Abstract
BACKGROUND:
Altered mental status (AMS) is a very common emergency case, but the exact etiology of many AMS patients is unknown. Patients often manifest vague symptoms, thus, AMS diagnosis and treatment are highly challenging for emergency physicians. The aim of this study is to provide a framework for the assessment of AMS patients. This assessment should allow providers to better understand the etiology of mental status changes and therefore improve diagnostic skills and management.
METHODS:
This is a prospective cohort observational study. We recruited all adult patients with undifferentiated AMS at a single center tertiary care academic emergency department over 24 months (June 2009 to June 2011). Demographic characteristics, clinical manifestations, assessment approaches, causative factors, emergency treatments and outcomes were collected prospectively.
RESULTS:
In 1934 patients with AMS recruited, accounting for 0.93% of all emergency department (ED) patients, 1 026 (53.1%) were male, and 908 (46.9%) female. Their average age was 51.95±15.71 years. Etiologic factors were neurological (n=641; 35.0%), pharmacological and toxicological (n=421; 23.0%), systemic and organic (n=266; 14.5%), infectious (n=167; 9.1%), endocrine/metabolic (n=145; 7.9%), psychiatric (n=71; 3.9%), traumatic (n=38; 2.1%), and gynecologic and obstetric (n=35; 1.9%). Total mortality rate was 8.1% (n=156). The death rate was higher in elderly patients (≥60) than in younger patients (10.8% vs. 6.9%, P=0.003).
CONCLUSIONS:
Patients with AMS pose a challenge for ED physicians. The most frequently encountered diagnostic categories causing AMS were primary CNS disorders, intoxication, organ system dysfunction, and endocrine/metabolic diseases. AMS has a high fatality rate in the ED. AMS is an important warning signal for ED patients because of its potentially fatal and reversible effects. Prompt evaluation and treatment are essential to decreasing morbidity and mortality associated with AMS.
KEY WORDS: Altered mental status, Emergency department, Demographic characteristics, Clinical feature, Assessment, Etiology, Mortality, Algorithm
INTRODUCTION
Altered mental status (AMS) comprises a group of clinical symptoms rather than a specific diagnosis, and includes cognitive disorders, attention disorders, arousal disorders, and decreased level of consciousness.[1] AMS is a very common emergency case, but the exact etiology of many AMS patients is unknown. Patients often manifest vague symptoms, thus, AMS diagnosis and treatment are highly challenging for emergency physicians. An in-depth understanding of the pathogenesis of AMS and complete patient assessment will help increase the diagnosis rate and ensure treatment accuracy.
Current epidemiological studies rarely focus on AMS with very few studies worldwide.[2] Nevertheless, in the standardization of the emergency department acuity level sponsored by a group emergency physicians at the Harvard medical school, AMS syndrome is significant to establish an emergency severe index (ESI) for which Level 1 is “no response” (most critical level) and Level 2 is “other acute changes in consciousness (drowsiness, mental confusion, disorientation, etc)” for timely diagnosis and efficient treatment.[3] This study aims to determine the demographic characteristics, clinical assessment methods, etiology, clinical prognosis, and emergency intervention strategies that are implemented among emergency AMS patients.
METHODS
Research design and subjects
This research was a prospective observational cohort study. The subjects of the study were 110 000 emergency patients at the medical center, a 2000-bed teaching hospital. The research duration was from June 1, 2009 to May 31, 2011. The study involved 207 450 emergency patients, in which 33 490 (16.1%) were elderly patients aged 60 years and over.
Research protocol
In this study, the clinical records of adult (≥14 years) AMS patients in the emergency department were collected by a previously designed case registration form which contained patient demographics, time and manner of admission, medical history, signs and symptoms upon admission (including vitals), laboratory tests, imaging data, etiology of diagnosis, clinical assessment methods, and emergency intervention/outcome. Suicidal motive and tendencies, history of mood disorders, anxiety, and psychotic symptoms were evaluated by a psychiatrist. All AMS patients were treated in the emergency department and subjected to observation for at least 24 hours from the time of admission to discharge. The patients who developed AMS symptoms during throughput in the emergency department were also included in the study.
Inclusion criteria
The subjects of the study needed to meet one of the following criteria:[2] Glasgow coma score <15; socially withdrawn and exhibits place and/or time disorientation; diminished or absent response to verbal or physical stimuli; somnolent; inability to maintain arousal; hallucinates; confusion; and other abnormally behavior.
Exclusion criteria
The research subjects were adult AMS patients. Children aged <14 years were excluded because of their poor representation (small sample size). This study focused on AMS patients with acute exacerbation and symptoms lasting for <1 week; hence, chronic AMS patients such as those with Alzheimer’s and schizophrenia, or those with AMS symptoms for more than 1 week were excluded. Patients who had experienced one-time AMS symptoms prior to hospitalization, with symptoms disappearing prior to emergency treatment, as well as those who experienced loss of consciousness or cardiac arrest during emergency treatment were excluded.
A total of 1 934 qualified AMS patients were included in this study. Among them, 1 727 exhibited AMS (89.3%) prior to emergency treatment and 207 exhibited AMS (10.7%) during emergency treatment. The collected research data were retrospectively analyzed by an independent group of physicians (two emergency department physicians, a neurologist, and a psychiatrist) to determine the origin of symptoms and identify an emergency method for diagnosis. Almost 1 831 AMS patients (94.7%) were diagnosed at the time of hospital discharge.
Research grouping
The patients were divided into groups according to age, i.e., elderly (>60 years) and non-elderly (≤60 years), as well as according to AMS etiology, i.e., primary nervous system and non-nervous system factors.
Statistical analysis
In this study we utilized the SPSS 17.0 statistical software for data analysis. Statistical data were compared using the chi-square test where P <0.05 was considered statistically significant.
RESULTS
Demographic characteristics
In the 1 934 AMS patients collected, accounting for 0.93% of the total emergency patients, 1 026 were male (53.1%) and 908 female (46.9%); their age ranged from 14 to 97 years (average age 51.95±15.71 years). Almost 701 patients were <40 years (36.3%), 436 were 40–60 years (22.5%), and 797 were>60 years (41.2%). Figure 1 shows the age distribution of emergency patients as a bi-peak distribution; the first peak was for patients aged 33 years, and the second peak was for patients aged 72 years.
Figure 1.
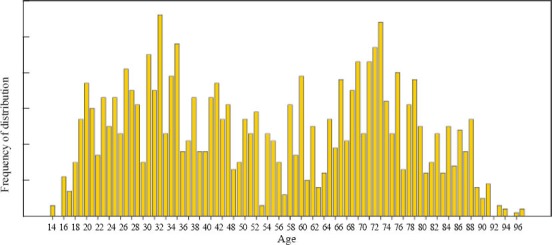
Frequency of occurrence based on the specific age of the participants.
The modes of patient arrival to the hospital were as follows: ambulance (43%), private car or taxi (34%), ambulatory (20%), and police car (3%). The places of origin prior to hospital arrival were as follows: home or work/study places (71%), on the way to the hospital (12%), other hospitals (11%), nursing home (3%), and police department (3%). The times of hospital arrival were as follows: 8 am–5 pm (44%), 6 pm–11 pm (39%), and 12 am–7 am (17%). The onsets of AMS symptoms prior to hospital arrival were as follows: <2 hours (40%), <12 hours (33%), <24 hours (15%), <3 days (6%), and <1 week (6%).
AMS classification and composition
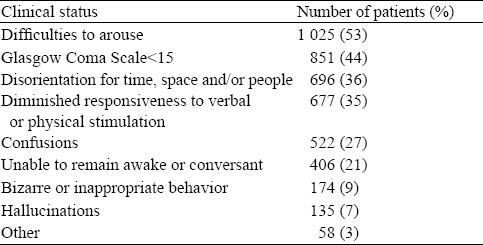
Patients were classified according to AMS symptoms from total loss of consciousness to extreme excitation, and were categorized as follows: 1) central nervous system inhibition: coma, drowsiness, and confusion; 2) central nervous system stimulation: irritability and aggressiveness; and 3) abnormal behavior. The first category accounted for 70%; 24% of the patients in this group were unresponsive to pain and verbal stimuli and 46% were deeply asleep or had waking-up difficulty. The second category accounted for 12%, and third category accounted for 18%. Table 1 shows the proportional composition of the clinical manifestations according to the AMS standards (a patient may meet more than one AMS standard).
Table 1.
Disease profile for AMS patients in the emergency department
Emergency assessment of AMS
Analysis of the assessment method used for the causative diagnosis of AMS in patients showed that routine emergency assessment methods were important for accurate diagnosis. The clinical values of the diagnostic evaluation were as follows: patients diagnosed by history of disease (40%), by previous history of AMS (including medication history) (32%), by physical examination (21%), by treatment responses (19%), and by all four assessment methods (60%). The other diagnostic assessment methods used were imaging examinations (16%), 12-lead ECG (3%), laboratory tests (13%; 5% on arterial blood gas, 5% on blood chemistry, 2% on routine urinalysis, 1% on complete blood count, and 0% coagulation studies). Diagnosis aided by a brain CT scan accounted for 82% (n=1 585), whereas abnormal CT scans accounted for 45%. However, diagnosis of the cause of AMS by CT alone accounted for only 15% (237/1 585), and that by electroencephalogram (EEG) alone accounted for 1% (n=18).
Etiological analysis of AMS
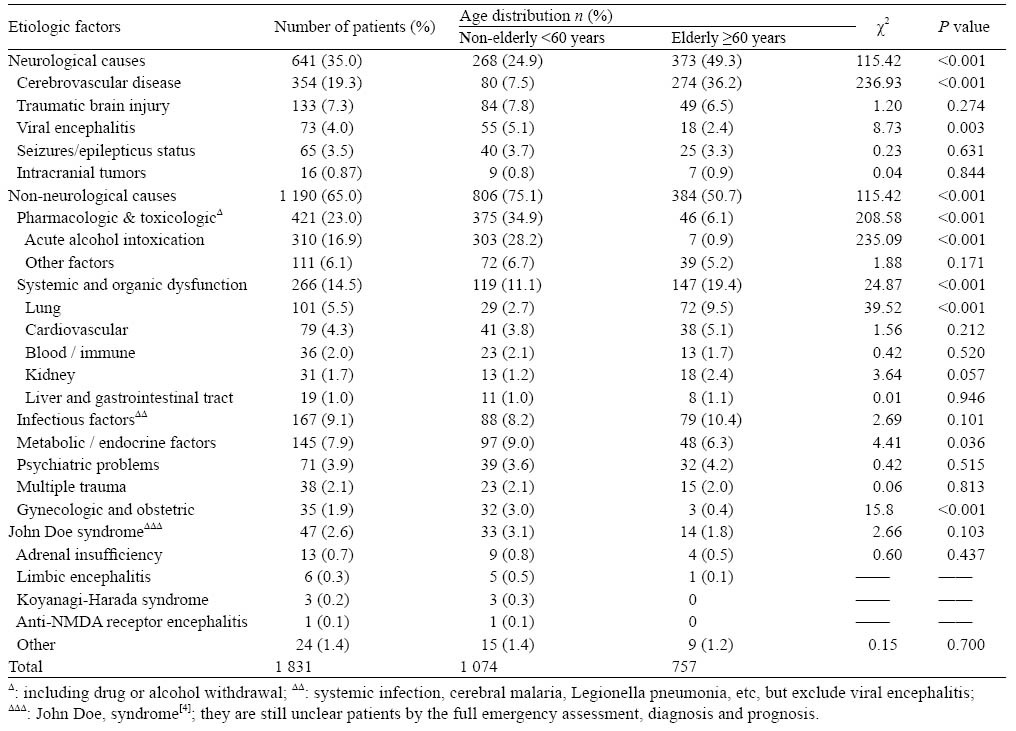
The causes of 1 831 AMS patients were confirmed. However, 5.3% of all patients remained undiagnosed. Neurological causes (stroke, head trauma, or mass lesion) accounted for 35.0% (n=641), whereas 65.0% originated from non-neurological factors (n=1 190). Table 2 shows the causative composition of AMS according to the age group. For the elderly group, the top three causes of AMS were cerebrovascular disease (36.2%), system and organ dysfunction (19.4%), and infection (10.4%). For the middle-aged and young groups, the top three causes were drugs or toxic factors (34.9%), system and organ dysfunction (11.1%), and metabolic/endocrine factors (9.0%). Both age groups had a significant difference in the constituted etiology (P<0.001).
Table 2.
Etiologic factors of AMS in different age groups (n=1 831)
Emergency intervention and clinical outcomes
Among the 1 934 AMS patients in the emergency department, 4.9% (n=94) were assessed by triage as level 1 and admitted to the critical care unit. The average length of the hospital stay was 3.8 days, during which 11% of the patients needed medication to restrict movement and 23% required physical limitations. About 28% (n=540) of the patients were treated in the emergency room and subsequently discharged, 2% (n=39) were voluntarily discharged (left against medical advice), 17% (n=329) were admitted to the emergency ward, 26% were admitted to the ICU or EICU (average length of stay in ICU was 10.8 days, n=503), 20% (n=385) admitted to the relevant inpatient clinic, and 7% referred to other hospital (n=138).
During the study, 144 AMS patients (7.4%) were treated with tracheal intubation and 156 patients died (including some patients who voluntarily discharged because of very poor prognosis). The mortality rate was 8.1%, and 74% (n=116) of the patients died in the emergency department and 26% (n=40) died in the wards. Within the same period, the total death rate in the ED critical care unit was 8.9% (477/5 360). The main causes of death were system and organ failure (n=49), cerebrovascular disease (n=42), and trauma (n=34). The numbers of fatal patients were 82 in the elderly group and 74 in the non-elderly group. The mortality rate of the elderly group was significantly higher than that of the non-elderly group (10.8% vs. 6.9%, P=0.003).
DISCUSSION
Demographic data
AMS may be found in 4%–10% of ED patients, this proportion may be higher in special subgroups (such as in the elderly patients).[5,6] However, in our study, AMS patients only represented 0.93% of total emergency patients and 2.38% in the elderly-patient subgroup (797/33, 490). This was significantly lower than previous data that may be related to the following reasons: 1) the current exclusion criteria were more stringent than those of the previous study; and 2) part of intellectually disabled patients (detected by mini mental score examination, MMSE) had not been recruited in our study because MMSE is not commonly used in the emergency setting.
Our data showed that age distribution of AMS patients had two peak segments (the first peak was for patients aged 33 years, and the second peak was for those aged 72 years) as a result of the distinct etiology of AMS among the two age groups. Subsequent analysis revealed that the causative disease of AMS in the elderly group differed from that in the non-elderly group, i.e., metabolic diseases, trauma, and poisoning were often found in young people, whereas cerebral vascular disease, and organ/system failure were frequently seen in the elderly. In acute AMS, this pattern of age distribution was similar to Kanich and his colleague’s research.[7]
Emergency assessment
The emergency assessment of AMS is very difficult because of incomplete and inaccurate disease histories provided by the patient. Emergency physicians focused on the acute physical diseases and past history often ignore details of acute mental changes in patients. Data from one single-center study showed that misdiagnosis of AMS patients was as high as 75% in delirium patients of more than 65 years old.[8] In a report,[9] 4% of the patients admitted to the psychiatric ward were forcibly transferred because of urgent medical rescue, suggesting that the assessment capacity of emergency physicians with regard to AMS should be strengthened.
A study[10] showed that the medical history and physical examination are more important than laboratory testing and imaging in the diagnostic evaluation of AMS. Physical examination also helps determine the development of the condition. The medical history, physical examination, past history, and treatment responses of patients are important in assessing the causes of AMS. Our data indicated that the use of the four basic tools could provide 60% of emergency AMS patients with a clear diagnosis of its cause. CT can reveal several intracranial space-occupying diseases, intracranial bleeding, and structural brain damage. However, more patients with AMS exhibited negative CT results.
In the present study, the CT diagnosis rate for AMS etiology was only 15%. An over reliance on CT scan probably lead to serious negative impacts on the assessment and treatment of non-neurological causes involved in the pathogenicity of AMS, such as hypoglycemia. However, researchers argued that the value of CT-head should not be underestimated, even when the CT-head report was negative, because the AMS patients with acute poisoning CT scan can help to elucidate whether or not combined with brain injury.[11] In our study, CT-head exhibited the highest negative rate in terms of AMS diagnosis, suggesting that emergency physicians no longer wait for the results of CT that may lead to delayed assessment and treatment.
The value of EEG in the assessment of the causes of emergency AMS is not certain. In our study, the application rate of EEG in the AMS patients was 1%, which was much lower than that reported previously.[12] A study[13] showed that the cerebrospinal fluid analysis of acute AMS in the elderly had a positive rate of 24% (10/42) for febrile and 18% (15/84) for afebrile patients. AMS assessment remains highly challenging among emergency physicians in terms of combining the four basic assessment tools and reasonably choosing methods of imaging, blood biochemistry, cerebrospinal fluid, and EEG assessment for the diagnosis of AMS. Thus, further related explorations are necessary.
Etiology of AMS
The variety of pathogenic factors that cause several clinical manifestations of AMS results in significantly different clinical treatment. Therefore, determining the cause of AMS is very important. Currently, most emergency medicine literature focuses on the AMS subgroup such as comatose patients, whose coma state may have triggered AMS. Generally, the etiology of emergency AMS is categorized into two factors: primary nervous system and non-neurological factors.[2] A recent study[14] considered neurological events to be the most important factors that cause AMS, and account for about 28% of AMS patients.
In our study the AMS proportion caused by primary nervous system factors was 35%, almost 50% in the elderly people. Despite the events in the nervous system as the most common reason for acute AMS, more than half of the AMS patients were caused by non-nervous system factors. We also found that in the elderly group, the top three causes of AMS were cerebrovascular disease, systemic and organic failure, and infection. In the non-elderly group, the top three causes were drugs and toxic factors, systemic and organic failure, and metabolic and endocrine disorders.
The non-neurological causes of AMS in the emergency department included drugs and substance intoxication, infection, metabolic endocrine abnormalities, trauma, cancer, and system/organ dysfunction.[15] Among these causes, acute alcoholism was considered to be the main factor out of AMS neurological causes. In our study, drugs and toxic factors (alcoholic and non-alcoholic factors) accounted for 23%; in the non-elderly group, it was as high as 34.9%. Besides, system and organ dysfunction was a significant cause of acute AMS. Primarily, the lungs and cardiovascular system accounted for 9.8% of the AMS patients. Thus, organ failure in AMS patients is an important factor and potentially fatal.
Trauma and infection are two important factors that cause acute AMS. Yagmur et al[16] reported trauma as the second largest cause of emergency AMS and that trauma accounts for 39% of all AMS deaths, primarily head trauma. However, the etiology of AMS is not consistent in all countries and regions. Infection is thought to be the most common factor of non-traumatic AMS, and cerebral malaria is the primary cause of AMS in Ethiopia and Zambia.[17] Therefore, several uncommon factors known to cause AMS should be considered, such as acute fatty liver of pregnancy, environment-related diseases, and adrenal insufficiency because of the potentially fatal and reversible damage inflicted by AMS.
Emergency treatment
Acute AMS is potentially life-threatening.[1] AMS should be considered in the comprehensive treatment of ED conditions and serve as an admission criterion. In the ESI triage tool (4th editor), Acute AMS is usually divided into level 1 (no response; the most dangerous level) or level 2 (lethargy, mental confusion, disorientation).[3] In our study, only 4.9% of AMS patients triaged as level 1 were sent to the ED critical care unit. However, the actual case fatality rate of AMS was as high as 8.1%, close to the ED critical care unit mortality of 8.9% within the same period, which indicated that emergency physicians lack sufficient knowledge on the seriousness of AMS. At the onset of symptoms of acute AMS, these patients, especially elderly patients should be immediately treated, closely monitored, and rapidly assessed, Algorithm (Figure 2) shows the clinical intervention strategy of AMS patients based on the constituted cause, risk factor, necessary interventions.
Figure 2.
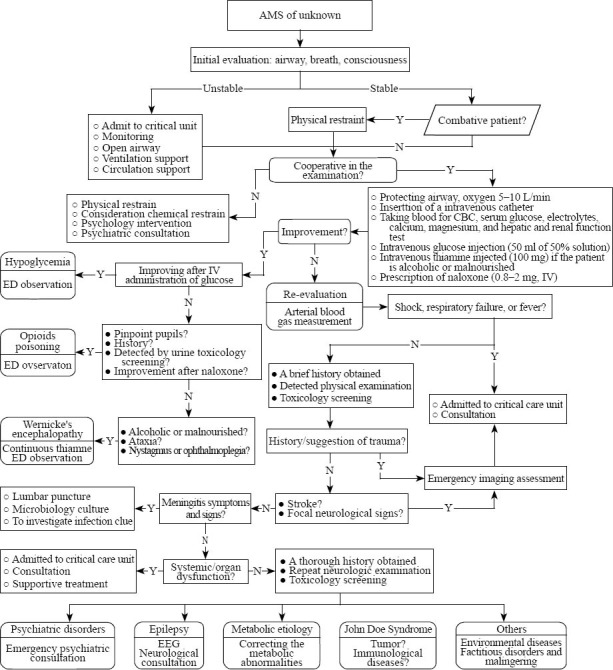
Algorithm for AMS patient assessment and treatment in ED.
The cause of AMS in patients cannot be clearly detected from its initial onset in the ED. Some patients diagnosed in the ward as having the John Doe syndrome,[4] such as adrenal insufficiency, limbic encephalitis, and anti-NMDA receptor encephalitis, which often correspond to high fatality rates and risks of disability. Interestingly, glucocorticoid action is usually rapid and effective in these diseases. A newly published article reported that anti-NMDA receptor encephalitis due to ovarian teratoma should make clinicians to take the disease seriously.[18] Patients can be cured after teratoma removal. However, with untime diagnosis, the disease often progress to muscle weakness and respiratory failure, which are ultimately life-threatening. Therefore, full emergency assessment and immediate life-saving interventions remain a challenge for emergency physicians.
Limitations
Firstly, emergency physicians lack adequate understanding of AMS because of its complex clinical features, which results in some missed AMS patients, particularly in elderly patients with chronic cognitive impairment. Secondly, this study was only a single-center investigation. Our data may not represent the same situation encountered in other emergency departments. Thus, emergency physicians need to be cautious in the application and interpretation of results. Thirdly, we failed to fully capture all assessment factors that place patients at risk of death (such as C-reactive protein, lactic acid, etc.) because we underrated the risk of this acute condition. Therefore, further research is needed to assess the risk of death of AMS patients.
In conclusion, a systematic analysis of acute AMS patients reveals that the common causes of AMS are primary neurological factors, drug and poisoning, system/organ dysfunction, and metabolic and endocrine factors. The etiology of AMS is significantly different in various age groups. The reversibility of diseases and the potentially fatal factors associated with AMS require timely assessment and rapid intervention for the potential causes and conditions of the disease.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Ethical Committee of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China.
Conflicts of interest: There are no competing interests involving this study.
Contributors: Xiao HY proposed and wrote the paper. All authors approved the final version.
REFERENCES
- 1.American College of Emergency Physicians. Clinical policy for the initial approach to patients presenting with altered mental status. Ann Emerg Med. 1999;33:251–280. doi: 10.1016/s0196-0644(99)70406-3. [DOI] [PubMed] [Google Scholar]
- 2.Kekec Z, Senol V, Koc F, Seydaoglu G. Analysis of altered mental status in Turkey. Int J Neurosci. 2008;118:609–617. doi: 10.1080/00207450701849133. [DOI] [PubMed] [Google Scholar]
- 3.Storm-Versloot MN, Ubbink DT, Kappelhof J, Luitse JS. Comparison of an informally structured triage system, the emergency severity index, and the manchester triage system to distinguish patient priority in the emergency department. Acad Emerg Med. 2011;18:822–829. doi: 10.1111/j.1553-2712.2011.01122.x. [DOI] [PubMed] [Google Scholar]
- 4.Claps PJ, Berk WA. The John Doe syndrome: diagnosis and outcome of patients unidentified at the time of emergency department admission. Am J Emerg Med. 1992;10:217–218. doi: 10.1016/0735-6757(92)90212-G. [DOI] [PubMed] [Google Scholar]
- 5.Erkinjuntti T, Wikström J, Palo J, Autio L. Dementia among medical inpatients: Evaluation of 2000 consecutive admissions. Arch Intern Med. 1986;146:1923–1926. [PubMed] [Google Scholar]
- 6.Wofford J, Loehr L, Schwartz E. Acute cognitive impairment in elderly ED patients: Etiologies and outcomes. Am J Emerg Med. 1996;14:649–653. doi: 10.1016/S0735-6757(96)90080-7. [DOI] [PubMed] [Google Scholar]
- 7.Kanich W, Brady WJ, Huff JS, Perron AD, Holstege C, Lindbeck G, et al. Altered mental status: Evaluation and etiology in the ED. Am J Emerg Med. 2002;20:613–617. doi: 10.1053/ajem.2002.35464. [DOI] [PubMed] [Google Scholar]
- 8.Han JH, Zimmerman EE, Cutler N, Schnelle J, Morandi A, Dittus RS, et al. Delerium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16:193–200. doi: 10.1111/j.1553-2712.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tintinalli J, Peacock F, Wright M. Emergency medical evaluation of psychiatric patients. Ann Emerg Med. 1994;23:859–862. doi: 10.1016/s0196-0644(94)70326-4. [DOI] [PubMed] [Google Scholar]
- 10.Mistovich JJ, Krost WS, Limmer DD. Beyond the basics: interpreting altered mental status assessment findings. EMS Mag. 2008;37:90–97. [PubMed] [Google Scholar]
- 11.Leong LB, Wei Jian KH, Vasu A, Seow E. Identifying risk factors for an abnormal computed tomographic scan of the head among patients with altered mental status in the Emergency Department. Eur J Emerg Med. 2010;17:219–223. doi: 10.1097/MEJ.0b013e328331dde5. [DOI] [PubMed] [Google Scholar]
- 12.Bautista RE, Godwin S, Caro D. Incorporating abbreviated EEGs in the initial workup of patients who present to the emergency room with mental status changes of unknown etiology. J Clin Neurophysiol. 2007;24:16–21. doi: 10.1097/WNP.0b013e318030e8cb. [DOI] [PubMed] [Google Scholar]
- 13.Shah K, Richard K, Edlow JA. Utility of lumbar puncture in the afebrile vs. febrile elderly patient with altered mental status: a pilot study. J Emerg Med. 2007;32:15–18. doi: 10.1016/j.jemermed.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 14.Koita J, Riggio S, Jagoda A. The mental status examination in emergency practice. Emerg Med Clin North Am. 2010;28:439–451. doi: 10.1016/j.emc.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Nassisi D, Korc B, Hahn S, Bruns J, Jr, Jagoda A. The evaluation and management of the acutely agitated elderly patient. Mt Sinai J Med. 2006;73:976–984. [PubMed] [Google Scholar]
- 16.Yagmur Y, Kiraz M, Kara IH. Looking at trauma and deaths: Diyarbakir city in Turkey. Injury. 1999;30:111–114. doi: 10.1016/s0020-1383(98)00230-7. [DOI] [PubMed] [Google Scholar]
- 17.Melka A, Tekie-Haimanot R, Assefa M. Aetiology and outcome of non-traumatic altered states of consciousness in north western Ethiopia. E Afr Med J. 1997;74:49–53. [PubMed] [Google Scholar]
- 18.Sameshima A, Hidaka T, Shima T, Nakashima A, Hasegawa T, Saito S. Anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian immature teratoma. J Obstet Gynaecol Res. 2011;37:1883–1886. doi: 10.1111/j.1447-0756.2011.01671.x. [DOI] [PubMed] [Google Scholar]


