Abstract
Massive rotator cuff tears defying primary repair have been treated with debridement, arthroscopic subacromial decompression, partial repair, muscle-tendon transfer, and joint prosthesis, among other techniques. However, the treatment results have not been satisfactory compared with those of small- to medium-sized rotator cuff tears; each procedure has its merits and demerits, and currently, there is no single established method. For massive rotator cuff tears defying primary repair, the arthroscopic patch graft procedure has been reported as an effective surgical procedure, and this procedure is chosen as the first-line treatment in our department. In this procedure, suture anchors are generally used to fix the patch graft to the footprint on the side of the greater tuberosity. However, tendon-to-bone healing is frequently difficult to achieve, and bone-to-bone healing seems more advantageous for the repair of the rotator cuff attachment site. To improve the results of treatment, a new patch graft procedure was developed, in which the iliotibial ligament with bone was collected at Gerdy's tubercle and the bone was anchored to the footprint on the side of the greater tuberosity. With this procedure, excellent results were obtained, although only short-term results are available at present. The technique and its results so far are reported.
Despite the development of instruments and techniques in arthroscopic surgery, reconstruction of massive rotator cuff tears continues to be a challenge, with a high retear rate.1,2 Strengthening with a patch graft in such cases is an effective reconstructive procedure that can be expected to produce biological and biomechanical improvements. Recently, the use of several types of biological patches has been reported—for instance, swine small intestinal mucous membrane (Restore Implant; DePuy, Warsaw, IN), human skin (GraftJacket; Wright Medical Technology, Arlington, TN), bovine skin (Tissue Mend; TEI Biosciences, Boston, MA),3 and autologous fascia lata femoris. With these tissues, however, healing at the attachment site on the greater tuberosity of the rotator cuff might be difficult to achieve. To achieve bone-to-bone healing at the rotator cuff attachment site, the iliotibial ligament with bone as a patch graft was develoed as an alternative procedure. With the use of this patch, we believe that the purposes of patch strengthening could be achieved, including (1) increasing early strength, (2) providing a bridge for cellular ingrowth to improve the biological environment, and (3) not inducing a foreign-body reaction, thereby not interfering with the healing process.
Our objective is to report the operative technique and describe the results of treatment because excellent short-term results are now available. The technique is demonstrated in Video 1.
Surgical Technique
The patient underwent arthroscopy under general anesthesia in the beach-chair lateral-traction position. A secondary lesion in the scapulohumeral joint, if detected, was treated simultaneously. The treatment involved mostly synovectomy and debridement of the degenerated acetabular labrum and biceps tendon. Then, the rotator cuff stump was dissected thoroughly by use of bursoscopy. Subsequently, the stump was held with a grasper and pulled out toward the greater tuberosity to determine whether repair should be performed. If primary repair was judged impossible, patch grafting was performed as follows:
-
1.
If there were tears in the subscapularis and infraspinatus tendons, these tears were first repaired. At this stage, the defect was of the superior facet only (partial repair).
-
2.
The internal-external and anterior-posterior sizes of the torn area that remained after partial repair were determined.
-
3.
Four Prolene sutures (Ethicon, Somerville, NJ) were placed in the stump of the remaining cuff. The suture that emerged from the subacromial bursa was retrieved through the Neviaser portal, and the suture that emerged from the scapulohumeral side was retrieved through the anterior portal and taken out of the body. These were the relay sutures for introducing the graft ligament into the joint space.
-
4.
The iliotibial ligament with bone was collected based on the size determined in step 2 (Fig 1). Because the ligament would be doubled over later, twice the length of the internal-external size of the ligament plus bone was collected. The width of the collected ligament was usually 1.5 cm, and the size of bone was usually 1.5 cm (anterior-posterior) × 1.0 cm (internal-external) because the anterior-posterior length of the superior facet is approximately 1.5 cm (Fig 2). The same size of Neoveil (Gunze Ltd, Kyoto, Japan) was then sutured to the defect left after collection of the ligament and bone.
-
5.
The graft was formed. Three strong sutures were placed in the fascial graft. These sutures were later used for mattress suturing of the fascial graft to the remaining cuff. Four Prolene sutures were placed around the border between the bone and the ligament. We did so to pass the fascial graft by relaying the suture anchor within the graft when the bone would be fixed to the side of the greater tuberosity by the suture-bridge technique.
-
6.
The graft was introduced into the joint with the Prolene sutures mentioned in step 3 as the relay sutures. Placement of a 1.5-cm-diameter cannula at the anterolateral portal was convenient for graft introduction. After placement of a 1.5 cm diameter cannula at the anterolateral portal, we retrieve the Prolene sutures collected on the anterior portal out of the cannula. The strong sutures that passed through the patch were then tied with Prolene sutures outside the body for relaying. To introduce the graft, while the Prolene sutures retrieved through the Neviaser portal were pulled, the bone was held with a clamp and the graft was pushed with it (Fig 3).
-
7.
The strong sutures were retrieved from the anterolateral portal, and the graft and the remaining cuff were stitched together with a mattress suture.
-
8.
The anchor portal was connected with the anterolateral portal to render the site mini-open. The cortical bone was shaved at the footprint on the side of the greater tuberosity (superior facet) until it fit the size of the bone, and it was taken out of the cancellous bone.
-
9.
The bone was fixed by the suture-bridge technique with 2 Healix sutures (DePuy Mitek, Raynham, MA) on the inside and 2 Versalok sutures (DePuy Mitek) on the outside (Fig 4).
Fig 1.
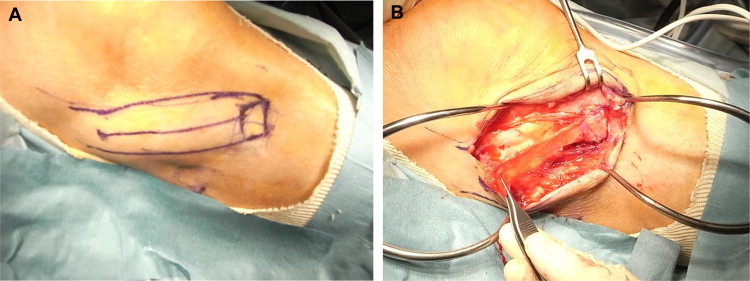
(A) Skin incision from Gerdy's tubercle to center along iliotibial ligament. (B) Collection of iliotibial ligament with bone at Gerdy's tubercle.
Fig 2.
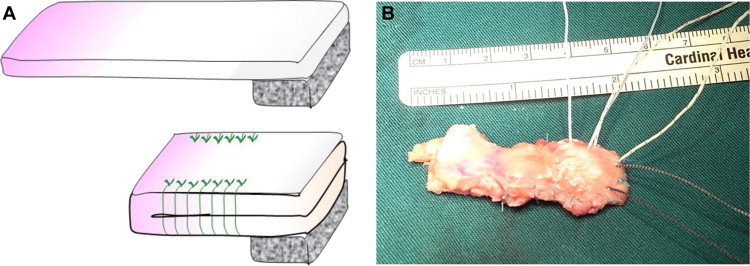
Formation of patch graft. (A) The iliotibial ligament is doubled over so that it will overlap the bone. (B) Passage of sutures (FiberWire; Arthrex, Naples, FL) through the formed graft is performed in advance.
Fig 3.
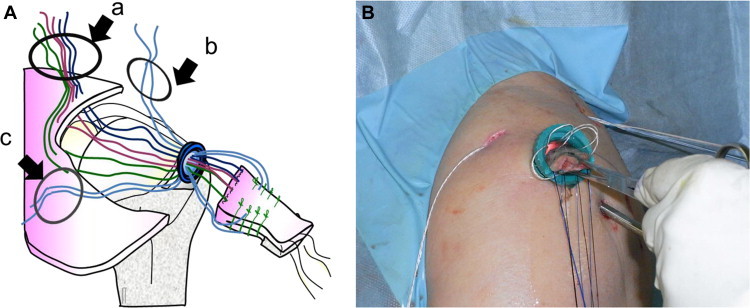
Introduction of patch graft into joint cavity (beach-chair position, right side, with lateral portal used as viewing portal). (A) Neviaser portal (a), anterior portal (b), and posterior portal (c). (B) Introduction of graft into joint through cannula.
Fig 4.
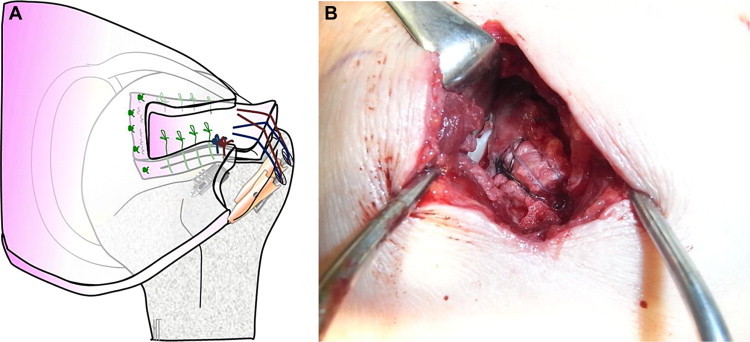
The graft is fixed by the suture-bridge technique with 2 Healix sutures on the inside and 2 Versalok sutures on the outside. (A) Schema. (B) Intraoperative image.
We have devised certain equipment and tools to use for the surgical procedure. One device is a larger-than-usual cannula (diameter, 1.5 cm) that we use when inserting a graft. This is used with a thoracoscope and is extremely convenient when inserting a bone-attached graft inside the joint. Another is trick, when inducing a graft to inside the joint, I hold the graft's bone part by pinching it with an Allis forceps. This prevents the graft from turning upside-down inside the joint and entangling the thread.
The surgical procedure had been performed by the described technique in 10 patients at the time of this report. All cases had massive tears. In all cases surgery was performed because severe pain or limited range of motion persisted with conservative treatment. The mean postoperative follow-up period was 5.5 months (range, 2 to 9 months). The clinical course of 4 patients, in whom at least 6 months had elapsed after surgery, is reported in this article. Pain improved remarkably in all the cases. The flexion range of motion was 170° or greater at 6 months postoperatively in all 4 cases. The postoperative external rotation angle was less than 30° in 2 cases; the preoperative external rotation angle in these 2 cases was less than 5°. In all 4 cases with a postoperative follow-up period of at least 6 months, bone-to-bone healing of the graft and the greater tuberosity area of the cuff was confirmed by computed tomography (Fig 5C). Good cuff integrity was detected by magnetic resonance imaging (Fig 5A and B). No problems occurred at the site of ligament-bone collection.
Fig 5.
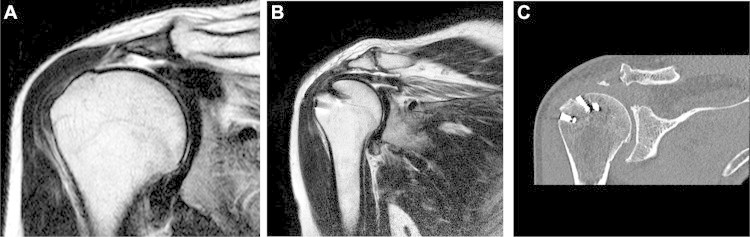
(A) Preoperative magnetic resonance imaging scan (coronal view) showing rotator cuff tear. (B) Postoperative magnetic resonance imaging scan (coronal view) showing continuity of rotator cuff, graft, and bone. (C) On the postoperative computed tomography scan, healing of the bone of the graft and the greater tuberosity is confirmed.
Discussion
Primary repair of massive rotator cuff repairs is difficult, and there is no decisive method available. Various procedures have been proposed.3,4 An arthroscopic patch graft was used as the treatment of first choice. With a patch graft, the joint cavity can be closed without applying excessive tension to the stump. Moreover, improvement of abductor muscle strength can be expected from reconstruction of the rotator cable. The materials reported so far for patch grafts include artificial materials, such as Teflon and polyglycolic acid sheet, and biological materials, such as fascia lata femoris and iliotibial ligament. Use of swine small intestinal mucous membrane, human skin, and bovine skin has been reported overseas.3 Relatively good short-term results have been obtained with all of these materials. However, long-term results are unclear, and there is no consensus on the best patch graft. We previously used fascia lata femoris as a patch graft but encountered difficulty associated with tendon-to-bone healing because of postoperative recurrence of tears at the footprint on the side of the greater tuberosity. Thus, considering the good results obtained by fixing bone fragments of the fracture of the greater tuberosity using the suture-bridge technique,5 we started using the new patch graft reported in this article. The advantages of this technique are as follows: (1) There is no risk of rejection or other adverse reactions because an autograft is used. (2) Because the bone is attached to the graft (iliotibial ligament), even more anatomically appropriate and solid cuff reconstruction can be expected to be performed in the footprint of the rotator cuff, through bone-to-bone healing. (3) When the graft (bone part) is anchored to the footprint, the suture-bridge technique is used; however, because the bone is crimped to the bone, we can expect to see even more solid initial fixation compared with the ordinary method of crimping the soft tissue to the bone.6 (4) When conducting mattress suturing of the graft to the residual rotator cuff, the graft comes beneath the residual rotator cuff, providing a large working space for subsequent procedures. This is also believed to be a method that may lead to reconstruction of the joint capsule.
The risks (disadvantages), on the other hand, include surgical scars remaining around the knee due to collection of the iliotibial ligament. However, none of the patients have had sequelae, such as pain at the site or other symptoms, for extended periods.
Excellent results were obtained in the short period of 6 postoperative months, although the number of cases was limited. Computed tomography showed bone healing on the side of the greater tuberosity, and magnetic resonance imaging confirmed good repair of the rotator cuff. We therefore believe that we can expect good long-term results with the described procedure. Long-term follow-up with more cases is necessary.
Acknowledgment
The authors are grateful to Drs. T. Hirooka and T. Fujita for their valuable advice concerning the design of this study.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique video.
References
- 1.Lafosse L., Brozska R., Toussaint B., Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. doi: 10.2106/JBJS.F.00305. [DOI] [PubMed] [Google Scholar]
- 2.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Labbé M.R. Arthroscopic technique for patch augmentation of rotator cuff repairs. Arthroscopy. 2006;22:1136.e1–1136.e6. doi: 10.1016/j.arthro.2006.03.022. Available at www.arthroscopyjournal.org. [DOI] [PubMed] [Google Scholar]
- 4.Gerber C., Maquieria G., Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am. 2006;88:113–120. doi: 10.2106/JBJS.E.00282. [DOI] [PubMed] [Google Scholar]
- 5.Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Arthroscopic fixation for displaced greater tuberosity fracture using the suture-bridge technique. Arthroscopy. 2008;24:120.e1–120.e3. doi: 10.1016/j.arthro.2007.05.003. Available at www.arthroscopyjournal.org. [DOI] [PubMed] [Google Scholar]
- 6.Neyton L., Godenèche A., Nové-Josserand L., Carrillon Y., Cléchet J., Hardy M.B. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: Healing rate and retear pattern. Arthroscopy. 2013;29:10–17. doi: 10.1016/j.arthro.2012.06.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique video.


