Abstract
BACKGROUND:
The role of Inter-facility transport (IFT) of patients is an emerging specialty requiring service reorganization, diversion of major trauma to trauma center. This study aimed to determine the patients who are more prone to en route adverse event during the period of 22:00 to 07:00, based on critical in-patient needs provided by the Emergency Department (ED) nursing staff at Alice Ho Miu Ling Nethersole Hospital (AHNH).
METHODS:
This study included all 22:00 to 07:00 IFTs accompanied by ED nurses at AHNH for a period of 28 months from August 2006 until December 2008. The transports were reviewed for: (1) age, (2) gender, (3) transport configuration, (4) clinical category, and (5) physiological instability before transport.
RESULTS:
A total of 79 patients were transported during the 22:00 to 07:00 timeframe within the study period. The types of patients were mainly neurosurgical emergencies (n=32; 40.5%), surgical emergencies (n=28; 35.4%), and upper gastrointestinal bleeding (UGIB) (n=11; 13.9%). En route adverse events were encountered by the accompanying nurses in 16 transports (20.3%) with a higher incidence of adverse events during transport of surgical emergencies, UGIB and patients who were physiological unstable before transport (P< 0.05).
CONCLUSION:
A specialized transport team from the ED can assist other clinical departments by providing expert care during IFT. In spite of the high quality of care, adverse events do commonly occur.
KEY WORDS: Inter-facility transport, Specialized transport team, Hong Kong
INTRODUCTION
Inter-facility transport (IFT), in general, is equivalent to secondary transport that no longer a minor part of emergency medical services and solely the transport of critically ill patients. Transport to or from the emergency department (ED) is a frequent occurrence.[1-4] IFT service will play a vital and emerging role in a centralized model of acute specialist care and its role is emerging parallel to the past and future healthcare development including centre of excellence, primary trauma diversion and doctor work-hour reform.
IFT service itself is not without risks and is known to be a potentially hazardous process that exposes patients to adverse events, morbidity or even mortality especially when it is prepared inadequately.[1,5] The presumed end result of providing IFT service is to receive a high quality of care, superior to that provided by the staff transporting patients in an impromptu and ad hoc manner as adverse events can easily occur en route.[6-9]
The aim of this study is to stratify risk of ED in providing nighttime IFT service for other in-patient departments in a local hospital in Hong Kong and to identify risk factors associated with adverse event during transport.
METHODS
Alice Ho Miu Ling Nethersole Hospital (AHNH) is located in Tai Po which is lack of emergency surgical, obstetrical and gastrointestinal endoscopies services. Since August 2006, trained nurses in AHNH ED were responsible to provide nighttime (22:00 to 07:00) IFT services when requested by other in-patient departments with the supplement of standardized IFT guidelines, documentation mean, transport kits, and monitoring devices.
Data collection
This was a prospective study with recording of nighttime IFT accompanied by a specialized transport team (STT) dispatched by AHNH ED from August 2006 for 28 consecutive months till December 2008. ED and ambulance records within the study period were reviewed for patients who required this service and accompanied by a trained registered nurse plus paramedics as well as a doctor if advanced expertise was necessary. Clinical progress en route was collected from IFT forms (Figure) that are specifically designed for the STT to perform legible en route documentation.
Figure 1.
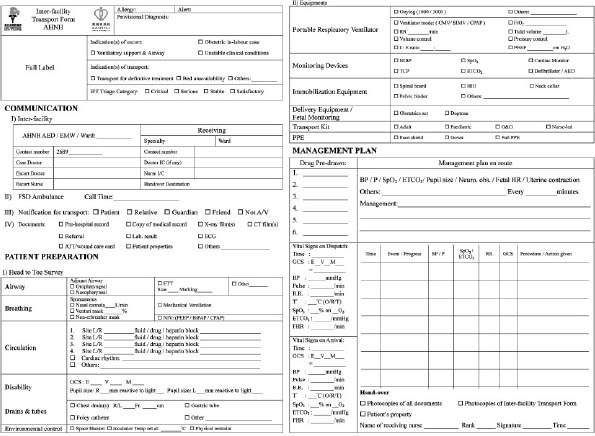
Inter-facility transport (IFT) form.
Data analysis
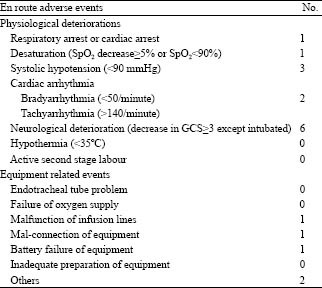
Transports were reviewed for: age, gender, transport configuration, clinical category, and physiological instability before dispatch. En route adverse events including physiological deterioration and equipment related events were defined (Table 1). Descriptive statistics was used to demonstrate information concerning the demography, clinical categorization and physiological status of patients. Non-parametric tests were employed to determine any association between specific factors with occurrence of adverse events en route.
Table 1.
Definition of en route adverse events
RESULTS
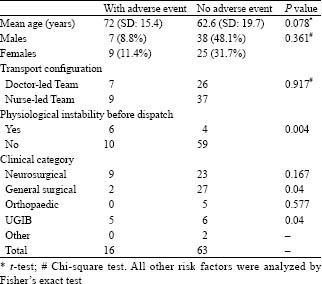
A total of 79 patients were transported during nighttime (Table 2). Their ages ranged from 3 to 96 years, with more male patients (n=45; 57%) being transported than female ones (n=34; 43%). IFT services were requested in the majority of them due to neurosurgical emergencies (n=32; 40.5%), surgical emergencies (n=28; 35.4%), UGIB (n=11; 13.9%), and orthopedic emergencies (n=5; 6.3%) for definitive care in tertiary centers. Forty-six transports (58.2%) were accompanied by nurse-led team whereas another 33 transports (41.8%) were by doctor-led team. Before dispatch, 8 patients were known to have physiological instability. En route adverse events were recognized by the STT in 16 transports (20.3%). The factors we analyzed in this study showed the presence of associations with adverse events en route on patients with surgical emergencies, UGIB and physiological instability before dispatch (P<0.05) (Table 2).
Table 2.
Analysis of risk factors for en route adverse events
DISCUSSION
The whole continuum of an IFT could be divided into 3 stages–pre-transport, during transport (en route) and post-transport. The pre-transport preparation composes of communication, documentation, equipment support, pharmaceutical preparation, risk assessment and determination of transport configuration which is by far the most referrer-dependent stage and prone to problem rising. As for en route management, its quality depends not only on the skill of accompanying staff but also their ability to anticipate and prevent possible deterioration.[10-15]
A recent trend within the emergency medicine era is to make use of risk assessment tools such as guidelines or scoring systems to govern safe transportation of patients with focuses on the pre-transport preparation.[5-6] However, there are no widely accepted standards in place to stratify risk when embarking on IFT.[8] In addition, there is evidence that the provision of a dedicated trained STT could offer a more consistent and quality standard of en route management in view of greater familiarity with specialized transport equipment, better capability to identify common physiological derangements during transport and even a shorter patient preparation time which were widely recommended in various studies.[16-20] However, we have not proven whether a STT would improve the quality of transports in our catchments area.
Although this nighttime IFT service was well established and risk-assessed, this study still demonstrates an occurrence of en route adverse events in around 20% of all STT accompanied transports. These “low” risk deteriorations though contributed no mortality or significant morbidity during transport but were potentially to do so. It is not surprisingly that en route adverse events were more likely to occur in IFT of patients with physiological instability prior to transport but were also more prone to occur during IFT of patients with surgical emergencies and UGIB. This stresses on the significance of promulgating a guideline target on IFT for risk stratification priory with particular emphases on clinical category and pre-transport physiological parameters. Moreover, the guideline needs to be regularly updated and evidence-based.
However, risk stratification of IFT and subsequent decision on transport configuration depend not only objectively on clinical factors, but also numbers of other factors such as availability of staff, level of training and expertise of the staff and distance of transport.[21] These considerations need to be balanced with issue of ED operation as well as staff safety and in general demand that a senior emergency physician is available for service coordination.
This study is designed to eliminate recall bias by its prospective collection of relevant data but on the other hand limited by its dependence on accurate documentation that hindered by lost and illegible medical records as well as inaccurate provisional diagnoses.
In conclusion, STT from a clinical department can help other clinical departments to accomplish safe IFT, and adverse events commonly occur despite it is performed by a dedicated team. Special attention is worth to be paid on transport of patients with surgical emergencies and UGIB.
ACKNOWLEDGEMENTS
The researchers thank all the staff of Emergency Department and Department of Medicine of Alice Ho Miu Ling Nethersole Hospital for their contribution to this study. We are also grateful for the support from members of Inter-facility Critical Care Transport Medicine (ICCTM) team.
Footnotes
Funding: None
Ethical approval: The study was approved by Clinical Research Ethical Committee, New Territories East Cluster-Chinese University of Hong Kong.
Competing interest: None.
Contributors: Larry Lee proposed the study and wrote the first draft. All authors contributed to the design and interpretation of the study and to the further draft.
REFERENCES
- 1.Crandon IW, Harding HE, Williams EW, Cawich SO. Inter-hospital transfer of trauma patients in a developing country: A prospective descriptive study. Int J Surg. 2008;6:387–391. doi: 10.1016/j.ijsu.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Ramnarayan P. Measuring the performance of an interhospital transport service. Arch Dis Child. 2009 doi: 10.1136/adc.2008.147314. [DOI] [PubMed] [Google Scholar]
- 3.Tan TK. Interhospital and intrahospital transfer of the critically ill patient. Singapore Med J. 1997;38:244–248. [PubMed] [Google Scholar]
- 4.Emergency Department, Alice Ho Miu Ling Nethersole Hospital; Inter-facility & Critical Care Transport Medicine (ICCTM) Team, Quarterly Audits. [Google Scholar]
- 5.Guidelines for the transfer of critically ill patients. Guideline Committee of the American College of Critical Care Medicine, Society of Critical Care Medicine and American Association of Critical-Care Nurses Transfer Guidelines Task Force. Crit Care Med. 1993;21:931–937. [PubMed] [Google Scholar]
- 6.Second edition, Sept 2008. ICCTM Team, Alice Ho Miu Ling Nethersole and Pok Oi Hospitals; Inter-facility Transport Triage Guideline. ISBN 978-962-8741-10-6. [Google Scholar]
- 7.Lim MT, Ratnavel N. A prospective review of adverse events during interhospital transfers of neonates by a dedicated neonatal transfer service. Pediatr Crit Care Med. 2008;9:289–293. doi: 10.1097/PCC.0b013e318172dbfd. [DOI] [PubMed] [Google Scholar]
- 8.Lee LL, Yeung KL, Lo WY, Lau YS, Tang SY, Chan JT. Evaluation of a simplified therapeutic intervention scoring system (TISS-28) and the modified early warning score (MEWS) in predicting physiological deterioration during inter-facility transport. Resuscitation. 2008;76:47–51. doi: 10.1016/j.resuscitation.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Warren J, Fromme RE, Orr RA, Rotello LC, Horst HM. Guidelines for inter-and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–262. doi: 10.1097/01.CCM.0000104917.39204.0A. [DOI] [PubMed] [Google Scholar]
- 10.Craig SS. Challenges in arranging interhospital transfers from a small regional hospital: an observational study. Emerg Med Australas. 2005;17:124–131. doi: 10.1111/j.1742-6723.2005.00703.x. [DOI] [PubMed] [Google Scholar]
- 11.Samet JH, Burstin HR, Green J, Singer DE. Sociodemographic determinants in the hospitalization decision: evaluation of an emergency department interhospital transfer policy. Ann Emerg Med. 1993;22:813–818. doi: 10.1016/s0196-0644(05)80797-8. [DOI] [PubMed] [Google Scholar]
- 12.Maxwell B, Miller B. Smooth the way for safe emergency transfers. RN. 1988;51:34–37. [PubMed] [Google Scholar]
- 13.Koppenberg J, Taeger K. Interhospital transport: transport of critically ill patients. Curr Opin Anaesthesiol 15. :211–215. doi: 10.1097/00001503-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Gray A, Bush S, Whiteley S. Secondary transport of the critically ill and injured adult. Emerg Med J. 2004;21:281–285. doi: 10.1136/emj.2003.005975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aylott M. Expanding the role of the neonatal transport nurse: nurse-led teams. Br J Nurs. 1997;6:800–804. doi: 10.12968/bjon.1997.6.14.800. [DOI] [PubMed] [Google Scholar]
- 16.Edge WE, Kanter RK, Weigle CG, Walsh RF. Reduction of morbidity in interhospital transport by specialized pediatric staff. Crit Care Med. 1994;22:1186–1191. doi: 10.1097/00003246-199407000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Britto J, Nadel S, Maconochie I, Levin M, Habibi P. Morbidity and severity of illness during interhospital transfer: specialized paediatric retrieval team. BMJ. 1995;311:836–839. doi: 10.1136/bmj.311.7009.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vos GD, Nissen AC, Nieman FH, Meurs MM, van Waardenburg DA, Ramsay G, et al. Comparison of interhospital pediatric intensive care transport accompanied by a referring specialist or a specialist retrieval team. Intensive Care Med. 2004;30:302–308. doi: 10.1007/s00134-003-2066-7. [DOI] [PubMed] [Google Scholar]
- 19.McGinn GH, MacKenzie RE, Donnelly JA, Smith EA, Runcie CJ. Interhospital transfer of the critically ill trauma patient: the potential role of a specialist transport team in a trauma system. J Accid Emerg Med. 1996;13:90–92. doi: 10.1136/emj.13.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bellingan G, Olivier T, Batson S, Webb A. Comparison of a specialist retrieval team with current UK practice for the transport of critically ill patients. Intensive Care Med. 2000;26:740–744. doi: 10.1007/s001340051241. [DOI] [PubMed] [Google Scholar]
- 21.Lees M, Elcock M. Safety of interhospital transport of cardiac patients and the need for medical escorts. Emerg Med Australas. 2008;20:23–31. doi: 10.1111/j.1742-6723.2007.01020.x. [DOI] [PubMed] [Google Scholar]


