Abstract
BACKGROUND:
Patients with acute chest pain remain a great diagnostic challenge to emergency physicians. Ischemia-modified albumin (IMA) is a recently developed biomarker of transient myocardial ischemia. IMA has already been licensed by the US Food and Drug Administration for diagnosis of suspected myocardial ischemia. This study aimed to assess the diagnostic value of IMA in treatment of patients with acute coronary syndrome(ACS).
METHODS:
IMA level was detected by ultra-filtration assay combined with albumin-cobalt binding (ACB) test as well as tests of myoglobin (MYO), creatine kinase-MB (CK-MB) and cardiac troponin I (cTnI) in 169 consecutive patients with acute chest pain onset within 24 hours. Receiver operating characteristic (ROC) curve for IMA in diagnosing ACS was established to determine the cut-off point. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of IMA and its combinations with other agents were analyzed.
RESULTS:
Area under the ROC curve (AUC) was 0.754. As the cut-off point for IMA in this study was 70.4 U/ml, the sensitivity, specificity, PPV and NPV of IMA were 79.8%, 65.2%±77.7%, and 69.7%, respectively. The sensitivity and NPV of IMA combined with the conventional cardiac marker panel for the diagnosis of ACS were 93.4% and 86.0%, respectively.
CONCLUSION:
IMA is a useful biochemical marker for the early diagnosis of ACS. IMA combined with the conventional cardiac marker panel can improve early diagnosis of ACS compared with the traditional combinations of myocardial biochemical markers.
KEY WORDS: Ischemia-modified albumin, Acute coronary syndrome
INTRODUCTION
Patients with acute chest pain remain a great diagnostic challenge to emergency physicians. It is estimated that 30% of patients presenting with chest pain will be diagnosed with an acute coronary syndrome.[1] However, none of the traditional clinical data, 12-lead ECG, biochemical markers of necrosis, or imaging techniques can be considered a true gold standard for the diagnosis of cardiac ischemia.
Ischemia-modified albumin (IMA) is a recently developed biomarker of transient myocardial ischemia. Previous studies have shown that IMA levels rise within minutes after cardiac ischemia.[2] IMA is a serum albumin in which the N-terminus has been chemically modified. The diagnostic albumin CO2+ binding (ACB) test for IMA is based on the observation that the affinity of serum albumin for CO2+ is reduced after N-terminus modifications. The test has already been licensed by the US Food and Drug Administration for diagnosis of suspected myocardial ischemia.[3]
In the present study, we detected the IMA levels by ultra-filtration assay combined with ACB test so as to assess the diagnostic value of IMA for patients with acute coronary syndrome (ACS).
METHODS
This study was performed in the chest pain unit (CPU) of XinHua Hospital and the emergency room of Zhongshan Hospital, Shanghai, China. The enrollment period was between April and August 2008. We recruited, on a prospective sequential basis, 198 patients aged from 18 to 80 years and arrived at the unit or room within 24 hours after onset of chest pain. Patients with positive cardiac troponin on ED admission, acute or chronic renal failure, symptomatic peripheral vascular disease, and cerebral ischemia were excluded. For discharge diagnosis, we applied the ACC/AHA 2007 Guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction[4] and ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction.[5]
After obtaining consent from patients, blood (10 ml) was drawn into tubes, centrifuged, transported immediately to the department of laboratory medicine, and serum was prepared for the cardiac marker, with an additional venous sample for measurement of IMA which was frozen at -4°C within 2 hours and stored until the measurement. IMA was measured by the albumin cobalt binding test (ACB test) on an automated biochemical instrument (CaiHong, China). The kit of ACB test was purchased from Shanghai Microwells China(lot number 08030109). Blood was collected in serum separated tubes for the IMA test. Specimens were frozen at -20°C or lower within two hours. Frozen samples were gently vortexed after thawing. By the ACB test, 100μ1 of a patient sample and 200μ1 of cobalt chloride [(CoII)] and phosphate buffered saline (PBS) were incubated for five minutes in a centrifugal ultra-filtration device. During the incubation, the Co(II) binded to the N-terminus of unaltered albumin in the sample; albumin for which the N-terminus is altered as a result of ischemic processes binded to the Co(II) to a far lesser extent. After the incubation, the centrifugal ultra-filtration device was placed in an ultracentrifuge to remove the protein; the time and velocity were 20 minutes and 1000g respectively. Then, the liquid of mixture filtered was collected, and 450μl of dithiothreitol (DTT) was added to the mixture. DTT formed a colored complex with the Co (II) that is not bound at the N-terminus of albumin, and this complex was measured spectrophotometrically at 470 nm. Duplicate IMA values were obtained with the mean recorded as the result of the assay.
cTnI, MYO and CK-MB were measured by electrochemiluminescence. Immunoassay used Access 2 (Beckman Coulter, America). The cut-off values suggested by the manufacturer, MYO >70.0 ng/ml, CK-MB >25.0 ng/ml, cTnI >0.06 ng/ml were considered positive. ECG was recorded by FX-3010 Electrocardiograph (FOTON, Japan). Significant ECG changes (unless known to be old) included ST segment elevation 1 mm or T wave inversion in two continuous leads. Left bundle branch block was considered positive.
Diagnostic assay data for normally distributed continuous variables are expressed as mean±standard deviation (SD). Differences between the two groups were compared with independent sample tests. Statistical significance was established at the 0.05 confidence level. The cut-off values for IMA were experimentally determined by receiver operator characteristic (ROC) analysis. The sensitivity and specificity of serum IMA were assessed by the ROC curve. The areas under the curves were calculated and compared (significance established at the 0.05 confidence level). Positive predictive value (PPV) and negative predictive value (NPV) were calculated. The SPSS 10.0 (SPSS, Chicago, IL) and MedCalc version 6.0 (MedCalc, Mariakerke, Belgium) statistical software package were used for all calculations.
RESULTS
Sufficient data were available in 169 of the 198 patients (92 men and 77 women, mean age 65.2 ±15.3 years). According to the ACC/AHA 2007 Guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction, 102 of the 169 enrolled patients were discharged with a final diagnosis of ACS and 67 with the diagnosis of non-ischemic chest pain (NICP). A clear non-cardiac cause of chest pain was identified in 55 NICP patients (a final diagnosis of stable angina in 6 patients, myocarditis in 2, heart failure in 15, aortic dissection in 1, arrhythmia in 11, pneumo-infection in 10, costal chondritis in 5, pleuritis in 1, gastroesophageal reflux disease in 1, gastritis in 2, and cholecystitis in 1). In the ACS group, a clinical diagnosis was made in 43 patients , meanwhile, other 59 patients underwent angiography (32 patients with >70% stenosis).
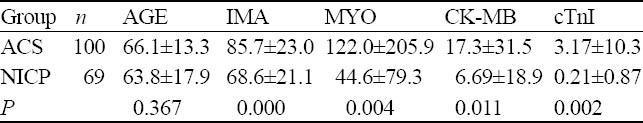
Serum samples from the ACS group had higher levels of IMA, MYO, CK-MB and cTnI compared with those from the NICP group; the difference was statistically significant (Table 1).
Table 1.
Levels of IMA, MYO, CK-MB and cTnI on admission in the ACS or non-ACS groups
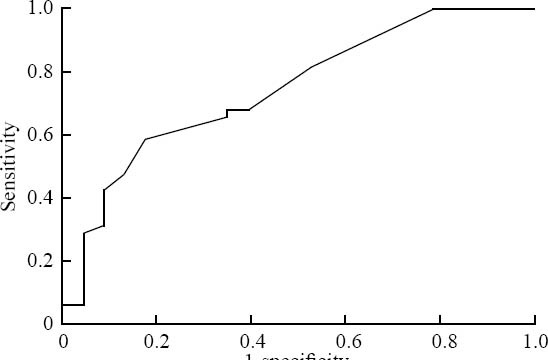
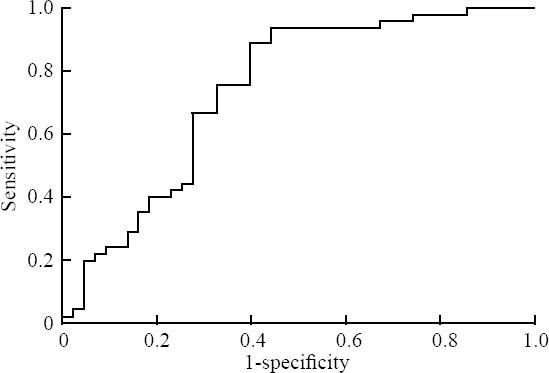
An ROC curve was plotted for IMA results in this study population (Figure 1). Area under the ROC curve(AUC) was 0.754 (95% CI, 0.677-0.832). For the optimum diagnostic cut-off value of 70.4mg/L, the sensitivity and specificity were 79.8% and 65.2%, respectively, and the negative and positive predictive values were 69.7% and 77.7% , respectively. ROC curves of IMA and TNI during the different periods are shown in Figures 2-5. The AUC of IMA decreased from 0.836 below 6 hours after chest pain to 0.793 over 6 hours after presentation; however , the AUC of TNI elevated from 0.750 to 0.838 during the same time.
Figure 1.
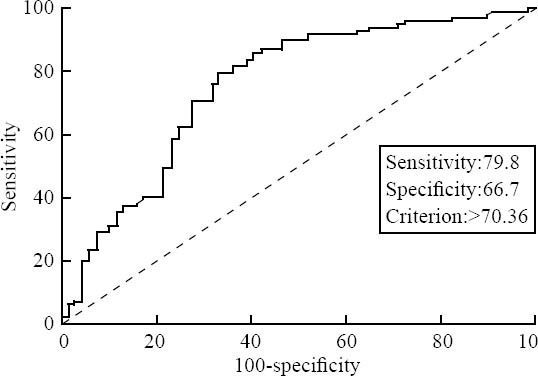
ROC curve of IMA (all patients involved)
Figure 2.
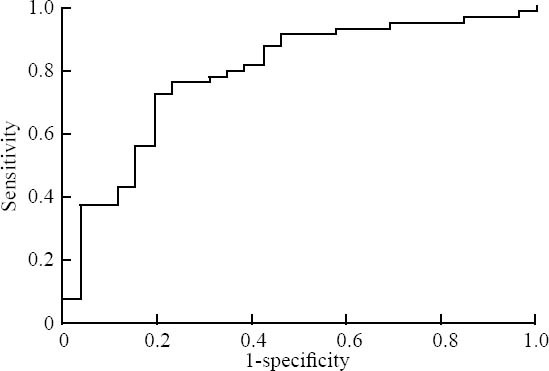
ROC curve of IMA (0-6 h)
Figure 5.
ROC curve of TNI (>6 h)
Figure 3.
ROC curve of IMA (≥6 h) 1-specificity
Figure 4.
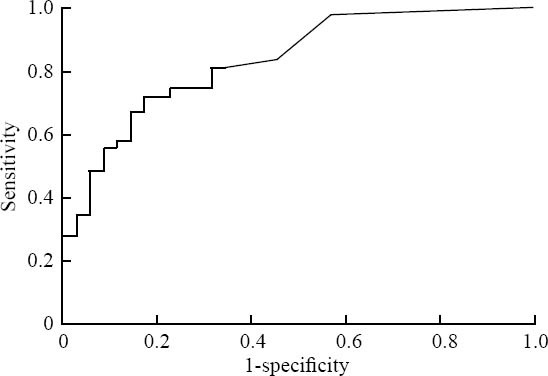
ROC curve of TNI (0-6 h)
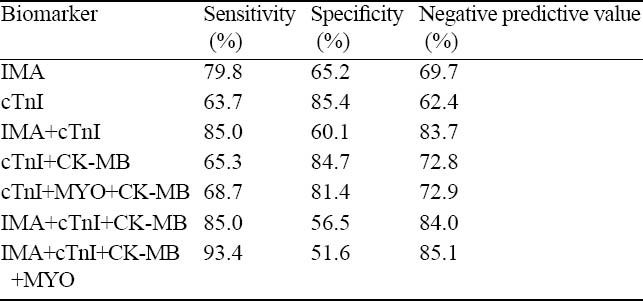
The sensitivity and specificity of the conventional cardiac marker panel (myoglobin, CK-MB and troponin T) for the diagnosis of ACS were 68.7% and 81.4%,respectively or 93.4% and 51.6%, respectively. With the IMA test included in the conventional panel, its NPV and PPV were shown to be 85.1% and 65.0% (Table 2).
Table 2.
Sensitivity,specificity and negative predictive value for diagnosis of ACS at ER presentation
DISCUSSION
This study shows that IMA has a comparatively high specificity for prediction of a discharge diagnosis of ACS, possibly we measured IMA with an ultra-filtration assay, which filters unnecessary protein to reduce background interference such as hemolysis,blood liquid and drug.
Meanwhile, IMA has a low sensitivity in this study compared with others,[6,7] presumably because of kinetics of IMA. Previous studies have shown that IMA levels rise within minutes after ischemia and return to the baseline level within 6-12 hours.[2, 8] In the present study, 82 patients arrived at ED at the time exceeding 6 hours after the onset of chest pain, and 42 patients among those patients had a discharge diagnosis of ACS. The kinetics can also explain why the AUC of IMA decreased from 0.836 below 6 hours after chest pain to 0.793 over 6 hours after presentation.
To the present, the mechanism of IMA is not clear. Reduced cobalt binding has also been found in patients with skeletal muscle ischemia or with peripheral vascular disease, as well as in patients with diseases associated with oxidative stress such as systemic sclerosis.[9-11] Besides, many factors have been reported to affect the ACB test, including tests of plasma cysteine/cystine ratio and plasma pH.[12] Hence IMA alone does not appear to fulfill the criteria of an ideal marker of myocardial ischemia, and its results must be interpreted cautiously, taking into consideration of clinical circumstances and co-morbidity. We recommend using the combination of IMA and the cardiac panel, giving a higher value for sensitivity and specificity, especially for NPV. The combination seems to have a clear potential to save time and shorten stay in the emergency department, but needs to be proved clinically useful by adequate test.
Footnotes
Funding: The paper was supported by the grants from the Shanghai Health Bureau, Science and Technology Development Fund (2007108).
Ethical approval: The study was approved by the ethical Committee of Xinhua Hospital Shanghai Jiaotong University.
Competing interest: We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work, there is no professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of, the manuscript entitled.
Contributors: Pan SM wrote the first draft of this paper. All authors contributed to the intellectual content and approved the final version.
REFERENCES
- 1.Storrow AB, Gibler WB. Chest pain centers: diagnosis of acute coronary syndromes . Ann Emerg Med. 2000;35:449–461. [PubMed] [Google Scholar]
- 2.Bar-Or D, Winkler JV, Vanbenthuysen K, Harris L, Lau E, Hetzel FW. Reduced albumin-cobalt binding with transient myocardial ischemia after elective percutaneous transluminal coronary angioplasty: a preliminary comparison to creatine kinase-MB, myoglobin and troponin I. Am Heart J. 2001;141:985–991. doi: 10.1067/mhj.2001.114800. [DOI] [PubMed] [Google Scholar]
- 3.Peacock F, Morris DL, Anwaruddin S, Christenson RH, Collinson PO, Goodacre SW, et al. Meta-analysis of ischemia-modified albumin to rule out acute coronary syndromes in the emergency department. Am Heart J. 2006;152:253–262. doi: 10.1016/j.ahj.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 4.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Jiang SL, Ji XP, Zhang Y. Introduction to ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction(2004 revision) . Natl Med J China. 2005;85:62–64. [PubMed] [Google Scholar]
- 6.Collinson PO, Gaze DC, Bainbridge K, Morris F, Morris B, Price A, et al. Utility of admission cardiac troponin and “Ischemia Modified Albumin” measurements for rapid evaluation and rule out of suspected acute myocardial infarction in the emergency department. Emerg Med J. 2006;23:256–261. doi: 10.1136/emj.2005.028241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinha MK, Roy D, Gaze DC, Collinson PO, Kaski JC. Role of “Ischemia modified albumin”, a new biochemical marker of myocardial ischaemia, in the early diagnosis of acute coronary syndromes. Emerg Med J. 2004;21:29–34. doi: 10.1136/emj.2003.006007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinha MK, Gaze DC, Tippins JR, Collinson PO, Kaski JC. Ischemia modified albumin is a sensitive marker of myocardial ischemia after percutaneous coronary intervention. Circulation. 2003;107:2403–2405. doi: 10.1161/01.CIR.0000072764.18315.6B. [DOI] [PubMed] [Google Scholar]
- 9.Roy D, Quiles J, Gaze DC, Collinson P, Kaski JC, Baxter GF. Role of reactive oxygen species on the formation of the novel diagnostic marker ischaemia modified albumin. Heart. 2006;92:113–114. doi: 10.1136/hrt.2004.049643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apple FS, Quist HE, Otto AP, Mathews WE, Murakami MM. Release characteristics of cardiac biomarkers and ischemia-modified albumin as measured by the albumin cobalt-binding test after a marathon race. Clin Chem. 2002;48:1097–1100. [PubMed] [Google Scholar]
- 11.Borderie D, Allanore Y, Meune C, Devaux JY, Ekindjian OG, Kahan A. High ischemia-modified albumin concentration reflects oxidative stress but not myocardial involvement in systemic sclerosis. Clin Chem. 2004;50:2190–2193. doi: 10.1373/clinchem.2004.034371. [DOI] [PubMed] [Google Scholar]
- 12.Bar-Or D, Rael LT, Bar-Or R, et al. The cobalt-albumin binding assay: in sights into its mode of action. Clin Chim Acta. 2008;387:120–127. doi: 10.1016/j.cca.2007.09.018. [DOI] [PubMed] [Google Scholar]


