Abstract
BACKGROUND:
Fluid and electrolyte balance is a key concept to understand for maintaining homeostasis, and for a successful treatment of many metabolic disorders. There are various regulating mechanisms for the equilibrium of electrolytes in organisms. Disorders of these mechanisms result in electrolyte imbalances that may be life-threatening clinical conditions. In this study we defined the electrolyte imbalance characteristics of patients admitted to our emergency department.
METHODS:
This study was conducted in the Emergency Department (ED) of Uludag University Faculty of Medicine, and included 996 patients over 18 years of age. All patients had electrolyte imbalance, with various etiologies other than traumatic origin. Demographic and clinical parameters were collected after obtaining informed consent from the patients. The ethical committee of the university approved this study.
RESULTS:
The mean age of the patients was 59.28±16.79, and 55% of the patients were male. The common symptoms of the patients were dyspnea (14.7%), fever (13.7%), and systemic deterioration (11.9%); but the most and least frequent electrolyte imbalances were hyponatremia and hypermagnesemia, respectively. Most frequent findings in physical examination were confusion (14%), edema (10%) and rales (9%); and most frequent pathological findings in ECG were tachycardia in 24%, and atrial fibrillation in 7% of the patients. Most frequent comorbidity was malignancy (39%). Most frequent diagnoses in the patients were sepsis (11%), pneumonia (9%), and acute renal failure (7%).
CONCLUSIONS:
Electrolyte imbalances are of particular importance in the treatment of ED patients. Therefore, ED physicians must be acknowledged of their fluid-electrolyte balance dynamics and general characteristics.
KEY WORDS: Emergency department, Electrolyte imbalance, Patient characteristics
INTRODUCTION
Fluid and electrolyte balance is one of the key issues in maintaining homeostasis in the body, and it also palys important roles in protecting cellular function, tissue perfusion and acid-base balance. Fluid and electrolyte balance must also be maintained for the management of many clinical conditions. Electrolyte imbalances are common findings in many diseases.[1,2] Imbalances in every electrolyte must be considered in a combined and associated fashion, and examinations must aim to clarify the clinical scenario for an effective and successful treatment. Most of important and prevailing electrolyte imbalances are hypo- and hyper-states of sodium, potassium, calcium, and magnesium.
The kidney is a principally responsible organ for retention and excretion of electrolytes and fluid in healthy individuals.[3] But, other mechanisms like hormonal interactions of antidiuretic hormone, aldosterone, and parathyroid hormone, and other factors such as physiological stress also play important roles in regulating fluid and electrolyte balance in the organism. Studies about the clinical prevalence of electrolyte imbalances often report that these disorders are frequently seen in elderly and critically ill patients, and occur in the progression of diseases such as diabetes mellitus, acute or chronic renal failures, severe cardiovascular events like myocardial infarctions, etc.[4–6] To summarize, disturbances in electrolyte balances are mathematically measurable biochemical parameters in the bloodstream that determines the clinical manifestations of interactions between metabolic events such as sepsis,[7] hormones,[8] vascular events,[9] medications,[10] hydration deficiencies,[11] and renal physiology.
In this study we evaluated the general characteristics of patients admitted to our emergency department (ED), and diagnosed as having electrolyte imbalance. Literature data generally focused on imbalances of specific electrolytes, and the majority of the studies recruited patients of a specific disease or risk group. To our knowledge, only three studies focused on electrolyte imbalances in emergency department patients, and two of them conducted with elderly patients.[12–14] According to our search in PubMed database, our study will be the second study that investigates the generic electrolyte disturbances in ED admissions, and we think that it will contribute to the literature data by providing valuable information for the ED physicians.
METHODS
This study was conducted in the ED of Uludag University Faculty of Medicine, and included 996 patients with electrolyte imbalance. The patients were over 18 years of age and admitted to the ED with complaints other than traumatic in origin.
After admission and clinical examinations, data were collected from the patients with electrolyte imbalance after written informed consent was obtained. Demographic and clinical parameters of the patients included date of birth, complaints, vital signs, electrocardiographic (ECG) findings, physical examination findings, pathologic signs, oncological disease and metastatic state if any, drugs used, diagnosis, serum electrolyte levels, and discharge information from the ED. The local ethical committee of Uludağ University Faculty of Medicine approved this study (17-Jan-2012; Approval No: 2012-2/16).
Statistical analysis
SPSS v16.0 software was used for statistical analyses in this study. Descriptive statistics were presented as frequencies and percentages.
RESULTS
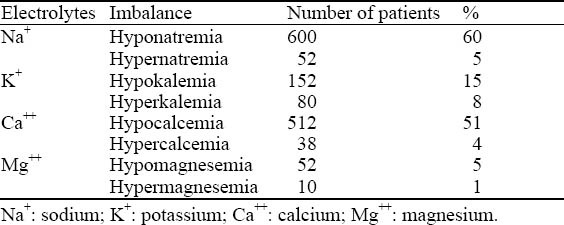
In the 996 patients with electrolyte imbalance, 55% (n=545) were male. The mean age of patients was 59.28 ±16.79 years. The most common symptoms of the patients were dyspnea (14.7%, n=146), fever (13.7%, n=136), and systemic deterioration (11.9%, n=118). Most and least frequent electrolyte imbalances were hyponatremia and hypermagnesemia, respectively. The distribution of electrolyte imbalances in our study population is presented in Table 1.
Table 1.
Distribution of electrolyte imbalance
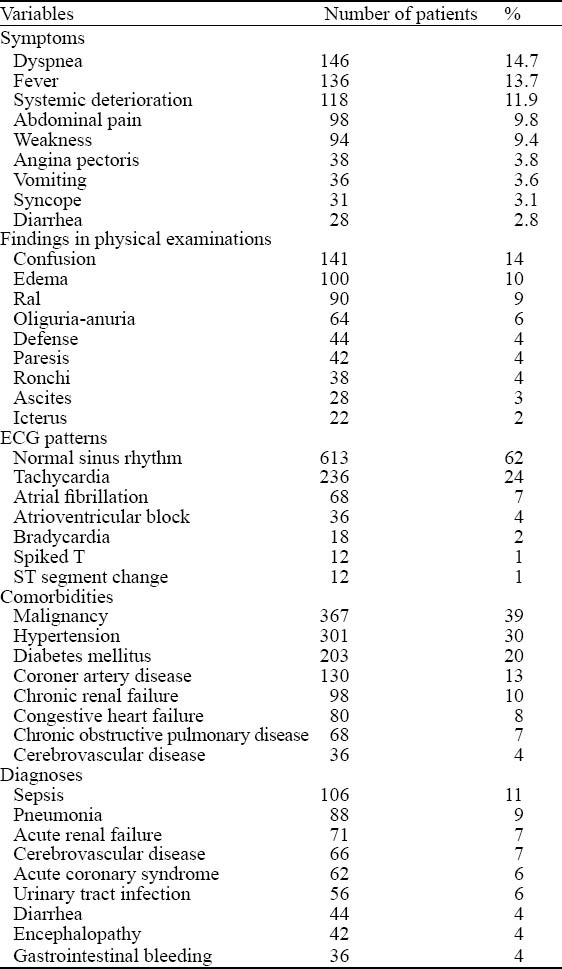
Confusion (14%), edema (10%) and rales (9%) were most frequently seen in physical examination. ECG examinations revealed normal sinus rhythm in 62% of the patients, and most frequent pathological findings were tachycardia (24%) and atrial fibrillation (7%). Some patients also had chronic diseases, which were treated with drugs. The most frequent comorbidity was malignancies, which are seen in 39% (n=367) of the patients. Most frequent oncological diagnoses in these patients were lung and hematological malignancies. By physical, clinical and laboratory examinations, sepsis was frequently diagnosed in 11% of the patients, pneumonia in 9%, and acute renal failure in 7%. All patients had at least one comorbid disease. The frequencies of prevalent symptoms, findings of physical examinations, ECG patterns, comorbidities and diagnoses are summarized in Table 2.
Table 2.
Most frequent symptoms, findings, ECG patterns, comorbidities and diagnoses of the patients
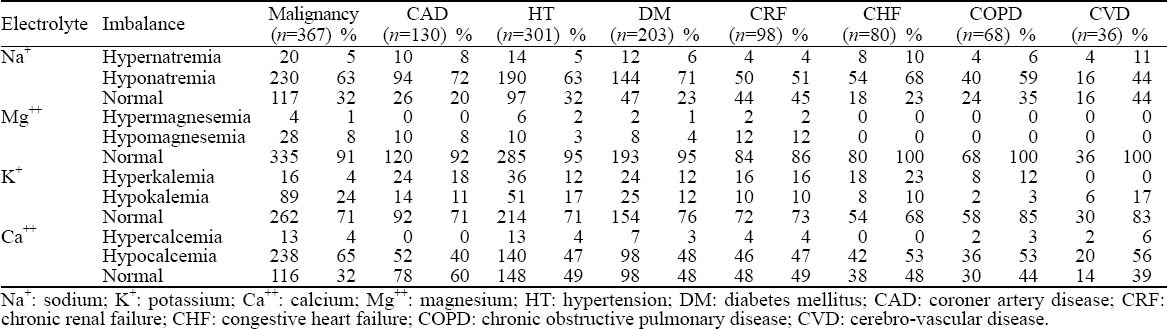
Electrolyte imbalances according to chronic diseases of the patients are presented in Table 3. According to this table all electrolytes were lower than their normal levels in chronic disease states.
Table 3.
Electrolyte imbalances according to chronic diseases
DISCUSSION
Electrolyte gradients are controlled precisely between intra- and extracellular compartments for sustaining the normal physiological functions of the muscles and nerves. The main responsible organ for this regulation is the kidney, but other mechanisms like hormonal activities of antidiuretic hormone, aldosterone and parathyroid hormone are also involved in this process. The disorders of these systems may deteriorate the electrolyte balances and results in emergencies.
Sodium imbalances are particularly important in patients who need intensive care because both hypo- and hypernatremia are associated with increased mortality in these patients regardless of age, gender and diagnoses.[15] Our study center provides tertiary health services in its region as a university based hospital, and particularly deals with clinically advanced diseases and complicated patients. Therefore, we particularly investigated electrolyte imbalances in our patients carefully, with an awareness of clinical importance of this entity. We determined sodium imbalance in 65% of our patients, and 60% of them had hyponatremia. This rate of sodium imbalance was defined in accordance with the literature data.
The second most frequent imbalanced electrolyte was calcium in our patients. Calcium has many functions in intracellular enzymatic pathways, and also plays a role in cellular damage and cell death.[16] We determined hypo- and hypercalcemia in 51% and 4% of our patients, respectively. Confusion was the most frequent finding in physical examinations, and this supposed to be a result of hypocalcemia in our patients. Other frequent findings in physical examinations of our patients were tetany and Chvostek-Trousseau signs, which may be associated with calcium balance disorders. We think that most of calcium imbalances were related to oncological diseases in our patients. The malignancy rate was as high as 39%, and the prevailing diagnoses were cancers of the lung and gastrointestinal system (23% each). The high rates of oncological diagnoses resulted in high frequencies of calcium balance disorders.
One of the main effects of high calcium levels is on the cardiovascular system and electrical transmission pathways of the heart. Therefore, we determined shortened corrected QT intervals and the first degree of atrioventricular block in ECG examinations. Compared these ECG findings according to the higher and lower levels of calcium, we found that hypocalcemic patients had more tachycardia, bradicardia and atrial fibrillation, and hypercalcemic patients had more atrioventricular blocks, spiked T waves and ST segment changes. The rates of these differences between the imbalance groups were statistically significant.
The third most frequent imbalance was in the level of potassium. We found the incidence of hypo- and hyperkalemia was 15% and 8% respectively in our patients. By checking physical examination findings, we found that hypokalemia was characterized by confusion, paresis, and aphasia. Although the clinical signs and symptoms cannot be attributed to a single disorder of electrolyte imbalances, it is meaningful to determine the physical aspects of hemodynamic changes of electrolyte levels in bloodstream. Hyperkalemia is a rare condition, but we found it in 8% of our patients. Williams et al[17] reported that potassium secretion from thrombocytes and leukocytes in severe thrombocytosis and leukocytosis may cause pseudo-hyperkalemia. We determined that the first three of most frequent diagnoses were sepsis, infections, and renal failure, and concluded that these clinical conditions, particularly renal failure, might have caused hyperkalemia in our patients. Statistical analyses showed that patients with hyperkalemia, but not with normo- or hypokalemia, had spiked T waves in ECG examinations. It is known that spiked T waves are specific to hyperkalemia, but not all of our patients with hyperkalemia had spiked T waves. We concluded that the interactions in multiple electrolytes had effect on ECG findings in these patients.
The least frequent electrolyte imbalances were hypo- and hypermagnesemia, which were determined in 5% and 1% of our patients, respectively. Hypomagnesemia is known to have a high prevalence rate, but its diagnosis may be intrigued by some factors. First, it has nonspecific manifestations, and frequently overlooked. Second, magnesium level is not examined “routinely” in blood test.[18] Third, patients may be hypomagnesemic, even with a normal serum magnesium level. And finally, magnesium deficiencies are generally masked by other electrolyte deficiencies.
In conclusion, our patients were diagnosed with various oncological diseases (40%). These malignancies expose a major risk for electrolyte imbalances. Therefore, we were aware of electrolyte imbalances in patients admitted to the ED, particularly in those with underlying oncological diseases. Hence our frequencies may not truly reflect the actual prevalence of each electrolyte's imbalance in the general population.
As we cannot assume that patients have single electrolyte imbalances, we conclude that clinical symptoms and findings are reflections of multiple interactions of electrolytes and regulatory systems in the organism. Therefore, ED physicians must be acknowledged of fluid-electrolyte balance dynamics because of the high incidence rate of clinical entities.
Footnotes
Funding: None.
Ethical approval: The local ethical committee of Uludag University Faculty of Medicine approved this study (17-Jan-2012; Approval No: 2012-2/16).
Conflicts of interest: There are no competing interests involving this study.
Contributors: Balcı AK proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts. All authors read and approved the final version of the manuscript.
REFERENCES
- 1.Lee CT, Guo HR, Chen JB. Hyponatremia in the emergency department. Am J Emerg Med. 2000;18:264–268. doi: 10.1016/s0735-6757(00)90118-9. [DOI] [PubMed] [Google Scholar]
- 2.Shiber JR, Mattu A. Serum phosphate abnormalities in the emergency department. J Emerg Med. 2002;23:395–400. doi: 10.1016/s0736-4679(02)00578-4. [DOI] [PubMed] [Google Scholar]
- 3.Bockenkamp B, Vyas H. Understanding and managing acute fluid and electrolyte disturbances. Current Paediatrics. 2003;13:520–528. [Google Scholar]
- 4.Ito H, Fujimaki H, Inoue J, Shiraki M. Disorders of fluid and electrolyte metabolism in elderly diabetics. Nihon Ronen Igakkai Zasshi. 1989;26:233–239. [PubMed] [Google Scholar]
- 5.Goldberg A, Hammerman H, Petcherski S, Zdorovyak A, Yalonetsky S, Kapeliovich M, et al. Prognostic importance of hyponatremia in acute ST-elevation myocardial infarction. Am J Med. 2004;117:242–248. doi: 10.1016/j.amjmed.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg A, Hammerman H, Petcherski S, Nassar M, Zdorovyak A, Yalonetsky S, et al. Hyponatremia and long-term mortality in survivors of acute ST-elevation myocardial infarction. Arch Intern Med. 2006;166:781–786. doi: 10.1001/archinte.166.7.781. [DOI] [PubMed] [Google Scholar]
- 7.Mahowald JM, Himmelstein DU. Hypernatremia in the elderly: relation to infection and mortality. J Am Geriatr Soc. 1981;29:177–180. doi: 10.1111/j.1532-5415.1981.tb01761.x. [DOI] [PubMed] [Google Scholar]
- 8.Sonnenblick M, Algur N. Hypernatremia in the acutely ill elderly patients: role of impaired arginine-vasopressin secretion. Miner Electrolyte Metab. 1993;19:32–35. [PubMed] [Google Scholar]
- 9.Solini A, Zamboni P, Passaro A, Fellin R, Ferrannini E. Acute vascular events and electrolytes variations in elderly patients. Horm Metab Res. 2006;38:197–202. doi: 10.1055/s-2006-925224. [DOI] [PubMed] [Google Scholar]
- 10.Clark BA, Shannon RP, Rosa RM, Epstein FH. Increased susceptibility to thiazide-induced hyponatremia in the elderly. J Am Soc Nephrol. 1994;5:1106–1111. doi: 10.1681/ASN.V541106. [DOI] [PubMed] [Google Scholar]
- 11.Miller PD, Krebs RA, Neal BJ, McIntyre DO. Hypodipsia in geriatric patients. Am J Med. 1982;73:354–356. doi: 10.1016/0002-9343(82)90726-4. [DOI] [PubMed] [Google Scholar]
- 12.Singal BM, Hedges JR, Succop PA. Efficacy of the stat serum electrolyte panel in the management of older emergency patients. Med Decis Making. 1992;12:52–59. doi: 10.1177/0272989X9201200109. [DOI] [PubMed] [Google Scholar]
- 13.Singal BM, Hedges JR, Succop PA. Prediction of electrolyte abnormalities in elderly emergency patients. Ann Emerg Med. 1991;20:964–968. doi: 10.1016/s0196-0644(05)82973-7. [DOI] [PubMed] [Google Scholar]
- 14.Wilson RF, Sibbald WJ. Fluid and electrolyte problems in the emergency department. JACEP. 1976;5:339–346. doi: 10.1016/s0361-1124(76)80058-5. [DOI] [PubMed] [Google Scholar]
- 15.Funk GC, Lindner G, Druml W, Metnitz B, Schwarz C, Bauer P, et al. Incidence and prognosis of dysnatremias present on ICU admission. Intensive Care Med. 2010;36:304–311. doi: 10.1007/s00134-009-1692-0. [DOI] [PubMed] [Google Scholar]
- 16.Bilezikian JP. Etiologies and therapy of hypercalcemia. Endocrinol Metab Clin North Am. 1989;18:389–414. [PubMed] [Google Scholar]
- 17.Williams ME, Rosa RM, Epstein FH. Hyperkalemia. Adv Intern Med. 1986;31:265–291. [PubMed] [Google Scholar]
- 18.Whang R, Hampton EM, Whang DD. Magnesium homeostasis and clinical disorders of magnesium deficiency. Ann Pharmacother. 1994;28:220–226. doi: 10.1177/106002809402800213. [DOI] [PubMed] [Google Scholar]


