Abstract
BACKGROUND:
Rapid sequence induction and intubation (RSII) is a medical procedure involving a prompt induction of general anesthesia by using cricoid pressure that prevents regurgitation of gastric contents. The factors affecting RSII are prophylaxis for aspiration, preoxygenation, drug and equipment preparation for RSII, ventilation after induction till intubation and patient condition. We sometimes saw difficulties with the practice of this technique in our hospital operation theatres. The aim of this study was to assess the techniques of rapid sequence induction and intubation.
METHODS:
Hospital based observational study was conducted with a standardized checklist. All patients who were operated upon under general anesthesia during the study period were included. The techniques of RSII were observed during the induction of anesthesia by trained anesthetists.
RESULTS:
Altogether 140 patients were included in this study with a response rate of 95.2%. Prophylaxis was not given to 130 patients (92.2%), and appropriate drugs were not used for RSII in 73 patients (52.1%), equipments for difficult intubation in 21 (15%), suction machines with catheter not connected and turned on in 122 (87.1%), ventilation for patients after induction and before intubation in 41 (29.3%), cricoid pressure released before cuff inflation in 12 (12.1%), and difficult intubation in 8 (5.7%), respectively. RSII with cricoid pressure was applied appropriately in 94 (67.1%) patients, but cricoid pressure was not used in 46 (32.9%) patients.
CONCLUSIONS:
The techniques of rapid sequence induction and intubation was low. Training should be given for anesthetists about the techniques of RSII.
KEY WORDS: Rapid sequence, Induction, Intubation, Pulmonary aspiration, General anesthesia
INTRODUCTION
Airway control is the initial priority in the management of emergency and elective patients with the risk of pulmonary aspiration.[1] Rapid sequence induction and intubation (RSII) is preferred in emergency department because it results in rapid unconsciousness and neuromuscular blockage paralysis.[2] Before rapid sequence induction, a clinician or anesthetist must ensure a successful intubation following the assessment of airway.[3]
Manual ventilation before tracheal intubation was avoided to prevent gastric distension. Cricoid pressure is most debatable in its effectiveness in preventing pulmonary aspiration.[4] It is used by 10 N force before induction and by 20–30 N after induction of anesthesia.[5] RSII should be approached cautiously in patients with the difficult airway.[6]
In the USA study, about 93% of 610 patients were intubated, but RSII was used with cricoid pressure in 84%.[7] Other studies from the emergency departments of the USA, Canada and Singapore showed that of 7 712 patients who had emergency intubation, 49% underwent RSII.[8]
A study from Ottowan University Hospital, Canada showed that in a total of 184 clinical trials, of which 163 were randomized control trials, 52 were evaluated by cricoid pressure. The outcomes showed that the prevention of aspiration and mortality could not be evaluated from the trials because the components of rapid sequence induction were uncertained.[9]
The rate of aspiration was found to be increased from 1.9% with one attempt to 22% with three or more attempts during intubation.[10] Over the past decades, the practice of rapid sequence induction was evolved with newer drugs and equipments, but the practice was different from country to country and from anesthetist to anesthetist.[11]
A French study[12] showed that aspiration in 1 of 7 400 cases caused 1 death of 33 000 anesthetics. The authors of this study concluded that rapid sequence induction was employed to minimize this risk. Morgan and colleagues[13] reported the results after the use of the best induction agent in the absence of neuromuscular blocking agents. Studies on the efficacy of cricoids pressure showed success in preventing regurgitation.[14]
Many emergency and elective patients with a high risk of pulmonary aspiration were operated upon under anesthesia in our hospital. We found occasionally difficulty in application of this technique. This study aimed to assess the techniques of rapid sequence induction and intubation, and factors affecting this technique.
METHODS
Patients
An observational study was conducted from April 21 to May 21, 2013 in our hospital. The study subjects included emergency and elective adult or pediatric patients with a risk of aspiration who were operated on under general anesthesia with rapid sequence induction and intubation during the study period.
Patients with a risk of aspiration who were subjected to surgery for fracture of the cervical spine, those with anticipated difficulty in intubation, and those who were operated on under regional anesthesia and sedation were excluded.
Age, sex, mallampati score, ASA status, preoperative respiratory disease, and preoperative oxygen desaturation of the patients and experience of qualified anesthetists were recorded.
Also recorded were prophylaxis for aspiration, types of surgery, suction machines with a catheter ready for use, equipments for difficult intubation, presence of assistant, professional status of assistant, cricoid pressure applied or not, types of drugs used for induction and relaxation, preoxygenation, ventilation after induction till intubation with the cuff being inflated, laryngoscopic attempts, patient position, difficult intubation, and complications during intubation.
Operation
Rapid sequence induction and intubation
The technique that is carried out by a practicing anesthetist includes preoxygenation, rapid use of predetermined induction and paralytic drugs, concurrent application of cricoid pressure, avoidance of bag and mask ventilation, and direct laryngoscopy followed by a tracheal intubation accompanied with a suction machine with a suction catheter for ready use. Cricoid pressure was applied till the endotracheal tube cuff was inflated.
When the assistance identified the anatomic landmark for cricoid pressure before induction, and the applied cricoid pressure after loss of consciousness or the anatomic landmark was identified after induction and cricoid pressure was applied after loss of consciousness or application of both anatomic landmark identification and cricoid pressure after induction and loss of consciousness.
Cricoid pressure and RSII technique
If anatomic landmark is identified before induction of anesthesia, 10 N can be applied and continues with 20–30 N after induction till the endotracheal tube cuff is being inflated.
Since RSII is a critical and life-saving technique, it should be used for every patient with a risk of aspiration unless there is a special consideration. Drugs must be as much as possible with rapid onset and offset induction anesthetic drugs and muscle relaxants though it may be affected by the available facilities. All consecutive emergency and elective adult and pediatric patients with a risk of aspiration, who were operated on under general anesthesia with rapid sequence induction and intubation during the study period in our hospital, were included.
Data collection and analysis
An English version of standardized checklist was used for data collection, and patients' charts were reviewed. Two trained anesthetists were involved in data collection. Data collectors were trained, and pre-test was done. The data collectors were supervised by investigators.
Data analysis
Windows version 20.0 software was used for data analysis. Descriptive statistics were presented in Tables.
Ethical consideration
Ethical approval was obtained from the institutional ethical review committee. Both participating patients and qualified anesthetists were blinded to the study. Confidentiality was ensured by using the anonymous checklist and keeping the checklist locked.
RESULTS
Altogether 147 patients were operated on during the study. Seven patients were excluded from the study because 5 patients had no data collected and 2 patients had incomplete data.
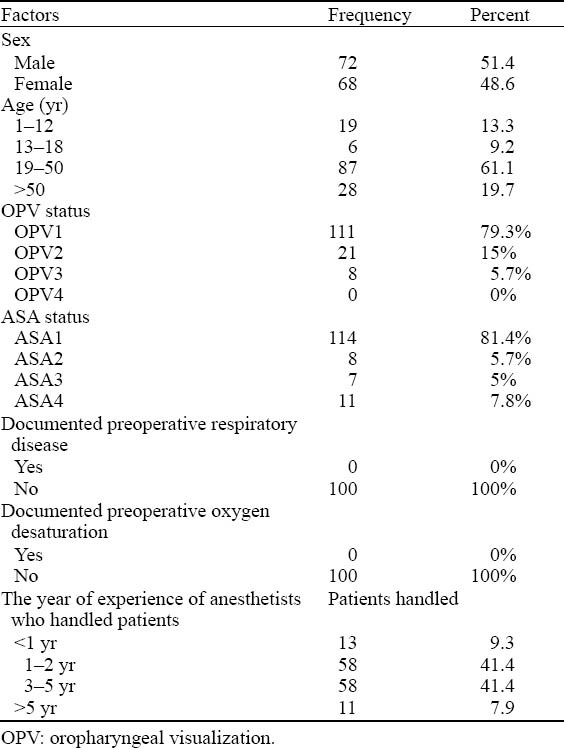
A total of 140 patients were included in this study with a response rate of 95.2%. In these patients, 72 (51.4%) were male and 68 (48.6%) female. The age of 19 (13.3%) patients ranged from 1 to 12 years, 6 (9.2%) from 12 to 18 years, 87 (61.1%) from 19 to 50 years, and 28 (19.7%) was >50 years, respectively.
Fifty-eight (41.4%) of the procedures were done by anesthetists with 1–2 years of experience, 58 (41.4%) by those with 3–5 years of experience, 13 (9.3%) by those with less than 1 year of experience and 11 (7.9%) by those with more than 5 years of experience, respectively (Table 1).
Table 1.
Socio-demographic characteristics of the respondents, 2013 (n=140)
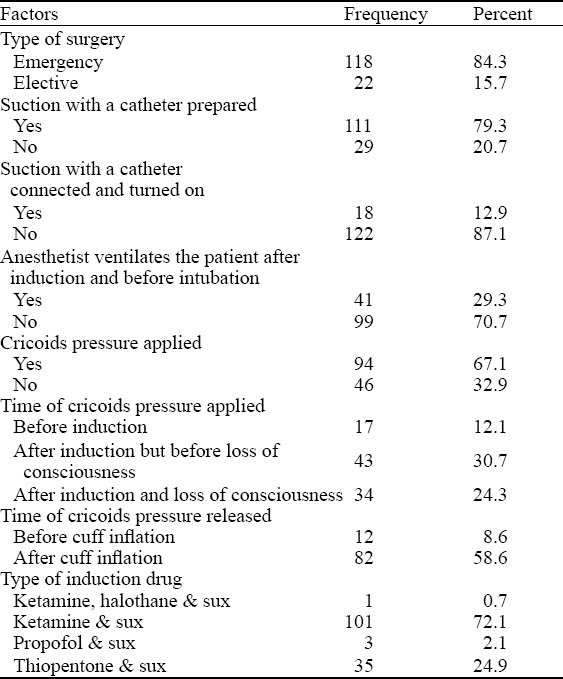
The majority (118, 84.3%) of procedures were emergency procedures. Most patients (130, 92.2%) were not given prophylactic drugs as a pretreatment for pulmonary aspiration. Seven patients (5%) were given methoclopromide, 2 (1.4%) cimetidine, and 1 (0.7%) methoclopromide and cimetidine, respectively. Seven (5%) patients were given prophylactic drugs before 30 minutes and 3 (2.1%) in less than 30 minutes before surgery. Appropriate drugs for RSI were not prepared for 73 (52.1%) patients. Most of the intubations (126, 90%) were performed in supine position and 14 (10%) in head up position.
Monitors used during the procedure were 3 lead ECG, pulseoximetry, and non-invasive blood pressure apparatus. All patients (140, 100%) were pre-oxygenated with 100% of oxygen before induction of anesthesia.
Suction machine with a catheter was used in 111 (79.3%) patients before induction of anesthesia, and in 122 (87.1%) patients the catheter was not connected and turned on during induction of anesthesia. Anesthetists had assistants for 138 (98.6%) patients. Cricoids pressure was used in 41 (29.3%) of the procedures by 4 year anesthesia students, in 37 (26.4%) by qualified anesthetists, in 13 (9.3%) by 3rd year anesthesia students, and in 3 (2.1%) by others.
Equipments for difficult intubation were prepared for 109 (77.9%) patients. One hundred and thirty-two (94.3%) patients were intubated without the use of difficult airway equipments. Of these, 85 (60.7%), 30 (21.4%) and 17 (12.1%) patients were intubated after first, second and third laryngoscopy attempts respectively. Ten patients among those who intubated after the second laryngoscopy attempt developed moderate hypoxia (<90%), whereas 6 (4.3%) patients who were intubated after the third laryngoscopy attempt developed severe hypoxia (<85%) during RSII. Six of ten (4.3%) patients who developed moderate hypoxia were American Society of Anesthesiologists class three (ASA3), whereas three (2.1%) patients among those who developed severe hypoxia were ASA4. Difficult intubation happened in 8 patients where 6 (4.3%) patients were intubated with stylet and 2 (1.4%) patients using bougie. Of those patients with difficult intubation, 1 (1.4%), 3 (2.1%) and 4 (2.8%) patients had mallampati score (OPV) OPV1, OPV2 and OPV3, respectively. There were no other immediate complications during RSII other than hypoxia and difficult intubation (Table 2).
Table 2.
Factors related to anesthesia and surgery, 2013 (n=140)
The anesthetists did not get any updating training about the techniques of rapid sequence induction and intubation after graduation except during the undergraduate and postgraduate courses irrespective of the contents and the sufficiency of the training provided.
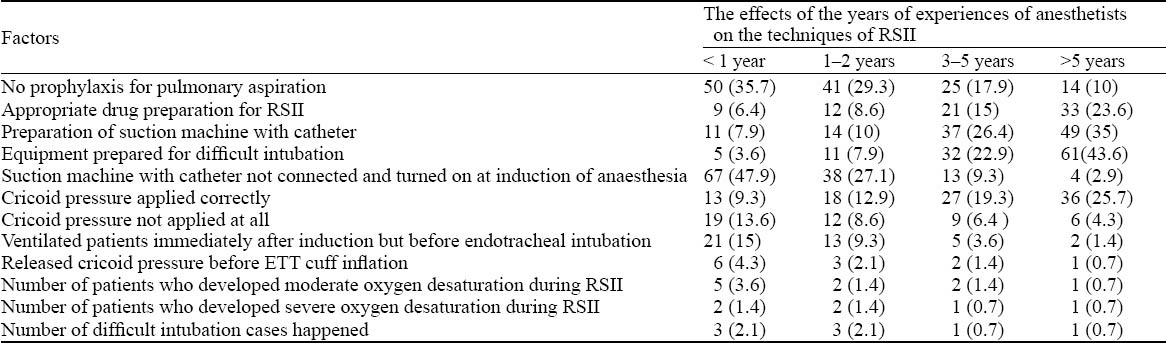
The years of experiences of anesthetists markedly affected the anesthetists’ techniques about rapid sequence induction and intubation in our hospital. Equipments for difficult intubation were prepared for 5 (3.6%), 11 (7.9%), 32 (22.9%) and 61 (43.6%) patients by the anesthetist with the years of experiences of less than 1 year,1–2 years, 3–5 years, and more than 5 years, respectively. On the other hand, cricoid pressure was not applied at all during RSII for 19 (13.6%), 12 (8.6%), 9 (6.4%), and 6 (4.3%) patients by the anesthetist with the years of experiences of less than 1 year, 1–2 years, 3–5 years and more than 5 years, respectively (Table 3).
Table 3.
The effects of the years of experiences of anesthetists on the techniques of rapid sequence induction and intubation, 2013 (n, %)
DISCUSSION
The induction of general anesthesia in patients with risk of aspiration can result in regurgitation of gastric content and pulmonary aspiration. The role of rapid sequence induction and intubation is to minimize the time interval between the loss of the airway protection reflexes and intubation with an endotracheal tube. Although RSII has possible complications such as hypoxia, bradycardia, precipitating an emergent airway, and various steps have been suggested, it remains the standard of care in emergency airway management for patients with a risk of aspiration, who would be operated on under general anesthesia with endotracheal intubation.
In this study, the raid sequence induction and intubation technique with cricoid pressure application was used in 94 (67.1%) patients. This finding was not similar to a study conducted in the USA where the use of RSII technique was 84%.[9] This discrepancy could be due to a difference in study design and training methods on techniques of RSII for anesthetists and physicians.
In our study, prophylaxis was not given for 130 (92.2%) patients, appropriate drugs were not prepared for RSII for 73 (52.1%) patients, equipments for difficult intubation were not prepared for 21 (15%) patients, suction machine with a suction catheter was not connected and turned on during the induction of anesthesia for 122 (87.1%) patients and cricoid pressure released before cuff inflation for 12 (12.1%) patients, respectively. These areas of poor practice might predispose patients to different complications during the perioperative period.
In this study, the timing of anatomic land mark identification before induction, after induction but before loss of consciousness, and after induction and loss of consciousness was 17 (12.1%), 43 (30.7%) and 34 (24.3%), respectively. These figures were lower than those reported by a study from North Carolina (19%, 70% and 10% respectively).[15] This discrepancy might be due to a difference in training of anesthetists and physicians, and there are also variations regarding the techniques of RSII across the world.
In this study, the anesthetists ventilated 41 (29.3%) patients after induction, before intubation and endotracheal tube cuff inflation. This finding was not in line with the study from North Carolina where the ventilation rate was 63 %.[15] This discrepancy might be due to frequent desaturation in Carolina because there were a large number of obese patients. But in our study, the patients were slim and desturation might not be frequent during induction of anesthesia unlike in Carolina. The other explanation could be the number of patients with anticipated difficult mask ventilation and intubation that would affect the need to ventilate after induction.
In our study, ketamine and suxamethonium were used as induction agents in 101 (72.1%) patients, and thiopental and suxamethonium in 35 (24.9%) patients. This could be due to the trend to use ketamine and suxamethonium for induction of anesthesia in our hospital unless there is specific contraindication such as hypertension and head injury for ketamine, and major burn for suxamethonium.
In conclusion, the techniques of rapid sequence induction and intubation were not satisfactory in our hospital's operation theatres. The years of experiences of anesthetists markedly affected the anesthetists' techniques including rapid sequence induction and intubation. Most patients were not given pretreatment prophylaxis in case of risk of aspiration. Appropriate equipments and drugs were not prepared for RSII and difficult intubation in many patients. Cricoid pressure was not applied for a large number of patients. Many anesthetists ventilated the patients after induction and before intubation, and some of the anesthetists released cricoid pressure before endotracheal tube cuff inflation.
Footnotes
Funding: None.
Ethical approval: The study was approved by the institutional ethical board of University of Gondar.
Conflicts of interest: The authors do not have any conflict of interest.
Contributors: Endale GG proposed the study, analyzed the data and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Reynolds SF, Heffner J. Air way management of the critically ill patients. Rapid sequence induction. Chest. 2005;127:1397–412. doi: 10.1378/chest.127.4.1397. [DOI] [PubMed] [Google Scholar]
- 2.Sagarin MJ, Barton ED, Chng YM, Walls RM. National Emergency Airway Registry Investigators. Air way management by USA and Canadian emergency medicine residents. Multicenter analysis of more than 6000 endotracheal tube attempts. Ann Emerg Med. 2005;46:328–336. doi: 10.1016/j.annemergmed.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Bair AE, Filbin MR, Kulkarni RG, Walls RM. The failed intubation attempt in the emergency department. Analysis of prevalence, rescue techeniques and personnel. J Emerge Med. 2002;23:131–140. doi: 10.1016/s0736-4679(02)00501-2. [DOI] [PubMed] [Google Scholar]
- 4.EL-Orbany M, Connoly LA. Rapid sequence induction and intubation. Current controversy. Anesth Analg. 2010;110:1318–1325. doi: 10.1213/ANE.0b013e3181d5ae47. [DOI] [PubMed] [Google Scholar]
- 5.Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department: rapid sequence tracheal intubation. A risk- benefit analysis. Ann Emerg Med. 2007;50:653. doi: 10.1016/j.annemergmed.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Wilcox SR, Bittner EA, Elmer J, Seigel TA, Nguyen NT, Dhillon A, et al. Neuromuscular blocking agent administration for emergent tracheal intubation is associated with decreased prevalence of procedure-related complications. Crit Car Med. 2012;40:1808–1813. doi: 10.1097/CCM.0b013e31824e0e67. [DOI] [PubMed] [Google Scholar]
- 7.Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Air way management in the emergency department. A one year study of 610 tracheal intubation. Ann Emerg Med. 1998;31:325. doi: 10.1016/s0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 8.Bair AE, Filbin MR, Kulkarni RG, Walls RM. The failed intubation attempt in the emergency department. Analysis of prevalence, risk technique and personnel. Emerg Med. 2005;28:131. doi: 10.1016/s0736-4679(02)00501-2. [DOI] [PubMed] [Google Scholar]
- 9.Neilipovitz DT, Crosby ET. Evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anaesth. 2007;54:748–764. doi: 10.1007/BF03026872. [DOI] [PubMed] [Google Scholar]
- 10.Mort TC. Emergency tracheal intubation. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 11.Morris J, Cook TM. Rapid sequence induction. A national survey of practice. Anaesthesia. 2001;56:109–115. doi: 10.1046/j.1365-2044.2001.01962.x. [DOI] [PubMed] [Google Scholar]
- 12.Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration in the perioperative period. Anesthesiology. 1993;78:56–62. doi: 10.1097/00000542-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, suxamethonium and vecuronium for rapid sequence induction of anaesthesia in adult patients. Anesthesiology. 1993;79:913–918. doi: 10.1097/00000542-199311000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Vanner RG, Assai T. Safe use of cricoids pressure. Anaesthesia. 1999;54:1–3. doi: 10.1046/j.1365-2044.1999.00756.x. [DOI] [PubMed] [Google Scholar]
- 15.Schelesinger S, Blanchfield D. Modified rapid-sequence induction of anesthesia: a survey of current clinical practice. AANA J. 2001;69:4. [PubMed] [Google Scholar]


