Abstract
BACKGROUND:
The outcome of cardiopulmonary resuscitation (CPR) may depend on a variety of factors related to patient status or resuscitation management. To evaluate the factors influencing the outcome of CPR after cardiac arrest (CA) will be conducive to improve the effectiveness of resuscitation. Therefore, a study was designed to assess these factors in the emergency department (ED) of a city hospital.
METHODS:
A CPR registry conforming to the Utstein-style template was conducted in the ED of the First Affiliated Hospital of Wenzhou Medical College from January 2005 to December 2011. The outcomes of CPR were compared in various factors groups. The primary outcomes were rated to return of spontaneous circulation (ROSC), 24-hour survival, survival to discharge and discharge with favorable neurological outcomes. Univariate analysis and multivariable logistic regression analysis were performed to evaluate factors associated with survival.
RESULTS:
A total of 725 patients were analyzed in the study. Of these patients, 187 (25.8%) had ROSC, 100 (13.8%) survived for 24 hours, 48 (6.6%) survived to discharge, and 23 (3.2%) survived to discharge with favorable neurologic outcomes. A logistic regression analysis demonstrated that the independent predictors of ROSC included traumatic etiology, first monitored rhythms, CPR duration, and total adrenaline dose. The independent predictors of 24-hour survival included traumatic etiology, cardiac etiology, first monitored rhythm and CPR duration. Previous status, cardiac etiology, first monitored rhythms and CPR duration were included in independent predictors of survival to discharge and neurologically favorable survival to discharge.
CONCLUSIONS:
Shockable rhythms, CPR duration ≤15 minutes and total adrenaline dose ≤5 mg were favorable predictors of ROSC, whereas traumatic etiology was unfavorable. Cardiac etiology, shockable rhythms and CPR duration ≤15 minutes were favorable predictors of 24-hour survival, whereas traumatic etiology was unfavorable. Cardiac etiology, shockable rhythms, CPR duration ≤15 minutes were favorable predictors of survival to discharge and neurologically favorable survival to discharge, but previous terminal illness or multiple organ failure (MOF) was unfavorable.
KEY WORDS: Cardiac arrest, Cardiopulmonary resuscitation, Utstein-style, Logistical regression analysis, Outcome
INTRODUCTION
Cardiopulmonary resuscitation (CPR) has been used in clinical practice for over 50 years, and there have been many developments in resuscitation in recent years, but the clinical outcomes of CPR after cardiac arrest (CA) especially the rate of survival to discharge has not been satisfactorily improved.[1] The current research of resuscitation still focuses on influencing factors for outcomes of CPR and optimizing the effeciveness of resuscitation effort.[2] The recommended Utstein-style template[3–5] for uniform registering and reporting of data, as a basis of clinical research on resuscitation, has promoted the modification of international CPR guidelines,[6] which are urgently needed in the mainland of China. In the present study, the data of CA patients in emergency department (ED) were uniformly collected according to Utstein template, and the influencing factors for outcomes after CPR were analyzed in order to provide some evidence for domestic clinical research of CPR.
METHODS
Study subjects
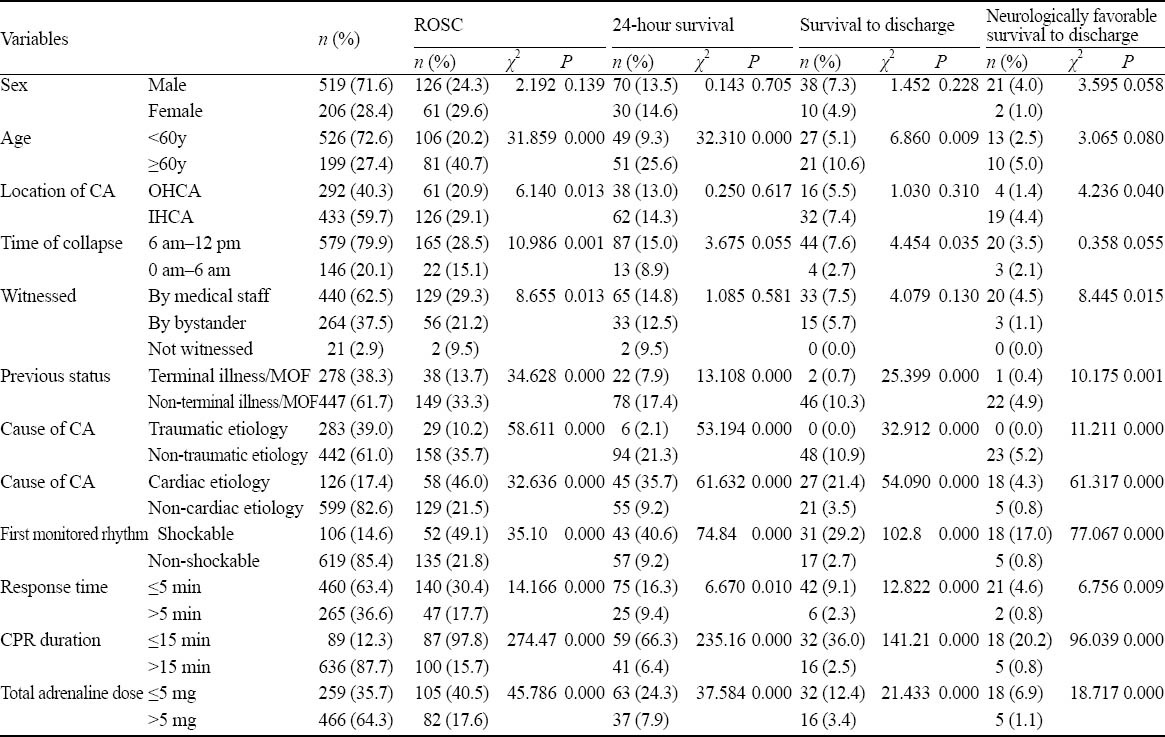
This randomized study included 725 consecutive patients presented in the ED of the First Affiliated Hospital of Wenzhou Medical College during January 2005 to December 2011, who underwent CA in the ED (in-hospital cardiac arrest, IHCA) or were imminently delivered to ED after out-of-hospital cardiac arrest (OHCA). The judging standard of CA conformed to the international guidelines of CPR. The exclusion criteria of patients included unknown arrest time, age <15 years, with DNAR (do not attempt resuscitation) decision, or incomplete registered data. A total of 725 patients were admitted to the ED with a mean age of 46.94±19.05 (range from 15 to 91 years). The different factors groups are showed in Table 1.
Table 1.
Outcomes of the patients in different factor groups after CPR
Data registration
The registry form of CPR, by reference to Utstein-style template[3–5] combined with epidemiology requirement, was applied timely to all patients who underwent CA and CPR. The data entry consisted of patients information (age, sex, illness, etc), CA information (time, site, etiology, witness, response time, duration of CPR, the first monitored rhythm, adrenaline doses, etc) and CPR outcomes (ROSC, 24-hour survival, survival to discharge, neurologically favorable survival to discharge, etc). The first monitored rhythm means the initial cardiac rhythm recorded via a cardiogram monitor or defibrillator, including ventricular fibrillation (VF), pulseless ventricular tachycardia (pulseless VT), asystole, pulseless electrical activity (PEA) and unknown rhythms. Shockable rhythms included VF and pulseless VT, and the rest were defined as non-shockable rhythms. Neurological outcome at hospital discharge was rated by cerebral performance category (CPC) scale: favorable neurological outcome (CPC 1–2, CPC 1=good cerebral performance, CPC 2=moderate cerebral disability) or unfavorable neurological outcome (CPC 3–4, CPC 3= severe cerebral disability, CPC 4=coma or vegetative).
CPR strategy
According to basic requirements of international guidelines or consensus, all patients accepted urgent CPR attempt consisted of continued chest compression, opening airway and breathing support (balloon mask, tracheal intubation and mechanical ventilation as necessary), rapid defibrillation as required, intravenous passageway for injection, adrenaline, and integrated post-cardiac arrest care.
Statistical analysis
Statistical analysis was performed using SPSS V13.0. The count data were presented by ratio, the chi-square test was used to analyze among groups. Univariate logistic regression analysis was performed to evaluate factors associated with outcome, and multivariate unconditional logistic regression analysis was made for significant variables (P≤0.05). Variables were screened step by step. The significance levels of introducing variables were set at αin=0.05, and those of eliminating variables were set at αout=0.1.
RESULTS
Comparison of outcomes for the patients in different factor groups after CPR
Of 725 patients, 187 (25.8%) had ROSC, 100 (13.8%) survived to 24 hours, 48 (6.6%) survived to hospital discharge, and 23 (3.2%) survived to discharge with favorable neurological outcomes. In comparison between different relevant factors groups, cardiac etiology, shockable rhythms, response time ≤5 minutes, duration of CPR ≤15 minutes, or total adrenaline doses ≤5 mg group had higher ROSC, 24-hour survival, survival to discharge and survival to discharge with favorable neurological outcomes (P<0.01); age ≥60 group had higher ROSC, 24-hour survival, survival to discharge (P<0.01); IHCA group or witnessed by medical staff group had higher ROSC and survival to discharge with favorable neurological outcomes (P<0.05); previous terminal illness/MOF group or traumatic etiology group had lower ROSC, 24-hour survival, survival to discharge and discharge with favorable neurological outcomes (P<0.01); CA during 0 am–6 am group had lower ROSC (P<0.01) and survival to discharge (P<0.05) (Table 1).
Univariate logistic regression analysis of factors related to outcomes after CPR
In univariate logistic regression analysis, 11 variables including age, location, time, witness, previous status, traumatic etiology, cardiac etiology, first monitored rhythms, response time, duration of CPR and total adrenaline does were correlated with ROSC (P<0.01 or P<0.05); 8 variables including age, previous status, traumatic etiology, cardiac etiology, first monitored rhythms, response time, duration of CPR and total adrenaline dose were correlated with 24-hour survival (P<0.01 or P<0.05); 9 variables including age, time, previous status, traumatic etiology, cardiac etiology, first monitored rhythms, response time, duration of CPR and total adrenaline dose were correlated with survival to discharge (P<0.01 or P<0.05). Nine variables including location, witness, previous status, traumatic etiology, cardiac etiology, first monitored rhythms, response time, duration of CPR, and total adrenaline does were correlated with survival to discharge with favorable neurological outcomes (P<0.01 or P<0.05) (Table 2).
Table 2.
Univariate logistic regression analysis on factors related to outcomes after CPR

Multivariate logistic regression analysis of factors related to outcomes after CPR
Multivariate logistic regression analysis revealed that the independent predicting factors associated with ROSC included taumatic etiology, first monitored rhythms, duration of CPR, and total adrenaline dose, in which taumatic etiology was an unfavorable predictor (P<0.01), whereas shockable rhythms, duration of CPR ≤15 minutes and total adrenaline dose ≤5 mg were favorable predictors (P<0.01 or P<0.05). Moreover the independent predicting factors associated with 24-hour survival included taumatic etiology, cardiac etiology, first monitored rhythms, and duration of CPR, in which taumatic etiology was an unfavorable predictor (P<0.01), whereas cardiac etiology, shockable rhythms, and duration of CPR ≤15 minutes were favorable predictors (P<0.01 or P<0.05); the independent predicting factors associated with survival to discharge and survival to discharge with favorable neurological outcomes included previous status, cardiac etiology, first monitored rhythms, duration of CPR, in which cardiac etiology, shockable rhythms, and duration of CPR ≤15 minutes were favorable predictors (P<0.01), whereas terminal illness/MOF was an unfavorable predictor (P<0.01) (Table 3).
Table 3.
Multivariate logistic regression analysis on factors related to outcomes after CPR

DISCUSSION
Although resuscitation is evolving rapidly in several ways, the overall outcome after CPR is still unsatisfactory clinically, and the rate of survival to discharge has not been substantially improved since 2005.[6] As the most severity and complexity of pathological state and event, CA patients have to be attempted the essential resuscitation so as to ensure each link of chain of life. Therefore, to assess the factors influencing the outcome of CPR will help to evaluate the efficiency of resuscitation. Utstein-style definitions and reporting templates have been used while increasing effectively the clinical outcomes after resuscitation and making great progress toward international guidelines or consensus on resuscitation science.[5,6] In recent years, Utstein-style registering templates have been used clinically in a few domestic regions.[7–11]
The survival rate of patients with traumatic CA is poor.[12] A study reported that patients with traumatic CA admitted to ICU from ED had a poorer survival rate of discharge compared with patients with non-traumatic CA,[13] but in 383 traumatic CA patients, 25.8% had ROSC, 13% survived 24 hours, 7% survived to discharge, and 3% survived to discharge with favorable neurological outcomes.[14] In the present study, patients with traumatic CA accounted for 39.0% (283/725). Of the 283 patients with traumatic CA, 10.2% had ROSC, 2.1% survived for 24 hours, and none survived to discharge. Multivariate logistic regression analysis demonstrated that traumatic etiology was an independent unfavorable predictor for ROSC and 24-hour survival. The traumatic CA patients suffered from severe craniocerebral injury and late hemorrhage shock, and 67.5% of them had previous MOF/terminal illness, which may result in poor outcomes. In MOF/terminal illness patients (278/725, 38.3%), 13.7% had ROSC, 7.9% survived for 24 hours, 0.7% survived to discharge and 0.4% survived to discharge with favorable neurological outcomes. Multivariate logistic regression analysis showed MOF/terminal illness was an independent unfavorable predictor for surviving to discharge and surviving to discharge with favorable neurological outcomes.
Different with the reported results[15], age <60 group had poorer outcomes of CPR than age ≥60 group in our study, and traumatic etiology and MOF/terminal illness status occupied a larger proportion in age <60 group than age ≥60 group (49.0% vs. 12.6%, 41.6% vs. 29.6%). Univariate logistic regression analysis showed that age was a relevant factor for ROSC, 24-hour survival and surviving to discharge, but multivariate logistic regression analysis denied that age is associated with the outcome of CPR.
Compared with OHCA, IHCA had a 2.52 times chance to ROSC and a 8.69 times chance to discharge,[16] and had a 1.4 times chance to ROSC and a 3.1 times chance to discharge with favorable neurological outcomes (P<0.05), but there was no significant difference in 24-hour survival or survival to discharge in the present study. In a study by Dumot et al,[17] CA with witness had a 2.2 times chance for surviving to discharge, compared with CA without witness. Rafati et al[18] also reported the similar observation. Of the 725 patients in our study, 97.1% were witnessed, therein 89.4% of OHCA witnessed by bystander vs. 99.3% of IHCA witnessed by medical staff. Among different witness groups, CA witnessed by medical staff had a better rate of ROSC and surviving to discharge with favourable neurological outcomes than witnessed by bystanders, and the worst was no witness (P<0.05).
Gomes et al[15] reported that 50% of CA patients in a general hospital had cardiac etiology. Herlitz et al[19] reported that 15% of 1 105 young adults with OHCA had cardiac etiology, and 14.8% of cardiac CA patients survived to 1 month. In the present study, 17.4% of all 725 patients had cardiac CA and they had higher ratios of ROSC and surviving to discharge with favorable neurological outcomes compared with those without cardiac CA. Univariate logistic regression analysis showed that cardiac etiology was a favorable predictor for ROSC, 24-hour survival, surviving to discharge or surviving to discharge with favorable neurological outcomes, and multivariate logistic regression analysis showed it was a favorable predictor for 24-hour survival, surviving to discharge or surviving to discharge with favorable neurological outcomes.
Shockable rhythms were verified not to be a large proportion in the initial monitored rhythms. A study[20] showed that of 14 420 patients with OHCA, 26% had shockable rhythms, and in another study, asystole accounted for 42%, and VF or VT, 35%.[15] Herlitz et al[19] reported that 17% of young adults with OHCA had VF and 20.8% of them survived to 1 month, and they believed that ventricular fibrillation at the arrival of the rescue team was an independent predictor of increased chance for survival. Rafati et al[18] found that 16% of 256 patients had VF or VT, and their survival rate of hospital discharge was respectively 40% or 25%. In a larger number of trials reviewed by Nadkarni et al,[21] in 36 902 adult CA patients, the prevalence of VF or pulseless VT as the initially monitored rhythm was 23%, whereas the prevalence of asystole and PEA was 35% and 32% respectively, and those with VF or pulseless VT (62%) had ROSC, 47% survived 24 hours, and 36% survived to hospital discharge. In our study, 106 (14.6%) of 725 patients showed shockable rhythms in the initial rhythms, and 49.1% had ROSC, 40.6% survived for 24 hours, 29.2% survived to hospital discharge, 17.0% survived to discharge with favorable neurological outcomes. Multivariate logistic regression analysis revealed that the initial shockable rhythm was an independent favourable predictor for ROSC, survival at 24 hours, survival to hospital discharge and survival to discharge with favorable neurological outcomes.
Hajbaghery et al[22] found that all patients survived to discharge and 97.5% of patients with a short-term survival had a response within 1–6 minutes, and 81.8% of them survived to hospital discharge were resuscitated within the first 3 minutes after CA. Gomes et al[15] reported that the patients with a response time of ≤5 minutes had a 2.53 times chance to survive compared with those with a response time of >5 minutes. In our study, CA patients with a response time of ≤5 minutes had a higher rate of ROSC, survived for 24 hours, survived to hospital discharge, or survived to discharge with favorable neurological outcomes, compared those with a response time of >5 minutes.
It was reported that those with cardiac arrest during 0 am–6 am had a poor ROSC and survived to discharge. Patients with CA during 0 am–6 am had also a poor outcome after CPR. There was a significant difference in 24-hour survival (P<0.01) and survival to discharge (P<0.05) compared during other periods of time in our study. Among them who had cardiac arrest during 0 am–6 am, 48.6% had traumatic etiology and 52.7% had MOF/terminal illness.
The duration of CPR over 10 minutes, even over 15 minutes, was reported as an independent unfavorable predictor for ROSC and survival to discharge.[14,17,18] Hajbaghery et al[22] thought that the duration of CPR could be used to assess the response time, the severity of patients, and the efficiency of CPR. In our study, the patients with a duration of CPR ≤15 minutes had a better outcome of ROSC, 24-hour survival, survival to hospital discharge, and neurologically favorable survival to discharge. Among all patients who survived to discharge, 66.7% (32/48) had a duration of CPR ≤15 minutes, and in addition, among all patients who survived to discharge with favorable neurological outcomes, 78.3% (18/23) had a duration of CPR ≤15 minutes. Multivariate logistic regression analysis showed that the duration of CPR ≤15 minutes was a favorable predictor for outcomes of CPR.
Studies found that less total adrenaline given during CPR was a favorable predictor for ROSC.[15,17] In the present study, the patients with total adrenaline ≤5 mg had a better ROSC, survived for 24 hours, survived to hospital discharge, or survived to discharge with favourable neurological outcomes, compared those with total adrenaline >5 mg (P<0.01), whereas multivariate logistic regression analysis showed that total adrenaline level ≤5 mg was identified as a favorable predictor for ROSC. Currently, a larger number of trials and a randomized controlled trial[23,24] focused on outcomes of CA patients whenever adrenaline given or not. It was verified that adrenaline administration was associated with improved short-term survival (ROSC/being admitted to hospital), but decreased survival to 1 month/hospital discharge and survival with favorable neurological outcome after OHCA.
Footnotes
Funding: This study was supported by grants from Important Scientific Research Project of Wenzhou Medical College (yxyzd-B2005-03) and Undergraduate Students Research Project in Innovating and Pioneering of Zhejiang Province (2008 year).
Ethical approval: The present study was approved the Ethical Committee of the First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China.
Conflicts of interest: The authors declare that there is no conflict of interest in this study.
Contributors: Chen SQ designed the study and finalized the manuscript. Xue JK, Leng QY and Gao YZ wrote the first draft. All authors contributed to registering effectiveness and approved the final version.
REFERENCES
- 1.Hazinski MF, Nolan JP, Billi JE, Böttiger BW, Bossaert L, de Caen AR, et al. Part. 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendation. Circulation. 2010;122:S250–S275. doi: 10.1161/CIRCULATIONAHA.110.970897. [DOI] [PubMed] [Google Scholar]
- 2.He AW, Chen SQ. The new development on science of cardiopulmonary resuscitation. Chin Crit Care Med (electrical) 2012;4:218–223. [Google Scholar]
- 3.Reardon PM, Magee K. Epinephrine in out-of-hospital cardiac arrest: A critical review. World J Emerg Med. 2013;4:85–91. doi: 10.5847/wjem.j.issn.1920-8642.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. A statement for healthcare professionals from the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, the Australian Resuscitation Council, and the Resuscitation Councils of Southern Africa. Resuscitation. 1997;34:151–183. doi: 10.1016/s0300-9572(97)01112-x. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 6.Nadkarni VM, Nolan JP, Billi JE, Bossaert L, Böttiger BW, Chamberlain D, et al. Part. 2: International collaboration in resuscitation science: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122:S276–S282. doi: 10.1161/CIRCULATIONAHA.110.970921. [DOI] [PubMed] [Google Scholar]
- 7.Ezquerra García AM, Suberviola, Fernández I, Pavía Pesquera MC. Evaluation of the effectiveness of an in-hospital cardiac alarm system. Enferm Intensiva. 2009;20:58–68. doi: 10.1016/s1130-2399(09)71147-2. [DOI] [PubMed] [Google Scholar]
- 8.Wallace SK, Abella BS, Shofer FS, Leary M, Agarwal AK, Mechem CC, et al. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation. 2013 Mar 18; doi: 10.1161/CIRCULATIONAHA.113.002058. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Nicolasora N, Pannala R, Mountantonakis S, Shanmugam B, DeGirolamo A, Amoateng-Adjepong Y, et al. If asked, hospitalized patients will choose whether to receive life-sustaining therapies. J Hosp Med. 2006;1:161–167. doi: 10.1002/jhm.78. [DOI] [PubMed] [Google Scholar]
- 10.Roshana S, Batajoo KH, Piryani RM, Sharma MW. Basic life support: knowledge and attitude of medical/paramedical professionals. World J Emerg Med. 2012;3:141–145. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsung JW, Blaivas M. Feasibility of correlating the pulse check with focused point-of-care echocardiography during pediatric cardiac arrest: a case series. Resuscitation. 2008;77:264–269. doi: 10.1016/j.resuscitation.2007.12.015. Epub 2008 Feb 15. [DOI] [PubMed] [Google Scholar]
- 12.Lockey D, Crewdson K, Davies G. Traumatic cardiac arrest: who are the survivors? Ann Emerg Med. 2006;48:240–244. doi: 10.1016/j.annemergmed.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 13.Lundy DJ, Ross SE, Schorr C, Jones AE, Trzeciak S. Outcomes of trauma victims with cardiac arrest who survive to intensive care unit admission. J Trauma. 2011;71:E12–16. doi: 10.1097/TA.0b013e3181fc5c70. [DOI] [PubMed] [Google Scholar]
- 14.Gräsner JT, Wnent J, Seewald S, Meybohm P, Fischer M, Paffrath T, et al. Cardiopulmonary resuscitation traumatic cardiac arrest—there are survivors. An analysis of two national emergency registries. Crit Care. 2011;15:R276. doi: 10.1186/cc10558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gomes AM, Timerman A, Souza CA, Mendes CM, Póvoas Filho HP, Oliveira AM, et al. Prognostic factors of survival in post-cardiopulmonary-cerebral resuscitation in general hospital. Arq Bras Cardiol. 2005;85:262–271. doi: 10.1590/s0066-782x2005001700006. [DOI] [PubMed] [Google Scholar]
- 16.Ishtiaq O, Iqbal M, Zubair M, Qayyum R, Adil M. Outcome of cardiopulmonary resuscitation -predictors of survival. J Coll physicians Surg Pak. 2008;18:3–7. [PubMed] [Google Scholar]
- 17.Dumot JA, Burval DJ, Sprung J, Waters JH, Mraovic B, Karafa MT, et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of “limited“ resuscitations. Arch Intern Med. 2001;161:1751–1758. doi: 10.1001/archinte.161.14.1751. [DOI] [PubMed] [Google Scholar]
- 18.Rafati H, Saghafi A, Saghafinia M, Panahi F, Hoseinpour M. Survival after in-hospital cardiopulmonary resuscitation in a major referral center during 2001–2008. Iran J Med Sci. 2011;36:50–53. [PMC free article] [PubMed] [Google Scholar]
- 19.Herlitz J, Svensson L, Silfverstolpe J, Angquist KA, Wisten A, Engdahl J, et al. Characteristics and outcome amongst young adults suffering from out-of-hospital cardiac arrest in whom cardiopulmonary resuscitation is attempted. J Intern Med. 2006;260:435–441. doi: 10.1111/j.1365-2796.2006.01705.x. [DOI] [PubMed] [Google Scholar]
- 20.Weisfeldt ML, Everson-Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, et al. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 22.Hajbaghery MA, Mousavi G, Akbari H. Factors influencing survival after in-hospital cardiopulmonary ouresuscitation. Resuscitation. 2005;66:317–321. doi: 10.1016/j.resuscitation.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Ducros L, Vicaut E, Soleil C, Le Guen M, Gueye P, Poussant T, et al. Prehospital epinephrine use and survival among patients with t-of-hospital cardiac arrest. JAMA. 2012;307:1161–1168. doi: 10.1001/jama.2012.294. [DOI] [PubMed] [Google Scholar]
- 24.Olasveengen TM, Wik L, Sunde K, Steen PA. Outcome when adrenaline (epinephrine) was actually given vs. not given -post hoc analysis of a randomized clinical trial. Resuscitation. 2012;83:327–332. doi: 10.1016/j.resuscitation.2011.11.011. [DOI] [PubMed] [Google Scholar]


