Abstract
BACKGROUND:
Abdominal wall hematoma is due to trauma, coagulation disorders or anticoagulation therapy complications.
METHODS:
In this report we present a case of a 44-year-old female who suffered from blunt abdominal trauma and presented to the emergency department with sharp abdominal pain and ecchymosis. FAST and abdominal computerized tomography (CT) revealed an abdominal wall hematoma. Treatment with an ultrasound-guided percutaneous drainage was performed successfully.
RESULTS:
The patient remained under observation for six hours with serial ultrasound scans, and no signs of hematoma recurrence were present. She was discharged the same day with clinical improvement.
CONCLUSION:
Complete history investigation and clinical examination help to make a correct diagnosis of abdominal wall hematoma, select a prompt treatment, and reduce complications.
KEY WORDS: Rectus sheath hematoma, Abdominal wall hematoma, Emergency Department, FAST, Ultrasound guided percutaneous drainage
INTRODUCTION
Ultrasonography scans in the emergency department are progressively being used to perform guided percutaneous drainages (thoracocentesis, paracentesis, abscess drainage and others). In this paper we report an ultrasound-guided drainage of a traumatic abdominal wall hematoma in the emergency department.
CASE REPORT
A 44-year-old female with no medication or surgical history presented to the emergency department (ED) complaining of sharp abdominal pain in the lower abdomen without any other related symptoms. She had suffered from mild blunt abdominal trauma in a bus accident the day before.
Vital signs on arrival were stable. Examination revealed a 10 cm×4 cm ecchymosis over the hypogastric region and painful palpation without palpable masses, muscular rigidity or rebound tenderness. Computerized tomography revealed a hematoma of the anterior abdominal wall with no other abdominal findings (Figure 1). Pain subsided and the patient was discharged home with analgesics.
Figure 1.
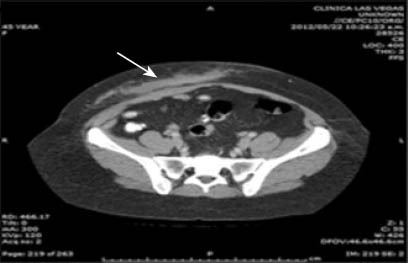
Abdominal wall hematoma. White arrow shows blood in the abdomen.
The next day she returned to the ED with persistence of her abdominal pain and abdominal bloating. There was no hemodynamic instability or acute surgical indications.
An examination with a Welld 3100 (Shenzhen-China) portable ultrasound with a 2.5–5.5 MHz curvilinear probe confirmed the abdominal hematoma. After verifying its location, a guided percutaneous drainage (Figures 2 and 3) was performed and 270 mL of sanguineous fluid was aspirated. The patient was observed for six hours with serial ultrasound scans, but no signs of hematoma recurrence were present. She was discharged the same day with clinical improvement.
Figure 2.

Hematoma. White arrow shows a needle inside.
Figure 3.

Hematoma after ultrasound guided drainage.
DISCUSSION
Isolated abdominal wall injuries caused by traffic accidents are not frequent in ED.
In a series,[1] rectus sheath hematoma (RSH) was the most frequent cause of abdominal wall hematoma and only 2.4% occurred in traumatized patients. The vast majorities are caused by anticoagulation related bleeding complications. Less common causes and risk factors are cough attacks, physical exercise,[2,3] intra-abdominal injections, over 50 years old, and pregnancy.[4,5]
RSH is a collection of blood that occurs between the rectus sheath of the abdominal wall due to disruption of epigastric (inferior or superior) vessels or rectus muscle. Sometimes clinical manifestations of RSH are not specific and they require a complete clinical evaluation to make an appropriate diagnosis. Intra-abdominal injury which is always a differential diagnosis must be ruled out. The typical clinical presentation includes abdominal pain, abdominal bloating, wall mass and decreased hemoglobin level. Sometimes nausea, vomiting, tachycardia, peritoneal irritation, hypotension or fever may be present.[1–3]
An early diagnosis made with CT or ultrasound may reduce complications such as infections, abdominal compartment syndrome, hypovolemic shock, or death. It was reported that ultrasound is highly sensitive in the diagnosis of abdominal wall hematoma.[6] Also, with ultrasound, trained physicians can distinguish abdominal wall injury from intra-abdominal injury.[7]
Selection of treatment modalities in RSH depends on patient’s medical history, comorbidities, hemodynamic stability and risk factors and clinical presentation of hematoma. Conservative management including bed rest, analgesia, and intravenous fluid replacement is the first line treatment for stable patients. Meanwhile surgical ligation of affected arteries, mainly superior and inferior epigastric arteries, is the treatment of choice for the patient in shock.[8] If bleeding continues and there is hemodynamic instability, other treatments such as empirical trans-catheter arterial embolization, digital subtraction angiography with arterial embolization and angiography with vasodilators, anticoagulants, and thrombolytic may be used.
In the management of this injury, ultrasound can be used to diagnose, follow or drain the hematoma if necessary. The benefits of ultrasound are well known as a technology free of radiation, portable, enables a quick bedside examination. Findings can be immediately integrated with patient conditions, and in patients with abdominal trauma with wall hematoma, ultrasound is helpful in diagnosis and guided therapeutic treatment.
In conclusion, abdominal wall hematoma is a rare entity caused by trauma. It might be misdiagnosed as an acute abdomen and unnecessary surgical interventions can be made. Complete history investigation and clinical examination help to make a correct diagnosis, select a prompt treatment, and reduce complications.
In this paper we report an ultrasound-percutaneous drainage of a traumatic wall hematoma treated in the emergency department with no complications. An ultrasound-guided drainage under strict observation might be an appropriate management for the patients with abdominal wall hematoma who have no medical history, are not subjected to anticoagulation therapy but clinically stable, and have no immediate surgical indications.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there is no conflict of interest.
Contributors: Trujillo L wrote the initial draft. All authors contributed to the design, interpretation of the study and revision of the paper.
REFERENCES
- 1.Cherry WB, Mueller PS. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore) 2006;85:105–110. doi: 10.1097/01.md.0000216818.13067.5a. [DOI] [PubMed] [Google Scholar]
- 2.Altman AM, Akers D. Rectus sheath hematoma secondary to a tussive paroxysm. J La State Med Soc. 2007;159:250–251. [PubMed] [Google Scholar]
- 3.Varol E, Ozaydin M. Rectus sheath hematoma due to cough attacks in an elderly patient on oral anticoagulant therapy. Anadolu Kardiyol Derg. 2007;7:235–236. [PubMed] [Google Scholar]
- 4.Johnson R. Abdominal wall injuries: rectus abdominis strains, oblique strains, rectus sheath hematoma. Curr Sports Med Rep. 2006;5:99–103. doi: 10.1007/s11932-006-0038-8. [DOI] [PubMed] [Google Scholar]
- 5.Tseng GS, Liau GS, Shyu HY, Chu SJ, Ko FC, Wu KA. Expanding refractory rectus sheath hematoma: a therapeutic dilemma. Diagn Interv Radiol. 2012;18:139–141. doi: 10.4261/1305-3825.DIR.4237-11.1. [DOI] [PubMed] [Google Scholar]
- 6.Moreno Gallego A, Aguayo JL, Flores B, Soria T, Hernández Q, Ortiz S, et al. Ultrasonography and computed tomography reduce unnecessary surgery in abdominal rectus sheath haematoma. Br J Surg. 1997;84:1295–1297. [PubMed] [Google Scholar]
- 7.Donaldson J, Knowles CH, Clark SK, Renfrew I, Lobo MD. Rectus sheath haematoma associated with low molecular weight heparin: a case series. Ann R Coll Surg Engl. 2007;89:309–312. doi: 10.1308/003588407X179152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salemis NS, Gourgiotis S, Karalis G. Diagnostic evaluation and management of patients with rectus sheath hematoma. A retrospective study. Int J Surg. 2010;8:290–293. doi: 10.1016/j.ijsu.2010.02.011. [DOI] [PubMed] [Google Scholar]


