Abstract
Bone marrow stimulation techniques for the treatment of articular cartilage defects such as microfracture so far have solely reproduced mechanically inferior fibrous cartilage tissue, which might result in unsatisfactory clinical results at midterm follow-up. A recent study has shown an improvement in repair tissue quality by enhancing microfracture with a chitosan-based biomaterial (BST-CarGel; Piramal, Laval, Quebec, Canada). BST-CarGel so far has only been applied by arthrotomy, which might lead to increased scar tissue formation and thus compromise recovery time and clinical outcome. We describe a surgical technique for an arthroscopic treatment of cartilage defects of the knee with microfracture in combination with BST-CarGel to benefit from improved repair tissue quality and to reduce arthrotomy-related morbidity.
Articular cartilage defects virtually have no self-healing capacity. As a consequence, a surgical approach for symptomatic grade III or IV defects is required. The most frequently used bone marrow–based cartilage restoration technique is the microfracture technique introduced by Steadman et al.1 The limitations of this technique include a high rate of intralesional new bone formation2 or progressive ossification of the regenerated tissue and limited biomechanical tissue properties, that is, formation of fibrous cartilage.3
Autologous chondrocyte implantation4 has proved to partially avoid the degeneration of repair tissue and change in phenotype (from cartilage-like tissue toward bone) over time and to produce, in many cases, a regenerated tissue histologically quite similar to hyaline joint cartilage with superior mechanical properties.3 The flaws of this technique are the expense and the fact that a 2-stage procedure is required.
A new chitosan-based biomaterial was developed to form a stable clot in the cartilage lesion after microfracture procedure. It allows ingrowth of mesenchymal progenitor cells from the subchondral bone and, thereby, formation of repair tissue. The major component, chitosan, is derived from deacetylation of chitin, the structural component of crustacean shell. It is characterized by low toxicity and by biocompatibility, biodegradability, and adhesivity to tissues.5 A recently published randomized clinical trial was able to show that the application of BST-CarGel (Piramal, Laval, Quebec, Canada) in combination with microfracture quantitatively and qualitatively improved cartilage repair tissue when compared with microfracture alone.6 A major drawback of the application of BST-CarGel is that a mini-arthrotomy is required for the implantation. Shive et al.5 proposed an arthroscopic delivery in case the entire lesion can be observed within the arthroscopic field of view.
We thus propose our arthroscopic surgical technique for the treatment of cartilage lesions with microfracture in combination with BST-CarGel to benefit from the enhanced cartilage repair by BST-CarGel and the reduced morbidity of an arthroscopic treatment.
Technique
The BST-CarGel may be applied in combination with microfracture in a single-step procedure. The key steps are shown in Fig 1 and Video 1.
Fig 1.
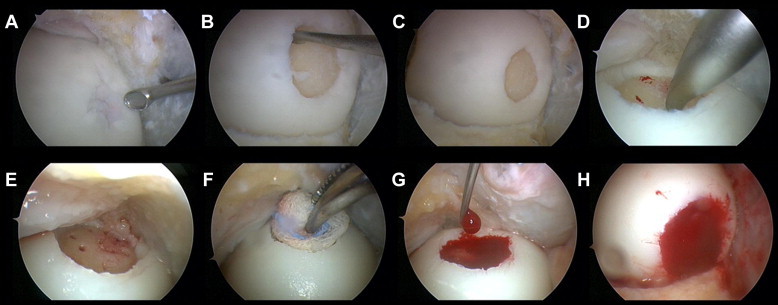
Key steps of arthroscopic treatment of cartilage lesions with microfracture and BST-CarGel. (A-C) The cartilage defect is debrided down to the subchondral bone, with removal of the calcified layer, and to a stable rim of healthy cartilage. (D) Microfractures are performed with an awl. (E) The defect is arranged in a horizontal position, and the liquid is drained. (F) The defect can be further dried with a swab. (G) The BST-CarGel is injected into the defect and (H) forms a stable clot in the defect after 15 minutes.
The defect is exposed arthroscopically, and protruding synovial tissue is removed. Proper visualization of the defect in a horizontal position is a prerequisite for later polymerization of the biomaterial and must be ensured before one establishes the final indication for an arthroscopic cartilage repair approach. Subsequently, the damaged cartilage is debrided with a sharp curette (Fig 1A) and shaver. The calcified layer is removed to allow adequate adhesion of bone marrow cells (Fig 1B). A stable rim of healthy surrounding cartilage should be respected with regard to the containment of the defect (Fig 1C). The surgeon performs the microfractures with an awl, picking holes of 3 to 4 mm in depth at a distance of 3 to 4 mm (Fig 1D). Subsequently, the leg is lifted to arrange the defect in a horizontal position, and the arthroscopy liquid is drained (Fig 1E). The defect can be further dried by use of a small swab (Fig 1F). Meanwhile, the BST-CarGel is prepared according to the manufacturer's instructions with 4.5 mL of autologous venous blood. The BST-CarGel is then injected and the defect entirely filled (Fig 1G). Leakage of the BST-CarGel must be avoided. After 15 minutes, stable clotting of the BST-CarGel is usually accomplished (Fig 1H). An intra-articular drainage (without suction) is inserted, and the arthroscopy portals are closed in standard fashion. The leg is immobilized in extension for 24 hours. Helpful advice for this surgical technique is summarized in Table 1, and magnetic resonance imaging results are shown in Fig 2.
Table 1.
Tips for Arthroscopic Treatment With Microfracture and BST-CarGel
| Tips | Reasons |
|---|---|
| Thoroughly remove protruding synovial tissue to facilitate visualization of the defect in the horizontal position. | Compromised visualization and/or contact of synovial tissue with the lesion site might impede application of the biomaterial. |
| Debride the damaged cartilage down to the subchondral bone with removal of the calcified layer. | Remaining damaged tissue may compromise repair tissue formation. |
| Dry the defect with suction or with a swab. | Dryness of the defect bed is crucial for adhesion of the BST-CarGel. |
Fig 2.
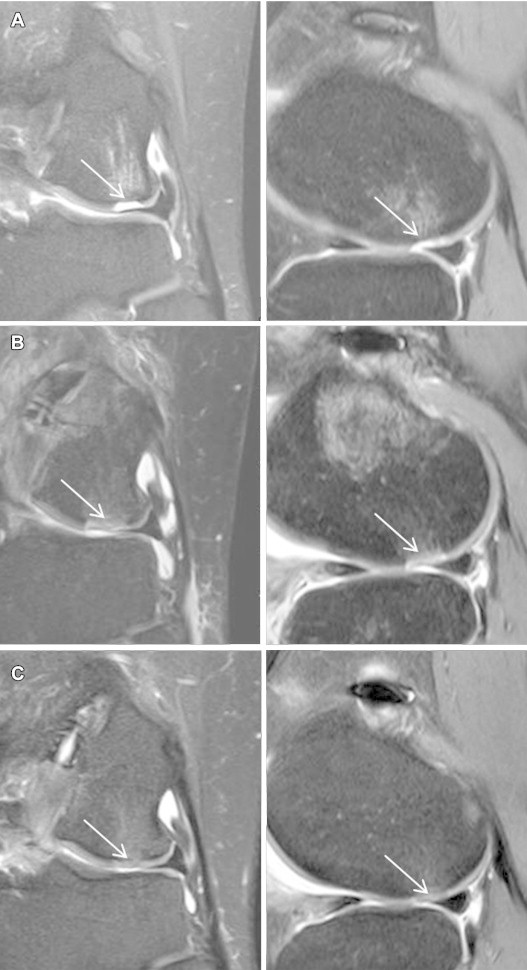
Frontal and sagittal views of echo-planar diffusion-weighted magnetic resonance imaging study (A) before, (B) 6 weeks after, and (C) 6 months after arthroscopic treatment with microfracture in combination with BST-CarGel application for cartilage defect of lateral femoral condyle. The magnetic resonance imaging results indicate complete filling of the defect and remission of the subchondral bone edema over time (arrows). After 6 months, the repair tissue appears more or less isointense compared with the native surrounding cartilage.
Discussion
We have shown the feasibility of an arthroscopic application of BST-CarGel in combination with microfracture. The less invasive approach could lead to reduced morbidity and a faster recovery. In terms of economic reasons, the minimally invasive approach could reduce operative times and prove cost-effective. Nonetheless, the arthroscopic approach is technical demanding and not applicable for all defect localizations. In particular, defects of the patella and of the posterior part of the femoral condyles are difficult to address because a horizontal position of the defects can hardly be achieved. Table 2 summarizes the advantages and disadvantages of the arthroscopic approach.
Table 2.
Advantages and Disadvantages of Arthroscopic Treatment of Cartilage Lesions With Microfracture and BST-CarGel
| Advantages | Disadvantages |
|---|---|
| Minimally invasive surgery | Demanding surgical technique |
| Faster operative time | Some localizations of cartilage defects (patella, posterior condyles) may not be addressed |
| Less scar tissue formation and faster recovery | No long-term data |
BST-CarGel seems to be capable of enhancing microfracture and possibly overcoming some of the major shortcomings of this technique by stabilizing the blood clot. Unfortunately, to date, only 12 months' follow-up is available for this biomaterial. Further clinical studies are therefore required to evaluate the long-term benefit of enhanced microfracture with BST-CarGel and of the arthroscopic application versus open surgery.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Key principles and surgical steps of arthroscopic treatment of cartilage lesions with microfracture and BST-CarGel.
References
- 1.Steadman J.R., Rodkey W.G., Singleton S.B., Briggs K.K. Microfracture technique for full-thickness chondral defects: Technique and clinical results. Oper Tech Orthop. 1997;7:300–304. [Google Scholar]
- 2.Mithoefer K., McAdams T., Williams R.J., Kreuz P.C., Mandelbaum B.R. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: An evidence-based systematic analysis. Am J Sports Med. 2009;37:2053–2063. doi: 10.1177/0363546508328414. [DOI] [PubMed] [Google Scholar]
- 3.Saris D.B., Vanlauwe J., Victor J. Treatment of symptomatic cartilage defects of the knee: Characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(suppl 1):10S–19S. doi: 10.1177/0363546509350694. [DOI] [PubMed] [Google Scholar]
- 4.Brittberg M., Lindahl A., Nilsson A., Ohlsson C., Isaksson O., Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331:889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 5.Shive M.S., Hoemann C.D., Restrepo A. BST-CarGel: In situ chondroinduction for cartilage repair. Oper Tech Orthop. 2006;16:271–278. [Google Scholar]
- 6.Stanish W.D., McCormack R., Forriol F. Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am. 2013;95:1640–1650. doi: 10.2106/JBJS.L.01345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Key principles and surgical steps of arthroscopic treatment of cartilage lesions with microfracture and BST-CarGel.


