Abstract
BACKGROUND:
The widespread use of gastrointestinal bleeding prophylaxis in critically ill patients was one of the most controversial issues. Since few studies reported the incidence of gastrointestinal bleeding in mechanically ventilated patients, this study aimed to identify the incidence and risk factors related to gastrointestinal bleeding in patients undergoing mechanical ventilation for more than 48 hours.
METHODS:
A total of 283 ICU patients who had received mechanical ventilation for longer than 48 hours at a provincial hospital affiliated to Shandong University from January 1, 2007 to December 31, 2009 were analyzed retrospectively. Those were excluded from the study if they had a history of gastrointestinal bleeding or ulceration, recent gastrointestinal surgery, brain death and active bleeding from the nose or throat. Demographic data of the patients included patient age, diagnosis on admission, duration of ICU stay, duration of ventilation, patterns and parameters of ventilation, ICU mortality, APACHE II score, multiple organ dysfunction, and indexes of biochemistry, kidney function, liver function and coagulation function. Risk factors of gastrointestinal bleeding were analyzed by univariate analysis and multiple logistic regression analysis.
RESULTS:
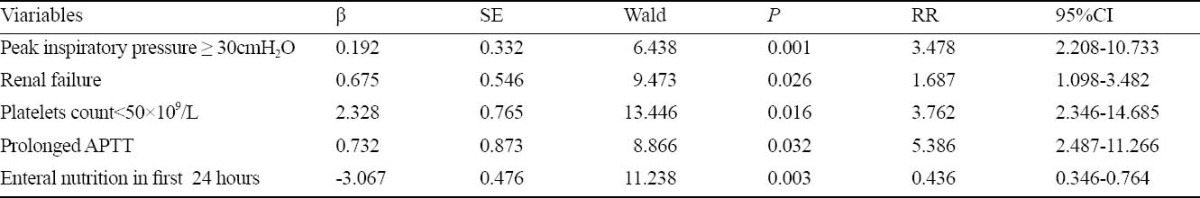
In the 242 patients who were given mechanical ventilation longer than 48 hours, the incidence of gastrointestinal bleeding was 46.7%. The bleeding in 3.3% of the patients was clinically significant. Significant risk factors were peak inspiratory pressure ≥30cmH2O, renal failure, liver failure, PLT count<50×109/L and prolonged APTT. Enteral nutrition had a beneficial effect on gastrointestinal bleeding. However, the multiple logistic regression analysis revealed that the independent risk factors of gastrointestinal bleeding were as follows: high pressure ventilator setting ≥ 30cmH2O(RR=3.478, 95%CI=2.208-10.733), renal failure(RR=1.687, 95%CI = 1.098-3.482), PLT count<50×1 09/L (RR=3.762, 95%CI=2.346-14.685), and prolonged APTT(RR=5.368, 95%CI=2.487-11.266). Enteral nutrition(RR=0.436, 95%CI= 0.346-0.764) was the independent protective factor.
CONCLUSIONS:
The incidence of gastrointestinal bleeding was high in the patients who received mechanical ventilation, and bleeding usually occurred within the first 48 hours. High pressure ventilator setting, renal failure, decreased PLT count and prolonged APTT were the significant risk factors of gastrointestinal bleeding. However, enteral nutrition was the independent protective factor.
KEY WORDS: Mechanical ventilation, Gastrointestinal bleeding, Risk factors
INTRODUCTION
Stress ulceration of the gastrointestinal tract causes overt and clinically important bleeding in critically ill patients. The incidence of gastrointestinal bleeding varies from 15% to 50% in the first 24 hours of ICU stay[1] and that of clinically significant upper gastrointestinal bleeding from 2% to 6%[2]. It is suggested that mechanical ventilation is one of the most significant risk factors of gastrointestinal bleeding in the intensive care unit.[3] Clinical studies demonstrated the benefit of prophylaxis of pharmacologic gastrointestinal bleeding in mechanical ventilated patients. However, the prophylaxis may not be cost-effective, but is likely to increase the incidence of ventilator-associated pneumonia.[4] The international guidelines for management of severe sepsis and septic shock released in 2008 indicated that the limitations must be considered before using stress ulcer prophylaxis to prevent gastrointestinal bleeding.[5] Accordingly, the benefit of the widespread use of stress ulcer prophylaxis in critically ill patients has been questioned, and the prophylaxis targeting at those patients who are most likely to bleed has been suggested. Since few studies reported the incidence of gastrointestinal bleeding in mechanically ventilated patients, this study was designed to assess the incidence and risk factors associated with gastrointestinal bleeding in critically ill patients who had received mechanical ventilation and to identify the patients at risk who may be benefitted from the prophylaxis of gastrointestinal bleeding.
METHODS
Patients
All patients aged 18-70 years who had received mechanical ventilation for more than 48 hours in the ICU of the Provincial Hospital affiliated to Shandong University from January 1, 2007 to December 31, 2009 were included in this retrospective study. Excluded from the study were those with a history of gastrointestinal bleeding or ulceration, recent gastrointestinal surgery, brain death, and active bleeding from the nose or throat.[6]
In this study gastrointestinal bleeding was categorized into overt and clinically significant bleeding. Overt bleeding was diagnosed if there was evidence of hematemesis, “coffee ground” material or positive occult blood in nasogastric aspirates, melena or hematochezia. Clinically significant bleeding was defined as overt bleeding plus one of the following features in the absence of other causes: a) a spontaneous decrease in systolic or diastolic blood pressure of more than or equal to 20 mm Hg within 24 hours of upper gastrointestinal bleeding; b) an increase in pulse rate of 20 beats/min and a decrease in systolic blood pressure of 10 mmHg on orthostatic change; c) a decreased hemoglobin level of more than or equal to 2 g/dl (20 g/L) in 24 hours and transfusion of 2 units of packed red blood cells within 24 hours of bleeding; or d) failure of the hemoglobin level to increase by at least the number of units transfused minus 2 g/dl (20 g/L).[6]
Renal failure was defined in patients with a serum creatinine level of more than 177μmol/L or analysis indication existed.[7]
Liver failure was defined in patients with a total bilirubin level of more than 60 μmol/L, and the levels of AST and ALT were at least two times the upper limit of normality.[7]
Coagulation disorder was defined in patients with the prothrombin time (PT) more than 3 seconds above the control value, the activated partial thromboplastin time (APTT) >10 seconds above the control value.[7]
Gastrointestinal bleeding prophylaxis was conducted by administration of two or more doses of the following agents: histamine H2-receptor antagonists, sucralfate, and proton pump inhibitors.[7]
Demographic data included patient characteristics, admission diagnosis, duration of ICU stay, duration of ventilation, patterns and parameters of ventilation, ICU mortality, APACHE II score,[8] multiple organ dysfunction score,[9] and laboratory data such as hemoglobin level, platelet count, PT, APTT, blood urea nitrogen, creatinine, and liver function within 24 hours after admission to ICU.
Statistical analysis
All data were analyzed by the SPSS16.0 for Windows and were expressed as mean ± SD. The parameters were compared between the patients with and without gastrointestinal bleeding by Student's t test. Measurement data were expressed as percentage of total patients, and the parameters were compared between the patients with and without gastrointestinal bleeding by the chi-square test. The relative risk and 95% confidence interval of the significant factors were calculated. Multiple logistic regression analysis was made to identify the independent risk factors. A P value<0.05 was considered statistically significant.
RESULTS
A total of 283 ICU patients who had had mechanical ventilation for more than 48 hours at the Provincial Hospital affiliated to Shandong University from January 1, 2007 to December 31, 2009 were reviewed retrospectively. Forty-one patients were excluded from the study for a history of gastrointestinal bleeding or ulceration (13 patients), recent gastrointestinal surgery (21), active bleeding from the nose or throat (5), and brain death (2). At last 242 patients were included in the study. Among these patients, 113 (46.7%) experienced gastrointestinal bleeding, 86 had coffee ground material or positive occult blood in nasogastric aspirates, 12 had positive occult blood in stools, 5 had hematemesis, 2 had hematochezia, and 2 had both hematemesis and hematochezia. Eight patients with gastrointestinal bleeding (3.3%) were diagnosed with clinically significant bleeding (Four patients developed hypotension, and two needed surgery). Most patients (67.3%) developed gastrointestinal bleeding during the first 48 hours of mechanical ventilation and 80% during the first 2 weeks of mechanical ventilation. Characteristics of the patients with and without gastrointestinal bleeding are shown in Table 1, the factors associated with gastrointestinal bleeding in Table 2, and the characteristics of the patients with independent factors of bleeding in Table 3.
Table 1.
Results of univariate analysis in count data of gastrointestinal bleeding and no gastrointestinal bleeding in mechanically ventilated patients
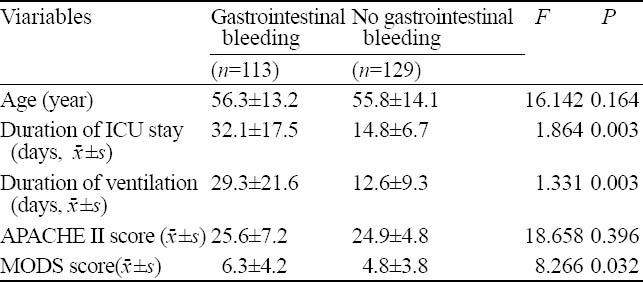
Table 2.
Results of univariate analysis in measurement data of gastrointestinal bleeding and no gastrointestinal bleeding in mechanically ventilated patients
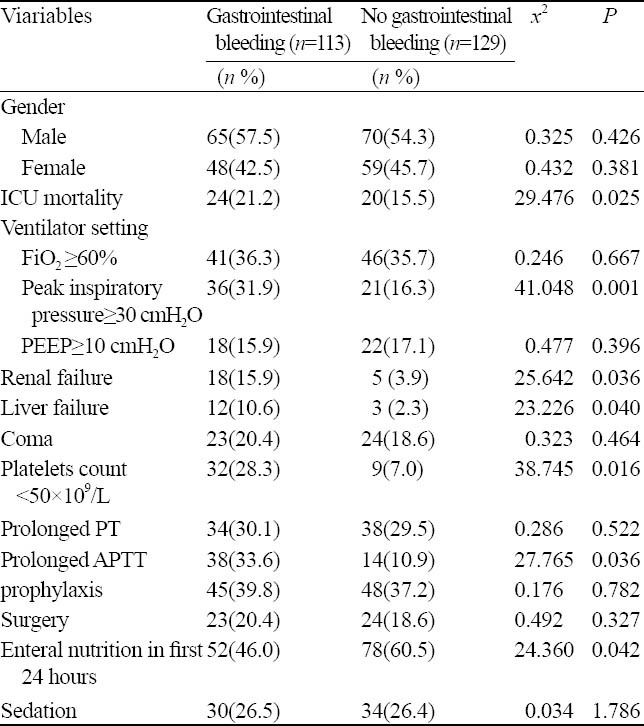
Table 3.
Results of multivariate logistic regression analysis in gastrointestinal bleeding of mechanically ventilated patients
DISCUSSION
Altogether 242 patients were retrospectively studied. We found that the high incidence of gastrointestinal bleeding in mechanically ventilated patients was consistent with that reported by Cook et al.[10] The average duration in ICU on admission and duration of mechanical ventilation in the patients with gastrointestinal bleeding were longer than in those without gastrointestinal bleeding. The mortality of patients with gastrointestinal bleeding was significantly higher than that of those without gastrointestinal bleeding.
All patients in this study had respiratory failure and required mechanical ventilatory support. The significant risk factors of gastrointestinal bleeding in ICU patients in this study was consistent with that reported elsewhere[11]. The independent risk factor identified by the multivariate analysis was peak inspiratory pressure≥30cmH2O. The mechanism underlying gastrointestinal bleeding was likely to be associated with pressure-related mucosal damage.[12] The effect of high airway pressure on venous return resulted in reduced cardiac output and defective tissue perfusion, which subsequently caused injury to the gastrointestinal mucosa.
It has been demonstrated that prolonged APTT and low platelet count are independent risk factors for the occurrence of gastrointestinal bleeding in critically ill patients. This finding is similar to that of other studies.[13] In the present study renal failure was found to be another independent risk factor identified by multivariate analysis. The mechanisms by which renal failure predisposed to bleeding were likely multifactorial and included gastric erosions and impaired perfusion of the gastric mucosa.[14]
Enteral nutrition was proved to be the only independent protective factor associated with the occurrence of gastrointestinal bleeding in the present study. Patients receiving enteral nutrition in the first 24 hours had a lower rate of bleeding than those patients receiving no enteral nutrition. It is suggested that a beneficial mucosa effect is related to the alkaline pH of feeding.[15] In a recent study of 526 burned patients, the rate of serious bleeding in cimetidine-treated patients was 2.0%, whereas the rate in patients tolerating early enteral nutrition was only 0.7%.[16] However, similar to other studies, the patients were not randomized to receive or not to receive enteral feeding. Thus, an equally plausible explanation for our finding was that patients with a lower intrinsic risk of bleeding were those who better tolerated to enteral feeding.
The widespread use of gastrointestinal bleeding prophylaxis in critically ill patients was one of the most controversial issues. Several studies reported the usefulness of gastrointestinal bleeding prophylaxis in patients who were subjected to mechanical ventilation. [17,18] However, many studies also reported side-effects (nosocomial pneumonia) and high financial costs.[19,20] In our study, there was no significant association between gastrointestinal bleeding prophylaxis and overt gastrointestinal bleeding. There were significant risk factors for gastrointestinal bleeding in 8 patients with clinically significant bleeding in the study, including peak inspiratory pressure≥30cmH2O, prolonged APTT, low platelet count, and/or renal failure. The percentage of patients with clinically significant bleeding was not high enough to that of the recommended prophylactic therapy in all patients receiving mechanical ventilation. The suggestion of gastrointestinal bleeding prophylaxis targeted at those patients who are most likely to bleed was also supported by Gauvin et al.[21] Thus, gastrointestinal bleeding prophylaxis should be selective, and it is indicated for high-risk patients. Identification of risk factors for gastrointestinal bleeding in mechanically ventilated patients may lead to a better approach for gastrointestinal bleeding prophylaxis, which may reduce side-effect of prophylactic therapy and costs.
In conclusion, our study demonstrated the high incidence of overt gastrointestinal bleeding in the critically ill patients receiving mechanical ventilation. Gastrointestinal bleeding usually occurs within the first 48 hours. High pressure ventilator setting, renal failure, PLT count <50×109/L, and prolonged APTT are the independent risk factors of gastrointestinal bleeding in mechanically ventilated patients. Moreover, enteral nutrition is the independent protective factor.
Footnotes
Funding: The study was supported by a grant from the Shandong Medical and Health Development Project (2009HZ055).
Ethical approval: Not needed.
Conflicts of interest: None.
Contributors: Chu YF wrote the first draft of this paper. All authors contributed to the intellectual content and approved the final version.
REFERENCES
- 1.Faisy C, Guerot E, Diehl JL, Iftimovici E, Fagon JY. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress-ulcer prophylaxis. Intensive Care Med. 2003;29:1306–1313. doi: 10.1007/s00134-003-1863-3. [DOI] [PubMed] [Google Scholar]
- 2.Kantorova I, Svoboda P, Scheer P, Doubek J, Rehorkova D, Bosakova H, et al. Stress ulcer prophylaxis in critically ill patients: A randomized controlled trial. Hepatogastroenterology. 2004;51:757–761. [PubMed] [Google Scholar]
- 3.Miano TA, Reichert MG, Houle TT, MacGregor DA, Kincaid EH, Bowton DL. Nosocomial pneumonia risk and stress ulcer prophylaxis: a comparison of pantoprazole vs ranitidine in cardiothoracic surgery patients. Chest. 2009;136:440–447. doi: 10.1378/chest.08-1634. [DOI] [PubMed] [Google Scholar]
- 4.Kahn JM, Doctor JN, Rubenfeld GD. Stress ulcer prophylaxis in mechanically ventilated patients: integrating evidence and judgment using a decision analysis. Intensive Care Med. 2006;32:1151–1158. doi: 10.1007/s00134-006-0244-0. [DOI] [PubMed] [Google Scholar]
- 5.Hicks P, Cooper DJ, Webb S, Myburgh J, Seppelt I, Peake S, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 6.Kantorova I, Svoboda P, Scheer P, Doubek J, Rehorkova D, Bosakova H, et al. Stress ulcer prophylaxis in critically ill patients: a randomized controlled trial. Hepatogastroenterology. 2004;51:757–761. [PubMed] [Google Scholar]
- 7.Lv ZY, Zhong NS. Internal Medicine. 7th Edition. Beijing: People's Medical Publishing House; 2008. [Google Scholar]
- 8.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–825. [PubMed] [Google Scholar]
- 9.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638–1652. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Cook DJ, Reeve BK, Guyatt GH, Heyland DK, Griffith LE, Buckingham L. Stress ulcer prophylaxis in critically ill patients. Resolving discordant meta-analyses. JAMA. 2006;275:308–314. [PubMed] [Google Scholar]
- 11.López-Herce J. Gastrointestinal complications in critically ill patients: what differs between adults and children? Curr Opin Clin Nutr Metab Care. 2009;12:180–185. doi: 10.1097/MCO.0b013e3283218285. [DOI] [PubMed] [Google Scholar]
- 12.Duerksen DR. Stress-related mucosal disease in critically ill patients. Best Pract Res Clin Gastroenterol. 2003;17:327–344. doi: 10.1016/s1521-6918(03)00028-3. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg KP. Stress-related mucosal disease in the critically ill patient: Risk factors and strategies to prevent stress-related bleeding in the intensive care unit. Crit Care Med. 2002;30:S362–S364. doi: 10.1097/00003246-200206001-00005. [DOI] [PubMed] [Google Scholar]
- 14.Raff T, Germann G, Hartmann B. The value of early enteral nutrition in the prophylaxis of stress ulceration in the severely burned patient. Burns. 2007;23:313–318. doi: 10.1016/s0305-4179(97)89875-0. [DOI] [PubMed] [Google Scholar]
- 15.Xie JX, Wu S, Kuang ZC. The comparison of early enteral and parenteral nutrition support in mechanical ventilation patients. Chin J Emerg Med. 2003;12:734–736. [Google Scholar]
- 16.Ali T, Harty RF. Stress-induced ulcer bleeding in critically ill patients. Gastroenterol Clin North Am. 2009;38:245–265. doi: 10.1016/j.gtc.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Wahl WL, Arbabi S, Zalewski C, Wang SC, Hemmila MR. Intensive care unit core measures improve infectious complications in burn patients. J Burn Care Res. 2010;31:190–195. doi: 10.1097/BCR.0b013e3181c89f0b. [DOI] [PubMed] [Google Scholar]
- 18.Janicki T, Stewart S. Stress-ulcer prophylaxis for general medical patients: a review of the evidence. J Hosp Med. 2007;2:86–92. doi: 10.1002/jhm.177. [DOI] [PubMed] [Google Scholar]
- 19.Kantorova I, Svoboda P, Scheer P, Doubek J, Rehorkova D, Bosakova H, et al. Stress ulcer prophylaxis in critically ill patients: A randomized controlled trial. Hepatogastroenterology. 2004;51:757–761. [PubMed] [Google Scholar]
- 20.Faisy C, Guerot E, Diehl JL, Iftimovici E, Fagon JY. Clinically significant gastrointestinal bleeding in critically ill patients with and without stress ulcer prophylaxis. Intensive Care Med. 2003;29:1306–1313. doi: 10.1007/s00134-003-1863-3. [DOI] [PubMed] [Google Scholar]
- 21.Gauvin F, Dugas MA, Chaïbou M, Morneau S, Lebel D, Lacroix J. The impact of clinically significant upper gastrointestinal bleeding acquired in a pediatric intensive care unit. Pediatr Crit Care Med. 2001;2:294–298. doi: 10.1097/00130478-200110000-00002. [DOI] [PubMed] [Google Scholar]


