Abstract
Objective
The study examines differences in the prevalence and nature of co-rumination during real-world social interactions with peers and parents among adolescents with major depressive disorder (MDD) compared to healthy controls.
Method
Sixty youth (29 with current MDD and 31 no-psychopathology controls) completed a self-report measure of co-rumination and a three-week ecological momentary assessment (EMA) protocol that measured the nature of face-to-face social interactions with peers and parents following a negative event in the adolescents’ daily lives. Specifically, EMA was used to assess rates of problem talk, including both co-rumination and co-problem-solving. Group differences in self-report and EMA measures were examined.
Results
Adolescents with MDD reported co-ruminating more often than adolescents with no Axis 1 disorders during daily interactions with both parents (Cohen’s d = .78) and peers (d = 1.14), and also reported more co-rumination via questionnaire (d = .58). Adolescents with MDD engaged in co-problem-solving with peers less often than healthy controls (d = .78), but no group differences were found for rates of co-problem-solving with parents.
Conclusions
Results are consistent with previous research linking co-rumination and depression in adolescence and extend these self-report--based findings to assessment in an ecologically valid context. Importantly, results support that MDD youth tend to co-ruminate more and problem-solve less with peers in their daily lives compared to healthy youth, and that co-rumination also extends to parental relationships. Interventions focused on decreasing co-rumination with peers and parents and improving problem-solving skills with peers may be helpful for preventing and treating adolescent depression.
Keywords: Co-rumination, depression, problem-solving, adolescence, ecological momentary assessment
Introduction
Talking about a problem or distressing experience with others is a common, everyday human experience, often motivated by our need for help solving a problem or regulating negative emotion. Engaging others to assist with emotion regulation begins during infancy1–3 and continues into adulthood.2 As adolescents grow more independent from parents and rely increasingly on peers such as friends and romantic partners for provision of social affiliative needs,4,5 it becomes particularly important that they select social partners who are skilled in assisting with this interpersonal process of emotional regulation.
Difficulty obtaining the socio-emotional benefits of interpersonal relationships is commonly associated with depression. For example, dysfunctional interpersonal behaviors associated with depression, such as negative feedback-seeking,6 excessive reassurance seeking,7 or social withdrawal,8 are believed to maintain depressive symptoms by interfering with normative social exchange.6–9 Importantly, dysregulation of emotion is considered to be one of the hallmarks of depression during adolescence,10 with theorists emphasizing the role of social dysfunction in emotional dysregulation.11–13
A breakdown in the effectiveness of discussing problems with others has been cited as a possible risk of depression among youth.14,15 Co-rumination refers to a pattern of interpersonal behavior characterized by “frequently discussing problems, discussing the same problem repeatedly, mutual encouragement of discussing problems, speculating about problems, and focusing on negative feelings.”14(p1830) Although co-rumination appears to be socially functional, with youth who engage in co-rumination with peers reporting higher friendship quality,15 it is associated concurrently14,16 and prospectively15,17 with higher rates of depressive symptoms among children and adolescents.
These findings are consistent with evidence that involuntary engagement strategies for regulating affect, such as rumination, are less effective than more active strategies for regulating negative affect, such as problem-solving, in adolescents.18,19 Social partners who are engaged in co-rumination actively encourage each other to ruminate about a distressing event or emotion.14 By fostering rumination, co-rumination is unlikely to improve mood. In contrast, by supporting a more productive form of coping, social partners who facilitate problem-solving may be more effective than co-ruminators in assisting with emotion regulation. This may be particularly true when discussing more controllable events (i.e., in situations that could actually be improved by problem-solving).18
Because adolescence is a key development period for the shift from a primary focus on social interaction with parents to an increasing focus on peer relations,4,5 it is important to assess how adolescents discuss problems with both parents and peers. Youth whose interactions with peers are characterized by levels of problem-solving similar to levels observed during interactions with parents may be more successful in obtaining positive, rewarding experiences – including help coping with negative experiences -- from peer relations, thus indicating they are making a smoother transition away from a central reliance on parents. On the other hand, youth who frequently co-ruminate and rarely problem-solve with peers may be less successful in negotiating the socio-emotional transitions of adolescence and may be at greater risk for emotional difficulties.
Most studies of co-rumination have involved community samples.14–17 However, two studies to date examined co-rumination in relation to DSM-IV major depressive disorder (MDD). In the first,20 adolescents who reported more co-rumination at baseline were more likely to experience a major depressive episode (MDE) within two years; among those who became depressed, greater co-rumination predicted longer, more severe MDEs. A second study21 found that co-rumination was linked to a past history of MDD. The present study is the first to examine the prevalence of co-rumination among adolescents currently meeting DSM-IV criteria for MDD.
This existing research on co-rumination in adolescence has relied primarily on self-report questionnaires, which may be limited by retrospective reporting biases and do not capture subtle differences in the content of peer discussion about problems. The current study introduces an ecological momentary assessment (EMA) approach to assessing co-rumination in daily life. By assessing participants’ social and emotional functioning during daily social interactions over several weeks, EMA provides a more ecologically valid measurement of adolescents’ actual day-to-day experiences than global self-report measures. Although EMA has been used to study affective and social functioning among adolescents with depression,22,23 this is the first application of EMA to examine co-rumination or co-problem-solving in this population. EMA permits a fine-grained examination of daily social interactions, allowing us to examine how often youth talk about problems with others and how often this problem talk involves co-rumination.
This study also extends previous work by examining the prevalence of productive interpersonal interactions, such as problem-solving with others, in addition to dysfunctional interpersonal behavior, such as co-rumination. An important element of co-rumination is the tendency to engage in co-rumination to the exclusion of other forms of social interaction.14 Thus, it seems reasonable to expect that individuals who engage in co-rumination may also be less likely to engage in co-problem-solving (i.e., problem-solving with others).
Although most studies of co-rumination to date have focused on examining co-rumination in interactions between friends,14,15 there is a burgeoning interest in co-rumination within other close relationships. For example, co-rumination between mothers and adolescents has recently been linked to depressive symptoms in community samples.24,25 In the current study, we used EMA methods to examine co-rumination and co-problem-solving during face-to-face social interactions with both peers and parents.
The purpose of the present study was to examine the prevalence of co-rumination (using both questionnaire and EMA measures) among youth currently meeting DSM-IV criteria for MDD, relative to controls with no lifetime history of psychopathology. Specifically, our first goal was to examine whether youth with MDD differ from controls on co-rumination measured via a widely utilized self-report measure, the Co-Rumination Questionnaire (CRQ).14 Our second and primary goal was to examine differences between youth with MDD and healthy controls in the nature of real-world face-to-face discussions with parents and peers about negative events (i.e., ‘problem talk’). We used EMA to compare rates of problem talk with parents and peers that included (a) co-rumination (i.e. adolescent-reported ruminating during a face-to-face discussion about a negative event with a parent or peer) and (b) co-problem-solving (i.e. adolescent-reported problem-solving during a face-to-face discussion about a negative event with a parent or peer). We expected that youth with MDD would engage in problem talk more frequently than healthy controls. We also expected that rates of co-rumination with parents and peers in daily life would be higher among youth with MDD than controls. Conversely, we hypothesized that rates of co-problem-solving with parents and peers in daily life would be lower among youth with MDD than healthy controls. Our final goal was to examine the degree of concordance between the questionnaire and EMA measures of co-rumination with peers. We expected that scores on the CRQ would be positively associated with two EMA variables: 1) overall frequency of problem talk; and 2) frequency of co-rumination.
Method
Participants
Participants were 60 youth ages 11–17 years (M = 14.47; SD = 1.79) who participated in a study of pediatric major depressive disorder. Twenty-nine youth were in a major depressive episode at the onset of the study. Controls (n = 31) had no lifetime history of psychopathology and were matched to participants with MDD by age and gender. Because some youth with depressive symptoms originally recruited for the study did not meet final criteria for inclusion, the final sample contained three more controls than participants with MDD. Thus, the groups are not identical with regard to age and gender. However, groups do not differ significantly on these characteristics. Demographic characteristics are summarized in Table 1. Consistent with gender differences in the prevalence of MDD in adolescence,26,27 there were more females (71.7%) than males in the study sample. The sample was European American (70%), African-American (26.7%), and Asian American (3.3%); control and MDD groups did not differ significantly with regard to race. However, educational attainment was higher among mothers of control participants than mothers of adolescents with MDD.
Table 1.
Demographic Characteristics, Depression Treatment, and Depressive Symptom Severity
| Healthy Controls n = 31 |
Youth with MDD n = 29 |
|t| or χ2 | p | |
|---|---|---|---|---|
| Age (years), mean (SD) | 14.52(1.82) | 14.41(1.78) | .220 | .827 |
| Sex (% male) | 32.3 | 24.1 | .487 | .485 |
| Race (%) | 1.792 | .408 | ||
| European American | 77.4 | 62.1 | ||
| African American | 19.4 | 34.5 | ||
| Asian American | 3.2 | 3.4 | ||
| Maternal education (%) | 6.866 | .032 | ||
| High school graduate | 0.0 | 20.8 | ||
| Some college | 46.4 | 29.2 | ||
| Degree from 4-year college or more | 53.6 | 50.0 | ||
| Currently taking SSRI (%) | 0.0 | 6.90 | 2.21 | .137 |
| Mood and Feelings Questionnaire – Child, mean (SD) | 4.90(6.46) | 34.89(14.98) | 9.78 | <.00001 |
Note: Maternal education data were missing for 8 participants. Mood and Feelings Questionnaire scores were unavailable for one participant in the control group and one participant with major depressive disorder (MDD). SSRI = selective serotonin reuptake inhibitor.
Youth with MDD
On average, youth with MDD reported levels of depressive symptoms on the Mood and Feelings Questionnaire (MFQ)28,29 (M = 34.89, SD = 14.98) that were consistent with other samples of adolescents with MDD.30,31 Additionally, 75% of youth with MDD reported MFQ scores above the clinical cutoff of 27 employed in other studies.31,32 Twenty youth (69%) had a history of outpatient mental health treatment (range: 3 weeks to 13 years); of these, three had also received inpatient treatment. At the outset of the study, 11 youth were participating in outpatient psychotherapy in the community; of those, two were taking selective serotonin reuptake inhibitors (SSRIs). Regarding comorbidity, 11 (37.9%) youth had one or more anxiety disorders including generalized anxiety disorder (GAD; n = 9); specific phobia (n = 4); social phobia (n = 2); separation anxiety disorder (SAD; n = 1); and panic disorder with (n = 1) and without (n = 1) agoraphobia; two participants had oppositional defiant disorder (ODD), and one had Enuresis.
Inclusion criteria
Participants in the MDD group met DSM-IV33 diagnostic criteria for current MDD, diagnosed by structured clinical interview using the Schedule for Affective Disorders and Schizophrenia in School-Age Children—Present and Lifetime version (K-SADS-PL).34 While the K-SADS-PL queries about any lifetime history of depressive symptoms, diagnoses of current MDD were made if youth met DSM-IV criteria for MDD based on symptoms experienced during the two weeks prior to the interview. Controls were eligible for the study if they had no lifetime history of any Axis I disorder with the exception of Enuresis, which was permitted.
Exclusion criteria
Because the original study also involved biological measures such as functional magnetic resonance imaging (fMRI) and pupillometry, which occurred after participants completed EMA, adolescents were excluded if they had significant motor impairments, history of head injury, neurological disorders, visual impairments (uncorrected vision < 20/40), or had metal objects in their body. Also excluded were adolescents currently taking psychotropic medications other than SSRIs or stimulants and those who were acutely suicidal. Two adolescents with MDD were taking SSRIs during the study, and none were taking stimulants. Participants in the MDD group were excluded from the study if they had ever met DSM-IV criteria for a developmental disorder (e.g., autism spectrum disorder(ASD), mental retardation [IQ < 70]), schizophrenia, schizoaffective disorder, psychotic depression, or bipolar disorder (BD), or currently met criteria for posttraumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), conduct disorder (CD), substance abuse or dependence, or attention-deficit/hyperactivity disorder (ADHD: predominantly hyperactive-impulsive type or combined type).
Procedure
This study was approved by the University of Pittsburgh’s Institutional Review Board. Youth with MDD were recruited from multiple sources (i.e., mental health treatment clinics, other research studies, and community advertisements), while control participants were recruited via community advertisements. After participants’ parents provided informed consent and participants provided either consent or assent, depending on their age, participants completed a phone screen and a two-hour study visit. During the study visit, adolescents and their parent(s) completed structured clinical interviews to assess current and lifetime history of DSM-IV33 disorders and completed questionnaire measures. All adolescents then completed an EMA protocol designed to assess emotional and social functioning in adolescents’ daily lives over the course of the following three weeks. Although the study did not include a treatment component, study staff provided information about treatment options in the university and local community to all participants with MDD.
Measures
Structured diagnostic interviews
The K-SADS-PL34 was used to assess current and lifetime psychopathology. Parents and youth were interviewed separately, and results were synthesized by the clinician who had conducted the interviews. Fifteen percent of interviews were double-coded to assess reliability; for diagnoses of current and lifetime MDD, interrater agreement between two raters was 100%.
Self-reports
Youth completed the 27-item CRQ.14 The CRQ was designed to assess the degree to which individuals engage in co-rumination within friendships. Items were designed to assess an extreme form of self-disclosure that exclusively focuses on negative events or problems. For example, “If one of us has a problem, we will spend our time together talking about it, no matter what else we could do instead.” Youth indicate the degree to which each item applies to them (1 = Not at all true; 5 = Really true). The mean of all 27 items is used as a measure of co-rumination. In the current study, CRQ scores were available for 57 participants (30 controls; 27 with MDD). Internal reliability was high (α = .96).
EMA
All participants completed an EMA protocol that assessed social behavior and emotional functioning in a naturalistic setting using a method similar to previous EMA studies with adolescents.18,22,23 For three consecutive weeks, adolescents received phone calls from research staff who were blind to participants’ MDD diagnostic status over a five-day block (i.e., from 4 PM on Thursday to 10 PM on Monday). Each block of 14 calls included three weekdays and two weekend days. In all, 42 calls were made to each participant. On weekdays, calls were made in the afternoon and evening to avoid interfering with school. No calls were made between 10 PM and 11 AM on any day. Fifty-nine participants completed at least 50% of calls and were included in EMA analyses. The final sample for EMA analyses consisted of 30 controls and 29 youth with MDD. Completed calls (M = 35.32 calls or 84.1% of calls made) did not differ between youth with MDD (M = 35.24, SD = 4.75) and control groups (M= 35.40, SD = 4.45; t[57] = .133, p = .895).
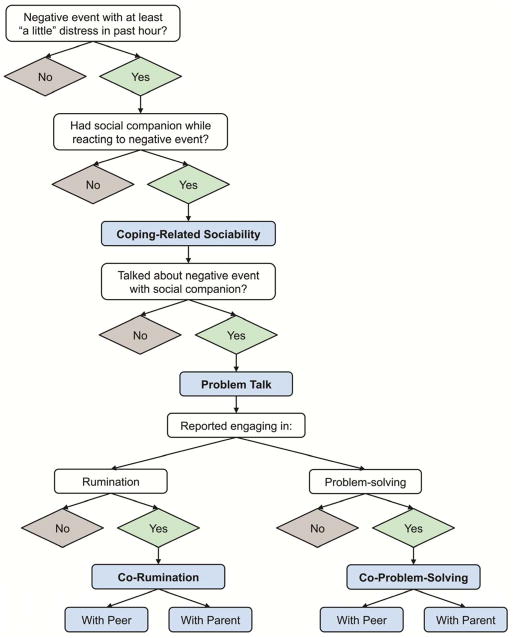
Each call consisted of a brief, structured interview that assessed behavior, social context, and emotional responding at three time points during the hour immediately preceding the call: (1) the time of the call, (2) when youth felt the worst or most negative, and (3) when youth felt the best or most positive.18 The present study focused on social context, social behavior, and coping strategies associated with the most negative event reported on each call. EMA variables, including both co-rumination and co- problem-solving, were calculated as shown in Figure 1. First, adolescents were asked to describe the most negative event that had occurred in the previous hour. Youth were asked to rate how negatively they felt about the event on a 1–5 scale along 5 dimensions (“angry”, “sad”, “nervous”, “upset”, or “bored”). To ensure that data included in analyses reflected at least mild negative events, only calls in which adolescents reported feeling at least “a little” distressed by the event on one of five negative affect ratings were included; mean number of emotional calls per participant were similar for adolescents with MDD (M = 28.21, SD = 9.42) and controls (M = 29.73, SD = 7.20; t[57]= .701, p = .486). Coping strategies were then assessed using a list of strategies from Silk and colleagues.18 Rumination was assessed via the item: “Were you unable to stop thinking about how you were feeling – thoughts about [most negative event] kept popping up into your mind?”18 Problem-solving was measured with the item: “Did you do something to fix the problem or think of a way to make things better?”18 Next, presence or absence of problem talk was assessed by asking two questions. First, youth were asked, “Was someone with you when you did those things/coping strategies?” If youth reported having a social companion, they were asked, “Did this person talk with you about the negative event?” The event was considered to include co-rumination in instances where the adolescent reported engaging in rumination while talking with a peer or parent about the event. The event was considered to include co-problem-solving when the adolescent reported engaging in problem-solving while talking with a peer or parent about the event.
Figure 1.
Derivation of ecological momentary assessment (EMA) measures of coping-related sociability, problem talk, co-rumination, and co-problem-solving from EMA items.
Proportion scores were calculated for each participant to indicate the proportion of calls involving each type of problem talk with each companion out of the total number of calls involving problem talk with that companion (i.e., co-rumination with peers = total number of calls in which a participant reported ruminating about a problem with a peer / total number of calls in which the participant talked to a peer about a problem). Scores were created separately for co-ruminating with parents, co-ruminating with peers, co-problem-solving with parents, and co-problem-solving with peers. To ensure that any group differences in EMA measures were not driven by differences in overall sociability or tendency to associate with others when coping with negative emotion, we also calculated a proportion variable to reflect coping-related sociability (i.e., proportion of calls in which participants reported having a social companion with them while coping with the negative event / total number of calls containing a negative event).
Results
Preliminary Analyses
Coping-related sociability
All participants reported having a social companion when coping with a negative event on at least one EMA call. Results from two-tailed independent samples t-tests indicated that youth with MDD and controls were similarly likely to report having a peer (t[57] = .385, p = .701) or parent (t[57] = .876, p = .385) as a social companion while coping with a negative event.
Self-Report Questionnaire Measure of Co-Rumination
On the CRQ, adolescents with MDD (M = 2.66, SD = .89) reported significantly higher levels of co-rumination than healthy controls (M = 2.17, SD = .80; t[55] = −2.170, p = .034, Cohen’s d = .58).
EMA Measures of General Problem Talk, Co-Rumination, and Co-Problem-Solving
Problem talk
Adolescents with MDD (M = .48, SD = .34) and healthy controls (M = .46, SD = .38) engaged in problem talk with peers (t[48] = .211, p = .834) at similar rates. For rates of problem talk with parents, youth with MDD (M = .55, SD = .32) also did not differ from controls (M = .46, SD = .39; t[49] = .878, p = .384).
Two subtypes of problem talk (i.e., co-rumination and co-problem-solving) were examined within the subsets of youth who discussed problems with peers or parents. We found that the subset of youth who discussed problems with peers consisted of the same 40 participants (22 controls; 18 with MDD) who discussed problems with parents.
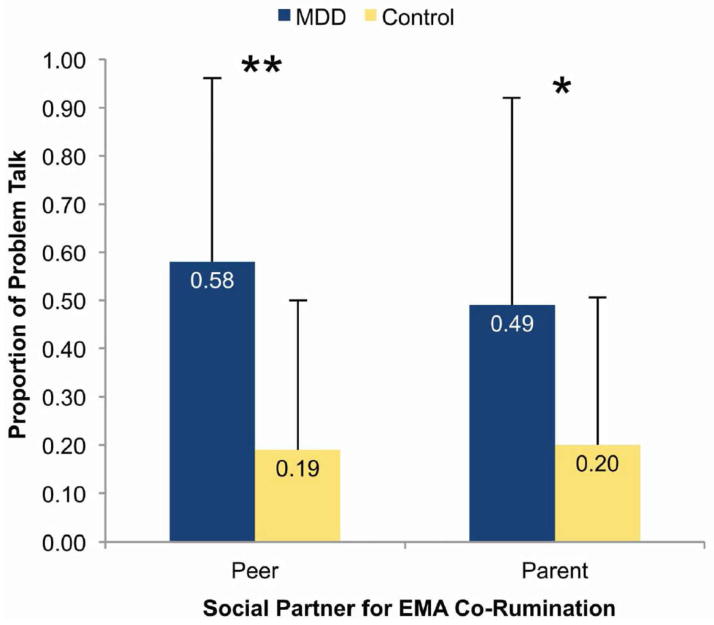
Co-rumination
As shown in Figure 2, youth with MDD reported engaging in co-rumination with peers nearly three times as often as controls (t[38] = −3.569, p = .001). Per Cohen’s35 guidelines, this was a large effect (d = 1.14). Among the same 40 youth, those with MDD engaged in co-rumination with parents more than twice as often as controls (t[29.73] = −2.405, p = .023). This difference was a moderate to large effect (d = .78).
Figure 2.
Group differences in rates of ecological momentary assessment (EMA) co-rumination with peers and parents. Note: *p < .05, **p < .01.
Co-problem-solving
As shown in Figure 3, co-problem-solving with peers was reported more than twice as often by controls than youth with MDD (t[36.64] = 2.351, p = .024). This difference was a moderate to large effect (d = .78). However, adolescents with MDD and healthy controls reported engaging in problem-solving with parents at similar rates (t[38] = −.214, p = .832).
Figure 3.
Group differences in rates of co-problem-solving with peers and parents. Note: *p < .05.
Associations Between Questionnaire and EMA Measures of Co-Rumination With Peers
CRQ scores were positively associated with EMA problem talk (r = .22, p = .07) and EMA co-rumination with peers (r = .22, p = .10), but these correlations did not reach statistical significance. Youth who reported higher levels of co-rumination on the CRQ engaged in significantly less co-problem-solving with peers (r = −.42, p = .010).
Discussion
The present study demonstrates that adolescents currently meeting DSM-IV criteria for MDD are more likely to co-ruminate with peers during real-time problem talk compared to healthy adolescents. This is the first study of which we are aware to document increased co-rumination in a sample of adolescents currently experiencing a depressive disorder and is consistent with other reports showing that self-reported co-rumination predicts future20 and past21 depressive episodes in community samples. Taken together, these studies suggest that co-rumination appears to be present before, during, and after a depressive episode in youth and therefore merits considerable attention as a potential target for depression prevention and intervention.
We found that adolescents with MDD reported higher levels of co-rumination on a questionnaire measure of co-rumination compared to healthy controls, consistent with research linking higher levels of self-reported co-rumination to depressive symptoms in community samples.14,15 This suggests that co-rumination research conducted in community samples is applicable to clinically significant depressive disorders in youth.
Although both the EMA and questionnaire measures revealed higher levels of co-rumination in youth with MDD, EMA analyses provide a more nuanced picture of the nature of problem talk in peer dyads. By using EMA, we were able to ask adolescents to indicate whether problem talk included problem-solving or ruminative content. This more fine-grained analysis indicated that although youth with MDD engaged in much higher rates of co-rumination with their peers, they engaged in much lower rates of problem-solving with peers. Thus, there appears to be an important distinction between ruminative and problem-solving forms of problem talk in peer dyads, and depression involves a specific alteration in ruminative problem talk as well as a concomitant deficit in co-problem-solving with peers. Because co-rumination and co-problem-solving may both be considered subtypes of emotion regulation, these findings suggest that adolescent MDD is characterized by a particular pattern of interpersonal emotion regulation deficits in relationships with peers.
The EMA approach also allowed us to examine co-rumination with other social interaction partners, such as parents. Results suggest that adolescents with MDD spend more time co-ruminating with their parents compared to healthy youth. This is consistent with prior work suggesting that co-rumination is not limited to the peer dyad.24,25 Interestingly, in our study, youth with MDD did not differ from controls in rates of co-problem-solving with parents. This suggests that parents may be more effective than peers at focusing adolescents with MDD on adaptive problem-solving when they are distressed. Future research using observational methods would be useful in further testing this possibility.
Additionally, group differences in rates of co-problem-solving with peers may reflect differences in adolescents’ choice of friends. Youth with MDD may select less healthy friends who are less equipped to co-problem-solve or who also have depression.36,37 Further, youth with depression may have fewer options when it comes to selecting friends because they tend to withdraw from friendships with peers who are not depressed38 or because they display aversive social behaviors that limit their ability to establish friendships6,7,39 Alternatively, research also supports that peers grow increasingly similar to each other with regard to depression over time.38,40,41 Thus, adolescents who co-ruminate may discourage friends’ co-problem-solving attempts over time. Taken together, the increasing importance of peers for meeting adolescents’ affiliative and emotional needs emphasizes the need to target the development of healthy friendship (including lack of co-problem solving) in depression interventions.
The CRQ and EMA measures of co-rumination were modestly correlated in the hypothesized direction but did not reach statistical significance. CRQ co-rumination was inversely associated with EMA-assessed co-problem-solving with peers; youth who reported more co-rumination on the questionnaire engaged in less co-problem-solving in daily interactions with peers. Multiple explanations for these findings are possible. First, we may have been unable to detect a significant correlation between CRQ and EMA measures of co-rumination due to the relatively small sample size. It is also possible that the EMA and questionnaire measures tap into different but related features of problem talk. Additionally, the association between EMA co-rumination with general peers and CRQ co-rumination, which assessed behavior only with same-sex friends, is likely to be somewhat underestimated due to the additional variance included in the EMA measure.
Overall, our findings suggest that the EMA approach exhibits utility for further clarifying the role of co-rumination on adolescent depression. There are several limitations that should be considered when interpreting the results of this study. First, although small samples are typical for clinical studies utilizing intensive methodologies such as EMA, this limited our power to detect small-to-medium effects. Second, the small sample size and particularly small number of males in the sample also precluded gender comparisons. Third, the wide age range represented in the sample limits what the findings can tell us about the developmental course of the behaviors studied. Fourth, although the EMA methodology limits retrospective bias by asking youth to recall events during the past hour, it still relies on youth report and may still be affected by adolescents’ potentially biased recall of events. Fifth, because participants with MDD were recruited from clinical and community settings, we were not able to standardize treatments obtained, and some youth were beginning treatment during the EMA assessment. Thus, treatment effects represent a potential confound that cannot be ruled out. Sixth, in the interest of preserving power, we included all subtypes of peers (i.e., friends, classmates, teammates, romantic partners) in the EMA co-rumination measure; future research may explore the rate and effects of co-rumination with specific peer groups. Seventh, only face-to-face conversations about problems are included in the EMA problem talk measure. Thus, future research may incorporate the role of text messaging, online and phone communication. Finally, we did not directly observe adolescents engaging in co-rumination or problem-solving discussions with others, and although we believe it is reasonable to assume that regulatory strategies and social interactions reported as occurring in response to the same event occurred together, we cannot be certain that this is the case.
Together, these findings align with prior research20,21 suggesting that co-rumination is elevated in adolescents’ peer interactions prior to and after experiencing a MDE. Thus, co-rumination with peers appears to be a particularly important interpersonal process in adolescent depression. Additionally, the results of this study and others24,25 together suggest that co-rumination with parents is concurrently associated with depression. Interventions targeting co-rumination with peers and parents may be useful for prevention, treatment, and relapse prevention. Further, results suggest that youth with depression may benefit from interventions that increase their skills engaging in problem-solving with peers. Of note, it seems that adolescents with depression do not discuss problems with parents or peers more frequently than adolescents who are not depressed. Instead, the quality of discussions about problems is altered among adolescents with depression. This finding is consistent with research indicating that co-rumination with friends is uniquely associated with internalizing symptoms in community samples of youth, whereas self-disclosure of problems to friends is not.25 Thus, interventions for youth with MDD should target skills needed to competently interact with others – particularly peers – when discussing a problem, rather than focus on altering the frequency with which adolescents talk about problems with others.
Clinical Guidance.
Adolescents with MDD talked about their problems with parents and peers as often as youth with no lifetime history of Axis I disorders, but the way that youth with MDD talked about their problems differed from healthy youth.
Adolescents with MDD engaged in co-rumination (i.e., a perseverative, ruminative style of discussing problems that involves an excessive focus on negative aspects of the problem) with peers and parents significantly more often than healthy youth. In co-rumination, social partners encourage one another to ruminate about the negative aspects of the problem. Therefore, it may be fruitful to engage both youth and parents in developing alternative, non- ruminative styles of communication to use when discussing a problem.
Adolescents with MDD were not less likely to problem-solve with parents about a distressing event. However, compared to healthy youth, adolescents with MDD were significantly less likely to engage in problem-solving when talking with their peers.
Acknowledgments
This research was supported by National Institute of Drug Abuse grant R21DA024144 (JSS, RED) and the Clinical and Translational Science Institute at the University of Pittsburgh (National Institutes of Health [NIH]/ National Center for Research Resources [NCRR]/ Clinical and Translational Science Awards [CTSA] Grant UL1 RR024153).
The authors thank staff and study families of the Youth Emotional and Social Development (YES-D) Study. In particular, the authors thank Han-Tsung Min, MS, and Marcie Walker, BS, of the University of Pittsburgh, as well as Katie Burkhouse, MS, of State University of New York Binghampton and Karen Garelik, BS, of San Diego State University for their efforts collecting and managing these data.
Footnotes
Disclosure: Drs. Silk, Stone, Dahl, and Ms. Waller report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mr. Jennifer M. Waller, University of Pittsburgh.
Dr. Jennifer S. Silk, University of Pittsburgh.
Dr. Lindsey B. Stone, University of Pittsburgh.
Dr. Ronald E. Dahl, University of California, Berkeley.
References
- 1.Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neurosci Biobehav Rev. 2010;34(6):867–876. doi: 10.1016/j.neubiorev.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson RA. Emotion and self-regulation. In: Thompson RA, editor. Nebraska Symposium on Motivation, 1988: Vol. 36, Socioemotional development. Lincoln, NE: University of Nebraska Press; 1990. pp. 25–52. [Google Scholar]
- 3.Campos JJ, Mumme DL, Kermoian R, Campos RG. A functionalist perspective on the nature of emotion. Dev Emot Regul Biol Behav Consid. 1994;59:284–303. [PubMed] [Google Scholar]
- 4.Furman W, Buhrmester D. Age and sex differences in perceptions of networks of personal relationships. Child Dev. 1992;63(1):103–115. doi: 10.1111/j.1467-8624.1992.tb03599.x. [DOI] [PubMed] [Google Scholar]
- 5.Berndt TJ. The features and effects of friendship in early adolescence. Child Dev. 1982;53:1447–1460. [Google Scholar]
- 6.Joiner T, Metalsky GI. A prospective test of an integrative interpersonal theory of depression: A naturalistic study of college roommates. J Pers Soc Psychol. 1995;69:778–788. doi: 10.1037//0022-3514.69.4.778. [DOI] [PubMed] [Google Scholar]
- 7.Coyne JC. Depression and the response of others. J Abnorm Psychol. 1976;85:186–193. doi: 10.1037//0021-843x.85.2.186. [DOI] [PubMed] [Google Scholar]
- 8.Boivin M, Hymel S, Bukowski WM. The roles of social withdrawal, peer rejection, and victimization by peers in predicting loneliness and depressed mood in childhood. Dev Psychopathol. 1995;7:765–785. [Google Scholar]
- 9.Joiner T, Coyne JC, Blalock J. On the interpersonal nature of depression: Overview and synthesis. In: Joiner T, Coyne JC, editors. The interactional nature of depression. Washington, DC: American Psychological Association; 2002. pp. 3–19. [Google Scholar]
- 10.Forbes EE, Dahl RE. Neural systems of positive affect: Relevance to understanding child and adolescent depression? Dev Psychopathol. 2005;17:827–850. doi: 10.1017/S095457940505039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davey CG, Yücel M, Allen NB. The emergence of depression in adolescence: Development of the prefrontal cortex and the representation of reward. Neurosci Biobehav Rev. 2008;32:1–19. doi: 10.1016/j.neubiorev.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 12.Nelson EE, Leibenluft E, McClure EB, Pine DS. The social re-orientation of adolescence: A neuroscience perspective on the process and its relation to psychopathology. Psychol Med. 2005;35:163–174. doi: 10.1017/s0033291704003915. [DOI] [PubMed] [Google Scholar]
- 13.Silk JS, Davis S, McMakin DL, Dahl RE, Forbes EE. Why do anxious children become depressed teenagers? The role of social evaluative threat and reward processing. Psychol Med. 2012;42(10):2095–2107. doi: 10.1017/S0033291712000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rose AJ. Co-rumination in the friendships of girls and boys. Child Dev. 2002;73:1830–1843. doi: 10.1111/1467-8624.00509. [DOI] [PubMed] [Google Scholar]
- 15.Rose AJ, Carlson W, Waller EM. Prospective associations of co-rumination with friendship and emotional adjustment: Considering the socioemotional trade-offs of co-rumination. Dev Psychol. 2007;43:1019–1031. doi: 10.1037/0012-1649.43.4.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starr LR, Davila J. Clarifying co-rumination: Associations with internalizing symptoms and romantic involvement among adolescent girls. J Adolesc. 2009;32:19–37. doi: 10.1016/j.adolescence.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hankin BL, Stone L, Wright PA. Corumination, interpersonal stress generation, and internalizing symptoms: Accumulating effects and transactional influences in a multiwave study of adolescents. Dev Psychopathol. 2010;22:217–235. doi: 10.1017/S0954579409990368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Dev. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- 19.Langrock AM, Compas BE, Keller G, Merchant MJ, Copeland ME. Coping with the stress of parental depression: Parents’ reports of children’s coping, emotional, and behavioral problems. J Clin Child Adolesc Psychol. 2002;31(3):312–324. doi: 10.1207/S15374424JCCP3103_03. [DOI] [PubMed] [Google Scholar]
- 20.Stone LB, Hankin BL, Gibb BE, Abela JRZ. Co-rumination predicts the onset of depressive disorders during adolescence. J Abnorm Psychol. 2011;120:752–757. doi: 10.1037/a0023384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone LB, Uhrlass DJ, Gibb BE. Co-rumination and lifetime history of depressive disorders in children. J Clin Child Adolesc Psychol. 2010;39:597–602. doi: 10.1080/15374416.2010.486323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silk JS, Dahl RE, Ryan ND, et al. Pupillary reactivity to emotional information in child and adolescent depression: Links to clinical and ecological measures. Am J Psychiatry. 2007;164:1873–1880. doi: 10.1176/appi.ajp.2007.06111816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silk JS, Forbes EE, Whalen DJ, et al. Daily emotional dynamics in depressed youth: A cell phone ecological momentary assessment study. J Exp Child Psychol. 2011;110:241–257. doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waller EM, Rose AJ. Adjustment trade-offs of co-rumination in mother–adolescent relationships. J Adolesc. 2010;33:487–497. doi: 10.1016/j.adolescence.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waller EM, Rose AJ. Brief report: Adolescents’ co-rumination with mothers, co-rumination with friends, and internalizing symptoms. J Adolesc. 2013;36(2):429–433. doi: 10.1016/j.adolescence.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 27.Wade TJ, Cairney J, Pevalin DJ. Emergence of gender differences in depression during adolescence: National panel results from three countries. J Am Acad Child Adolesc Psychiatry. 2002;42(2):190–198. doi: 10.1097/00004583-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res. 1995;5:237–249. [Google Scholar]
- 29.Messer SC, Angold A, Costello EJ, Loeber R, Van Kammen W, Stouthamer-Loeber M. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: Factor composition and structure across development. Int J Methods Psychiatr Res. 1995;5:251–262. [Google Scholar]
- 30.Daviss WB, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the Mood and Feelings Questionnaire for depressive episodes in clinic and non-clinic subjects. J Child Psychol Psychiatry. 2006;47(9):927–934. doi: 10.1111/j.1469-7610.2006.01646.x. [DOI] [PubMed] [Google Scholar]
- 31.Kent L, Vostanis P, Feehan C. Detection of major and minor depression in children and adolescents: Evaluation of the Mood and Feelings Questionnaire. J Child Psychol Psychiatry. 1997;38(5):565–573. doi: 10.1111/j.1469-7610.1997.tb01543.x. [DOI] [PubMed] [Google Scholar]
- 32.Wood A, Kroll L, Moore A, Harrington R. Properties of the Mood and Feelings Questionnaire in adolescent psychiatric outpatients: A research note. J Child Psychol Psychiatry. 1995;36(2):327–334. doi: 10.1111/j.1469-7610.1995.tb01828.x. [DOI] [PubMed] [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- 34.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:981. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 35.Cohen J. A power primer. Psychol Bull. 1992;112(1):155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 36.Segrin C. Concordance on negative emotion in close relationships: Transmission of emotion or assortative mating? J Soc Clin Psychol. 2004;23(6):836–856. [Google Scholar]
- 37.Schaefer DR, Kornienko O, Fox AM. Misery does not love company: Network selection mechanisms and depression homophily. Am Sociol Rev. 2011;76:764–785. [Google Scholar]
- 38.Van Zalk MHW, Kerr M, Branje SJT, Stattin H, Meeus WHJ. It takes three: Selection, influence, and de-selection processes of depression in adolescent friendship networks. Dev Psychol. 2010;46:927–938. doi: 10.1037/a0019661. [DOI] [PubMed] [Google Scholar]
- 39.Rudolph KD, Flynn M, Abaied JL. A developmental perspective on interpersonal theories of youth depression. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York: The Guilford Press; 2008. pp. 79–102. [Google Scholar]
- 40.Hogue A, Steinberg L. Homophily of internalized distress in adolescent peer groups. Dev Psychol. 1995;31:897–906. [Google Scholar]
- 41.Prinstein MJ. Moderators of peer contagion: A longitudinal examination of depression socialization between adolescents and their best friends. J Clin Child Adolesc Psychol. 2007;36:159–170. doi: 10.1080/15374410701274934. [DOI] [PubMed] [Google Scholar]