Abstract
BACKGROUND:
Good neurological outcome after cardiac arrest (CA) is hard to achieve for clinicians. Experimental and clinical evidence suggests that therapeutic mild hypothermia is beneficial. This study aimed to assess the effectiveness and safety of therapeutic mild hypothermia in patients successfully resuscitated from CA using a meta-analysis.
METHODS:
We searched the MEDLINE (1966 to April 2012), OVID (1980 to April 2012), EMBASE (1980 to April 2012), Chinese bio-medical literature & retrieval system (CBM) (1978 to April 2012), Chinese medical current contents (CMCC) (1995 to April 2012), and Chinese medical academic conference (CMAC) (1994 to April 2012). Studies were included if 1) the study design was a randomized controlled trial (RCT); 2) the study population included patients successfully resuscitated from CA, and received either standard post-resuscitation care with normothermia or mild hypothermia; 3) the study provided data on good neurologic outcome and survival to hospital discharge. Relative risk (RR) and 95% confidence interval (CI) were used to pool the effect.
RESULTS:
The study included four RCTs with a total of 417 patients successfully resuscitated from CA. Compared to standard post-resuscitation care with normothermia, patients in the hypothermia group were more likely to have good neurologic outcome (RR=1.43, 95% CI 1.14–1.80, P=0.002) and were more likely to survive to hospital discharge (RR=1.32, 95% CI 1.08–1.63, P=0.008). There was no significant difference in adverse events between the normothermia and hypothermia groups (P>0.05), nor heterogeneity and publication bias.
CONCLUSION:
Therapeutic mild hypothermia improves neurologic outcome and survival in patients successfully resuscitated from CA.
KEY WORDS: Cardiac arrest, Cardiopulmonary resuscitation, Return of spontaneous circulation, Mild hypothermia, Meta-analysis
INTRODUCTION
The incidence of out-of-hospital cardiac arrest (CA) in industrial countries is reported to be 128/100 000 to 36/100 000 persons/year.[1] The incidence of sudden cardiac death in China is about 41.8/1000 000 persons and more than 544 000 persons die from CA each year.[2] Among the patients who received cardiopulmonary resuscitation (CPR), 13% to 59% achieved the return of spontaneous circulation (ROSC), but only 4.6% could be discharged from the hospital.[3] Therefore, therapy in the first hour after CA is very important.
Therapeutic mild hypothermia is still a relatively new concept for neuroprotection in patients who resuscitated after CA. Some experimental studies and clinical trials demonstrated that therapeutic mild hypothermia was beneficial.[4–7] So, the 2010 AHA guidelines for CPR and emergency cardiovascular care (ECC) recommend that comatose adult patients with ROSC after out-ofhospital ventricular fibrillation (VF) cardiac arrest should be cooled to be 32 °C to 34 °C for 12 to 24 hours.[8] In recent years, clinical trials on therapeutic mild hypothermia in patients after CPR have emerged and therefore systematic updates of the literature are necessary to know new and effective developments. This meta-analysis aimed to assess the effectiveness and safety of therapeutic mild hypothermia in patients successfully resuscitated from CA.
DATA SOURCES
We searched the following databases. English language databases included MEDLINE (PubMed) (1966 to April 2012), OVID (1980 to April 2012) and EMBASE (1980 to April 2012). Chinese language databases included Chinese bio-medical literature & retrieval system (CBM) (1978 to April 2012), Chinese medical current contents (CMCC) (1995 to April 2012), and Chinese medical academic conference (CMAC) (1994 to April 2012). Keywords “cardiac arrest OR cardiopulmonary resuscitation AND hypothermia” were used to search articles limiting the search by human and age more than 19 years. References of all searched articles were reviewed to avoid omitting other relevant articles. All randomized controlled trials (RCTs) were included. The following criteria were used to identify the articles: 1) the study design was a RCT; 2) the study population included adult patients who suffered from CA and were successfully resuscitated; 3) the normothermia group received the standard treatment after CPR and was not cooled. The hypothermia group received therapeutic mild hypothermia (the target core temperature 32 °C to 34 °C) in addition to the standard treatment, regardless of how body temperature was reduced; 4) the study provided data on neurological recovery (cerebral performance categories one or two) and survival to hospital discharge. Exclusion criteria were age less than 18 years and CA patients who received other combined therapy except for hypothermia.
The methodological quality of included studies was assessed by Jadad score scales (0=worst, 5=best).[9] Jadad score scales evaluate all included trials quality from the adequacy of randomization, blinding and follow-up. Low quality studies have a score of ≤2 and high quality studies a score of ≥3. Statistical analysis was performed using RevMan 5.0 software. The relative risk and 95% confidence interval were calculated for all included studies on an intention-to-treat basis. Values of P below 0.05 were considered significant. Heterogeneity among the individual outcomes was assessed by the chi-square test. Values of I2 >50% and P<0.1 indicated significant heterogeneity. When there was no heterogeneity among the individual studies, pooled effect estimates were assessed using a fixed-effects model. A funnel plot was used to examine publication bias. An asymmetric funnel plot indicated publication bias.
RESULTS
A total of 1 836 studies were retrieved by the initial searches. Of these studies, 1 718 studies were excluded because of relevance to historical controlled trial, case report, editorial, review and so on. Next, 113 studies were excluded because of irrelevance to comparison of therapeutic mild hypothermia and normothermia. One trial was further excluded as therapy involved hemofiltration plus hypothermia. Finally, four RCTs were included for meta-analysis (Figure 1).
Figure 1.
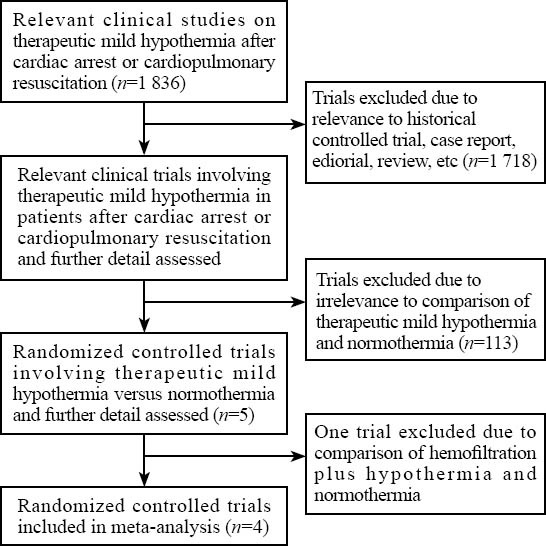
Flow diagram about the trials screened for meta-analysis.
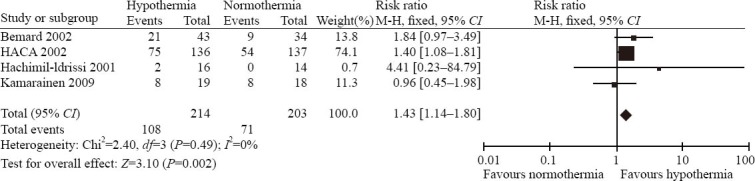
Four RCTs with a total of 417 patients successfully resuscitated from CA were included in this review. All the trials compared the effects of therapeutic mild hypothermia versus normothermia on outcomes in CA patients who were successfully resuscitated. Neurological recovery and survival to hospital discharge were the primary outcome in all the RCTs (Table 1). Jadad score was 5 for two RCTs, 4 for one RCT and 2 for one RCT among all four RCTs (Table 2).
Table 1.
Randomised controlled trials on mild hypothermia in the treatment of patients successfully resuscitated from cardiac arrest
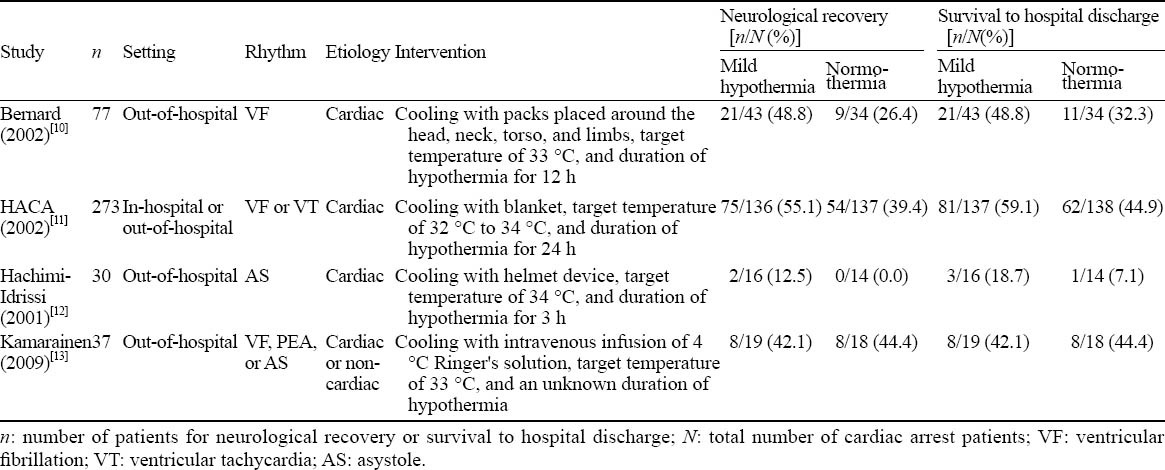
Table 2.
Jadad scores from all four randomized controlled trials
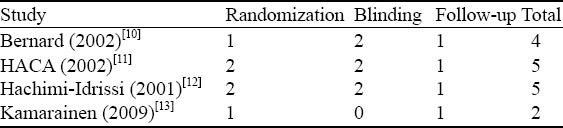
There was no heterogeneity from the outcome of neurological recovery in all the trials and a fixed-effects model was used to analyze. Meta-analysis demonstrated that the hypothermia group had better neurological oucome than the normothermia group (RR=1.43, 95% CI 1.14–1.80) (Figure 2). Similarly, there was no heterogeneity from the outcome of survival to hospital discharge and meta-analysis indicated that therapeutic mild hypothermia had an improvement in survival to hospital discharge compared with normothermia (RR=1.32, 95% CI 1.08–1.63) (Figure 3). The following adverse events were repor ted in al l four RCTs: pneumonia, pulmonary edema, bleeding, need for platelet transfusions, sepsis, arrhythmia, recurrence of CA, renal failure or oliguria, hemodialysis, pancreatitis, and seizures. However, there was no significant difference in reported adverse events beween hypothermia and normothermia (Table 3). A visual inspection of the funnel plot for neurological recovery and survival to hospital discharge showed that there was no publication bias (Figure 4).
Figure 2.
The effects of therapeutic mild hypothermia on neurological outcome after cardiac arrest.
Figure 3.
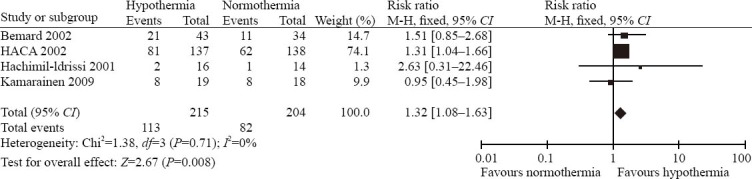
The effects of therapeutic mild hypothermia on surival to hospital discharge after cardiac arrest.
Table 3.
Adverse events associated with therapeutic mild hypothermia
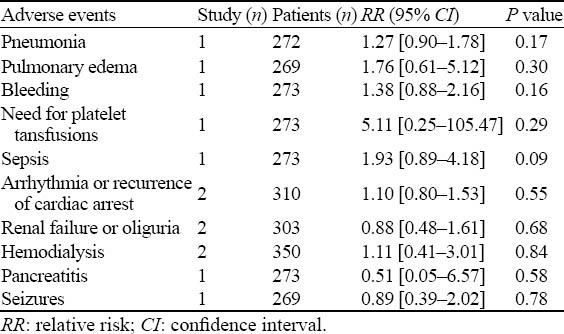
Figure 4.
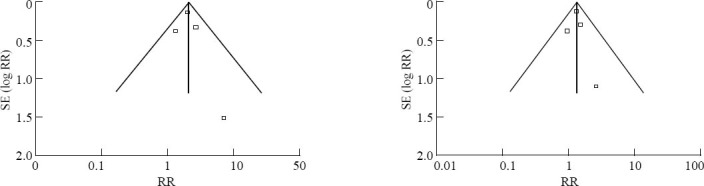
Funnel plot compares log relative risk (RR) versus the standard error of log RR for neurological outcome and survival to hospital discharge.
DISCUSSION
Across all the trials, a total of 417 patients who were successfully resuscitated from CA were included.[10–13] Meta-analysis demonstrated that therapeutic mild hypothermia improved neurological function and survival to hospital discharge compared with normothermia. Some clinical trials in China also showed that therapeutic mild hypothermia improved neurological function and long-term prognosis in patients successfully resuscitated from CA.[14,15] However, there was a shortage of high quality RCTs. At present, there is an argument on start of therapeutic mild hypothermia and duration of hypothermia. Bernard et al[7] found that early initiation of rapid cooling, preferably in the field soon after ROSC, could gain maximum benefits in both neurological outcome and survival. Another two interesting studies demonstrated that therapeutic mild hypothermia could improve neurological outcome and survival in patients after out-of-hospital VF although start of cooling was delayed for 4 to 8 hours.[10,11] Similarly, it is very important for the duration of hypothermia. When the duration of cooling is too short, hypothermia could not significantly improve neurological outcome. On the contrary, long-term hypothermia might cause obvious adverse effects. The duration of mild hypothermia in all the trials except one was 3, 12, and 24 hours, respectively. The pooled results showed that therapeutic mild hypothermia significantly improved neurological outcome and survival after CPR, but did not significantly increase the incidence of adverse events. Jadad scores of ≥3 among all four trials had three studies and Jadad scores of <3 had one study, indicating that three-fourths studies were of high quality. What’s more, there was no heterogeneity and publication bias in all the trials. Therefore, the conclusion is more reliable and further supports the guidelines which recommend that mild hypothermia is applied in CA patients.
Therapeutic mild hypothermia protects brain against damage in multiple ways. The possible mechanisms of therapeutic hypothermia for neuroprotection include: 1) Therapeutic hypothermia can inhibit the biosynthesis, release and uptake of several catecholamines and neurotransmitters especially glutamate and dopamine leading to brain damage;[16–21] 2) It can preserve the blood brain barrier and adenosine triphosphate stores, restitute cerebral microcirculation after ischemia, decrease intracranial pressure and increase cerebral brain blood flow;[22–25] 3) It also can reduce the amount of cell death in certain brain regions.[26–30] Although therapeutic mild hypothermia benefits CA patients, adverse events caused by mild hypothermia should not be neglected. Adverse events reported in all trials included pneumonia, pulmonary edema, bleeding, need for platelet transfusions, sepsis, arrhythmia, recurrence of CA, renal failure or oliguria, hemodialysis, pancreatitis, and seizures. But there was no significant difference in adverse events between hypothermia and normothermia. Hence therapeutic mild hypothermia is safe and beneficial for CA patients and should be largely popularized in clinical practice especially in China in future.
However, the study also suffers from several limitations including clinical and methodological heterogeneity, and less trials and cases. Different patient populations including etiology, setting and first recorded cardiac rhythm are included in four RCTs. Time from start of cooling to target temperature is largely different. At last, the target temperature and duration of hypothermia are different. Therefore, high quality studies and adequate cases should be required to further evaluate the effect of therapeutic mild hypothermia on subgroup such as non-defibrillation rhythm, in-hospital CA, etc. Another potential limitation of this meta-analysis is that the number of trial and the study size may have been inadequate. We predicted that the survival rate of hospital discharge in the normothermia group was 30%. For a power of 0.80 (α=0.05), assuming an improvement of 10% in survival rate of hospital discharge with mild hypothermia, 354 patients in each group would be required to detect the difference, and thus the study was underpowered.
In conclusion, based on the findings of four RCTs, therapeutic mild hypothermia improved neurological function and survival to hospital discharge in patients who were successfully resuscitated from CA. There was no significant difference in reported adverse events between hypothermia and normothermia. Therefore, therapeutic mild hypothermia is safe and beneficial for CA patients.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors state that there is no conflict of interest involving the study.
Contributors: Wang XP and Lin QM proposed the study and wrote the manuscript. All the authors read and approved the final version of the manuscript. Lin QM is the guarantor.
REFERENCES
- 1.Smith TW, Cain ME. Sudden cardiac death: epidemiologic and financial worldwide perspective. J Interv Card Electrophysiol. 2006;17:199–203. doi: 10.1007/s10840-006-9069-6. [DOI] [PubMed] [Google Scholar]
- 2.Sun RC, Yang SD, Zhou ZY, Liang JB. Clinicopathological analysis of sudden cardiac death cases by autopsy. Zhonghua Yi Xue Za Zhi. 2012;92:2707–2709. [PubMed] [Google Scholar]
- 3.Boyd TS, Perina DG. Out-of-hospital cardiac arrest. Emerg Med Clin North Am. 2012;30:13–23. doi: 10.1016/j.emc.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Cho JH, Ristagno G, Li Y, Sun SJ, Weil MH, Tang W. Early selective trans-nasal cooling during CPR improves success of resuscitation in a porcine model of prolonged pulseless electrical activity cardiac arrest. Resuscitation. 2011;82:1071–1075. doi: 10.1016/j.resuscitation.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Wu X, Li Z, Chen W, Wu X, Li Z, et al. Comparison of the durations of mild therapeutic hypothermia on outcome after cardiopulmonary resuscitation in the rat. Circulation. 2012;125:123–129. doi: 10.1161/CIRCULATIONAHA.111.062257. [DOI] [PubMed] [Google Scholar]
- 6.Cai XF, Sun JM, Bao LS, Li WB. Distribution and antibiotic resistance of pathogens isolated from ventilator-associated pneumonia patients in pediatric intensive care unit. World J Emerg Med. 2011;2:117–121. doi: 10.5847/wjem.j.1920-8642.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernard S, Buist M, Monteiro O, Smith K. Induced hypothermia using large volume, ice-cold intravenous fluid in comatose survivors of out-of-hospital cardiac arrest: a preliminary report. Resuscitation. 2003;56:9–13. doi: 10.1016/s0300-9572(02)00276-9. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part. 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 9.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 10.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 11.Kulstad EB, Courtney DM, Waller D. Induction of therapeutic hypothermia via the esophagus: a proof of concept study. World J Emerg Med. 2012;3:118–122. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hachimi-Idrissi S, Corne L, Ebinger G, Michotte Y, Huyghens L. Mild hypothermia induced by a helmet device: a clinical feasibility study. Resuscitation. 2001;51:275–281. doi: 10.1016/s0300-9572(01)00412-9. [DOI] [PubMed] [Google Scholar]
- 13.Kamarainen A, Virkkunen I, Tenhunen J, Yli-Hankala A, Silfvast T. Prehospital therapeutic hypothermia for comatose survivors of cardiac arrest: a randomized controlled trial. Acta Anaesthesiol Scand. 2009;53:900–907. doi: 10.1111/j.1399-6576.2009.02015.x. [DOI] [PubMed] [Google Scholar]
- 14.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 15.Pechman V, Rokyta R, Jr, Gajdos P, Pesek J. Treatment and outcome of patients after cardiopulmonary resuscitation admitted to the intensive cardiac care unit. Neuro Endocrinol Lett. 2009;30:363–367. [PubMed] [Google Scholar]
- 16.Boels PJ, Verbeuren TJ, Vanhoutte PM. Moderate cooling depresses the accumulation and the release of newly synthesized catecholamines in isolated canine saphenous veins. Experientia. 1985;41:1374–1377. doi: 10.1007/BF01949995. [DOI] [PubMed] [Google Scholar]
- 17.Okuda C, Saito A, Miyazaki M, Kuriyama K. Alteration of the turnover of dopamine and 5-hydroxytryptamine in rat brain associated with hypothermia. Pharmacol Biochem Behav. 1986;24:79–83. doi: 10.1016/0091-3057(86)90048-1. [DOI] [PubMed] [Google Scholar]
- 18.Choi DW, Maulucci Gedde M, Kriegstein AR. Glutamate neurotoxicity in cortical cell culture. J Neurosci. 1987;7:357–368. doi: 10.1523/JNEUROSCI.07-02-00357.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hachimi-Idrissi S, Van Hemelrijck A, Michotte A, Smolders I, Sarre S, Ebinger G, et al. Postischemic mild hypothermia reduces neurotransmitter release and astroglial cell proliferation during reperfusion after asphyxial cardiac arrest in rats. Brain Res. 2004;1019:217–225. doi: 10.1016/j.brainres.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Wang D, Zhao Y, Zhang Y, Zhang T, Shang X, Wang J, et al. Hypothermia protects against oxygen-glucose deprivation-induced neuronal injury by down-regulating the reverse transport of glutamate by astrocytes as mediated by neurons. Neuroscience. 2013;237:130–138. doi: 10.1016/j.neuroscience.2013.01.056. [DOI] [PubMed] [Google Scholar]
- 21.Takata K, Takeda Y, Sato T, Nakatsuka H, Yokoyama M, Morita K. Effects of hypothermia for a short period on histologic outcome and extracellular glutamate concentration during and after cardiac arrest in rats. Crit Care Med. 2005;33:1340–1345. doi: 10.1097/01.ccm.0000166351.19369.d3. [DOI] [PubMed] [Google Scholar]
- 22.Globus MY, Ginsberg MD, Harik SI, Busto R, Dietrich WD. Role of dopamine in ischemic striatal injury: metabolic evidence. Neurology. 1987;37:1712–1719. doi: 10.1212/wnl.37.11.1712. [DOI] [PubMed] [Google Scholar]
- 23.Karibe H, Zarow GJ, Graham SH, Weinstein PR. Mild intraischemic hypothermia reduces postischemic hyperperfusion, delayed postischemic hypoperfusion, blood-brain barrier disruption, brain edema, and neuronal damage volume after temporary focal cerebral ischemia in rats. J Cereb Blood Flow Metab. 1994;14:620–627. doi: 10.1038/jcbfm.1994.77. [DOI] [PubMed] [Google Scholar]
- 24.Mizuhara A. The protective effect of hypothermia in a new transient cerebral ischemic model of the rat—A 31P magnetic resonance spectroscopy in vivo study. Nihon Kyobu Geka Gakkai Zasshi. 1996;44:1–8. [PubMed] [Google Scholar]
- 25.Takasu A, Yagi K, Okada Y. Effect of mild hypothermia on ischemia-induced release of endothelin-1 in dog brain. Resuscitation. 1996;31:59–64. doi: 10.1016/0300-9572(95)00907-8. [DOI] [PubMed] [Google Scholar]
- 26.Marion DW, Penrod LE, Kelsey SF, Obrist WD, Kochanek PM, Palmer AM, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997;336:540–546. doi: 10.1056/NEJM199702203360803. [DOI] [PubMed] [Google Scholar]
- 27.Gong P, Hua R, Zhang Y, Zhao H, Tang Z, Mei X, et al. Hypothermia-induced neuroprotection is associated with reduced mitochondrial membrane permeability in a swine model of cardiac arrest. J Cereb Blood Flow Metab. 2013;33:928–934. doi: 10.1038/jcbfm.2013.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S, Wang S, Li C. Infusion of 4 °C normal saline can improve the neurological outcome in a porcine model of cardiac arrest. J Trauma Acute Care Surg. 2012;72:1213–1219. doi: 10.1097/TA.0b013e318246ed36. [DOI] [PubMed] [Google Scholar]
- 29.Weng Y, Sun S. Therapeutic hypothermia after cardiac arrest in adults: mechanism of neuroprotection, phases of hypothermia, and methods of cooling. Crit Care Clin. 2012;28:231–243. doi: 10.1016/j.ccc.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 30.Kim JY, Kim N, Yenari MA, Chang W. Mild hypothermia suppresses calcium-sensing receptor (CaSR) induction following forebrain ischemia while increasing GABA-B receptor 1 (GABA-B-R1) expression. Transl Stroke Res. 2011;2:195–201. doi: 10.1007/s12975-011-0082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


