Abstract
BACKGROUND:
This study aimed to determine the potential protective effect of inducing hypertransfusion to the gastrointestinal tract following a porcine model of cardiac arrest and cardiopulmonary resuscitation (CPR) by evaluating the influence of gastrointestinal ultrastructure, ATPase and serum diamine oxidase.
METHODS:
Ventricular fibrillation was induced by programmed electrical stimulation in 16 male domestic pigs (n=8/group). Four minutes after ventricular fibrillation, CPR was performed. The pigs that successfully restored spontaneous circulation received intravenous infusion of either norepinephrine to maintain the mean arterial pressure at 130% of the baseline before ventricular fibrillation or normal saline. Serum diamine oxidase and gastrointestinal ATPase activity were determined, and histopathological examination of the gastrointestinal tract was performed by light and electron microscopy.
RESULTS:
CPR caused significant injury to the gastrointestinal tract, elevating serum diamine oxidase and causing destruction of intestinal microvillus in control animals. Na+-K+ ATPase and Ca2+ ATPase activity in gastric tissue were significantly elevated in animals receiving hypertransfusion treatment compared with the control animals. Hypertransfusion also significantly reduced serum diamine oxidase to below control levels after CPR. Moreover, severe injury sustained by the gastrointestinal tissue was markedly ameliorated under hypertransfusion conditions compared with the control animals.
CONCLUSIONS:
Gastrointestinal injury and abnormal energy metabolism were strikingly evident following CPR. Hypertransfusion inducing hypertension can improve energy metabolism and ameliorate gastrointestinal mucosal injury, indicating that hypothermia significantly ameliorates gastrointestinal injury sustained following cardiac arrest.
KEY WORDS: Cardiopulmonary resuscitation, Cardiac arrest, Gastrointestinal tract, Diamine oxidase, Ultra structure
INTRODUCTION
Although the research on cardiopulmonary resuscitation (CPR) has been conducted for half a century, the final prognosis of patients after restoration of spontaneous circulation (ROSC) has not been improved.[1] The high mortality is primarily due to multiple organ dysfunction syndrome (MODS), the result of a systemic reaction to ischemia-reperfusion injury; the gastrointestinal tract is recognized as the initiating organ.[2] During cardiac arrest and resuscitation, the sensitivity of the gastrointestinal tract to ischemia is, in fact, equal to or greater than that of the brain.[3] Therefore, protection of the gastrointestinal tract is a critical factor in determining patient prognosis following CPR. Studies[4,5] have demonstrated that to maintain relatively high mean arterial pressure (MAP) after CPR may improve the prognosis of the nervous system. However, there are few studies investigating the extent of gastrointestinal injury following CPR, nor test methods to protect the gastrointestinal tract from CPR-induced injury. The present study was to investigate the effect of hypertransfusion on the gastrointestinal tract after CPR in a procaine model by observing enzymological and ultrastructural changes, and then determine the protective effect of relatively high MAP maintained by infusing norepinephrine after CPR on the gastrointestinal tract.
METHODS
Animal preparation
Sixteen male domestic pigs, 8-10 weeks, 27±2 kg, were purchased from Beijing Experimental Animal Center (license number: SCXK 11-00-002). The pigs were fasted for the night prior to the day of experimentation, with water available ad libitum. Propofol 1 mg/kg was given by a bolus injection via a peripheral ear vein cannulation. Anesthesia was maintained by continuous intravenous infusion of pentobarbital (8 mg/kg per hour) with saline infused continuously (10 mL/kg per hour) together. All animals were intubated by a cuffed 6.5-mm endotracheal tube and maintained in a surgical plane for mechanically ventilation (Sero900c, Siemens, Germany) at a rate of 12/min and tidal volume (TV) of 15mL/kg with room air. The parameters of the ventilator were properly regulated to maintain an end-tidal CO2 (ETPCO2) of 35-40 mmHg. An angiographic catheter was inserted into the right femoral artery for blood pressure monitoring. A Swan-Ganz catheter (7F, Edwards Life Sciences, USA) connected to a Vigilance II CCO monitor (Edwards Life Sciences, USA) was inserted into the left femoral vein and flow-directed into the pulmonary artery to monitor the hemodynamics. The right external jugular vein was punctured to insert an 8F sheathing canal to provide the route for liquid infusion and placement of pacing electrode.
Experimental protocols
A temporary pacemaker conductor was placed into the right ventricle via the sheathing canal in the jugular. The external end of the conductor was connected to a programmed electrical stimulator (GY-600A, Kai Feng Huanan Instrument Company, China). Electric stimulation was continuously performed with S1S2 mode (300/200 ms), 8:1 proportion and -10 ms pace length until ventricular fibrillation (VF) was induced. Cardiac arrest was defined as VF on the ECG and the loss of arterial pulsation; ventilation stopped at this time. After 4 minutes of VF, manual closed-chest CPR was immediately carried out for 2 minutes at a frequency of 100 compressions/min and a compression/ventilation ratio of 30/2 using 100% O2. If the waves of VF were still displayed on the monitor, defibrillation with 150J of diphase wave was performed once, and another cycle of 2-minute CPR was performed immediately. The procedure was repeated with the same defibrillation shock energy unless ROSC was accomplished. Compressions were haled for 10 seconds before another shock was performed to observe the rhythm of ECG. ROSC was defined as more than 10 consecutive minutes of maintenance of systolic blood pressure above 50 mmHg.[6] If spontaneous circulation was not restored within 15 minutes, the pig was thought to be dead.
After ROSC, the animals were randomly divided into two groups: a hypertransfusion group and a control group. In the hypertransfusion group, norepinephrine was infused continuously for 4 hours to maintain the mean arterial pressure (MAP) at about 130% of the baseline before ventricular fibrillation. In the control group, the baseline MAP was maintained. All animals were monitored for 4 hours. During the experiment protocol, the hemodynamics was recorded according to the designed time points. The drained blood samples were analyzed. After ROSC 24 hours, the animals were sacrificed with over-dose of anesthetics and dissected for measurement of their gastrointestinal tissues.
Measurements
Hemodynamic parameters, such as heart rate (HR), cardiac output (CO), systolic arterial pressure (SAP), diastolic arterial pressure (DAP) and mean arterial pressure (MAP) were measured at the baseline and 10 minutes, 60 minutes, 1 hour, 2 hours, 3 hours and 4 hours post-ROSC.
Oxygen metabolism parameters, such as oxygen supply (DO2), oxygen consumption (VO2) and oxygen extraction ratio (ERO2) were calculated by blood-gas analyses at baseline, 2 hours and 4 hours post-ROSC.
Colorimetric method was used to measure the activity of serum diamine oxidase (DAO). Each liter of serum can catalyze to form 1 μmol dihydrouracil dehydrogenase (Jiancheng Bioengineering Institute, Nanjing, China) at 37°C meant one unit (U) of enzymatic activity.
After the pig was sacrificed, gastrointestinal tissues were dissected to detect the Na+-K+ ATPase and Ca2+ ATPase by the spectrophotometric method. ATPase in each milligram of tissue protein that can decompose ATP (Jiancheng Bioengineering Institute, Nanjing, China) to produce 1 μmol inorganic phosphorus in each hour is one unit (U) of ATPase activity. The pathological and ultrastructural changes of gastrointestinal tissues were observed by light and electron microscopes (Hitachi Ltd., Tokyo, Japan) respectively.
Statistical analysis
Data were reported as mean±SD. Repeated measures ANOVA and multivariate ANOVA were used to determine the difference between each time point in the two groups in each time point respectively. A value of P<0.05 or P<0.01 was regarded as significant or very statistically significant respectively
RESULTS
Outcomes
Seven swine in each group were ROSC successfully, and one died in each group. The duration of CPR before ROSC was 430±96 seconds and shocks before ROSC were 1.45±0.72. There were no significant differences between two the groups (P>0.05).
Hemodynamic parameters
After ROSC, norepinephrine was administered in the latter group to maintain the mean arterial pressure (MAP) at about 130% of the baseline before ventricular fibrillation in a period between 10 minutes to 4 hours after ROSC. MAP, HR and CO in this period were significantly higher in the hypertransfusion group than in the control group (P<0.05) (Figure 1).
Figure 1.
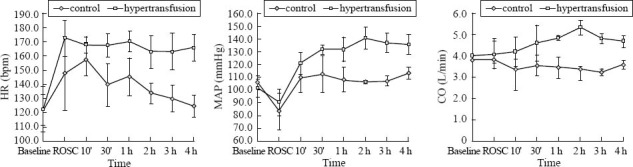
The changes of HR, MAP, and CO during the protocol between the control and hypertransfusion groups.
Oxygen metabolism
There were no significant differences in VO2, DO2 and ERO2 of baseline between the two groups. The levels of DO2 at 2 and 4 hours after ROSC in the hypertransfusion group were much higher than those in the control group (P<0.01), while the levels of VO2 were approximately the same in the two groups. The levels of ERO2 at 2 and 4 hours after ROSC were significantly lower in the hypertransfusion group than in the control group (P<0.05) (Figure 2).
Figure 2.
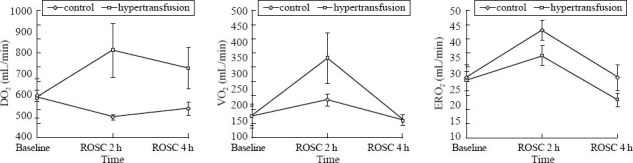
The changes of DO2, VO2, and ERO2 during the protocol between the control and hypertransfusion groups.
Changes of enzyme
No significant difference of serum DAO of baseline between the two groups was found. After ROSC at 2 and 4 hours, the levels of DAO of the control group were obviously higher than those before the ventricular fibrillation (P<0.05). There were significant differences, but these differences disappeared in the hypertransfusion group. At the same time, significant differences were found between the two groups (P<0.05) (Table 1).
Table 1.
The changes of DAO in serum of the two groups
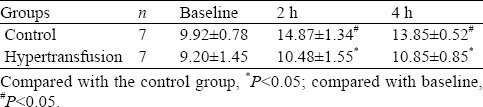
In the intestinal tissue, no significant differences of these two types of ATPase were found between the two groups at 24 hours after ROSC (P>0.05). However, they were higher in the hypertransfusion group than in the control group. In the gastric tissue, their activities after ROSC in the hypertransfusion group were much higher than those in the control group (P<0.05) (Table 2).
Table 2.
Intestinal and gastric tissue ATPase of the two groups 24 hours after ROSC (U/L)
Histopathological alterations
The slice of gastric tissue was observed with a light microscope. In the control group, the gastric mucosal epithelium was not complete; the cells of lamina propria were arranged loosely and disorderly; the structure of intestinal villi was nearly complete, but there were many inflammatory cells infiltrating, indicating ischemic changes. In the hypothermia group, the gastric mucosa was complete while the structure of intestinal villi was also complete (Figure 3).
Figure 3.
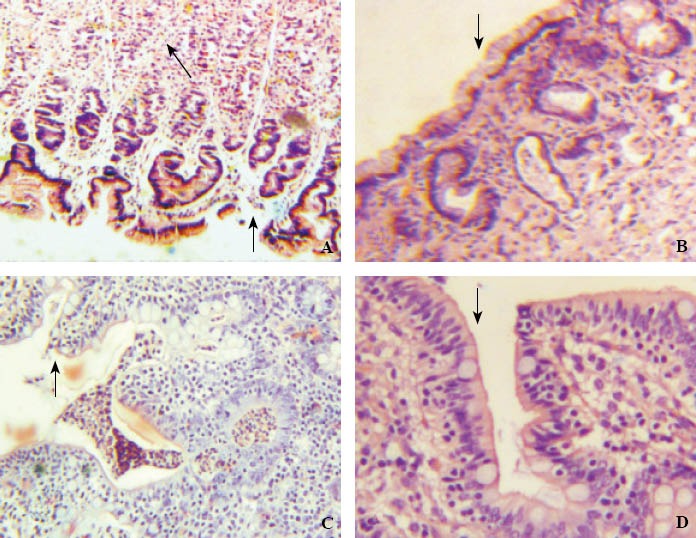
The pathological changes of gastrointestinal tissue structures observed by a light microscope in the control and hypothermia groups.
A: Gastric mucosa (×100) showing defect of mucosal epithelial cells (black arrow), the arrangement of cells in lamina propria layer loose and disordered, representing ischemic changes (white arrow head) in the control group; B: Gastric mucosa (×100) showing mucosal epithelium complete (black arrow head) in the hypertransfusion group; C: Intestinal mucosa (×100) showing the structure of intestinal villi basically complete, but the arrangement of cells irregular (black arrow) and a plenty of inflammatory cells in the mucosal layer (white arrow) in the control group; D: Intestinal mucosa (×400) showing the structure of intestinal villi complete and the arrangement of cells regular and dense (black arrow) in the hypertransfusion group.
The ultra-structure was observed by an electron microscope. Twenty-four hours after CPR, the gastric mitochondria were seriously injured, highly swollen with their ridges fragmental in the control group. While in the hypertransfusion group, the injury of gastric mitochondria was milder than that in the control group. The structure of mitochondria was complete with only their ridges hazy (Figure 4).
Figure 4.
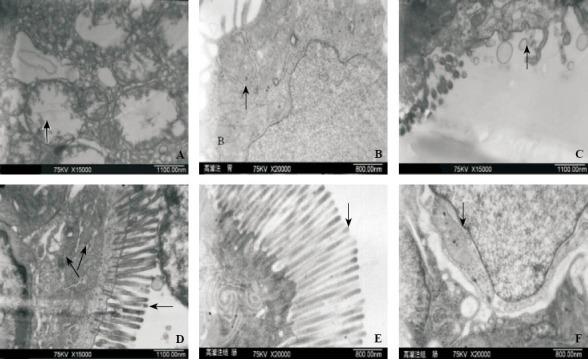
The pathological ultra-structural changes of gastric tissues observed with an electron microscope in the control and hypothermia groups.
A: Gastric mitochondria were highly swollen; vacuole–like changes with ridges fragmental could be observed (black arrow) in the control group; B: The structure of gastric mitochondria was complete with their ridges relatively clear (black arrow) in the hypertransfusion group; C: Defect of part of intestinal microvilli (black arrow) in the control group; D: In the control group, the arrangement of intestinal microvilli loose (black arrow) and the structure of intestinal mitochondria not distinct with their ridges hazy (black arrow); E: The arrangement of intestinal microvilli dense and regular (black arrow) in the hypertransfusion group; F: The intestinal mitochondria with their ridges manifesting basically clear (black arrow) in the hypertransfusion group.
DISCUSSION
The elevation of blood pressure can increase tissue perfusion, and administration of vasoactive drugs during CPR may improve the perfusion pressure in coronary and cerebral arteries,[7] which may improve the energetic condition during CPR. In the selection of drugs for increasing the blood pressure about shock in recent years, norepinephrine has shown to be effective for improving blood flow of the viscera.[8,9] So we used norepinephrine to increase the blood pressure and found that in the hypertransfusion group, CO and HR were significantly increased after blood pressure increased, resulting in DO2 in this group much higher than that in the control group, then improving tissue oxygen supply. Although VO2 was increased simultaneously in the hypertransfusion group, ERO2 was lower than that in the control group, indicating that hypertransfusion was effective to improve the oxygen metabolism.
There are many parameters that can be used to detect cardiac, liver and renal functions clinically. However, the parameters used to determine the gastrointestinal functions are few. In this experiment, DAO was chosen as a parameter to monitor the function of intestinal barrier. DAO is a specific cytoplasm enzyme of intestinal mucosal upper layer villus cells. When intestinal mucosal cells are injured or necrotic, DAO was released into the blood stream, leading to an elevation of plasma DAO level. Thus, the activity of DAO in the peripheral blood may reflect the integrity and the severity of intestinal mucosa injury. Some experimental and clinical studies have shown that DAO can be a sensitive parameter to reflect the severity of intestinal mucosal injury in the condition of extracorporeal circulation and MODS.[10] In our experiment, we found that the serum DAO was significantly increased in the control group at 2 hours after CPR and maintained high till 4 hours. Its increase was significantly depressed in the hypertransfusion group, demonstrating that the intestinal injury at early stage after CPR and the protecting effect of hypertransfusion to the gastrointestinal tract.
In this experiment, the activities of gastrointestinal tissue Na+-K+ ATPase and Ca2+ ATPase after CPR were detected. In intestinal tissues, these two types of ATPase in the hypertransfusion group were higher than those in the control group, but no statistical significant differences were found. In the gastric tissues, these two types of ATPase in the hypertransfusion group were obviously higher than those in the control group (P<0.05), suggesting that elevation of systemic blood pressure could improve the energy metabolism, enhance ATPase activity and have an affirmative protection to the gastrointestinal tract.
The mitochondria in cells are very sensitive to ischemia. In this experiment, we found that the gastrointestinal mitochondria were highly swollen with their ridges fragmental after CPR in the control group under an electron microscope; whereas in the hypertransfusion group, the structure of gastric mitochondria was hazy with their ridges still capable to be identified, and the intestinal mitochondrial ridges were relatively clear. The outcomes demonstrated that mitochondria were damaged seriously after CPR and hypertransfusion could protect the ultra-structure of cells. The results of electron microscope examination and ATPase were basically consistent each other, showing that hypertransfusion might enhance oxygen supply and, in turn, improve cell energy metabolism. In the previous study, the blood flow of the intestinal mesenteric artery after CPR could be increased effectively by hypertransfusion.[11] In addition, the intestinal microvilli were loose or defective in the control group, but they were basically normal in the hypertransfusion group, demonstrating that hypertransfusion had protective effect on intestinal mucosa.
In conclusion, after CPR and ROSC in a porcine model of cardiac arrest, norepinephrine was used to elevate the systemic blood pressure, which could improve oxygen transportation, reduce the oxygen extraction rate and improve tissue perfusion of gastrointestinal energy metabolism. Its protective effect was confirmed histopathologically under light and electron microscopes. The injuries of gastrointestinal mucosa and microvillus mitochondria in the hypertransfusion group were milder than those in the control group, indicating that the elevation of systemic blood pressure induced by norepinephrine after CPR had protective effect on the gastrointestinal tract.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: There is no conflict of interest regarding the contents of this study. None of the authors is affiliated with any of the companies whose products were used. Manufacturers were not involved with this study.
Contributors: Lu Y proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 2.Swank GM, Deitch EA. Role of the gut in multiple organ failure: bacterial translocation and permeability changes. World J Surg. 1996;20:411–417. doi: 10.1007/s002689900065. [DOI] [PubMed] [Google Scholar]
- 3.Korth U, Krieter H, Denz C, Janke C, Ellinger K, Bertsch T, et al. Intestinal ischemia during cardiac arrest and resuscitation: comparative analysis of extracellular metabolites by microdialysis. Resuscitation. 2003;58:209–217. doi: 10.1016/s0300-9572(03)00119-9. [DOI] [PubMed] [Google Scholar]
- 4.Guyot LL, Diaz FG, O’Regan MH, Song D, Phillis JW. Topical glucose and accumulation of excitotoxic and other amino acids in ischemic cerebral cortex. Horm Metab Res. 2000;32:6–9. doi: 10.1055/s-2007-978577. [DOI] [PubMed] [Google Scholar]
- 5.Sappey-Marinier D, Chileuitt L, Weiner MW, Faden AI, Weinstein PR. Hypoglycemia prevents increase in lactic acidosis during reperfusion after temporary cerebral ischemia in rats. NMR Biomed. 1995;8:171–178. doi: 10.1002/nbm.1940080406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stadlbauer KH, Rheinberger K, Wenzel V, Raedler C, Krismer AC, Strohmenger HU, et al. The effects of nifedipine on ventricular fibrillation mean frequency in a porcine model of prolonged cardiopulmonary resuscitation. Anesth Analg. 2003;97:226–230. doi: 10.1213/01.ane.0000068801.28430.ed. [DOI] [PubMed] [Google Scholar]
- 7.Meybohm P, Cavus E, Dörges V, Steinfath M, Sibbert L, Wenzel V, et al. Revised resuscitation guidelines: adrenaline versus adrenaline/vasopressin in a pig model of cardiopulmonary resuscitation--a randomised, controlled trial. Resuscitation. 2007;75:380–388. doi: 10.1016/j.resuscitation.2007.04.022. Epub 2007 Jun 20. [DOI] [PubMed] [Google Scholar]
- 8.Guérin JP, Levraut J, Samat-Long C, Leverve X, Grimaud D, Ichai C. Effects of dopamine and norepinephrine on systemic and hepatosplanchnic hemodynamics, oxygen exchange, and energy balance in vasoplegic septic patients. Shock. 2005;23:18–24. doi: 10.1097/01.shk.0000150549.45338.6c. [DOI] [PubMed] [Google Scholar]
- 9.Schaer GL, Fink MP, Parrillo JE. Norepinephrine alone versus norepinephrine plus lowdose dopamine : enhance renal blood flow with combination pressortherapy. Crit Care Med. 2005;13:492–499. doi: 10.1097/00003246-198506000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Nordmark J, Rubertsson S. Induction of mild hypothermia with infusion of cold (4 degrees C) fluid during ongoing experimental CPR. Resuscitation. 2005;66:357–365. doi: 10.1016/j.resuscitation.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Voelckel WG, Lindner KH, Wenzel V, Bonatti JO, Krismer AC, Miller EA, et al. Effect of small-dose dopamine on mesenteric blood flow and renal function in a pig model of cardiopulmonary resuscitation with vasopressin. Anesth Analg. 1999;89:1430–1436. doi: 10.1097/00000539-199912000-00020. [DOI] [PubMed] [Google Scholar]


