Abstract
Intense interest has focused on the recent description of the anterolateral ligament of the knee. Advancing knowledge of its anatomy and function is leading to a realization of its importance in the rotatory control of the tibia in anterior cruciate ligament injuries. Reconstruction of this structure will increasingly become an important goal during anterior cruciate ligament reconstruction. However, preoperative assessment of this ligament is difficult. Clinical assessment of rotatory laxity has poor reproducibility, and it is difficult to define using current imaging techniques. This article is the first to describe a safe and reproducible arthroscopic technique to allow identification and examination of the anterolateral ligament of the knee. With the knee at 90° of flexion, the arthroscope is introduced through the anterolateral portal to allow clear visualization of the lateral gutter. Under direct vision, an accessory portal is made over the inferior limit of the lateral gutter. A shaver is then introduced through this portal and used to debride this synovial recess and define the anterolateral ligament. This allows the surgeon to examine the integrity of the anterolateral ligament, in particular its femoral insertion. If required, this additional information can facilitate the performance of a more accurate and effective extra-articular reconstruction.
With the rapid increase in interest in the existence1,2 and role of the anterolateral ligament (ALL) of the knee, an additional lateral reconstructive procedure may regain popularity when one is performing anterior cruciate ligament (ACL) reconstruction. Recent literature supports the finding that a lack of rotational control can still occur after classic single-bundle ACL reconstruction.3 Double-bundle reconstruction was performed to try to minimize this rotational instability, but to date, there is no strong clinical or biomechanical evidence of its superiority.4 Extra-articular lateral reconstruction to treat anterolateral instability has been proposed.5 These procedures have not been widely popularized because of their additional morbidity and the lack of evidence-based clinical guidelines. New insight into the existence of a distinct ligamentous structure on the anterolateral aspect of the knee has focused our attention on the secondary restraint of the rotational laxity of the knee after ACL injury.
The location of the femoral and tibial attachments of the ALL has been recently clarified. As described, the attachment of the ALL to the lateral epicondyle was found to be anterior and distal to the attachment of the lateral collateral ligament (LCL), near the articular cartilage of the distal region of the lateral femoral condyle. According to Helito et al.,2 a bifurcation can be observed, terminating in 2 ligament attachments to the lateral meniscus, with a more distal attachment to the tibia between the Gerdy tubercle and the fibular head.
Arthroscopic examination of the ALL and other lateral structures of the knee could potentially aid the diagnosis of rotational instability due to ALL injury and help develop less invasive and more anatomic anterolateral reconstruction. On the basis of the anatomy, we report a simple and easy-to-use arthroscopic technique for the identification and examination of the ALL.
Surgical Technique
This study was conducted in 2 steps. In the first step, the ALL was arthroscopically identified in a patient who underwent arthroscopic treatment for iliotibial band syndrome. In the second step, a cadaveric study was performed. This consisted of arthroscopic identification of the ALL and its neighboring structures (popliteus tendon, LCL), followed by an open anatomic dissection, which was performed to confirm the correct identification of these anatomic structures.
Step 1: Arthroscopic Identification
After a standardized arthroscopic inspection of the joint, the knee is placed in 90° of flexion. By use of the anterolateral portal, the arthroscope is introduced into the lateral gutter of the knee joint. With a standard needle and under direct visualization, the optimal entrance point at the inferior limit of the lateral gutter is defined. An incision is placed directly over the hole from the needle to make an accessory superolateral portal (Fig 1). By use of this portal, a shaver is introduced into the lateral gutter to debride the synovial tissue situated between the lateral cortex of the femur and the fascia lata. This step allows clear identification of the 3 lateral structures, from proximally to distally (Video 1, Table 1): LCL, ALL, and popliteus tendon.
Fig 1.
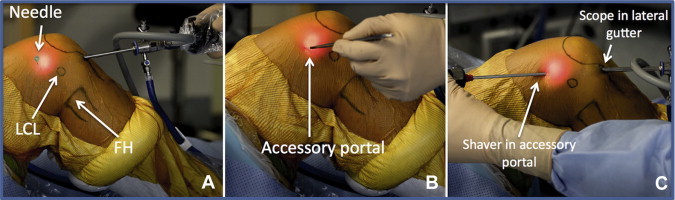
Accessory portal placement in a right knee. The arthroscope is introduced through the anterolateral portal and positioned in the lateral gutter. (A) A needle is placed proximally and anteriorly to the LCL insertion in the lateral gutter under direct arthroscopic vision. (B) A stab incision is performed directly over the hole from the needle to create the superolateral accessory portal. (C) The shaver is introduced through the accessory portal, and the arthroscope is placed in the lateral gutter to perform synovial debridement. (FH, fibular head.)
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Knee position during exposure of lateral structures of knee | The knee is positioned at 90° of flexion. Transillumination is used to correctly position the arthroscope within the lateral gutter. | Visualization of the lateral gutter and placement of the accessory portal are impaired with the knee in extension. |
| Placement of accessory superolateral portal | A standard needle is introduced under direct vision to optimize the positioning of the accessory superolateral portal. | Placement of the accessory superolateral portal in a too-distal position prevents adequate exposure of the lateral structures and the assessment of their integrity. |
| Debridement of synovial tissue between lateral cortex of femur and fascia lata | With the blade facing the fascia lata, the shaver is carefully passed between the fascia lata and the popliteus tendon. | Inadequate shaving results in poor visualization of the lateral structures. During debridement of the synovial tissue, the shaver blade must face the fascia lata to prevent injury to the lateral structures. |
| Assessment of integrity of ALL of knee | The shaver is removed, and a probe is inserted and placed around the ALL. Internal tibial rotation is performed to assess its anterolateral rotational control. | Probing of the ALL without assessment of its tension under internal tibial rotation is inadequate. The tibial insertion of the ALL is hidden below the lateral meniscus. |
Of note, distally, the shaver must be carefully passed between the fascia lata and the popliteus tendon with the blade facing the fascia lata. This step is critical because it prevents injury to the ALL. In particular, care is taken distally to preserve the fine ALL band coming from the femur to the tibia (Fig 2). At this stage, the shaver is removed, and a probe is introduced through the working portal to palpate and assess the integrity of the ALL during rotatory control.
Fig 2.
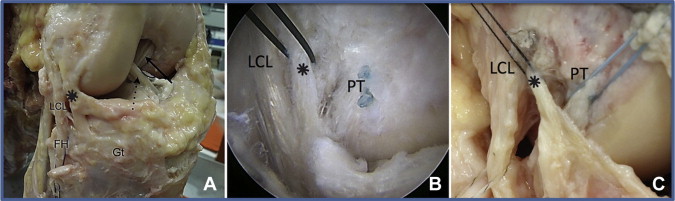
Cadaveric study in a right knee. (A) Cadaveric dissection of ALL (asterisk). (B) Arthroscopic view of the 3 lateral structures with a 70° arthroscope (slack ALL). (C) Knee after anatomic dissection (tight ALL). From distally to proximally, the popliteus tendon (PT), ALL (asterisk), and LCL are clearly identified (B, C). (FH, Fibular Head; Gt, Gerdy's tubercle.)
(Fig 2A reprinted with permission from Helito, C et al, Orthopedic Journal of Sports Medicine, Anatomy and Histology of the Knee Anterolateral Ligament (vol. 1, no. 7) pp. 1-5, copyright 2013, SAGE Publications, Inc.2)
Step 2: Cadaveric Study
Arthroscopic identification of the ALL was performed on a right knee specimen as described previously. With a Torpedo shaver (Arthrex, Naples, FL), as described earlier, the lateral gutter of the knee was debrided appropriately. From distally to proximally, the femoral insertions of the popliteus tendon, ALL, and LCL were easily identified.
The 30° arthroscope was then exchanged for a 70° arthroscope to improve the view of the lateral structures. Suture anchors with distinct suture thread colors were arthroscopically placed into the femoral insertions of the popliteus tendon, ALL, and LCL. An additional nitinol loop was placed around the ALL's femoral insertion (Video 1). An anatomic dissection of the specimen was performed to confirm the correct identification of the ALL and its neighboring structures (Fig 2).
Discussion
The ALL was first described in 1879 by Segond6 as a “pearly, resistant, fibrous band which invariably showed extreme amounts of tension during forced internal rotation of the knee.” Other authors have described it as an anatomic variation of the LCL7 or as a “capsular ligament” that is constantly present.8 More recently, the anatomic description of the ALL has been refined to a distinct ligamentous structure at the anterolateral aspect of the knee with consistent origin and insertion-site features.1,2 Histologic investigation had confirmed the ligamentous nature of this structure.2 Given its structure and location, it is proposed that the ALL controls internal tibial rotation. A high correlation between the pivot-shift phenomenon and lesions to the anterolateral structures has been shown to exist in a recent kinematic study by Monaco et al.9 Although single- and double-bundle ACL reconstruction techniques reliably restore functional knee stability, some patients continue to complain of rotational instability.4,10 Failure to repair the secondary stabilizers has been noted as a cause of reconstruction failure.11 The examination and assessment of this ligament will become increasingly important in the decision making before and during ACL surgery. However, it remains difficult to define on conventional sonographic or magnetic resonance imaging and has been previously described as more of a capsular reinforcement than a distinct ligament.8 In addition, the clinical assessment of rotatory instability after ACL injury when using the pivot-shift test can be difficult. The sensitivity of this test varies among examiners, depending on the method used, the force applied, and whether the patient is apprehensive or relaxed. Our article describes a simple-to-use arthroscopic technique for the identification of the ALL of the knee. This technique allows direct visualization and examination of the femoral insertion and proximal part of the ALL. Probing the ligament during external and internal tibial rotation aids assessment of its ability to control excessive internal tibial rotation. This could potentially help surgeons to decide whether an anterolateral reconstruction is required and optimize its anatomic placement during the anterolateral reconstruction. The limitation of this technique is that the arthroscopic visualization of the ALL is limited to its proximal part. Arthroscopic assessment of its tibial insertion is difficult because it lies below the lateral meniscus (Table 1).
The lateral accessory portal and the development of the synovial recess have been previously described in the arthroscopic treatment of iliotibial band syndrome.12 Thus the technique is safe, and we have found it to have a relatively short learning curve.
In this article we have described a simple and easy-to-use technique that allows for the intraoperative assessment of both the ALL of the knee and the other lateral structures. This additional information could potentially facilitate the performance of a more accurate and effective extra-articular reconstruction, if required. Further studies are required to investigate normal and abnormal ALLs, as well as the ALL's correlation with anterolateral instability.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.S-C., J-M.F., and M.T. receive support from Arthrex.
Supplementary Data
Arthroscopic identification of ALL of knee.
References
- 1.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helito C.P., Demange M.K., Bonadio M.B. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med in press, available online. 9 December, 2013 doi: 10.1177/2325967113513546. doi: 10.1177/2325967113513546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chouliaras V., Ristanis S., Moraiti C., Stergiou N., Georgoulis A.D. Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: An in vivo study comparing tibial internal-external rotation. Am J Sports Med. 2007;35:189–196. doi: 10.1177/0363546506296040. [DOI] [PubMed] [Google Scholar]
- 4.Misonoo G., Kanamori A., Ida H., Miyakawa S., Ochiai N. Evaluation of tibial rotational stability of single-bundle vs. anatomical double-bundle anterior cruciate ligament reconstruction during a high-demand activity—A quasi-randomized trial. Knee. 2012;19:87–93. doi: 10.1016/j.knee.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 5.McGuire D.A., Wolchok J.C. Extra-articular lateral reconstruction technique. Arthroscopy. 2000;16:553–557. doi: 10.1053/jars.2000.7670. [DOI] [PubMed] [Google Scholar]
- 6.Segond P. National Library of France; Paris: 1879. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse; pp. 1–85. Available at http://www.patrimoine.edilivre.com/recherches-cliniques-et-experimentales-sur-les-epanchements-sanguins-du-genou-par-entorse-par-paul-segond-segond-paul-ferdinand-dr-1879-ark-12148-bpt6k5712206r.html. [Google Scholar]
- 7.Diamantopoulos A., Tokis A., Tzurbakis M., Patsopoulos I., Georgoulis A. The posterolateral corner of the knee: Evaluation under microsurgical dissection. Arthroscopy. 2005;21:826–833. doi: 10.1016/j.arthro.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Hugston J.C., Andrews J.R., Cross M.J. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am. 1976;58:173–179. [PubMed] [Google Scholar]
- 9.Monaco E., Maestri B., Labianca L. Navigated knee kinematics after tear of the ACL and its secondary restraints: Preliminary results. Orthopedics. 2010;33(suppl):87–93. doi: 10.3928/01477447-20100510-58. [DOI] [PubMed] [Google Scholar]
- 10.Meredick R.B., Vance K.J., Appleby D., Lubowitz J.H. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: A meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 11.George M.S., Dunn W.R., Spindler K.P. Current concepts review: Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026–2037. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 12.Michels F., Jambou S., Allard M., Bousquet V., Colombet P., de Lavigne C. An arthroscopic technique to treat the iliotibial band syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17:233–236. doi: 10.1007/s00167-008-0660-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic identification of ALL of knee.


