Abstract
BACKGROUND:
This study aimed to observe the effect of early goal directed therapy (EGDT) on tissue perfusion, microcirculation and tissue oxygenation in patients with septic shock.
METHODS:
Patients with early septic shock (<24 hours) who had been admitted to the ICU of Zhongda Hospital Affiliated to Southeast University from September 2009 through May 2011 were enrolled (research time: 12 months), and they didn’t meet the criteria of EGDT. Patients who had one of the following were excluded: stroke, brain injury, other types of shock, severe heart failure, acute myocardial infarction, age below 18 years, pregnancy, end-stage disease, cardiac arrest, extensive burns, oral bleeding, difficulty in opening the mouth, and the onset of septic shock beyond 24 hours. Patients treated with the standard protocol of EGDT were included. Transcutaneous pressure of oxygen and carbon dioxide (PtcO2, PtcCO2) were monitored and hemodynamic measurements were obtained. Side-stream dark field (SDF) imaging device was applied to obtain sublingual microcirculation. Hemodynamics, tissue oxygen, and sublingual microcirculation were compared before and after EGDT. If the variable meets the normal distribution, Student's t test was applied. Otherwise, Wilcoxon's rank-sum test was used. Correlation between variables was analyzed with Pearson's product-moment correlation coefficient method.
RESULTS:
Twenty patients were involved, but one patient wasn’t analyzed because he didn’t meet the EGDT criteria. PtcO2 and PtcCO2 were monitored in 19 patients, of whom sublingual microcirculation was obtained. After EGDT, PtcO2 increased from 62.7±24.0 mmHg to 78.0±30.9 mmHg (P<0.05) and tissue oxygenation index (PtcO2/FiO2) was 110.7±60.4 mmHg before EGDT and 141.6±78.2 mmHg after EGDT (P<0.05). The difference between PtcCO2 and PCO2 decreased significantly after EGDT (P<0.05). The density of perfused small vessels (PPV) and microcirculatory flow index of small vessels (MFI) tended to increase, but there were no significant differences between them (P>0.05). PtcO2, PtcO2/FiO2, and PtcCO2 were not linearly related to central venous saturation, lactate, oxygen delivery, and oxygen consumption (P>0.05).
CONCLUSION:
Peripheral perfusion was improved after EGDT in patients with septic shock, and it was not exactly reflected by the index of systemic perfusion.
KEY WORDS: Transcutaneous pressure of oxygen, Transcutaneous pressure of carbon dioxide, Microcirculation, Septic shock, EGDT, Tissue perfusion, Tissue oxygenation, Sidestream dark field imaging
INTRODUCTION
Septic shock is associated with high morbidity and mortality.[1,2] Early goal-directed therapy (EGDT) can improve the prognosis of patients with septic shock, but the mortality of these patients is as high as 42.3%.[3] Tissue hypoperfusion may exist clinically, though the blood pressure, heart rate, urine output of the patients may return to normal. As a result, the endpoint of resuscitation in EGDT may not be sufficient for patients with septic shock.
Microcirculation dysfunction in patients with septic shock is characterized by the low density of perfused small vessels and the heterogeneity of microvascular blood flow.[4,5] Microcirculatory perfusion indices are more markedly impaired in nonsurvivors compared with survivors, and microvascular dysfunction is associated with organ failure.[4–6] In addition, microcirculatory alterations in patients with septic shock are independent of macrocirculation.[6,7] Tissue oxygenation measured in peripheral tissue as transcutaneous pressure of oxygen and carbon dioxide (PtcO2, PtcCO2) is early, and more sensitive indices reflecting hypoperfusion and hypoxia in shock[8,9] and trends of PtcO2 are related to the prognosis of patients.[10,11] As a result, monitoring of resuscitation during EGDT can help to identify tissue hypoperfusion.
The present study aims to investigate the effects of EGDT on tissue perfusion by monitoring of PtcO2, PtcCO2 and sublingual microcirculation before and after EGDT.
METHODS
Patients
Patients with early septic shock (<24 hours) who had been admitted to the ICU of Zhongda Hospital Affiliated to Southeast University from September 2009 through May 2011 were enrolled (research time,12 months), but they didn’t meet the criteria of EGDT. The diagnosis of septic shock was based on the Guidelines of Severe Sepsis and Septic Shock.[12] Written informed consent was obtained from patients or their legally authorized surrogates. Excluded were patients who met the following: neurogenic shock, stroke, head trauma, hypovolemic shock, obstructive shock, severe heart failure, acute myocardial infarction, cardiogenic shock, fluid overloading, age below 18 years, pregnancy, end-stage disease, cardiopulmonary arrest, severe burns, local skin with infection unsuitable for the placement of oxygen electrode, unfeasible access to sublingual microcirculation, fulfillment of the four criteria of EGDT, the onset of septic shock beyond 24 hours, and failure to obtain consent form.
Hemodynamic monitoring
A PiCCO catheter (4F, PV2014L16, PULSION Medical Systems AG, Germany) was inserted into the femoral artery, and a central venous catheter was placed in the internal jugular vein. After the catheter and wire were connected to the monitor, the hemodynamic data were obtained via the thermodilution method.
PtcO2 and PtcCO2 monitoring
TCM4 (Radiometer Copenhagen, Denmark) was used to obtain PtcO2 and PtcCO2. The cutaneous electrode of TCM4 was prepared according to the instructions of the manufacturer. After it was prepared, the electrode was placed on a shaved portion of the anterior thorax. The skin was cleaned with alcohol and dried to ensure good adhesion of the O-ring. The electrode was then attached to the ring by using a contact liquid as recommended by the manufacturer. The electrode temperature was set at 43 °C, and the alarm time was set at 4 hours. After 10–20 minutes, PtcO2 and PtcCO2 were then stabilized and could be read and recorded when necessary.
Sublingual microcirculation monitoring
The sublingual microvascular network was studied using side-stream dark field (SDF) imaging (MicroVision Medical, Amsterdam, The Netherlands). After removal of saliva and other secretions, the device was used without pressure on the sublingual region. Three images in a duration of at least 20 seconds were obtained from the sublingual region by an investigator and stored in the computer (Sony, Tokyo, Japan). Video clips were blindly analyzed with AVA 3.0 software package (MicroVision Medical, Amsterdam, The Netherlands) by two investigators who were not involved in data collection to get perfused vessel density (PVD) and proportion of perfused vessels (PPV). Quantification of flow (no flow: 0; intermittent flow: 1; sluggish flow: 2; and continuous flow: 3) was scored per quadrant for each vessel diameter cohort (small: 10–25 μm; medium 26–50 μm; and large 51–100 μm). The microvascular flow index (MFI) was calculated as the sum of each quadrant score divided by the number of quadrants in which the vessel type was visible. The final MFI was averaged over a maximum of 20 quadrants (three regions, four quadrants per region) derived from the overall flow impressions of all vessels with a particular range of diameter in a given quadrant. The heterogeneity index was also calculated.
Main outcome measures
The demographic data included age, sex, acute physiology and chronic health evaluation (APACHE)II score, sequential organ failure assessment (SOFA) score, vasoactive drugs, source of infection, and chronic complications. The hemodynamic data and systemic oxygenation index were heart rate (HR), mean arterial pressure (MAP), central venous pressure (CVP), cardiac output (CO), cardiac index (CI), stroke volume (SV), stroke volume index (SVI), extra-vascular lung water (EVLW), extra-vascular lung water index (EVLWI), oxygen delivery (DO2), oxygen consumption (VO2), oxygen extraction rate (O2ext), and lactate (Lac). Microcirculation indexes were PVD, PPV, MFI, and heterogeneity index. Tissue oxygenation indexes included PtcO2, PtcCO2, PtcO2/FiO2, PtcO2 shunt [(PaO2–PtcO2)/PaO2], PtcCO2 index (PtcCO2/PaCO2), and PCO2 gap (difference between PtcCO2 and PaCO2).
Implementation of EGDT and data collection
Protocol of EGDT
Fluid resuscitation was done to achieve a CVP of 8 to 12 mmHg. If the MAP was less than 65 mmHg, vasopressors were given to maintain a mean arterial pressure of at least 65 mmHg and urine output of at least 0.5 mL/kg per hour. If central venous oxygen saturation (ScvO2) was less than 70%, red cells were transfused to achieve a hematocrit of at least 30%. After the CVP, MAP, and hematocrit were thus optimized, if the ScvO2 was less than 70%, dobutamine was administered until the ScvO2 was 70% or higher or until a maximal dose of 20 µg per kilogram per minute was given.
Criteria of EGDT
The criteria for EGDT were as follows: MAP≥65 mmHg, CVP 8–12 mmHg, ScvO2≥70%, and urine output ≥0.5 mL/kg per hour.
Data collection
Data of hemodynamics, microcirculation and tissue oxygenation index were collected before and after EGDT.
Statistical analysis
Data were presented as mean ±SD, if they accorded with normal distribution or presented as a median and interquartile range (IQR) (M [P25, P75]). Paired sample Student's t test and Wilcoxon's rank-sum test were used as appropriate. Variable correlation was analyzed with Pearson's product-moment correlation coefficient method. Statistical significance was set when P<0.05. SPSS statistics software version 16.0 was used.
RESULTS
Demographic data
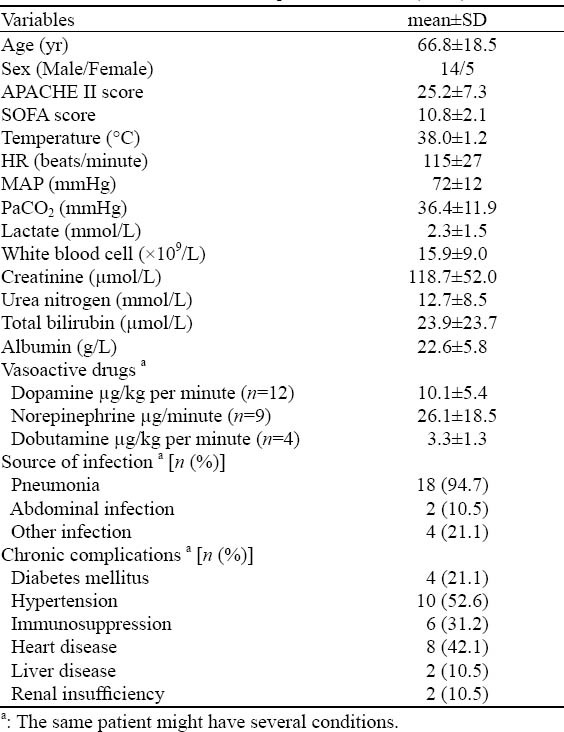
Twenty patients with septic shock were enrolled during the study period and 19 of them met the criteria of EGDT. The mean time of meeting EGDT was 2.94±2.72 hours (median time 2.0 hours). Tissue oxygenation was observed in the 19 patients. PiCCO was used to monitor hemodynamics in 13 patients and sublingual microcirculation was monitored in 4 patients. The mean APACHEII score was 25.2±7.3 and the mean SOFA score was 10.8±2.1. Fourteen patients were male (Table 1).
Table 1.
The characteristics of the patients enrolled (n=19)
Effect of EGDT on hemodynamics of patients with septic shock
HR of the patients decreased (P<0.05) and MAP and CVP increased (P<0.01) after EGDT in contrast to before EGDT. Other hemodynamic indexes were not shown to be significant (Table 2).
Table 2.
The effect of EGDT on hemodynamics during the period of septic shock (n=19)
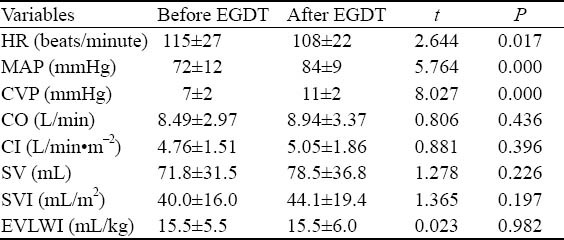
Effect of EGDT on systemic oxygenation of patients with septic shock
ScvO2 after EGDT was higher than that before EGDT (P<0.01). Lactate was 2.3±1.5 mmol/L before EGDT and was 2.2±1.1 mmol/L after EGDT. No significant difference was seen between them (P>0.05) and so was between DO2, VO2 and others (Table 3).
Table 3.
The effect of EGDT on systemic oxygenation during the period of septic shock (n=19)
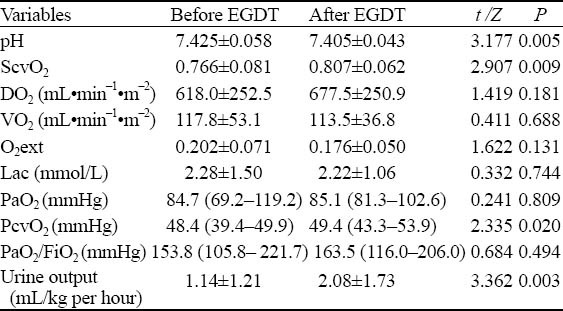
Effect of EGDT on sublingual microcirculation of patients with septic shock
Sublingual microcirculation was monitored in 4 patients. TVD, PVD, PPV, MFI and heterogeneity indexes were not changed significantly before and after EGDT (P>0.05). But PPV and MFI showed the trend of increasing (P was 0.051 and 0.074 respectively) (Table 4 and Figure 1).
Table 4.
The effect of EGDT on microcirculation during the period of septic shock (n=4)
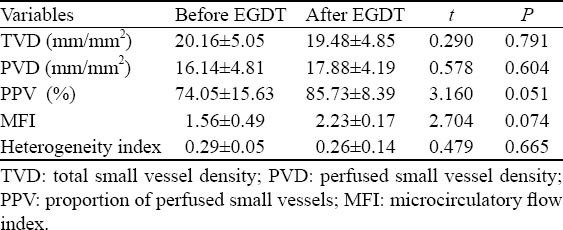
Figure 1.
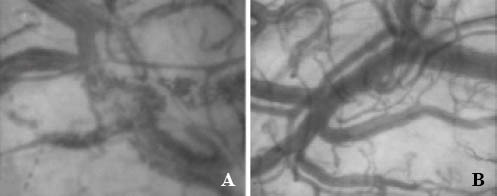
The sublingual microcirculation before and after EGDT in one patient. A: Before EGDT, sludged individual erythrocytes can be seen in microvessels; B: After EGDT, individual erythrocytes cannot be seen in microvessels.
Effect of EGDT on tissue oxygenation of patients with septic shock
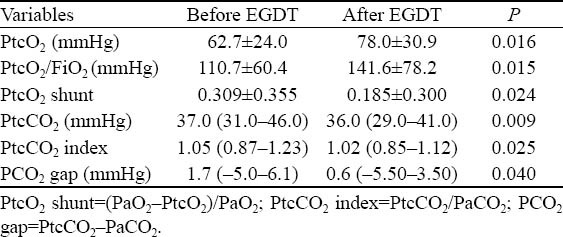
PtcO2 and PtcO2/FiO2 after EGDT increased more significantly than those before EGDT (P<0.05). PtcCO2, PtcO2 shunt, PtcCO2 index and PCO2 gap decreased significantly after EGDT (P<0.05) (Table 5).
Table 5.
The effect of EGDT on tissue oxygenation (n=19)
The correlation between tissue oxygenation index and hemodynamic index
There was no correlation between PtcO2 and MAP, CO, CI, SV, SVI, EVLW and EVLWI (All P>0.05). There were a positive linear relationship between PtcO2/FiO2 and MAP(r=0.354, P=0.029) (Figure 2) and a negative linear relationship between PtcO2/FiO2 and EVLWI (r=–0.467, P=0.016). No correlation was found between PtcO2/FiO2 and CO, CI, SV, SVI and EVLW (P>0.05). PtcCO2 was linear related to MAP (r=–0.354, P=0.029) (Figure 3), but not to CO, CI, SV, SVI, EVLW and EVLWI (P>0.05).
Figure 2.
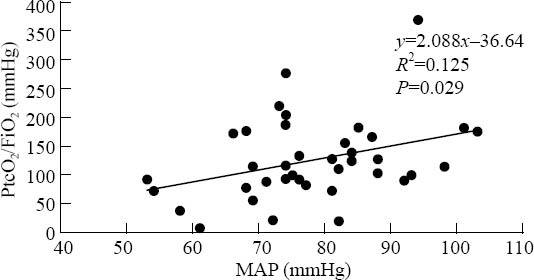
The correlation between PtcO2/FiO2 and MAP (n=19).
Figure 3.
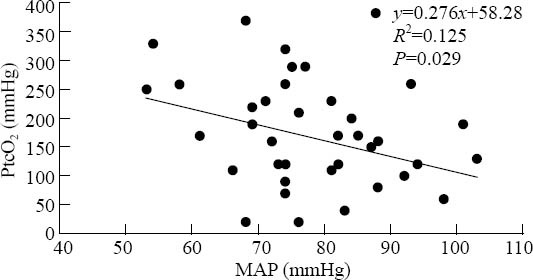
The correlation between PtcCO2 and MAP (n=19).
The correlation between tissue oxygenation index and systemic oxygenation index
No correlation was found among PtcO2 , DO2, VO2, O2ext, ScvO2, PaO2, PvO2 and Lac (All P>0.05). PtcO2/FiO2 was not linearly related to DO2, VO2, O2ext, ScvO2, PvO2 and Lac (All P>0.05). There was no correlation between PtcCO2 and DO2, VO2, O2ext, ScvO2 and Lac (All P>0.05).
DISCUSSION
Hypoxia due to tissue and organ hypoperfusion was the essence of shock. As a result, early correction of tissue and organ hypoxia was essential during shock resuscitation. Unfortunately, tissue hypoperfusion and hypoxia might still exist although hemodynamic indexes such as BP, HR, urine output, ScvO2 and systemic oxygenation index such as DO2 were within the normal range.[10] Recognition of the above limitations with global monitoring has stimulated efforts to look for ‘biomarkers’ at the regional level. Consequently, it is necessary to identify the tools of monitoring of shock resuscitation from the macrocirculation to microcirculation, from global oxygenation to tissue oxygenation. And SDF and tissue oxygen tension were the possible monitoring technologies.
The oxygen debt theory of shock indicates that shock is a state of hypoperfusion at the cellular level that occurs when DO2 to the tissues falls below VO2 requirements, and thus represents an imbalance between tissue DO2 and VO2.[13] In the EGDT study ScvO2 reflecting the balance of DO2 and VO2 is used as an endpoint of septic shock resuscitation and it improves the prognosis of patients with septic shock. But EGDT patients still have a high mortality, and many patients who met the criteria of EGDT still have tissue hypoperfusion and hypoxia. Hence, meeting the criteria of EGDT does not mean the match of DO2 and VO2 and the correction of tissue hypoxia . In addition, impairment of oxygen extraction is one of the main characteristics of septic shock.[14] Thus patients with septic shock still have the evidence of tissue hypoxia though DO2 is normal or supernormal after treatment.
Microcirculation dysfunction exists during the period of septic shock, and it is independent from correction of macrocirculation dysfunction. In our study, PPV and MFI showed the trend of improvement compared with those before the treatment, similar to the study of Trzeciak and colleagues.[5] But the heterogeneity of microcirculation was not improved because of the small sample size. Therefore, further clinical study is needed.
Yu et al[15,16] observed that oxygen challenge test (OCT) greater than 21 mmHg denotes the improvement of tissue perfusion during shock resuscitation, and treating patients with septic shock to an OCT value of 40 mmHg or more might provide an endpoint of resuscitation with better survival than resuscitating to DO2 and ScvO2. Our study revealed that PtcO2 and PtcO2/FiO2 increased and PtcCO2, PtcO2 shunt, PtcCO2 index and PCO2 gap decreased after EGDT, indicating that EGDT improved the local tissue oxygenation of patients with septic shock.
The correlation between index of global perfusion and systemic oxygenation such as lactate and ScvO2 and local tissue oxygenation index such as PtcO2 has rarely been studied. A study[17] revealed that oxygen tissue saturation (StO2) is less or not related to SvO2, urine output and lactate, suggesting that global perfusion is not consistent with local tissue perfusion. In our study, PtcO2, PtcO2/FiO2 and PtcCO2 were not correlated to DO2, VO2, O2ext, ScvO2 and lactate, showing that global tissue perfusion and oxygenation were not in accord with local perfusion and oxygenation.
LIMITATIONS
First, the sample size was small especially the sample of patients who had microcirculation data. Second, septic shock was largely due to pneumonia, not consistent with the cause of septic shock in ICU. Third, randomization and blindness were not adopted in the study in addition to the design of a control group. Consequently, subjective factors could not be removed completely and confounding factors and bias could not be vanished.
In conclusion, EGDT could improve local tissue perfusion of patients with septic shock and global perfusion might not reflect local tissue perfusion during the resuscitation of septic shock.
ACKNOWLEDGEMENTS
We are grateful to teacher Bing-wei Chen, who is working at School of Public Health of Southeast University, for his help in statistical analysis. We are also thankful to doctors and nurses working in the Zhong-da Hospital Affiliated to Southeast University.
Footnotes
Funding: None.
Ethical approval: The present study was approved Ethical Committee of Zhongda Hospital Affiliated to Southeast University, Nanjing, China.
Conflicts of interest: The authors have no competing interests relevant to the present study.
Contributors: Lu YH proposed and wrote the paper. All authors contributed to editing the final manuscript for content and style.
REFERENCES
- 1.Annane D, Aegerter P, Jars-Guincestre MC, Guidet B CUB-Réa Network. Current epidemiology of septic shock: the CUB-Réa Network. Am J Respir Crit Care Med. 2003;168:165–172. doi: 10.1164/rccm.2201087. [DOI] [PubMed] [Google Scholar]
- 2.Marty P, Roquilly A, Vallée F, Luzi A, Ferré F, Fourcade O, et al. Lactate clearance for death-prediction in severe sepsis or septic shock patients during the first 24 hours in Intensive Care Unit. An observational study. Ann Intensive Care. 2013;3:3. doi: 10.1186/2110-5820-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 4.De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL. Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med. 2002;166:98–104. doi: 10.1164/rccm.200109-016oc. [DOI] [PubMed] [Google Scholar]
- 5.Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, et al. Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. (98.e1-2).Ann Emerg Med. 2007;49:88–98. doi: 10.1016/j.annemergmed.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 6.Sakr Y, Dubois MJ, De Backer D, Creteur J, Vincent JL. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2004;32:1825–1831. doi: 10.1097/01.ccm.0000138558.16257.3f. [DOI] [PubMed] [Google Scholar]
- 7.De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant C, et al. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med. 2006;34:403–408. doi: 10.1097/01.ccm.0000198107.61493.5a. [DOI] [PubMed] [Google Scholar]
- 8.Tremper KK, Waxman K, Shoemaker WC. Effects of hypoxia and shock on transcutaneous PO2 values in dogs. Crit Care Med. 1979;7:526–531. doi: 10.1097/00003246-197912000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Tremper KK, Shoemaker WC, Shippy CR, Nolan LS. Transcutaneous PCO2 monitoring on adult patients in the ICU and the operating room. Crit Care Med. 1981;9:752–755. doi: 10.1097/00003246-198110000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Waxman K, Sadler R, Eisner ME, Applebaum R, Tremper KK, Mason GR. Transcutaneous oxygen monitoring of emergency department patients. Am J Surg. 1983;146:35–38. doi: 10.1016/0002-9610(83)90255-6. [DOI] [PubMed] [Google Scholar]
- 11.Tatevossian RG, Wo CC, Velmahos GC, Demetriades D, Shoemaker WC. Transcutaneous oxygen and CO2 as early warning of tissue hypoxia and hemodynamic shock in critically ill emergency patients. Crit Care Med. 2000;28:2248–2253. doi: 10.1097/00003246-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Society of Critical Care Medicine of Chinese Medical Association. Guidelines for hemodynamic monitoring and support of adult patients with severe sepsis and septic shock. Chin J Emerg Med. 2007;16:121–126. [Google Scholar]
- 13.Barbee RW, Reynolds PS, Ward KR. Assessing shock resuscitation strategies by oxygen debt repayment. Shock. 2010;33:113–122. doi: 10.1097/SHK.0b013e3181b8569d. [DOI] [PubMed] [Google Scholar]
- 14.Harrois A, Huet O, Duranteau J. Alterations of mitochondrial function in sepsis and critical illness. Curr Opin Anaesthesiol. 2009;22:143–149. doi: 10.1097/ACO.0b013e328328d1cc. [DOI] [PubMed] [Google Scholar]
- 15.Yu M, Morita SY, Daniel SR, Chapital A, Waxman K, Severino R. Transcutaneous pressure of oxygen: a noninvasive and early detector of peripheral shock and outcome. Shock. 2006;26:450–456. doi: 10.1097/01.shk.0000228798.18174.6a. [DOI] [PubMed] [Google Scholar]
- 16.Yu M, Chapital A, Ho HC, Wang J, Takanishi D., Jr A prospective randomized trial comparing oxygen delivery versus transcutaneous pressure of oxygen values as resuscitative goals. Shock. 2007;27:615–622. doi: 10.1097/shk.0b013e31802f0295. [DOI] [PubMed] [Google Scholar]
- 17.Leone M, Blidi S, Antonini F, Meyssignac B, Bordon S, Garcin F, et al. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology. 2009;111:366–371. doi: 10.1097/ALN.0b013e3181aae72d. [DOI] [PubMed] [Google Scholar]


