Abstract
BACKGROUND:
In this study, we attempted to find the relations between blood pressure (BP) measured on the brachial artery (bBP) and BP assessed on the radial artery (rBP) in the right arm.
METHODS:
Three hundred and fifteen patients were enrolled in this study. Those who had peripheral vascular disease, wounds of arm skin or subcutaneous tissue infection were excluded. After a 15-minute equilibration and stabilization period after inducation of anesthesia, three bBP and rBP records were obtained sequentially using an oscillometric device with an adult cuff and infant cuff, respectively. Order for each BP was randomized.
RESULTS:
The bBP was significantly lower than the rBP (P<0.05). The difference between the two values varied from 13 to 18 mmHg in systolic BP (SBP), diastolic BP (DBP) and mean blood pressure (MAP) respectively. And the rBP was positively correlated with the bBP (r=0.872, 0.754, 0.765; P<0.001, <0.001, <0.001; SBP, DBP, MAP, respectively).
CONCLUSION:
The bBP value can be evaluated by the noninvasive measurements of rBP using an appropriate cuff in clinical practice.
KEY WORDS: Blood pressure, Brachial artery, Radial artery, Correlation, Linear regression
INTRODUCTION
Blood pressure (BP) is a vital sign indicating general health of critically ill patients and guiding their treatment. It is well known that the accurate method for monitoring BP is passing a transducer connected to a catheter directly into the ascending aorta. However, this technique is invasive and not suitable for all patients. In general, non-invasive blood pressure monitoring is commonly used in the clinic. Systemic blood pressure is usually estimated by conventional measurements of brachial artery blood pressure with a brachial cuff using oscillometric devices.
However, when patients have some difficulties in monitoring BP on the upper arm, such as the wound on the skin or infection of subcutaneous tissues of the upper arm, brachial blood pressure (bBP) is not suitable for measurement. Meanwhile, looking for another way to monitor BP will be necessary. Under this condition, we found that in many patients with intact forearms, the radial blood pressure (rBP) on the wrist is easy to be measured. Therefore, we investigated the relationship between bBP and rBP using appropriate cuffs and intended to find that whether rBP can substitute bBP clinically.
METHODS
This study was approved by the Institutional Ethics Committee at Drum-Tower Hospital. A total of 315 patients, 149 males and 166 females, aged 18–79 years, were enrolled in this study. They all provided the written informed consent.
Participants were excluded if they had upper limb amputation, cuts or bruising of the skin at measurement sites. In addition, those with hypertension, arrhythmia, aortic coarctation, aortic dissection, peripheral vascular disease, congenital heart disease, and vasculitis were all excluded.
Under the condition of general anesthesia, the right upper limbs of all patients (in a supine position) were exposed. The upper arm and forearm were kept at heart level. Appropriate-sized cuffs were chosen according to the circumferences measured at the midpoint of the upper arm and forearm. Then we placed the two cuff bladders over the arterial pulsation and wrapped the cuffs snugly around the patients’ upper arm and forearm with the cuff bladders encircling at least 80 % of circumferences, because too small a cuff size leads to false high BPs and too large leads to false low BPs.[1,2] After induction of anesthesia and a 15-minute stabilization period, BP was recorded sequentially on the upper arm and forearm using two automated oscillometric BP monitors (Datex-Ohmeda, Madison, WI, USA). Order for site to be measured was first decided randomly, measurement should be repeated twice at intervals of at least 1 minute, and the 2 readings were averaged. When the two readings at the same site differed by >4 mmHg, the recording was removed, and additional readings should be obtained.[3]
Statistical analysis
Data were presented as mean and standard deviations (mean±SD). Statistical analysis was performed using SPSS v.13 (SPSS, Inc. Chicago, IL, USA.). bBP and rBP were compared using paired t-test. The association between bBP and rBP was evaluated using the intraclass correlation coefficient. We used one-way analysis of variance (ANOVA) to compare BPs of each interval. A P value of <0.05 was considered statistically significant.
RESULTS
Mean BMI was 23.2±3.5 kg/m2 (range 18.5–30.7 kg/m2), mean circumference of arm and forearm was 25.3±2.8 cm (range 22–34 cm) and 16.3±1.4 cm (range 13–20 cm), respectively. An infant cuff (appropriate circumference 10–20 cm) was used to measure rBP. We used various sizes of adult cuffs to measure bBP (12 cm×22 cm, for arm circumference of 22 to 26 cm; 16 cm×30 cm, for arm circumference of 27 to 34 cm).
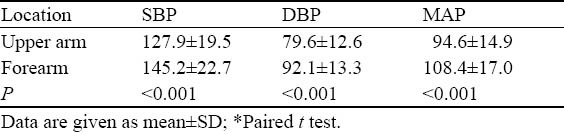
We obtained 1890 valid pressure readings from 315 patients. The mean BP value for each measurement of location is shown in Table 1. The mean SBP and DBP in the upper arm were both significantly higher than those in the forearm respectively (P<0.001).
Table 1.
BP values of the two measuring locations (mmHg)
Scatterplots of BP between the upper arm and forearm rSBP and bSBP were significantly correlated (r=0.872, P<0.001), and rDBP and bDBP were also significantly correlated (r=0.754, P<0.001) in addition to rMAP and bMAP (r=0.765, P<0.001) (Figure 1). Linear regression analysis showed a significant correlation between rBP and bBP.
Figure 1.
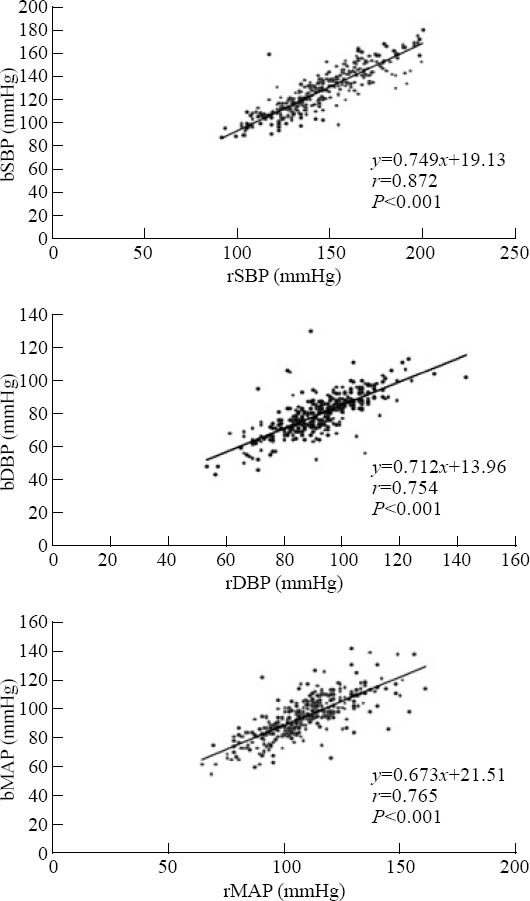
Scatterplots of rSBP, rDBP, and rMAP between rBP and bBP after general anesthesia. The x-axis indicates the mean of two readings of the bronchial artery; y-axis, the mean of BP values of the radial artery. Linear regression analysis showed a significant correlation between rBP and bBP.
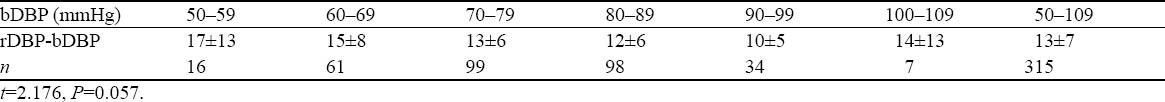
The absolute differences between rBP and bBP in SBP, DBP and MAP are shown in Tables 2–4. We divided bBP into several intervals for every 10 mmHg. There were no significant differences in absolute difference of rBP and bBP between the intervals (P=0.462, P=0.057, P=0.931). bBP could be obtained by subtracting 18, 13, 13 mmHg from rBP in SBP, DBP, and MAP, respectively.
Table 2.
Absolute differences of SBP between rBP and bBP in different intervals
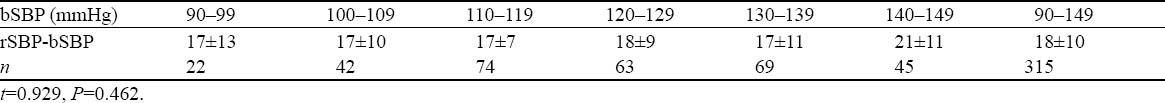
Table 4.
Absolute differences of MAP between rBP and bBP in different intervals
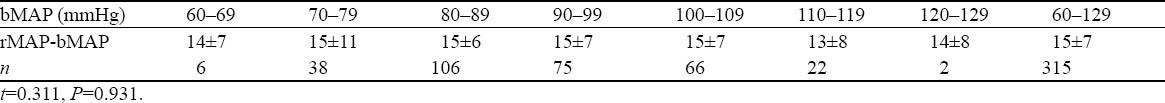
Table 3.
Absolute differences of DBP between rBP and bBP in different intervals
DISCUSSION
Usually, the BP of the brachial artery is measured using an oscillometric device with an appropriate cuff in a clinic. But in some patients, BP can’t be monitored on their upper arms because of the wound of skin or infection. Some studies[4,5] considered oscillometric devices for wrist measurement, but most studies have shown that these devices are inaccurate.[6–8] BPs at the wrist measured by oscillometric devices generally overestimate BP compared with conventional sphygmomanometry on the upper arm, and the differences could be substantial.[3] It was reported that systemic pressure increased as the measurement location was moved toward the periphery of the body away from the heart, whereas diastolic pressure was not different.[9] Nevertheless, our study showed that rDBP was much higher than bDBP. We thought this disparity might be due to the patients’ state. In Lee’s study,[9] the patients were measured before the induction of anesthesia, but our patients were measured during the maintainence of anesthesia.
Researchers[10,11] reported that there were marked differences between SBP of the radial artery and that of the brachial artery, and they were also correlated significantly with BMI. In our study, we found the differences between rBP and bBP, and also a strong linear relationship between them. Therefore, we can calculate bBP from the linear equation. Obviously, it is impractical to calculate bBP in the clinic. According to the absolute differences of BP values in the two sites, we could estimate dSBP, dDBP and dMAP by subtracting 18, 13, 13 mmHg from rSBP, rDBP, rMAP, respectively. And there was no significant difference between the calculated values and the measured values.
To avoid these influences of “white coat effect”, cold, tension, movement of arms, muscle fasciculation, blood pressure was measured in the maintenance of general anesthesia with room temperature at 24–26 °C during the experiment.[12,13] The position of the measured site could affect the values, i.e. the BP readings would be high if the arm was below the right atrium, whereas the readings would be low when the arm was above the heart level. These differences might be attributed to the effects of hydrostatic pressure and could be about 2 mmHg for every inch above or below the heart level.[2] Hence the midpoint of both upper arm and forearm was placed at the level of the heart in this study.[2,14]
From this study, we conclude that when BP value is difficult to be measured from the upper arm, it can be estimated by the measurement of the forearm as rBP using an appropriate cuff in clinical practice.
Footnotes
Funding: None.
Ethical approval: This study was approved by the Institutional Ethics Committee at Drum-Tower Hospital, Nanjing, China.
Conflicts of interest: The authors state that there is no conflict of interest invoving the study.
Contributors: All the authors contributed to the concept of the study, performance of the study, data collection, and writing of the manuscript.
REFERENCES
- 1.Amoore JN. Oscillometric sphygmomanometers: a critical appraisal of current technology. Blood Press Monit. 2012;17:80–88. doi: 10.1097/MBP.0b013e32835026b0. [DOI] [PubMed] [Google Scholar]
- 2.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals part. 1: blood pressure measurement in humans. A statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on high blood pressure research. Circulation. 2005;111:697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 3.O’Brien E, Pickering T, Asmar R, Myers M, Parati G, Staessen J, et al. Working group on blood pressure moiroring of the European society of hypertension international protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7:3–17. doi: 10.1097/00126097-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Zeng WF, Huang QF, Sheng CS, Li Y, Wang JG. Validation of the Kingyield BP210 wrist blood pressure monitor for home blood pressure monitoring according to the European Society of Hypertension International Protocol. Blood Press Monit. 2012;17:42–46. doi: 10.1097/MBP.0b013e32834f8301. [DOI] [PubMed] [Google Scholar]
- 5.Lu Y, Li CS, Wang S. Effect of hypertransfusion on the gastrointestinal tract after cardiac arrest in a porcine model. World J Emerg Med. 2012;3:49–54. doi: 10.5847/wjem.j.issn.1920-8642.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien E. Ambulatory blood pressure measurement is indispensable to good clinical practice. J Hypertens Suppl. 2003;21:S11–18. doi: 10.1097/00004872-200305002-00003. [DOI] [PubMed] [Google Scholar]
- 7.Akpolat T, Aydogdu T, Erdem E, Karatas A. Inaccuracy of home sphygmomanometers: a perspective from clinical practice. Blood Press Monit. 2011;16:168–171. doi: 10.1097/mbp.0b013e328348ca52. [DOI] [PubMed] [Google Scholar]
- 8.Latman NS, Latman A. Evaluation of instruments for noninvasive blood pressure monitoring of the wrist. Biomed Instrum Technol. 1997;31:63–68. [PubMed] [Google Scholar]
- 9.Lee JH, Kim JM, Ahn KR, Kim CS, Kang KS, Chung JH, et al. Study for the discrepancy of arterial blood pressure in accordance with method, age, body part of measurement during general anesthesia using sevoflurane. Korean J Anesthesiol. 2011;60:323–328. doi: 10.4097/kjae.2011.60.5.323. Epub 2011 May 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Hoeven NV, van den Born BJ, van Montfrans GA. Reliability of palpation of the radial artery compared with auscultation of the brachial artery in measuring SBP. J Hypertens. 2011;29:51–55. doi: 10.1097/HJH.0b013e32833e0ffa. [DOI] [PubMed] [Google Scholar]
- 11.Tomlinson LA, Wikinson IB. Does it matter where we measure blood pressure? Br J Clin Pharmacol. 2012;74:241–245. doi: 10.1111/j.1365-2125.2012.04203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dourmap C, Girerd X, Marquand A, Fourcade J, Hottelard C, Begasse F, et al. Systolic blood pressure is depending on the arm position when home blood pressure is measured with a wrist or an arm validated monitor. Blood Press Monit. 2010;14:181–183. doi: 10.1097/MBP.0b013e328337b4a2. [DOI] [PubMed] [Google Scholar]
- 13.O’Brien E, Waeber B, Parati G, Staessen G, Myers MG. On behalf of the European Society of Hypertension Working Group on Blood Pressure Monitoring. Blood pressure measuring devices: validated instruments. BMJ. 2001;322:531–536. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAlister FA, Straus SE. Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review. BMJ. 2001;322:908–911. doi: 10.1136/bmj.322.7291.908. [DOI] [PMC free article] [PubMed] [Google Scholar]


