Abstract
Labral reconstruction is becoming an important treatment modality for hips with nonsalvageable labra. Nonsalvageable labra can be present in cases of intrasubstance damage, revision surgery after debridement, labral calcification, and hypoplasia. Previous methods of reconstruction have been performed in an open manner and arthroscopically using ligamentum teres, iliotibial band, and gracilis autograft. We present an alternate method of arthroscopic labral reconstruction using capsular autograft. The technique uses readily available capsular tissue during arthroscopy with no donor-site morbidity. This technique may be valuable in appropriately selected patients with labral deficiency.
Biomechanical and clinical studies continue to document the importance of the hip labrum. Ferguson et al.1,2 have shown the importance of the labrum in providing a fluid seal and assisting in contact force transmission. Clinically, the results of labral repair appear to be better than those of labral resection.3,4 Ideally, when one is treating patients with labral tears, the labrum can be preserved because labral damage has been associated with degenerative changes in the hip joint.5
At the time of surgery, many patients have labral tissue that cannot be salvaged. This may be because of significant tearing, degenerative tissue, or hypoplasia. Patients also present after labral debridement with persistent postoperative pain. Many of these patients have undergone significant labral resection. When the labrum is nonsalvageable or nonexistent, labral reconstruction is a viable treatment option. To our knowledge, three types of labral reconstruction have been described. Philippon et al.6 described an arthroscopic technique using iliotibial band autograft with promising early results. Matsuda7 recently described an arthroscopic technique using gracilis autograft. Sierra and Trousdale8 reported an open technique using the ligamentum teres.
We introduce a method of arthroscopic labral reconstruction using local capsular autograft tissue. The indications for this technique are listed in Table 1. This method of labral reconstruction has the advantage of avoiding donor-site morbidity by using locally available tissue. At our institution, our standard technique uses hamstring autograft reconstruction; however, the local capsular autograft technique has found use in patients with smaller labral defects, when a gracilis tendon is not necessary but circumferential labral coverage is desirable. The technique, however, does preclude the ability to close or plicate the capsule, which we believe is important in cases with potential instability, and therefore should not be used in cases of borderline dysplasia or ligamentous laxity.
Table 1.
Advantages and Disadvantages of Capsular Autograft Reconstruction
| Advantages | Disadvantages |
|---|---|
| No donor-site morbidity | Inability to perform capsular closure |
| No risk of disease transmission | Less robust graft source |
| Ability to fill small segmental defects | |
| Locally available tissue |
Surgical Technique
Operating Room Preparation
We perform hip arthroscopy using a standard traction table in the supine position, as previously described by Kelly et al.9 A standard fluoroscope is used during portal placement, labral repair, and bony debridement. Proper anesthesia with paralysis is necessary for safe distraction of the hip joint and prevention of complications during hip arthroscopy. Hypotensive anesthesia has been shown to be beneficial in shoulder arthroscopy, and the same principles apply to hip arthroscopy.10 Lower blood pressures allow the surgeon to minimize pump pressure and prevent fluid extravasation.11,12
The patient is placed on a fracture table or a traction extension table, with a well-padded perineal post.13 The patient is placed in the slight Trendelenburg position to decrease perineal pressure on the post. The operative extremity is positioned in adduction, with the hip flexed to 10° and the femur internally rotated.14
Portal Placement
A 20-gauge spinal needle is used to vent the hip joint under gentle distraction.15 The bevel of the needle is positioned facing the femoral head and advanced toward the superior aspect of the joint space. With the bevel in this position, the possibility of damaging cartilage on the femoral head is minimized. The needle is advanced until a “pop” is felt as the needle passes through the anterosuperior joint capsule. The stylet of the needle is then removed to vent the joint and create an air arthrogram. Traction is applied to the hip. A 14-gauge needle and nitinol wire (Arthrex, Naples, FL) are then used to create an anterolateral portal using a technique that has been previously described.14 A 70° arthroscope is introduced into the hip joint through the anterolateral portal.
Dry arthroscopy of the hip is used to create a mid-anterior portal (MAP) by use of an outside-in technique. The MAP is placed at an approximately 30° angle anterior to the anterolateral portal. A 14-gauge spinal needle and nitinol wire are then advanced into the joint, adjacent to the labrum, through the anterior capsule. A 5-mm cannula is used to introduce a curved beaver blade (Smith & Nephew, London, England). An anterior capsulotomy is then created, with care taken to leave a satisfactory cuff of capsular tissue adjacent to the labrum and acetabular rim (Table 2). If the capsulotomy is performed too close to the acetabular rim, the cuff of capsular tissue will not be satisfactory for reconstruction.
Table 2.
Key Points for Capsular Autograft Reconstruction
| Point | Rationale |
|---|---|
| Ensure capsulotomy is performed close to the femoral head. | This allows sufficient capsular tissue for reconstruction. |
| Avoid trimming of the medial capsule until reconstruction has been performed. | Excessive trimming of the capsule will not allow sufficient tissue for reconstruction. |
| Use a high-speed burr to decorticate the acetabular rim. | This provides a bleeding surface for the graft to heal. |
| Avoid capsular autograft in patients with borderline dysplasia or ligamentous laxity. | This patient population should undergo capsular closure to avoid instability. |
Capsular Autograft Reconstruction
Diagnostic arthroscopy is carried out. The labral tissue is evaluated, and nonsalvageable tissue is debrided back to a stable base (Video 1). It should be noted that all salvageable labral tissue should be preserved. In many cases a portion of the labrum can be repaired and nonsalvageable labral tissue reconstructed with capsular tissue (Fig 1). A distal MAP is often created approximately 3 to 4 cm distal to the MAP. At this point, acetabuloplasty of the planned area, if any, should be performed. The capsule over the anterosuperior acetabulum is elevated from the bony rim by use of cautery (Smith & Nephew or Arthrex), with care taken to preserve the capsule adjacent to the acetabulum (Fig 2). The acetabuloplasty is performed with a round 5-mm high-speed burr. If no pincer lesion is present, the acetabular rim adjacent to the labral damage is decorticated to expose a healthy surface of bleeding bone for repair/reconstruction (Fig 3).
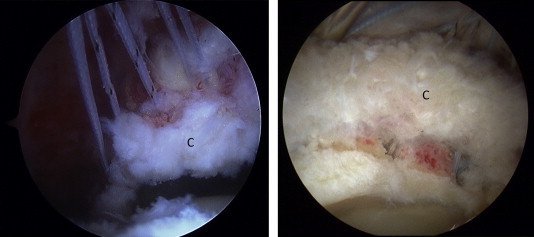
Fig 1.
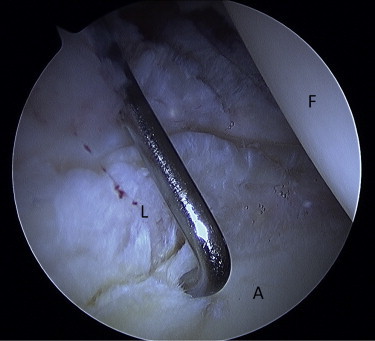
Arthroscopic view of right hip through anterolateral portal. Example of nonsalvageable labrum (L). (A, acetabulum; F, femoral head).
Fig 2.
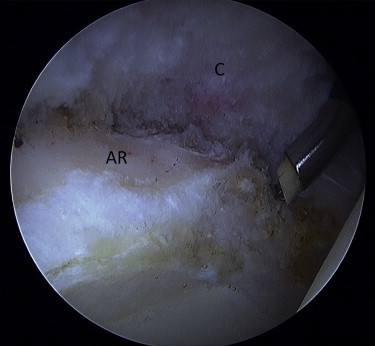
Arthroscopic view of right hip through anterolateral portal. The nonsalvageable labrum has been debrided. The capsule (C) has been elevated from the acetabular rim (AR).
Fig 3.
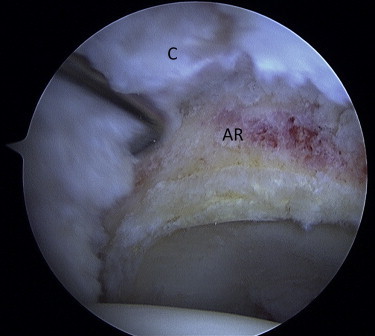
Arthroscopic birds-eye view of right hip through anterolateral portal. The capsule (C) has been elevated. The acetabular rim (AR) has been burred to remove a pincer lesion.
After acetabuloplasty, salvageable labral tissue is repaired if necessary with 2.9-mm Arthrex PushLock anchors. The transition zone between healthy labrum and nonsalvageable labrum is debrided until remaining labral tissue is stable. At this point, the acetabular rim and the area of labral deficiency are assessed. To perform capsular autograft reconstruction, the capsular tissue along the acetabular rim should be sufficient to cover the remaining rim and protrude equidistant to the native labrum. Planned anchor spacing in the area of labral deficiency is 5 to 8 mm. Anchors are placed at the terminal ends of the labral deficiency to overlap capsular tissue on labral tissue because this may better restore labral function. We use 3.0-mm single-loaded suture anchors (Arthrex) for reconstruction. Viewing is typically through the anterolateral portal. The distal MAP is used for drilling and anchor placement. After each anchor is placed, a 90° SutureLasso (Arthrex) is used to pass a nitinol wire loop through the adjacent capsular tissue via the MAP. Suture is then shuttled through the capsule. We use a mattress suture technique through the capsule (Fig 4). Care should be taken to ensure that when the suture is tied, the capsular tissue lies on the acetabular rim in a manner similar to the adjacent labral tissue. It should be noted that excess capsular tissue can be trimmed back with a suction shaver after reconstruction; however, if the suture is passed too close to the free edge of the capsular tissue, then the capsule will bunch and the tissue will not protrude beyond the rim when the knots are tied. This is critical if the capsular tissue is to restore labral function. Suture is then shuttled out the MAP and tagged. This process is repeated for each anchor (Fig 5). The sutures are then tied, and the capsular tissue is assessed. Excess capsular tissue is trimmed back so that the reconstructed tissue protrudes similarly to the adjacent health labral tissue (Fig 6).
Fig 4.
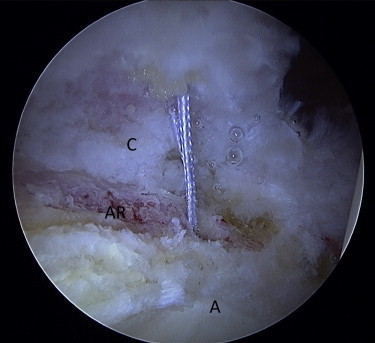
Arthroscopic view of right hip through anterolateral portal. A preloaded suture anchor has been inserted in the acetabular rim (AR). Suture has been shuttled through the capsule (C). (A, acetabulum.)
Fig 5.
Arthroscopic birds-eye view from peripheral compartment of right hip through anterolateral portal. Sutures have been passed in a horizontal mattress fashion through the capsule (C) overlying the labral defect.
Fig 6.
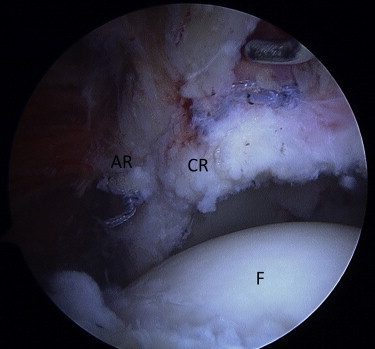
Arthroscopic birds-eye view from peripheral compartment of right hip through anterolateral portal. Sutures have been tied in a horizontal mattress fashion. The capsular reconstruction (CR) covers the labral defect and restores graft to the area. (AR, acetabular rim; F, femoral head.)
After labral reconstruction, all instruments are removed from the hip and traction is released. The reconstructed tissue should restore the suction seal of the labrum (Fig 7). Femoral head and neck osteoplasty can now be performed to remove cam deformity, if necessary. After femoral preparation, the capsule cannot be closed. We again caution that this technique is not an option for cases with acetabular dysplasia or borderline dysplasia. We do not use this method of reconstruction for patients with a lateral center-edge angle less than 25° or in cases of ligamentous laxity. Patients with dysplasia appear to benefit from capsular closure or capsular plication to restore hip stability, and capsular reconstruction will likely leave these patients with persistent instability.16
Fig 7.
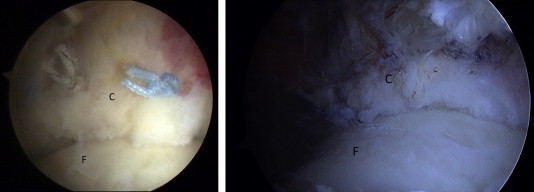
Arthroscopic birds-eye view from peripheral compartment of right hip through anterolateral portal. Traction has been released. The capsular reconstruction (C) functions as labral tissue. (F, femoral head.)
Postoperative Rehabilitation
The postoperative rehabilitation is patient specific and depends on concomitant procedures that are performed in addition to capsular autograft reconstruction. In general, patients with labral reconstruction are advised to maintain 20-lb heel-touch weight bearing for 6 weeks. A hip brace (DJO Global, Vista, CA) is used to limit range of motion to 90° of flexion for the first 2 to 6 weeks. Range of motion is then allowed to progress within a pain-free zone.
When the patient is fully weight bearing and achieves full range of motion, therapy is advanced. Gentle strengthening exercises begin with a stationary bicycle and isometrics. As strengthening progresses, patients start using an elliptical machine and slide board and perform hip girdle (gluteus medius) strengthening. When range of motion and strength are satisfactory, we begin sport-specific training.
Discussion
Labral reconstruction has become an important tool in the armamentarium of hip arthroscopists. Reports of satisfactory outcomes after labral debridement, labral refixation, and labral repair are well documented; however, it does appear that restoration of the labrum improves clinical results.3,4,17 Early reports of labral reconstruction using hamstring tendon and iliotibial band appear promising.6,18,19 No studies comparing graft choices are available at this time; however, it stands to reason that a collagen scaffold to restore labral function will be necessary. Reconstruction using capsular autograft is another option for the treatment of labral deficiency.
The advantages and disadvantages of capsular autograft reconstruction are presented in Table 1. A significant advantage of this technique is lack of donor-site morbidity. Capsular tissue is readily available along the acetabular rim, and if handled appropriately, it can serve as a reconstruction source. This avoids donor-site morbidity and may decrease postoperative pain, scarring, and blood loss. Capsular tissue is also well suited for filling small or segmental labral defects. We have typically used this method of reconstruction for defects measuring 10 to 20 mm. The main disadvantage of this technique is the inability to close or plicate the capsule after reconstruction. In our opinion this precludes the use of this technique in patients with a lateral center-edge angle less than 25°. It is unclear at this point how capsular tissue will compare with other graft choices such as hamstring tendon or iliotibial band.
Labral reconstruction is a new technique with limited outcomes data; however, preliminary reports show satisfactory results.6,18 Further research is needed to evaluate graft choices for labral reconstruction. Histologic studies after labral reconstruction are lacking. We believe that the technique of capsular autograft reconstruction may have a role in labral reconstruction going forward for patients without acetabular dysplasia.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.G.D. receives support from Arthrex, Pacira, MAKO Surgical, Breg, MedWest, ATI, Orthomerica, DJO Global, Stryker.
Supplementary Data
Labral reconstruction of hip using local capsular autograft.
References
- 1.Ferguson S.J., Bryant J.T., Ganz R., Ito K. The acetabular labrum seal: A poroelastic finite element model. Clin Biomech (Bristol, Avon) 2000;15:463–468. doi: 10.1016/s0268-0033(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson S.J., Bryant J.T., Ganz R., Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/s0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 3.Espinosa N., Rothenfluh D.A., Beck M., Ganz R., Leunig M. Treatment of femoro-acetabular impingement: Preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 4.Larson C.M., Giveans M.R., Stone R.M. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: Mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 5.McCarthy J.C., Noble P.C., Schuck M.R., Wright J., Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Philippon M.J., Briggs K.K., Hay C.J., Kuppersmith D.A., Dewing C.B., Huang M.J. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: Technique and early outcomes. Arthroscopy. 2010;26:750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Matsuda D.K. Arthroscopic labral reconstruction with gracilis autograft. Arthrosc Tech. 2012;1:e15–e21. doi: 10.1016/j.eats.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sierra R.J., Trousdale R.T. Labral reconstruction using the ligamentum teres capitis: Report of a new technique. Clin Orthop Relat Res. 2009;467:753–759. doi: 10.1007/s11999-008-0633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly B.T., Weiland D.E., Schenker M.L., Philippon M.J. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Morrison D.S., Schaefer R.K., Friedman R.L. The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy. 1995;11:557–560. doi: 10.1016/0749-8063(95)90131-0. [DOI] [PubMed] [Google Scholar]
- 11.Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: Complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84–88. doi: 10.1097/01.blo.0000043048.84315.af. [DOI] [PubMed] [Google Scholar]
- 12.Fowler J., Owens B.D. Abdominal compartment syndrome after hip arthroscopy. Arthroscopy. 2010;26:128–130. doi: 10.1016/j.arthro.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Byrd J.W. Hip arthroscopy. The supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 14.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
- 15.Domb B.G., Botser I.B. Iatrogenic labral puncture of the hip is avoidable. Arthroscopy. 2012;28:305–307. doi: 10.1016/j.arthro.2011.12.002. author reply 307-308. [DOI] [PubMed] [Google Scholar]
- 16.Domb B.G., Stake C.E., Lindner D., El-Bitar Y., Jackson T.J. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: Two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 17.Byrd J.W., Jones K.S. Hip arthroscopy for labral pathology: Prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Matsuda D.K., Burchette R.J. Arthroscopic hip labral reconstruction with a gracilis autograft versus labral refixation: 2-year minimum outcomes. Am J Sports Med. 2013;41:980–987. doi: 10.1177/0363546513482884. [DOI] [PubMed] [Google Scholar]
- 19.Boykin R.E., Patterson D., Briggs K.K., Dee A., Philippon M.J. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41:2296–2301. doi: 10.1177/0363546513498058. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Labral reconstruction of hip using local capsular autograft.


