Abstract
Given the extreme focus on perceived physical defects in body dysmorphic disorder (BDD), we expected that perceptual and cognitive biases related to physical appearance would be associated with BDD symptomology. To examine these hypotheses, participants (N = 70) high and low in BDD symptoms completed tasks assessing visual perception and cognition. As expected, there were significant group differences in self-, but not other-, relevant cognitive biases. Perceptual bias results were mixed, with some evidence indicating that individuals high (versus low) in BDD symptoms literally see themselves in a less positive light. Further, individuals high in BDD symptoms failed to demonstrate a normative self-enhancement bias. Overall, this research points to the importance of assessing both cognitive and perceptual biases associated with BDD symptoms, and suggests that visual perception may be influenced by non-visual factors.
Keywords: body dysmorphic disorder, perception, interpretation, cognitive bias, self-enhancement
“Beauty in things exists merely in the mind which contemplates them.”
– David Hume
People with body dysmorphic disorder (BDD) are excessively preoccupied with imagined or slight flaws in their physical appearance (e.g., the color or condition of their skin), and often experience debilitating feelings of shame (Phillips, 1986). To date, one of the most puzzling aspects of the disorder is why individuals with BDD experience such extreme distress regarding perceived physical defects in spite of a normal appearance. The current study uses an analogue sample to investigate this phenomenon by examining whether individuals who are high (versus low) in symptoms of BDD actually see themselves differently at a perceptual level, in addition to experiencing biases in cognition (e.g., interpretation biases). Further, we expand upon past research by examining whether cognitive biases are specific to evaluation of oneself or if they extend to the evaluation of others.
Cognitive Bias in BDD
Cognitive models of BDD predict that individuals “interpret normal visual input, such as minor flaws, in a biased way that results in further negative mental, emotional, and behavioral consequences” (Wilhelm & Neziroglu, 2002, p. 210). Research also suggests that among individuals with BDD, physical appearance values are often central to one’s identity, leading to a tendency to overestimate the importance of being attractive (Veale, Boocock, et al., 1996). Further, Buhlmann and colleagues (2002) demonstrated that relative to healthy participants, BDD patients exhibited an interpretive bias whereby they endorsed negative, appearance-related interpretations for ambiguous scenarios. Consistent with this finding, we expect individuals high (versus low) in BDD symptoms to make more negative interpretations about their appearance when confronted with ambiguous situations. Our hypotheses regarding other-relevant interpretations are more exploratory. However, one relevant study found that BDD patients misidentified emotional expressions as being ‘contemptuous’ only when imagining themselves (and not a friend) in a situation with someone displaying a given facial expression (Buhlmann, Etcoff, & Wilhelm, 2006). Following this, we expect no significant group differences in other-relevant interpretations.
Perceptual Bias in BDD
While we suspect that biased cognition plays a large role in maintaining BDD symptoms, there are many reasons to expect biased visual perception as well. Veale (2004), for example, suggests that self-focused attention and mental imagery lead to an enhanced awareness of specific features among individuals with BDD. In support of this theory, patients with BDD tended to focus on small details instead of first drawing more global features of a complex figure (Deckersbach et al., 2000). Moreover, individuals with BDD rate their facial photographs as significantly less attractive than do independent evaluators (Buhlmann, Etcoff, & Wilhelm, in press). Although these studies do not represent ‘pure’ measures of visual perception (distinct from cognitive processes), they provide hints that symptoms of BDD may literally result in a visual distortion.
Meanwhile, other evidence suggests that perceptual processing may be different for persons with BDD symptoms, but not necessarily biased. Individuals on a wait-list for cosmetic rhinoplasty made more accurate size estimations about their nose than did healthy control participants (Jerome, 1992). Given the relatively high percentage of BDD patients found within cosmetic surgery populations, this study provides insight into the perceptual processes that may be related to negative body image. Furthermore, researchers recently demonstrated that healthy persons may have a self-enhancement bias regarding their appearance (Epley & Whitchurch, submitted). In this study, participants saw versions of their faces that were morphed to be either more or less attractive. Healthy participants, particularly those higher in implicit self-esteem, typically judged the positively altered versions of the morphed images to be their actual face. Given the recent finding that individuals with BDD (versus healthy control participants) are relatively lower in implicit self-esteem (Buhlmann, Teachman, Gerbershagen, Kikul, & Rief, in press), this morphing study has interesting implications for the current study. Indeed, we expect that individuals high in BDD symptoms will not exhibit the same kind of normative self-enhancement bias seen among healthier individuals.
However, the question of whether visual perception can be influenced by non-visual factors (such as BDD symptoms) is a contentious issue. On the one hand, many visual scientists believe that vision is a modular process that is unaltered by outside factors (Pylyshyn, 2003). Yet, there are compelling reasons to believe that visual perception may involve non-visual influences. For example, past research indicates that expectations, intent, and effort all play a role in visual perception (Proffitt, 2006). Simply carrying a heavy backpack, for instance, makes a hill appear steeper. Proffitt theorizes that perception is affected not only by sensory input, but also by the costs associated with performing a given action. Thus, when metabolic costs increase, it makes sense that the hill would appear steeper. More directly tied to the clinical field, a recent study demonstrated that individuals high in height fear literally saw a balcony as higher than individuals low in height fear (Teachman, Stefanucci, Clerkin, Cody, & Proffitt, submitted). Drawing from this evidence that non-optical factors influence visual perception, we hypothesize that biases in perception likely play a role in differentiating individuals with and without symptoms of BDD.
Examining this hypothesis is methodologically challenging, however, given the lack of precedent for measuring visual perception tied to BDD symptoms. Further, the full body measurements typically used in other areas of body image disturbance (e.g., eating disorders) are not helpful for BDD research because more than 90% of perceived defects in BDD involve facial or head features (Phillips, McElroy, Keck, Pope, & Hudson, 1993). Finally, it is difficult to measure ‘pure’ perception related to one’s appearance. To address these issues, our perceptual tasks sought to capture what participants truly saw when looking at their features, distinct from their interpretations. For instance, participants completed the perceptual tasks while viewing their photograph to minimize recall biases. Additionally, to diminish the influence of cognitive biases, the perceptual tasks were not heavily dependent upon verbal report.
Method
Participants
Undergraduate students (N=70 for final sample; 32 women) participated in the study for course credit or payment. We recruited participants based on responses to three items from the Body Dysmorphic Disorder Questionnaire (BDDQ; Phillips, 1986), which was administered as part of a pre-screening battery for psychology students. To recruit for the high BDD symptom group, individuals who indicated that they were very concerned and preoccupied with some part(s) of their body (unrelated to weight concerns) were invited to participate. To recruit for the low BDD group, individuals expressing that they were not very concerned with some part(s) of their body were invited to participate.
To ensure accurate group assignment, an additional item from the State-Self Esteem Appearance Subscale (SSES-Appearance; Heatherton & Polivy, 1991) was used to confirm group allocation during the testing session. Participants were asked to respond to the statement: “I am pleased with my appearance right now,” on a 1 (not at all) to 5 (extremely) scale. Participants recruited for the high group, but who answered 4 or 5 on this item, were excluded because it was clear they were not consistently reporting body image concerns. Similarly, participants recruited for the low group, but who answered 1 or 2 on this item, were excluded. There were 21 participants (8 low, 13 high) excluded as a consequence of this extra screening. The final sample for the high BDD group (N=32, 47% female) had a mean age of 18.53 (SD=68), and race or ethnicity was reported as 94% Caucasian and 6% Biracial. Among individuals high in BDD symptoms, 63% indicated skin concerns, 50% facial feature concerns, 28% hair concerns, and 25% ‘other’ body concerns. The final sample for the low BDD group (N=38, 45% female) had a mean age of 18.21 (SD=.74), and race or ethnicity was reported as 92% Caucasian and 8% Biracial.1
Materials2
BDD Symptoms
The Body Dysmorphic Disorder Questionnaire (BDDQ; Phillips, 1986) is a self-report screening measure that assesses whether BDD may be present but does not give a definitive diagnosis.
The Body Dysmorphic Disorder - Yale-Brown Obsessive Compulsive Scale (BDD-YBOCS; Phillips, Hollander, Rasmussen, Aronowitz, Decaria, & Goodman, 1997) is the most widely used measure assessing the severity of BDD symptoms. In the present study, participants completed the BDD-YBOCS, modified for administration in a self-report format. Specifically, we eliminated the item assessing degree of insight since this would be difficult for participants to self-report, leaving 11 items (Cronbach’s alpha in the current sample was .88).
The State Self-Esteem Scale: Appearance subscale (SSES; Heatherton & Polivy, 1991) is a 6-item subscale of the SSES, and provides information about appearance self-esteem. It was used to confirm group assignment (Cronbach’s alpha was .80).
Cognitive and Perceptual Biases
Cognitive Bias
The Interpretations Questionnaire-modified (IQ-modified; adapted from Buhlmann et al., 2002) assesses the interpretations people make in everyday situations. Two versions of the questionnaire, counterbalanced across participants, were created. In the 11 self-relevant scenarios, participants read a short description of an ambiguous situation (e.g., “Two people are whispering and laughing behind you. You cannot hear them”), followed by the question: “What thoughts occur to you?” They then rated the likelihood of three thoughts coming to mind, including one related to body-image concerns (“They are making fun of how I look”) on a scale from 0 (very unlikely) to 4 (very likely). In the 11 other-relevant scenarios, participants read a comparable ambiguous situation about a friend, and then rated the likelihood of three thoughts coming to their friend’s mind. Half of these scenarios asked participants to imagine a male friend, and half a female friend. For all scenarios, the two non-negative thought options reflected neutral or positive interpretations and were not necessarily related to appearance.
Perceptual Bias
The Morphing Task (MT; modified from Rapien & Epley, 2005) required participants to examine morphed versions of their face. To make realistic morphs, we first made an oval image of each face that was devoid of hair or ears. Next, ‘attractive’ versions of each face were created by morphing the participant’s original photograph with a normed attractive composite picture (ACP; Braun, Gruendl, Marberger, & Scherber, 2001). ‘Unattractive’ versions of each participant’s face were created by morphing the participant’s original photograph with an unattractive composite picture (UCP; the UCPs were selected based on unattractiveness ratings collected through pilot testing).
The ACP and UCP were each blended in 8% increments with the participant’s actual photograph (e.g., 92% the participant’s actual photograph:8% the Attractive Composite). This resulted in one original photograph and 10 morphed photographs, ranging from ‘40% attractive:60% actual’ to ‘60% actual:40% unattractive’. During the first part of the task (Morph-Array), participants viewed an array with all 11 photographs (original, five ‘attractive’ and five ‘unattractive’ morphs), which were randomly arranged in three rows. Participants were asked to pick out which picture the experimenter had taken earlier in the session. Next, participants saw the same 11 faces individually (Morph-Likelihood), and indicated the likelihood on a 0 (extremely unlikely) to 100 (extremely likely) scale that each picture was their actual photograph. There were two versions of the Morphing Task to help account for order effects.
Throughout the Morphing Task, all participants had a mirror to inform their decisions. Notably, our procedure differed from Epley and Whitchurch (submitted), where participants did not have access to a mirror and completed the Morphing Task several weeks after their photograph was taken. Inclusion of the mirror was deemed important to access on-line perceptual bias, rather than recall bias.
Procedure
Participants’ photographs were taken at the outset of the study (no participants refused). Participants then completed the SSES, followed by the IQ-modified, the Morphing Task, and a question assessing perceptions of their physical attractiveness based on their photograph. The BDD-YBOCS (modified) was placed at the end of the study so participants would not be aware that the study was about BDD symptoms. Finally, independent evaluators rated the overall attractiveness of same-gendered participants’ original photographs to ensure that there were not objective differences in appearance across the groups.3
Results
Sample Characteristics
Independent samples t-tests indicated that the BDD groups differed on appearance self-esteem and BDD symptom measures in the expected direction (SSES–Appearance: t68=6.17, p<.001, d=1.47; BDD-YBOCS (modified): t68=4.50, p<.001, d=1.08). The high BDD group reported lower appearance self-esteem (M=19.03, SD=3.02) and greater BDD symptoms (M=15.47, SD=5.11) than the low BDD group (SSES-Appearance: M=23.26, SD=2.72; BDD-YBOCS (modified): M=9.74, SD=5.48). Chi-square tests revealed that there were no significant gender (χ2=.03, p >.10) or ethnicity (χ2=.07, p >.10) group differences.
Group Differences in Cognition: Interpretations Questionnaire-modified
Two dependent variables were calculated by taking an average of the ratings for the negative appearance interpretations made within the relevant scenario category (Self or Other). A repeated measures multivariate analysis of variance (MANOVA) was then conducted with one between-subjects factor (BDD group: high, low) and one within-subjects factor (target of interpretation: Self, Other). Results indicated that there was a nonsignificant trend for Group (F(1, 68)=3.88, p=.053, ηp2=.05) and target of interpretation (F(1,68)=3.67, p=.06, ηp2=.05).
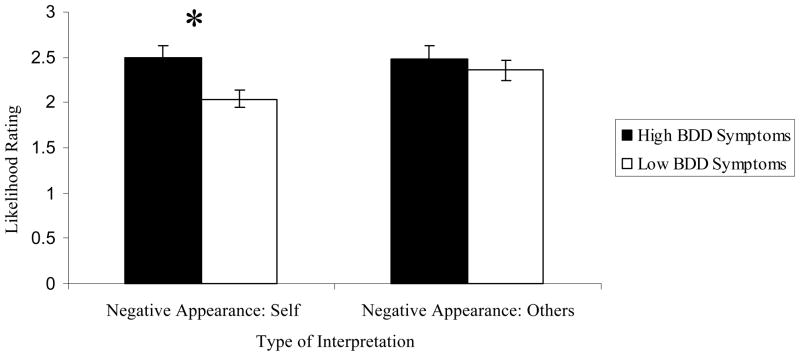
Of particular importance for the current study, results indicated that there was a significant interaction between BDD group and target of interpretation (F(1, 68)=4.02, p=.049, ηp2=.06). As expected, participants who were high (versus low) in BDD symptoms were more likely to make negative appearance-related interpretations in the self-relevant scenarios (Self: t68=2.81, p=.007, d=.67). Additionally, there were no significant between-group differences in Other interpretations (t68=.75, p>.10, d=.18). Within-group analyses indicated that the low BDD group rated negative appearance-related interpretations as more likely in Other- than in the Self-relevant scenarios (t37=3.01, p=.005, d=.49). There was no significant difference in the likelihood of negative appearance-related interpretations between the Self versus Other scenarios among individuals in the high BDD group (t31=.06, p>.01, d=.01; see Figure 1).
Figure 1.
Group differences in cognitive bias: Interpretations Questionnaire-modified
Note. Group mean (and SE bars) for item-level negative appearance interpretations on the Interpretations Questionnaire-modified. Higher scores indicate more negative interpretations.
Group Differences in Visual Perception: Morphing Task
Morph-Array
A dependent variable reflecting degree of morph selected (from 40% more negative to 40% more positive) was created. Contrary to expectations, when asked to select their actual image from the array of photographs, there was no significant group difference in the degree of morphed attractiveness of the image that was chosen (t63=.13, p>.10, d=.03).
Morph-Likelihood
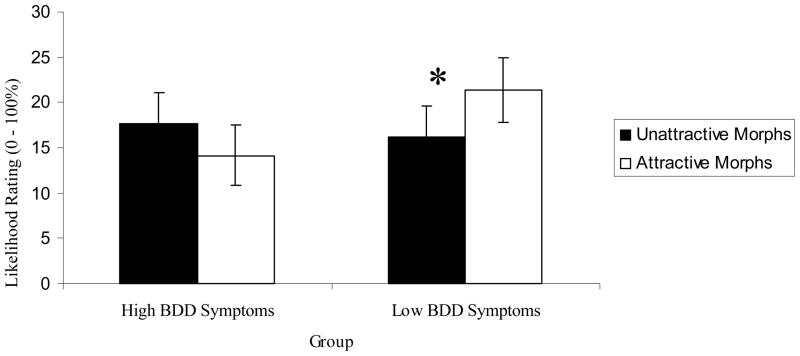
Three dependent variables were calculated: Extreme Attractive (Average of likelihood ratings for 32% and 40% ‘attractive’ photographs), Extreme Unattractive (Average of likelihood ratings for 32% and 40% ‘unattractive’ photographs), and Nearly Accurate (Likelihood rating for 24% Unattractive through 24% Attractive). We then conducted a MANOVA, which included one between-subjects factor (BDD group) and one within-subjects factor (Photograph Type: Extreme Attractive, Extreme Unattractive, and Nearly Accurate). Results indicated that there was not a significant main effect for group (F(1, 62)=.28, p>.10, ηp2=.004), but there was a non-significant trend for the interaction between group and Photograph Type (F(2, 61)=2.66, p=.08, ηp2=.08). Regardless of group, likelihood ratings for the participants’ Nearly Accurate photographs were significantly higher than for their Extreme Attractive (p<.001) and Extreme Unattractive (p<.001) photographs. Of particular importance, paired sample t-tests indicated that individuals in the low BDD group made higher likelihood ratings for the positively (versus negatively) altered images (t34 =2.31, p=.03, d=.26), replicating the normative self-enhancement bias (Epley & Whitchurch, submitted). Although means were in the expected direction (higher ratings for the negatively altered images), there was no significant difference between Extreme Attractive versus Extreme Unattractive likelihood ratings among individuals in the high BDD group (t29=1.11, p>.10, d=.19; see Figure 2).
Figure 2.
Group differences in perceptual bias: Morphing Task-Likelihood
Note. Group mean (and SE bars) for likelihood ratings of whether the morphed images were their actual photograph. Higher scores indicate higher likelihood ratings.
Independent Evaluator Ratings of Attractiveness
As anticipated, independent evaluators did not rate the BDD groups differently on overall attractiveness level (t56=0.07, p>.10, d=.02). Additionally, individuals in the low BDD group rated their overall attractiveness level as significantly more attractive than did the independent evaluators, again supporting a normative self-enhancement bias (t32=4.72, p<.001, d=1.13), and there was no significant difference between overall attractiveness ratings made by independent evaluators and ratings made by members of the high BDD group (t23=1.18, p >.10, d=.37).
Discussion
We hypothesized that both perceptual and cognitive biases would be associated with BDD symptomology. Results were largely in line with hypotheses for cognitive biases, but were mixed for perceptual biases. Further, ratings by independent evaluators verified that group differences across tasks could not be attributed to an actual discrepancy between groups in physical appearance.
Similar to Buhlmann et al. (2002), we found that when confronted with ambiguous self-relevant scenarios, individuals high (versus low) in BDD symptoms endorsed more negative appearance-related thoughts. Given our use of an analogue sample, it is unclear whether similar processes will be relevant for patients with BDD. However, we speculate that this type of biased interpretation may partially explain why individuals with BDD experience such extreme dissatisfaction with their objectively normal appearance. Anyone who regularly has negative appearance-related thoughts would presumably begin to experience shame about themselves and their bodies. This group difference is also consistent with cognitive models that suggest individuals with BDD ‘overvalue’ physical appearance (Wilhelm & Neziroglu, 2002; Veale, 2004).
Interestingly, we found that individuals high in BDD symptoms did not interpret all situations as more threatening than those low in BDD symptoms. There were no significant between-group differences in the degree of negative, appearance-related thoughts participants believed others would endorse in an ambiguous situation. However, within-group analyses indicated that while people low in BDD symptoms made fewer negative interpretations about themselves relative to others, individuals high in BDD symptoms were equally likely to believe others would have a negative thought tied to their appearance as they were. This finding indicates that people low in BDD symptoms may have a self-protective belief system (similar to a self-enhancement bias) where they are able to make healthier interpretations about themselves relative to a stranger.
Analogously, our task primarily assessing visual perception lends partial support to the idea that people with BDD symptoms do not have a normative self-enhancement bias. Consistent with our predictions, when shown each image in isolation on the Morphing Task, individuals low in BDD symptoms were more likely to believe that positively (versus negatively) altered photographs were their actual image; meanwhile, individuals high in BDD symptoms did not display this self-enhancement bias. According to Epley and Whitchurch (submitted), this type of bias is most commonly associated with implicit processes. Given that individuals with BDD have relatively lower implicit self-esteem (Buhlmann et al., in press), it is unsurprising that individuals high in BDD symptoms did not self-enhance. Also supporting a group difference in self-enhancement, individuals in the low BDD symptom group rated their overall attractiveness level as significantly more attractive than did independent evaluators; meanwhile, there was no significant difference in overall attractiveness ratings made by independent evaluators versus members of the high BDD group.
In spite of these provocative findings, there was no meaningful group difference in participants’ ability to select their actual image from an array of morphed photographs. Unlike Epley and Whitchurch (submitted), the majority of participants in the current study were able to accurately identify their image from the array (as opposed to selecting a positively altered photograph). At this stage, we can only speculate about why we failed to find a group difference. One explanation is that at a purely perceptual level, there might not be significant group differences between people with and without symptoms of BDD. However, this explanation is unsatisfactory for a number of reasons. First, it does not account for findings on the Morph-Likelihood task, where individuals low in BDD symptoms displayed a self-enhancement bias. While this task involved elements of verbal report, it seems unlikely that the group differences were solely the result of cognition. Second, our perceptual task was a blunt measure in that it did not directly assess specific areas of concern (e.g., shape of chin). The faces were not altered to exaggerate (or de-emphasize) specific disliked features. Thus, it could be that there exists a perceptual bias among individuals with BDD symptoms, but that it is very focused on specific body parts (as opposed to a more global facial perceptual deficit).
Finally, Proffitt (2006) theorizes that non-visual factors should affect visual perception primarily when one feels that he or she may incur costs when acting in the environment. Visual perception, he writes, “promotes survival by making us aware of both the opportunities and costs associated with action” (p. 111). Accordingly, visual perception related to BDD symptoms may be particularly affected by appearance-based fears of rejection in social contexts. Theoretically, if one believes that appearance-based rejection is a likely outcome, it is adaptive to be particularly discerning about how one appears. Given that individuals with BDD report extreme fears of negative evaluation tied to their appearance (Phillips, 1986), it seems plausible that this fear might literally fuel a more negative perception of one’s physical features. In short, we speculate that a bias in visual perception would be heightened if individuals with BDD symptoms believed they were interacting in a social environment and focused more specifically on their perceived ‘deficits’ (versus on their whole face).
Limitations and Conclusions
The present results must be interpreted in light of several limitations. We did not use a diagnosed sample of individuals with BDD, so it is unclear the extent to which these findings will generalize to a clinical sample. Moreover, we did not assess depressive symptoms or mood directly following the tasks4, and we lacked a measure of perception that tapped the heterogeneity of BDD concerns. Finally, the quality of some of the morphed images varied, and we were limited to using Caucasian morphs, meaning important questions about cultural and ethnic differences in evaluations of attractiveness could not be explored.
Despite these limitations, this study provides insight into the puzzling question of how individuals with BDD symptoms could feel such shame and preoccupation regarding their physical features, in spite of a normal appearance. The pattern for cognitive bias is clear – individuals with symptoms of BDD interpret information in a biased appearance-centric way, which presumably contributes to their appearance dissatisfaction. Meanwhile, our perceptual tasks provide some evidence that individuals with BDD symptoms do not demonstrate the same type of visual self-enhancement bias found among healthier individuals. Ultimately, the relationship between BDD symptoms and biases in cognition and perception is complicated, but both appear integral to understand how individuals with BDD concerns view themselves and the surrounding world.
Acknowledgments
The authors would like to thank Dennis R. Proffitt and members of the Program for Anxiety Cognition & Treatment (PACT) Lab for their helpful feedback. For research assistance, thanks to: Irina Bocarnea, Alden Gaertner, Erin Horn, Elizabeth Schottinger, and Jessica Zinder. Finally, this research was supported in part by the University of Virginia Raven Fellowship to Elise Clerkin, and an NIH RO1MH075781-01A2 grant to Bethany Teachman.
Footnotes
We were only able to create morphed versions of Caucasian faces, so only Caucasian individuals were invited to participate. However, due to an error in recruitment, 5 participants (3 low BDD, 2 high BDD) reported they were biracial. These participants are included in all analyses other than those specific to the Morphing Task. Additionally, one participant withdrew from the study.
Only those materials relevant to the current hypotheses are listed here. For a more complete listing, please contact the first author.
Two participants in the Low Group and 5 from the High Group refused to allow their pictures to be rated by the independent evaluators. Five additional participants were not rated due to experimenter or participant error.
As noted by one anonymous reviewer, the mirror exposure during the Morphing Task may have resulted in greater distress for the high BDD group, potentially influencing their responses. Future research should directly investigate the impact of mood on perception.
References
- Braun C, Gruendl M, Marberger C, Scherber C. Beautycheck - Ursachen und Folgen von Attraktivitaet. Report. [pdf-document] 2001 Available from: http://www.beautycheck.de/english/bericht/bericht.htm.
- Buhlmann U, Etcoff N, Wilhelm S. Facial attractiveness ratings and perfectionism in body dysmorphic disorder and obsessive compulsive disorder. Journal of Anxiety Disorders. doi: 10.1016/j.janxdis.2007.05.004. in press. [DOI] [PubMed] [Google Scholar]
- Buhlmann U, Etcoff N, Wilhelm S. Emotion recognition bias for contempt and anger in body dysmorphic disorder. Journal of Psychiatric Research. 2006;40:105–111. doi: 10.1016/j.jpsychires.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Buhlmann U, Teachman B, Gerbershagen A, Kikul J, Rief W. Implicit and explicit self-esteem and attractiveness beliefs among individuals with body dysmorphic disorder. Cognitive Therapy and Research in press. [Google Scholar]
- Buhlmann U, Wilhelm S, McNally R, Tuschen-Caffier B, Baer L, Jenike M. Interpretive biases for ambiguous information in body dysmorphic disorder. CNS Spectrums. 2002;7:435–443. doi: 10.1017/s1092852900017946. [DOI] [PubMed] [Google Scholar]
- Deckersbach T, Savage C, Phillips K, Wilhelm S, Buhlmann U, Rauch S, et al. Characteristics of memory dysfunction in body dysmorphic disorder. Journal of International Neuropsychological Society. 2000;6:673–681. doi: 10.1017/s1355617700666055. [DOI] [PubMed] [Google Scholar]
- Epley N, Whitchurch E. Mirror, mirror on the wall: Perceptual Self-enhancement in self-recognition. doi: 10.1177/0146167208318601. submitted. [DOI] [PubMed] [Google Scholar]
- Heatherton T, Polivy J. Development and validation of a scale for measuring state self-esteem. Journal of Personality and Social Psychology. 1991;60:895–910. [Google Scholar]
- Jerome L. Body dysmorphic disroder: A controlled study of patients requesting cosmetic rhinoplaty. American Journal of Psychiatry. 1992;149:577–578. doi: 10.1176/ajp.149.4.577. [letter] [DOI] [PubMed] [Google Scholar]
- Phillips KA. The broken mirror: Understanding and treating body dysmorphic disorder. Oxford: University Press; 1986. [Google Scholar]
- Phillips K, Hollander E, Rasmussen S, Aronowitz B, Decaria C, Goodman W. A severity rating scale for body dysmorphic disorder: Development, reliability and validity of a modified version of the Yale-Brown Obsessive-Compulsive Scale. Psychopharmacology Bulletin. 1997;33:17–22. [PubMed] [Google Scholar]
- Phillips K, McElroy S, Keck P, Pope H, Hudson S. Body dysmorphic disorder: 30 cases of imagined ugliness. American Journal of Psychiatry. 1993;150:302–308. doi: 10.1176/ajp.150.2.302. [DOI] [PubMed] [Google Scholar]
- Proffitt DR. Embodied perception and the economy of action. Perspectives on Psychological Science. 2006;1:110–122. doi: 10.1111/j.1745-6916.2006.00008.x. [DOI] [PubMed] [Google Scholar]
- Pylyshyn Z. Seeing and visualizing: It’s not what you think. Cambridge, MA: MIT Press; 2003. [Google Scholar]
- Teachman BA, Stefanucci JK, Clerkin EM, Cody MW, Proffitt DR. New modes of fear expression: Perceptual and implicit association biases in height fear. doi: 10.1037/1528-3542.8.2.296. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veale D. Advances in a cognitive-behavioural model of body dysmorphic disorder. Body Image. 2004;1:113–125. doi: 10.1016/S1740-1445(03)00009-3. [DOI] [PubMed] [Google Scholar]
- Veale D, Boockcok A, Gournay K, Dryden W, Shah F, Wilson R, et al. Body dysmorphic disorder—A survey of 50 cases. British Journal of Psychiatry. 1996;169:196–201. doi: 10.1192/bjp.169.2.196. [DOI] [PubMed] [Google Scholar]
- Wilhelm S, Neziroglu F. Cognitive Theory of Body Dysmorphic Disorder. In: Frost R, Steketee G, editors. Cognitive Approaches to Obsessions and Compulsions—Theory, Assessment, and Treatment. Oxford: Elsevier Science Ltd; 2002. pp. 203–214. [Google Scholar]