovascular morbidity and mortality, but the present study suggests otherwise. Previous studies have been inconsistent in findings of disease progression, with some showing disease development and others showing continued normal findings.[7,8,16,18,21,22,31-34] These studies are limited by small sample sizes (3-27 subjects) and are focused on young patients without significant co-morbidities who are unlikely to develop disease during short follow-up intervals.
Our outcomes are likely different due to our longer follow-up interval and lack of exclusion of patients with pre-existing diabetes mellitus, hypertension, or cardiomyopathy. Indeed, such subjects were specifically included to provide a more diverse comparison cohort to allow emergency physicians to interpret previous angiographic findings in patients with medical co-morbidities.
The mean TIMI risk score for the group was 1.6 (range 0-4); when applied to patients suffering from unstable angina or non-ST segment elevation myocardial infarction (a much higher risk group than this study population), this score predicts a 5%-8% chance of death, myocardial infarction, or need for revascularization within two weeks.[27] The observed 10.1% 5-year mortality and considerable rate of coronary heart disease development suggest that these angiographically normal subjects are at higher risk than the previously reported. Univariable analysis indicated that no traditional risk factor besides diabetes was predictive of death or event. Interestingly, however, a prior normal angiogram is the leading indicator of a high-risk adverse event, despite the traditional thought that this would identify a low-risk population.
Limitations
This study is limited by its reliance on the medical record for data elements. However, the main outcome variables are dichotomous, explicitly defined, and not subject to interpretation bias. We conservatively report adverse events as what is known to be true; subjects who did not undergo repeat angiography are presumed to have remained normal, and subjects without known death are presumed to have survived for at least 5 years. There is the possibility of missed events, although the use of shared medical record systems allowed non-site visits to be captured and missed events would have only served to increase the power of our results.
Original angiographic images were not reviewed by the study physicians. It is possible that some subjects reported as normal had minimal luminal irregularities on the initial angiogram. Such false negative patients may bias the outcome towards a higher mortality. However, in clinical practice, only the study's report, not the actual angiographic images, is typically available to emergency physicians to guide therapy and provide risk-stratification information.
All subjects underwent angiography at a tertiary referral center caring for the region's indigent patients. As well as possible differences between the population served at the study hospital and those at community hospitals, it is possible that more acutely and chronically ill patients were studied than at other hospitals. However, only patients with initially normal angiograms (theoretically those at the lowest risk) were followed up. The overall normal rate was 31.3% (182/582), which is comparable to past studies.[13]
Six of the subjects who did not survive were identified as dead from review of the Social Security Death Master File; therefore, specific causes of death cannot be determined. All-cause mortality, including large numbers of unknown causes of death, have been used as end-points in previous prognostic studies.[13, 18, 20, 21] Based on the finding of new coronary heart disease in the subgroup that underwent repeat angiography it is possible, but not certain, that coronary heart disease contributed to these deaths.
In conclusion, there is significant risk for death and coronary heart disease development during the natural 5-year course in a diverse cohort of subjects with normal coronary arteries. While the length of time for which a normal angiogram can be considered valid remains unclear, a patient cannot be considered to be at low cardiac risk based on past angiographic results alone.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there are not any financial interests or potential conflicts of interest relating to the manuscript.
Contributors: McMullan J Tproposed and wrote the study. All authors contributed to the intellectual content and approved the final version.
REFERENCES
- 1.Miniño AM, Heron MP, Murphy SL, Kochanek KD. Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep. 2007;55:1–119. [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 3.Cannon RO, 3rd, Quyyumi AA, Mincemoyer R, Stine AM, Gracely RH, Smith WB, et al. Imipramine in patients with chest pain despite normal coronary angiograms. NEJM. 1994;330:1411–1417. doi: 10.1056/NEJM199405193302003. [DOI] [PubMed] [Google Scholar]
- 4.Phibbs B, Fleming T, Ewy GA, Butman S, Ambrose J, Gorlin R, et al. Frequency of normal coronary arteriograms in three academic medical centers and one community hospital. Am J Cardiol. 1988;62:472–474. doi: 10.1016/0002-9149(88)90982-4. [DOI] [PubMed] [Google Scholar]
- 5.5Mintz GS, Painter JA, Pichard AD, Kent KM, Satler LF, Popma JJ, et al. Artherosclerosis in angiographically “normal” coronary artery reference segments: an intravascular ultrasound study with clinical correlations. J Am Coll Cardiol. 1995;25:1479–1485. doi: 10.1016/0735-1097(95)00088-l. [DOI] [PubMed] [Google Scholar]
- 6.Tuzcu EM, De Franco AC, Goormastic M, Hobbs RE, Rincon G, Bott-Silverman C, et al. Dichotomous pattern of coronary atherosclerosis 1 to 9 years after transplantation: insights from systematic intravascular ultrasound imaging. J Am Coll Cardiol. 1996;27:839–846. doi: 10.1016/0735-1097(95)00564-1. [DOI] [PubMed] [Google Scholar]
- 7.Haft JI, Bachik M. Progression of coronary artery disease in patients with chest pain and normal or intraluminal disease on arteriography. Am Heart J. 1984;107:35–39. doi: 10.1016/0002-8703(84)90130-3. [DOI] [PubMed] [Google Scholar]
- 8.Isner JM, Salem DN, Banas JS, Jr, Levine HJ. Long-term clinical course of patients with normal coronary arteriography: follow-up study of 121 patients with normal or nearly normal coronary arteriograms. Am Heart J. 1981;102:645–653. doi: 10.1016/0002-8703(81)90088-0. [DOI] [PubMed] [Google Scholar]
- 9.Lichtlen PR, Nikutta P, Jost S, Deckers J, Wiese B, Rafflenbeul W. Anatomical progression of coronary artery disease in humans as seen by prospective, repeated, quantitated coronary angiography: relation to clinical events and risk factors. Circulation. 1992;86:828–838. doi: 10.1161/01.cir.86.3.828. [DOI] [PubMed] [Google Scholar]
- 10.Crenshaw JH, el-Zeky F, Vander Zwaag R, Sullivan JM, Ramanathan KB, Mirvis DM. The effect of noncritical coronary artery disease on long-term survival. Am J Med Sci. 1995;310:7–13. doi: 10.1097/00000441-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Halcox JP, Schenke WH, Zalos G, Mincemoyer R, Prasad A, Waclawiw MA, et al. Prognostic value of coronary vascular endothelial dysfunction. Circulation. 2002;106:653–658. doi: 10.1161/01.cir.0000025404.78001.d8. [DOI] [PubMed] [Google Scholar]
- 12.Kemp HG, Kronmal RA, Vlietstra RE, Frye RL. Seven year survival of patients ith normal or near normal coronary arteriograms: a CASS Registry study. J Am Coll Cardiol. 1986;7:479–483. doi: 10.1016/s0735-1097(86)80456-9. [DOI] [PubMed] [Google Scholar]
- 13.Papanicolaou MN, Califf RM, Hlatky MA, McKinnis RA, Harrell FE, Jr, Mark DB, et al. Prognostic implications of angiographicaly normal and insignificantly narrowed coronary arteries. Am J Cardiol. 1986;58:1181–1187. doi: 10.1016/0002-9149(86)90378-4. [DOI] [PubMed] [Google Scholar]
- 14.Albertsson P, Emanuelsson H, Karlsson T, Lamm C, Sandén W, Lagerberg G, et al. Morbidity and use of medical resources in patients with chest pain and normal or near-normal coronary arteries. Am J Cardiol. 1997;79:299–304. doi: 10.1016/s0002-9149(96)00751-5. [DOI] [PubMed] [Google Scholar]
- 15.Ammann P, Marschall S, Kraus M, Schmid L, Angehrn W, Krapf R, et al. Characteristics and prognosis of myocardial infarction in patients with normal coronary arteries. Chest. 2000;117:333–338. doi: 10.1378/chest.117.2.333. [DOI] [PubMed] [Google Scholar]
- 16.Bemiller CR, Pepine CJ, Rogers AK. Long-term observations in patients with angina and normal coronary angiograms. Circulation. 1973;47:36–43. doi: 10.1161/01.cir.47.1.36. [DOI] [PubMed] [Google Scholar]
- 17.Da Costa A, Isaaz K, Faure E, Mourot S, Cerisier A, Lamaud M. Clinical characteristics, aetiological factors and long-term prognosis of myocardial infarction with an absolutely normal coronary angiogram: a 3-year follow-up study of 91 patients. Eur Heart J. 2001;22:1459–1465. doi: 10.1053/euhj.2000.2553. [DOI] [PubMed] [Google Scholar]
- 18.Hirota Y, Ohnaka H, Tsuji R, Ishii K, Kita Y, Suwa M, et al. Excellent prognosis of Japanese patients with chest pain and normal or nearly normal coronart arteries. Jpn Circ J. 1994;58:43–48. doi: 10.1253/jcj.58.43. [DOI] [PubMed] [Google Scholar]
- 19.Kaski JC, Rosano GM, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wilson PA. Cardiac Syndrome X: clinical characteristics and left ventricular function-long-term follow-up study. J Am Coll Cardiol. 1995;25:807–814. doi: 10.1016/0735-1097(94)00507-M. [DOI] [PubMed] [Google Scholar]
- 20.Kemp HG, Jr, Vokonas PS, Cohn PF, Gorlin R. The anginal syndrome associated with normal coronary arteriograms. Am J Med. 1973;54:735–742. doi: 10.1016/0002-9343(73)90060-0. [DOI] [PubMed] [Google Scholar]
- 21.Lichtlen PR, Bargheer K, Wenzlaff P. Long-term prognosis of patients with anginalike chest pain and normal coronary angiographic findings. J Am Coll Cardiol. 1995;25:1013–1018. doi: 10.1016/0735-1097(94)00519-v. [DOI] [PubMed] [Google Scholar]
- 22.Opherk D, Schuler G, Wetterauer K, Manthey J, Schwarz F, Kübler W. Four-year follow-up study in patients with angina pectoris and normal coronary arteriograms. Circulation. 1989;80:1610–1616. doi: 10.1161/01.cir.80.6.1610. [DOI] [PubMed] [Google Scholar]
- 23.Romeo F, Rosano GM, Martuscelli E, Lombardo L. Valente Long-term follow-up of patients initially diagnosed with Syndrome X. Am J Cardiol. 1993;71:669–673. doi: 10.1016/0002-9149(93)91008-6. [DOI] [PubMed] [Google Scholar]
- 24.Sharaf BL, Pepine CJ, Kerensky RA, Reis SE, Reichek N, Rogers WJ, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation[WISE] Study Angiographic Core Laboratory) Am J Cardiol. 2001;87:937–941. doi: 10.1016/s0002-9149(01)01424-2. [DOI] [PubMed] [Google Scholar]
- 25.Waxler EB, Kimbiris D, Dreifus LS. The fate of women with normal coronary arteriograms and chest pain resembling angina pectoris. Am J Cardiol. 1971;28:25–32. doi: 10.1016/0002-9149(71)90030-0. [DOI] [PubMed] [Google Scholar]
- 26.Hollander J, Blomkalns A, Brogan G, Diercks DB, Field JM, Garvey JL, et al. Standardized reporting guidelines for studies evaluating risk stratification of emergency department patients with potential acute coronary syndromes. Ann Emerg Med. 2004;44:589–596. doi: 10.1016/S0196064404012806. [DOI] [PubMed] [Google Scholar]
- 27.Hollander JE, Blomkalns AL, Brogan GX, Diercks DB, Field JM, Garvey JL, et al. The TIMI risk score for unstable angina/ non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 28.Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ. Compensatory enlargement of human atherosclerotic coronary arteries. NEJM. 1987;316:1371–1375. doi: 10.1056/NEJM198705283162204. [DOI] [PubMed] [Google Scholar]
- 29.Smith SC, Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC Guidelines for Secondary Prevention for Patients With Coronary and Other Atherosclerotic Vascular Disease: 2006 Update: Endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363–2372. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz L, Bourassa MG. Evaluation of patients with chest pain and normal coronary angiograms[Review] Arch Intern Med. 2001;161:1825–1833. doi: 10.1001/archinte.161.15.1825. [DOI] [PubMed] [Google Scholar]
- 31.Cox ID, Schwartzman RA, Atienza F, Brown SJ, Kaski JC. Angiographic progression in patients with angina pectoris and normal or near normal coronary angiograms who are restudied due to unstable symptoms. Eur Heart J. 1998;19:1027–1033. doi: 10.1053/euhj.1998.0870. [DOI] [PubMed] [Google Scholar]
- 32.Pitts WR, Lange RA, Cigarroa JE, Hillis LD. Repeat coronary angiography in patients with chest pain and previously normal coronary angiogram. Am J Cardiol. 1997;80:1086–1087. doi: 10.1016/s0002-9149(97)00610-3. [DOI] [PubMed] [Google Scholar]
- 33.Kimbiris D, Lavine P, Van Den Broek H, Najmi M, Likoff W. Devolutionary pattern of coronary atherosclerosis in patients with angina pectoris. Am J Cardiol. 1974;33:7–11. doi: 10.1016/0002-9149(74)90732-2. [DOI] [PubMed] [Google Scholar]
- 34.Marchandise B, Bourassa MG, Chaitman BR, Lesperance J. Angiographic evaluation of the natural history of normal coronary arteries and mild coronary atherosclerosis. Am J Cardiol. 1978;41:216–220. doi: 10.1016/0002-9149(78)90159-5. [DOI] [PubMed] [Google Scholar]


