Abstract
BACKGROUND:
This study aimed to determine whether modified shock index (MSI) is associated with mortality that is superior to heart rate, blood pressure, or the shock index (SI) in emergency patients.
METHODS:
A retrospective database review was performed on 22 161 patients who presented to Peking Union Medical College Hospital Emergency Department and received intravenous fluids from January 1 to December 31, 2009. We gathered data of the patients on age, gender, vital signs, levels of consciousness, presenting complaints, and SI and MSI were calculated for all patients.
RESULTS:
Multivariate regression analysis was performed to determine the correlation between risk factors and outcome. There is a significant correlation between emergency patient mortality rate and patient’s vital signs obtained at the triage desk (HR>120 beats/min, systolic BP<90 mmHg, diastolic BP<60 mmHg). MSI is a stronger predictor of emergency patient mortality compared to heart rate and blood pressure alone, whereas SI does not have a significant correlation with emergency patient mortality rate.
CONCLUSION:
MSI is a clinically significant predictor of mortality in emergency patients. It may be better than using heart rate and blood pressure alone. SI is not significantly correlated with the mortality rate of the emergency patient.
KEY WORDS: Emergency department, Modified shock index, Mortality rate, Predictor, Multivariate regression analysis
INTRODUCTION
The purpose of triage in the emergency department is to identify those patients in serious conditions and require immediate treatment and to separate them from those who do not require urgent care. In most hospitals, triage is done by an experienced nurse based on the patient’s vital signs, age, levels of consciousness and presenting complaints. We are now working to find out a simple marker that may easily be used to predict emergency patients’ outcome, which may be of great help to triage.
Shock index (SI) or heart rate (HR) divided by systolic blood pressure (SBP) has been suggested as such a marker that can be used to predict the severity of hypovolemic shock. And it has also been used in emergency patients with sepsis and some other serious conditions. In most studies, SI can be a valuable tool, raising suspicion when it is abnormal even when heart rate and blood pressure are not.[1,2] But patients present to the emergency department are complex, they may have sepsis or hypovolemia and may also have pneumonia, heart failure or even myasthenic crisis. There is rare evidence to show whether SI can be used in triage in all emergency patients. SI uses only systolic blood pressure, but from our experience, diastolic blood pressure (DBP) is also of undeniable importance when determining patient’s clinical severity. Hence we incorporated diastolic blood pressure and developed the modified shock index (MSI), which is a ratio of heart rate to mean blood pressure (MAP).
![]()
In this review, we compared the use of SI, MSI, heart rate and blood pressure in predicting outcome of emergency patients.
METHODS
We reviewed retrospectively all patients aged 10 to 100 years who presented to the Emergency Department, Peking Union Medical College Hospital and received intravenous fluids from January 1 to December 31, 2009. The review was based on a computer database tracing every patient admitted to out emergency department. We focused on the patients who received intravenous fluids because they were real “emergency” patients who required rapid treatment. The patients with cardiorespiratory arrest who had received resuscitation without triage were also excluded (Figure 1). Altogether, there were 22 161 patients, who met the criteria and had nearly all kinds of situations emergency doctors may encounter. Data were collected on age, gender, vital signs on the triage desk, levels of consciousness, presenting complaints. SI and MSI were calculated and multivariate regression analysis was made.
Figure 1.
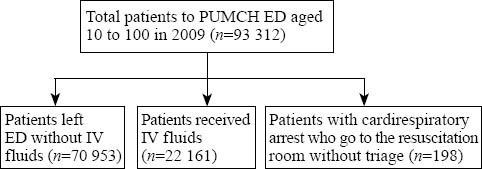
Flow chart of selecting patients.
Data collection and threshold determination
To obtain a value that can be easily analyzed, we determined threshold values for vital signs based on common cut-offs for normal values. The heart rate threshold was set at 120 beats per minute, systolic blood pressure was set at 90 mmHg, and diastolic blood pressure was set at 60 mmHg. Furthermore, the lower limit for SI was set at 0.5 and the upper limit was set at 0.9 according to the previous study.[3] Since no evidence was available for the use of MSI, we used the “MSI-mortality curve” as a starting point. Subsequently, regression analysis was made, the largest possible odds ratio was determined, and the threshold was set at 0.7 and 1.3. Our primary endpoint was the in-hospital mortality rate.
Statistical analysis
Using the SAS software, we performed multivariate logistic regression analysis. Because SI, MSI, heart rate, and blood pressure were interrelated, we analyzed each of them respectively against other factors.
RESULTS
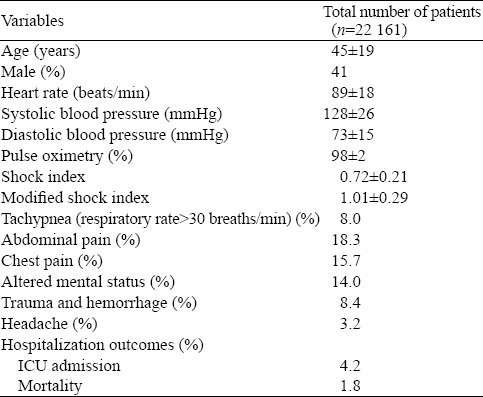
All the 22 161 patients complained of headache, chest pain, tachypnea, abdominal pain, altered mental status, trauma and hemorrhage. Among these patients, 938 (4.2%) were admitted to the ICU and 397 (1.8%) died (Table 1). To mimic real emergency department conditions, we collected major complaints instead of diagnosis, which cannot be obtained at the triage desk.
Table 1.
Patients’ characteristics in the derivation and validation sets
By plotting MSI on the X-axis and mortality rate on the Y-axis (Figure 2), we determined the relationship between MSI and mortality rate. The largest possible odds ratio was calculated by the vertex of the curve and regression analysis. According to this odds ratio, the threshold was set at 0.7, 1.3.
Figure 2.
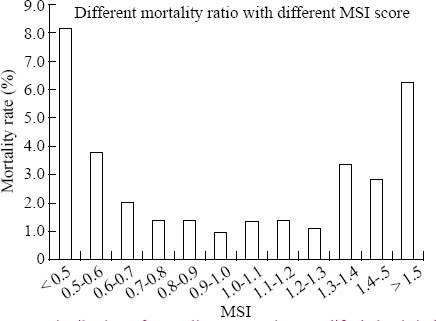
Distribution of mortality rate against modified shock index score.
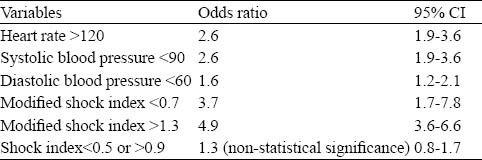
Multivariate logistic regression analysis demonstrated that HR>120 beats/min, SBP<90 mmHg and DBP <60 mmHg correlated with the mortality rate. When MSI or SI was used instead of heart rate and blood pressure, MSI>1.3 or <0.7 served as a stronger predictor of death. In contrast to traditional beliefs, SI of 0.5-0.9 was not correlated with the mortality rate of emergency department patients (Table 2).
Table 2.
Comparison of mortality rate prediction using heart rate, blood pressure, modified shock index and shock index as identified by multivariate analysis
DISCUSSION
Currently, most hospitals triage patients presenting to the emergency department into 3 to 5 levels. These levels include a minimum: life-threatening, possible life-threatening, and no urgency. But it is most difficult to separate patients with possible life-threatening illnesses from those with less acute diseases.
In this study, vital signs such as SBP<90 mmHg, DBP<60 mmHg, and HR>120 beats/min were found to be important predictors for outcomes of the patients. Most often, however, systolic blood pressure and diastolic blood pressure are underemphasized. In most studies, systolic blood pressure was used as blood pressure. In the present study diastolic blood pressure was found as an important predictor for outcomes of the patients and MSI was significantly related to the mortality rate of the patients.
Shock index is known as hemodynamic stability. The accepted value of shock index ranges from 0.5 to 0.7. This index is commonly used to assess the amount of blood loss and degree of hypovolemic shock. However, shock index in clinical practice is used to assess hypovolemic shock or the severity of non-hypovolemic shock.[3,4] It has been a predictor of clinical outcome better than blood pressure and heart rate alone in patients who are not in shock but have serious conditions such as pulmonary embolism.[5] This is due to hemodynamic instability , an indicator of clinical severity. Thus, shock index has been used by some emergency departments as a clinical severity score for critical patients.[1] But is the index useful in emergency conditions? So far the answer is unclear. There were different SI cutoff values used in different studies, but the commonly used SI value was 0.9 in patients with serious conditions. In our study, however, neither SI >0.9 nor <0.5 was an independent predictor for the mortality of emergency patients. The data of the study were only from one hospital, thus prospective studies are needed to confirm the result.
Shock index is observed in patients with hypovolemic shock at the very beginning. When systolic blood pressure is used, another important factor, diastolic blood pressure, may be neglected. Clinically, mean blood pressure can best represent tissue perfusion status. Our experience shows that diastolic blood pressure of a critical patient will decrease earlier than systolic blood pressure, and mean blood pressure is an accurate predictor for disease severity. If mean blood pressure replaces systolic blood pressure in SI, modified shock index (MSI) can be obtained from the following equation:
![]()
MSI indicates stroke volume and systemic vascular resistance. A high MSI denots a value of stroke volume and low systemic vascular resistance, a sign of hypodynamic circulation. Thus the patient may be compensating and the decompensation is rapid. A low MSI indicates that SI and SVR are high, and the patient is in a hyperdynamic state, which can also be a sign for serious conditions. Given the limited resources and information available at triage, MSI can be a valuable tool in predicting disease severity. Our results show that in patients with an MSI greater than 1.3, there is an increased probability of ICU admission and death. MSI is a more important clinical predictor than blood pressure and heart rate because MSI > 1.3 indicates a hypodynamic state. Conversely, low MSI is also a predictor of increased mortality. This is commonly seen in patients with cerebrovascular diseases, chest pain and palpitations. These patients often have increased ICP and arrhythmias, which can be easily identified.
In conclusion, MSI is an important predictor of mortality in patients presenting to the emergency department and it may be better than blood pressure and heart rate. SI is not significantly correlated with the mortality of emergency patients. When a patient with normal vital signs on the triage desk, MSI can be calculated to decide whether the condition of the patients is critical. Since this is a retrospective study, a prospective study is needed to confirm the result.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors have no financial or other conflicts of interest regarding this article.
Contributors: Wang Z proposed the study and Liu YC wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Rady MY, Smithline HA, Blake H, Nowak R, Rivers E. Comparison of the shock index and conventional vital signs to identify acute, critical illness in the emergency department. Ann Emerg Med. 1994;24:685–690. doi: 10.1016/s0196-0644(94)70279-9. [DOI] [PubMed] [Google Scholar]
- 2.Talmor D, Jones AE, Rubinson L, Howell MD, Shapiro NI. Simple triage scoring system predicting death and the need for critical care resources for use during epidemics. Crit Care Med. 2007;35:1251–1256. doi: 10.1097/01.CCM.0000262385.95721.CC. [DOI] [PubMed] [Google Scholar]
- 3.Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67:1426–1430. doi: 10.1097/TA.0b013e3181bbf728. [DOI] [PubMed] [Google Scholar]
- 4.Birkhahn RH, Gaeta TJ, Van Deusen SK, Tloczkowski J. The ability of traditional vital signs and shock index to identify ruptured ectopic pregnancy. Am J Obstet Gynecol. 2003;189:1293–1296. doi: 10.1067/s0002-9378(03)00663-x. [DOI] [PubMed] [Google Scholar]
- 5.Mehrdad Seilanian Toosi, John D, Merlino, Kenneth V, Leeper Prognostic value of the shock index along with transthoracic echocardiography in risk stratification of patients with acute pulmonary embolism. Am J Cardiol. 2008;101:700–705. doi: 10.1016/j.amjcard.2007.10.038. [DOI] [PubMed] [Google Scholar]


