Abstract
BACKGROUND:
Fifty years of our history in developing and advancing emergency medicine into an independent medical specialty will surely provide emergency medicine colleagues from all over the world with valuable suggestions and guidance.
DATA SOURCES: This systemic review is based on the author’s extensive experience through active involvement in the national and international development of emergency medicine.
RESULTS:
Emergency physicians in the U.S. emergency departments and sometimes other settings provide urgent and emergency care to patients of all ages, including definitive diagnosis of emergent conditions, prolonged stabilization of patients when necessary, airway management, and life-saving procedures using rapid sequence intubation and sedation. They use a multitude of diagnostic technologies including laboratory studies, bedside ultrasound and other sophisticated radiology, such as CT scan, and MRI.
CONCLUSION:
In the U.S., emergency medicine fits extremely well into the overall medical system, and is clearly the most efficient way to provide emergency patient care.
KEY WORDS: Emergency medicine, Systemic review, U.S.A.
INTRODUCTION
In order to explore the topic of emergency medicine in the U.S.A., we need to address several objectives: to understand the status of emergency medicine in the United States of America; to be able to describe the current status, role, and activities of organized emergency medicine; and to discuss historical milestones, successes, failures, and lessons learned in order to share this for mutual benefit.
Emergency room era
While attempts to provide emergency care are arguably as old as medicine, the history of emergency medicine as a specialty is only 50 years old. Along with England, Canada, and Australia, the United States was one of the “early adopters” of the specialty of emergency medicine.
The modern history of emergency medicine essentially began in the 1960s. In 1960, there was no emergency medicine as a defined academic specialty. Typical hospital emergency rooms staffing patterns used resident, intern, other hospital staff physicians, or rotating on-call duty of all specialties including those such as psychiatry and even pathology. There was neither coordination of hospital care nor organized pre-hospital care. At least half of all ambulance services run by morticians or funeral directors because they had vehicles that could transport people horizontally, often using untrained staff. There were no national coordinating organizations.
Early formation of emergency department
In 1961 four physicians led by James D. Mills M.D. left their private medical practices to staff an emergency department (ED) together in Alexandria, Virginia. Meanwhile, a similar effort by 23 physicians occurred in Pontiac, Michigan, leading to the “Pontiac and Alexandria Plans” for emergency medicine (Figure 1). This reflected the efforts of pioneering physicians around the world who independently realized the need for a specialist in emergencies who would be available to patients at all times or day or night. These physicians lit the flame of the modern specialty of emergency medicine so that the world could benefit from its light.
Figure 1.
Early emergency department (ED) staffing changes in the U.S..
Specialties have made advancements in medical knowledge and technology that have improved the best possible outcomes for most medical and surgical problems.[1] For people to benefit from this knowledge, they need to have access to the right specialist at the right time. Prior to emergency medicine, this was particularly problematic relative to caring for emergencies.
Before the establishment of emergency medicine in the U.S., emergencies that needed a specific specialist not in attendance were given to whatever physician could be found, regardless of expertise. Often this was a very junior doctor in training. While some older specialists still refer to these as “the good old days”. Unfortunately, they were not good for patients who had emergencies at the “wrong time”.
The problems with this approach were twofold. First, even the largest hospitals all specialists may not be valuable in the light of a typical day, but without the specialty of emergency medicine it is rarely possible to provide specialist care at 3 a.m. or on a holiday. Second, and more fundamental, is that atypical presentations of disease often make it unclear which specialist the patient needs in a timely manner. For example, if a patient has vomiting abdominal pain and headache, is the problem meningitis, migraine, myocardial infarction, dehydration, appendicitis, or something else? In the absence of an emergency medicine generalist, each would require a different specialist, and the time it took to determine which one could be harmful or fatal to the patient.
Historic milestones of academic emergency medicine
As the U.S. pioneers moved forward, they received support in the form of the 1966 National Academy of Sciences “White Paper”: “Accidental Death and Disability, the Neglected Disease of Modern Society” that described the poor state of emergency care in the U.S.. This led to the 1966 Federal Highway Safety Act, which for the first time set standards for ambulances and training in the U.S.. At the same time, the Vietnam War demonstrated how poor civilian trauma care was in comparison to that received by soldiers in the field (Figure 2).
Figure 2.
Need for the specialty in the U.S..
Other developments influenced the establishment of emergency medicine in the U.S. were the introduction of CPR as a resuscitation measure, the federal government began paying for in-hospital services through Medicare and Medicaid, leading for increased public demand and better quality of all types of healthcare services.
Founding of the American College of Emergency Physicians
In this environment, two physicians in Michigan who had dedicated their careers to emergency medicine practice, John Wiegenstein and John Rupke, started to talk about the future. “Maybe we should be a specialty”. “Maybe this is a specialty in which we should train physicians”. “We should focus our work in this specialty”.
In the wake of their discussions, the American College of Emergency Physicians (ACEP) was born on August 16, 1968 by eight physicians in Lansing, Michigan. John G. Wiegenstein was the founding president. Concurrent activities were occurring in Fairfax, Virginia, and shortly thereafter these physicians joined with ACEP.
The initial goals were to develop emergency medicine specific educational conferences, textbooks, and training materials, and to attain specialty board status and recognition. Their vision was that “Emergency Medicine should be practiced by qualified and certified Emergency Physicians”.
With this in mind, developing an educational program was a priority. The first ACEP Scientific Assembly was held in November, 1969 in Denver, Colorado; the fee was $ 50. There were 14 faculty and 128 attendees.
Recognization by the American Medical Association
Political activities within the house of medicine were also ongoing, and remarkably effective. In 1972 just four years after the founding of ACEP, the American Medical Association (AMA) recognized emergency medicine as a specialty and created the AMA Section of Interest on emergency medicine. To do so, the early leaders needed to overcome arguments against the specialty, including that there was “no unique body of knowledge”, “no research base”, “you will steal our patients”, and “we have too many specialties already”.
With this victory in hand, the task turned to advocating for approval by the American Board of Medical Specialties (ABMS). To this end, ACEP developed standards for residencies via the establishment of the Liaison Residency Endorsement Committee (LREC), which eventually evolved into the Residency Review Committee (RRC).
The next year, 1973, saw the passage of the federal Emergency Medical Services Systems Act (Public Law 93-154) that funded regional and local EMS services. In the private sector, the Advanced Cardiac Life Support (ACLS) and Advanced Trauma Life Support (ATLS) courses were developed in the 1970s. Meanwhile, public expectations were advanced by the television show “Emergency “ which publicized both the new Los Angeles paramedic ambulances and the doctors they delivered patients to, and the many pilots returning from Vietnam triggered an expansion of aero medical transport services which now number over 500 programs in the U.S.
Founding of the International Federation of Emergency Medicine
All of these events together led to arguably the earliest accomplishment of the modern definition of emergency medicine as promulgated by the International Federation for Emergency Medicine (IFEM).[2] This definition (Figure 3) focuses on the ability to take care of all types of acute illness and injury in patients of all age groups in all settings, both pre-hospital and in-hospital. While the U.S. “model” of emergency medicine is common, variation does exist between countries including physicians practicing extensively in the pre-hospital setting, or in the critical care unit of the hospital.[3,4] The IFEM definition, however, places a major focus of the specialty on the provision of emergency care in the receiving area of hospitals, the “Emergency Department” (ED), and of course this is true in the United States.
Figure 3.
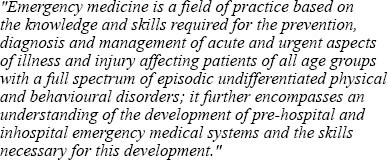
IEEM definition of emergency medicine.
Inauguration of the emergency residency programs
As the clinical specialty advanced, so did the academic specialty. In 1970 at the University of Cincinnati Dr. Bruce Janiak was the first emergency medicine resident trainee. In 1971, three residents were enrolled at University of Southern California in Los Angeles, making it the “oldest continuously running program”. And in 1972 the Medical College of Pennsylvania started its program, giving emergency medicine a “coast to coast” presence. These early programs were only two years length, usually after an internship of some sort. In 1980 these were standardized to a minimum of 24 months of emergency medicine, and 36 months of total training and in the late 1980s became a minimum of 36 months of emergency medicine training, with some programs lasting four years.
The Society of Academic Emergency Medicine
Shortly after the development of the first residency programs in the 1970s, the University Association for EMS and the Society of Teachers of Emergency Medicine were formed to provide means for academic emergency physicians to interact. Both organizations merged in 1990 to form the Society for Academic Emergency Medicine, which now has over 5000 members, publishes Academic Emergency Medicine, and holds an annual meeting each spring with over 1500 attendees.
The American Board of Emergency Medicine
The success in both clinical and academic arenas gave ACEP the confidence to fund the establishment of the American Board of Emergency Medicine (ABEM) in 1976. Within three years, the independent ABEM received specialty board approval in 1979 as the 23rd medical specialty in the U.S..
This approval was as a “conjoined” board, which meant that it included representatives from other “parent” specialties. Regardless, the existence of the board led to further development and expansion of the numbers of residencies and other ongoing educational efforts. This was reinforced by the announcement that the ability to accumulate the practice months and hours to take Certification Exam without completing a residency, known as the “Grandfather Clause” would end in 1988, which meant that to use this pathway physicians would need to be in practice by July 1983.
The focus on residency development took much of the specialty’s attention during the 1980s. At the same time, the realization that things were on track within the house of medicine turned leaders toward initiating advocacy for Emergency Medicine in Congress. This led to the opening of ACEP’s Washington Office in 1985.
Another manifestation of this outward looking approach was the U.S. role in establishing the International Federation for Emergency Medicine (IFEM), a consortium of national emergency medicine organizations that began with ACEP (U.S.A.), BAEM (U.K.), ACEM (Australia), and CAEP (Canada) in 1985 and was chartered in 1989. Initially the primary role of IFEM was to operate the semi-annual international conference on EM (I.C.E.M.) starting in 1986, including three times in the U.S.. In 1998, IFEM extended full membership extended to organizations from other countries with developed emergency medicine systems, and the first new member was Hong Kong. As IFEM has matured it has developed a number of functions, including forming policy statements on international health issues and creating educational curricula. It also has extended affiliated memberships to entities not qualifying for full membership. The U.S. affiliated members are the American Academy of Emergency Medicine, American College of Osteopathic Emergency Physicians, and the Society for Academic Emergency Medicine (Figure 4).
Figure 4.
U.S. national emergency medicine organizations.
The second full decade of U.S. emergency medicine ended on a high note with ABEM being granted “Primary Board Status” by ABMS in 1989. This meant ABEM was no longer “under” the other specialties, and could now pursue the independent development of subspecialty certifications.
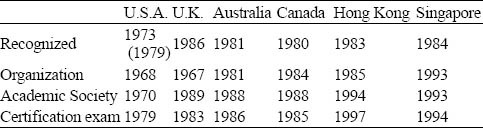
In accomplishing primary board status, the U.S. clearly completed the important milestones of specialty development defined by what are known as the “Arnold Criteria.”[2] The exact length and route of this journey to fully mature specialty varies by country, as seen by the U.S. comparison to selected others (Table 1), including two systems that began at a similar time to the initiation of emergency medicine here in Beijing in 1983. The U.S. chose an initial training and certification plan that included “grandfathering” provisions; this has not been used everywhere. In spite of this, it is important to understand that regardless of any initial pragmatism, the U.S., like other leading countries, was always focused on a future of emergency medicine practice with a fully trained and certified specialist workforce that meets the needs of the people.
Table 1.
Comaparative milestones of emergency medicine development in selected countries and regions
Public awareness of emergency medicine
In the 1990s, U.S. emergency medicine continued to grow, and this growth was fueled by the entertainment industry, which glamorized the specialty in movies and shows such as “ER”. The role of the media cannot be underestimated. This media encouragement has been a major factor in promoting the value of, and demand for, emergency medicine. It continued to drive public expectations, reinforcing that while emergency medicine development in the U.S. was led by a core group of physician believers. It was the needs and wants of the people that fanned the flames of its growth.
The media has also had a major role in promoting the rapid growth of pre-hospital EMS care. In many areas, the creation of a high quality EMS system actually drives improvements in hospital care; another example of “bottom-up” growth reinforces emergency medicine as the people’s specialty! Other factors that advance the need for emergency medicine are improved overall medical system development, rapid urbanization causing transition from infections to trauma and cardio-respiratory disease, increasing demand for outpatient medical visits, the success of emergency medicine in other high profile countries increasing expectations, international travel, and terrorist or other mass casualty events[5] (Figure 5).
Figure 5.
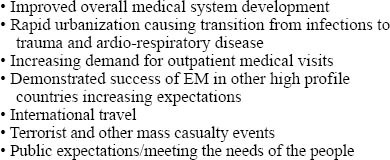
Factors stimulating emergency medicine growth in the 21st century.
Current situation
The United States CDC data show increasing demand for emergency services in the U.S.. Recent data for 2009 showed 124 million emergency department visits compared to 90.3 million in 1996 (up 35%). This was an average of 41.5 visits per 100 persons compared with 34.2 in 1996 (up 18%).
There is a greater increase of emergency services in aging population, with over 60 visits per 100 persons for those over 75 years old. This is not due to a lack of primary care as the majorities needed to be seen in the emergency department. According to the U.S. Government’s Centers for Disease Control, emergent patients who need to be seen within 15 minutes were 10.8%, with 1% requiring immediate resuscitation. Urgent patients, requiring 15-60 minute evaluation, were 36.6%, semi-urgent, 1-2 hours, were 22.0%, and non-urgent, 2-24 hours, 8.1%. Thirteen percent were not categorized.[6] In delivering such care to a high percentage of its population, the U.S. is fulfilling its obligations under the 2007 World Health Assembly resolution, urging member states “to ensure that a core set… of emergency care services are available to all people who need them.”
It is not just the patients who want emergency medicine. It is one of the most popular and competitive specialty choices of U.S. medical school graduates, similar to the situation in other well-established emergency medicine countries like UK and Australia. It is popular with other medical and surgical specialists as well. While there was some initial resistance, there was a realization that emergency medicine is a consulting specialty that does not take patients from other physicians, enabling other specialties to practice more efficiently by eliminating disruptions to their office and hospital rounds schedules.
So who is practicing emergency medicine in the U.S.? There are 35 000-40 000 practitioners, most the graduates of 199 residencies producing more than 2000 graduates per year, which are probably more than half of the current worldwide output. Over 25 000 emergency physicians are board certified, again, probably the majority of approximately 40 000 board certified emergency physicians globally.
In the U.S., there are emergency medicine meetings going on essentially every day. These meetings are held by multiple local and national organizations and usually attract 100 to 1000 participants from anywhere. The largest emergency medicine meeting in the U.S. is still the ACEP Scientific Assembly. The 41st Annual ACEP Scientific Assembly in Las Vegas, Nevada attracted 200 faculty, and 6200 attendees, of whom 95% were physicians.
Sub-specialties of emergency medicine in the U.S. include toxicology, pediatric emergency medicine, emergencies and disasters, critical care, hyperbaric medicine, administration/practice management and research.
Emergency physicians do not work alone. Other members of the team include specialized emergency nurses, emergency technicians, paramedics, and physician extenders such as physician assistants and certified nurse practitioners.
In fielding this extensive workforce to benefit of emergency medicine and the needs of people for quality emergency medical care, the U.S. is also accomplishing the goals of the World Health Assembly in Resolution 60.22 passed unanimously in 2007 that urges members: “…to ensure that a core set of trauma and emergency care services are available to all people who need them” and remaining firmly in the ranks of those countries where emergency medicine is an official well-established and well distributed or “mature” specialty with its own training programs and board exam.
Current issues and future directions
Once mature, a specialty must deal with its operational problems, and emergency medicine in the U.S. is no exception. The four biggest challenges for U.S. emergency medicine are professional liability, reimbursement, surge capacity, and workforce projections.
One of the more pressing concerns of U.S. emergency physicians is the unfortunate frequency of charges of malpractice. It has become so common that it is sometimes referred to as a “lawsuit lottery”, taking the stigma away but affecting access to care, and adding billions in costs from high liability insurance premiums and more importantly other costs of “defensive medicine” including unnecessary testing and treatments.
Reimbursement declining is an issue for all healthcare providers. It particularly affects emergency medicine since we have an inability to screen patients and requirement to see everyone who presents. Increasing public demands fewer resources and a lack of good societal decisions regarding what to pay for are requiring us to see progressively increasing numbers of patients with decreasing resources.
Crowding of emergency departments has led to reduced surge capacity in the emergency care system. There are many more elderly and complex patients due to shifting demographics, and they often require admission to a decreasing number of inpatient hospital beds. Combined with a nursing shortage this crowding has resulted in a changing role of emergency medicine, not all of it good. This same problem exists in most other countries.
It is very important for emergency medicine to plan its residency output to meet the emgergency medicine workforce needs of the U.S., but not to “overshoot” and produce too many specialty physicians, which has happened temporarily in other specialties. At this time, all the evidence indicates that emergency medicine will be an “undersupplied” specialty in the U.S. for at least 20 more years.
A newly recognized specialty is born an infant, and must be nurtured to grow. Like many countries, initially the U.S. allowed for a route for some established practitioners who advocated the start of the specialty and the ability to become certified in emergency medicine. While sometimes communicated differently, the period to begin practice in order to apply for the examination without doing training in the U.S. was effectively four years after the approval of the specialty board. Alternatively, other countries have begun with outside cadres who train the first native specialists as the only route to certification. The timeline and the decision are cultural and individual.
CONCLUSIONS
The most important thing for all of us to appreciate is that in the U.S., as in the rest of the world, people want and expect quality emergency care. This has led to the very rapid development of emergency medicine in the U.S. in the last 40 years.
In the U.S., emergency medicine fits extremely well into the overall medical system, and is clearly the most efficient way to provide emergency patient care. Demand for emergency care increases with overall access to medical care in the U.S., making meeting specialty workforce challenges a major source of controversy within the specialty.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there is no conflict of interest.
Contributors: Robert E. Suter proposed the study and wrote the paper.
REFERENCES
- 1.Weisz G. New York, NY: Oxford University Press; 2005. Divide and Conquer: A Comparative History of Medical Specialization. [Google Scholar]
- 2.Bodiwala G. Emergency Medicine. A Global Specialty. Emerg Med Australasia. 2007;19:287–288. doi: 10.1111/j.1742-6723.2007.00989.x. [DOI] [PubMed] [Google Scholar]
- 3.Arnold J. International emergency medicine and the recent development of emergency medicine worldwide. Ann Emerg Med. 1999;33:97–103. doi: 10.1016/s0196-0644(99)70424-5. [DOI] [PubMed] [Google Scholar]
- 4.Alagappan K, Holliman CJ. History of the development of international emergency medicine. Emerg Med Clin North Am. 2005;23:1–10. doi: 10.1016/j.emc.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Rochefort M. Comparative medical systems. Annu Rev Sociol. 1996;22:239–270. [Google Scholar]
- 6.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;7:1–38. [PubMed] [Google Scholar]


