ABSTRACT
Purpose: To examine discharge planning of patients in general internal medicine units in Ontario acute-care hospitals from the perspective of physiotherapists. Methods: A cross-sectional study using an online questionnaire was sent to participants in November 2011. Respondents' demographic characteristics and ranking of factors were analyzed using descriptive statistics; t-tests were performed to determine between-group differences (based on demographic characteristics). Responses to open-ended questions were coded to identify themes. Results: Mobility status was identified as the key factor in determining discharge readiness; other factors included the availability of social support and community resources. While inter-professional communication was identified as important, processes were often informal. Discharge policies, timely availability of other discharge options, and pressure for early discharge were identified as affecting discharge planning. Respondents also noted a lack of training in discharge planning; accounts of ethical dilemmas experienced by respondents supported these themes. Conclusions: Physiotherapists consider many factors beyond the patient's physical function during the discharge planning process. The improvement of team communication and resource allocation should be considered to deal with the realities of discharge planning.
Key Words: discharge planning, internal medicine, survey
RÉSUMÉ
Objectif : Étudier la préparation du départ des patients dans les unités de médecine interne générale des hôpitaux de soins actifs de l'Ontario du point de vue des physiothérapeutes. Méthodes : Une étude transversale portant sur l'utilisation d'un questionnaire en ligne a été envoyée aux participants en novembre 2011. Les caractéristiques démographiques des répondants et le classement des facteurs ont été analysés par statistique descriptive et l'on a procédé à des tests-t pour déterminer les différences entre groupes (compte tenu des caractéristiques démographiques). On a codé les réponses aux questions ouvertes de façon à dégager des thèmes. Résultats : La mobilité était considérée comme le principal facteur de la détermination de la préparation au départ. Les autres facteurs ont inclus la disponibilité des moyens de soutien social et des ressources communautaires. La communication entre les professions a été jugée importante, mais les processus étaient souvent informels. Les politiques sur le départ, la disponibilité au moment opportun d'autres options sur le plan du départ et les pressions exercées en faveur du départ hâtif ont une incidence sur la planification du départ. Les répondants ont aussi signalé un manque de formation en planification des départs et des anecdotes portant sur les dilemmes éthiques vécus par les répondants ont appuyé ces thèmes. Conclusions : Les physiothérapeutes tiennent compte de nombreux facteurs en plus de la fonction physique du patient au cours du processus de planification du départ. Il faudrait envisager d'améliorer la communication et la répartition des ressources au sein de l'équipe pour faire face aux réalités de la planification des départs.
Mots clés : Physiothérapeute, physiothérapie, planification des départs, départ des patients, médecine interne
Ontario's health care system is under pressure to meet service demands along the continuum of care from initial hospitalization to the transition back into the community or to an alternative care setting. Many changes to the structure of the system have been made in recent years to manage this pressure. One example of such a change is the development of Local Health Integration Networks (LHINs).1 These networks' mandate is to address fragmentation of health service delivery, determine the health services priorities in distinct geographic regions, and create an integrated model of health care with the goal of “providing the right care in the right place at the right time.”2(p.7) In Ontario, Community Care Access Centres (CCACs) are integral components of LHINs and provide support services to help people continue to live at home.3 Demands on our health care system will continue to escalate as a result of the unprecedented increase in the aging population, which includes many people with multiple co-morbidities, and the number of people requiring health services. In 2011, an estimated 5 million Canadians were 65 years or older, and this number is expected to double in the next 25 years.4 In Ontario in 2009, people aged 65 and older represented only 13% of the population but accounted for almost 60% of total hospital patient days.5 The rising demand for hospital resources and the need to ensure available capacity has led to an increased emphasis on formalized discharge planning.
Hospital discharge planning is a complex process requiring inter-professional team collaboration.6,7 To be effective, this process must not only prepare the patient for discharge from the hospital but, more importantly, must assess the patient's ability to function outside of the hospital setting. This necessitates the identification and coordination of supports required to allow patients to return to safe community living. Health care professionals in hospitals are responsible for providing services to patients to meet their acute-care needs, optimizing their function, and supporting them with community services as they return home after their acute-care stay.
Physiotherapists' role in acute care is well described in the document “Essential Competency Profile for Physiotherapists in Canada”:
Physiotherapists are primary health care practitioners who consult and collaborate with clients and others to provide quality client-centred services. Physiotherapists contribute to keeping people productive throughout their lives by maximizing function and improving quality of life … Physiotherapists practice both independently and as part of inter-professional teams along the health system continuum from primary to tertiary care.8(p.5)
Physiotherapists play an important role in the inter-professional team by making appropriate discharge recommendations and integrating multiple factors into the planning process. Jette and colleagues found that physiotherapists consider a patient's physical status, goals and wants, ability to participate in care, and life context when making a discharge recommendation.6 It has been suggested that when a physiotherapist's discharge recommendations are not implemented, patients are more likely to be readmitted to acute care within a short period.9 If a patient's level of functioning at the time of discharge is too discrepant from their pre-hospitalization level, and external supports are not available or put in place, then the patient may be at risk of physical injury, psychosocial harm, and further decline or failure to thrive, which could lead to readmission and further stress on the overall health care system. The purpose of the current study, therefore, was to examine the discharge planning experience from the perspective of physiotherapists working in general internal medicine (GIM) units in Ontario teaching hospitals. Results from the study may be used in creating strategies to improve discharge experiences for patients and health professionals.
Methods
We conducted a cross-sectional survey of physiotherapists using a self-administered electronic questionnaire sent to participants in November 2011.
Participants
A total of 19 eligible organizations were identified from the membership of the Council of Academic Hospitals of Ontario and the University of Toronto's Academic Practice Leaders group. Physiotherapists were recruited if they were currently practising in (1) acute-care GIM teaching hospitals (academic or community), (2) facilities with >100 in-patient beds, and (3) adult care. Physiotherapists working in pediatrics, non-acute care (e.g., rehabilitation), non-teaching hospitals, or hospitals with <100 beds were excluded.
Questionnaire development and distribution
We developed an electronic questionnaire based on a review of the literature and the clinical expertise of the research team. Prior to distribution, we pilot-tested the questionnaire for face and content validity with six physiotherapists working in GIM units at the research site who met the inclusion criteria and were not part of the research team. These pilot-testers independently evaluated the questionnaire for content, wording, clarity, comprehensiveness, response choices, and balance of open- and closed-ended questions. We then met face-to-face with each tester to understand any concerns and to discuss suggestions for improvement. Suggested revisions were incorporated before we administered the questionnaire to the study sample. For the purposes of this study, we defined discharge planning as “the process by which health care providers in an acute-care facility plan a destination and date for patients to move from acute care to another setting.”
The self-administered online questionnaire was created using the web-based SurveyMonkey software platform. The questionnaire consisted of 31 closed-ended and six open-ended questions divided into nine sections: (1) subject and practice demographics, (2) the discharge planning process, (3) importance and ranking of factors in the discharge process, (4) satisfaction with the process, (5) internal and (6) external factors affecting discharge, (7) practice issues, (8) ethical considerations, and (9) respondent experiences and recommendations to improve the process.
To gain an overall understanding of the discharge process, we asked respondents about the primary method of coordinating discharge at their hospital, which health professionals were involved, and the use of discharge risk-assessment tools. The closed-ended questions asked respondents to rank the importance of and their satisfaction with internal factors such as team communication, family communication, team collaboration, role awareness, and timing of referrals, along with internal and external factors in the process such as organization discharge policies and inadequate community supports. Most of the closed-ended questions included an open-text box where participants could provide additional comments or further information about their response choices. The open-ended questions asked respondents to comment on discharge planning training in their curricula, examples of ethical dilemmas they had experienced with discharge planning, and their recommendations (opportunities for improving the process). The questionnaire took about 20 minutes to complete.
We recruited participants by sending email messages to all eligible Physiotherapy Practice Leaders (PLs) or Managers who had physiotherapists working in GIM units. The PLs' contact emails were obtained from the University of Toronto's Academic Practice Leaders distribution list. Our initial letter of invitation asked PLs to introduce the study to physiotherapist colleagues in their organization who worked within GIM. A separate letter of information for these potential participants was included, which detailed the purpose of the study, the study design, and confidentiality and provided a link to the survey. We asked PLs to reply to the email, giving only the number of physiotherapists (no names or contact details) who had received the questionnaire so as to maintain confidentiality while tracking response rates. We sent follow-up emails to the PLs with a request to forward a reminder letter to eligible physiotherapists at 2 weeks and 4 weeks after the initial email. Participants could complete the questionnaire over the course of several sessions. We did not seek written informed consent, as participants who returned completed questionnaires were deemed to have provided implied consent. No financial or other incentives were offered for participation in the study. The study was approved by the University Health Network's Research Ethics Committee and complied with its guidelines.
Data analysis
Of the 81 physiotherapists who met the inclusion criteria, we received responses from 55; of these, only 39 were fully completed questionnaires (48% response rate). Responses were exported from SurveyMonkey into the Statistical Package for the Social Sciences, version 16 (SPSS Inc., Chicago, IL) for subsequent data management. We excluded the 16 partially completed questionnaires from the final analysis. Descriptive statistics were used to characterize the whole sample with respect to demographics. To determine the impact of demographic characteristics on discharge practices, we divided respondents into groups by practice type (academic teaching vs. community teaching facilities), geographic location (within vs. outside Toronto), and unit characteristics (bed size; number of GIM units). Between groups comparisons were made using t-tests (p≤0.05).
Responses to open-ended questions were read multiple times by each member of the research team independently to gain an overall understanding of the data. We thoroughly examined the entire data set and then coded the data into smaller meaningful parts to identify themes. A consensus exercise was used for verification and agreement on common themes.
Results
Demographics for the whole group, practice type, geographic location, and unit characteristics are shown in Table 1. The most common conditions/reasons for referrals to physiotherapy were falls (94.9%), failure to cope (89.7%), and cardiorespiratory conditions (69.2%). Respondents indicated that the main factors leading to readmissions after discharge were premature discharge (patient discharged with unresolved health issues), discharge to an inappropriate or less than ideal destination, and inadequate support in the community for patients and their families (including lack of access or long wait times for services).
Table 1.
Participant and Practice Demographics
| Practice type |
Geographic location |
No. of GIM beds |
No. of GIM units |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Group | Academic | Community | Within GTA | Outside GTA | ≥45 | ≤44 | ≥4 | ≤4 |
| Sex, % (no.) | |||||||||
| F | 93.9 (46) | 100.0 (21) | 88.9 (16) | 96.3 (26) | 87.5 (7) | 90.0 (10) | 96.3 (26) | 100.0 (13) | 90.9 (20) |
| M | 6.1 (3) | 0.0 (0) | 11.1 (2) | 3.7 (1) | 12.5 (1) | 9.1 (1) | 3.7 (1) | 0.0 (0) | 9.1 (2) |
| Age, y | |||||||||
| Mean (SD) | 38.7 (9.3) | 35.0 (8.4)* | 42.7 (7.6)† | 39.8 (0.0) | 36.4 (11.2) | 35.3 (10.1) | 40.1 (8.2) | 36.1 (10.1) | 40.0 (0.6) |
| Range | 24–60 | 24–52 | 30–60 | 24–60 | 24–50 | (24–50) | (24–60) | (24–55) | (24–60) |
| Mean (SD) time in acute care, y | 11.3 (9.0) | 8.7 (7.7) | 13.5 (0.8) | 11.9 (10.1) | 10.3 (10.7) | 10.1 (9.8) | 11.2 (7.5) | 7.7 (6.7) | 13.0 (8.7) |
| Organizational management structure, % (no.) | |||||||||
| Program | 53.8 (21) | 57.1 (12) | 50.0 (9) | 47.1 (8) | 62.5 (5) | 72.7 (8) | 48.1 (13) | 69.2 (9) | 50.0 (11) |
| Functional | 28.2 (11) | 23.8 (5) | 33.3 (6) | 29.4 (5) | 37.5 (3) | 18.2 (2) | 33.3 (9) | 23.1 (3) | 36.4 (8) |
| Mixed/Matrix | 17.9 (7) | 19.0 (4) | 16.7 (3) | 23.5 (4) | 0.0 (0) | 9.1 (1) | 18.5 (5) | 7.7 (1) | 13.6 (3) |
| Highest clinically relevant education, % (no.) | |||||||||
| Baccalaureate | 53.1 (26) | 47.6 (10) | 82.4 (14) | 52.0 (13) | 50.0 (4) | 45.5 (5) | 70.4 (19) | 46.2 (6) | 72.7 (16) |
| Masters | 34.7 (17) | 47.6 (10) | 17.6 (3) | 44.0 (11) | 50.0 (4) | 54.5 (6) | 25.9 (7) | 53.8 (7) | 27.3 (6) |
| Doctoral | 2.0 (1) | 4.8 (1) | 0.0 (0) | 4.0 (1) | 0.0 (0) | 0.0 (0) | 3.7 (1) | 0.0 (0) | 0.0 (0) |
| Practice type, % (no.) | |||||||||
| Academic | 21.0 | 100.0 (21) | 0.0 (0) | 52.4 (11) | 47.6 (10) | 81.8 (9) | 40.7 (11) | 53.8 (7) | 50.0 (11) |
| Community | 18.0 | 0.0 (0) | 100.0 (18) | 94.4 (17) | 5.6 (1) | 18.2 (2) | 59.3 (16) | 46.2 (6) | 50.0 (11) |
| Geographic location, % (no.) | |||||||||
| Within GTA | 71.8 (28) | 52.4 (11) | 94.4 (17) | — | — | 50.0 (4) | 25.0 (4) | 25.0 (2) | 57.1 (8) |
| Outside GTA | 28.2 (11) | 47.6 (10) | 5.6 (1) | — | — | 50.0 (4) | 75.0 (12) | 75.0 (6) | 42.9 (6) |
| Characteristics of GIM unit and workload measures per day, mean (SD) | |||||||||
| No. of beds | 46.4 (28.0) | 50.6 (28.7) | 41.9 (28.9) | 42.9 (20.2) | 61.6 (41.3) | 82.5 (30.6) | 31.8 (6.6) | 47.2 (36.3) | 47.5 (26.0) |
| No. of GIM units | 3.9 (2.1) | 3.3 (1.2) | 4.4 (2.7) | 3.6 (1.3) | 4.3 (3.3) | 3.9 (2.8) | 3.9 (1.7) | 5.8 (2.4) | 2.8 (0.5) |
| No. of assessments | 3.5 (1.3) | 3.7 (1.3) | 3.3 (1.2) | 3.5 (1.5) | 3.4 (1.5) | 4.1 (1.4) | 3.3 (1.2) | 2.7 (0.9) | 3.9 (1.2) |
| No. of treatments | 8.4 (4.1) | 7.4 (3.8) | 9.7 (4.1)‡ | 8.4 (3.9) | 8.1 (5.6) | 8.8 (5.1) | 8.1 (3.7) | 7.5 (4.2) | 9.2 (4.1) |
| No. of discharges | 2.2 (0.8) | 2.2 (0.8) | 2.1 (0.9) | 2.3 (0.8) | 2.0 (1.2) | 2.6 (0.9) | 2.0 (0.8) | 2.2 (0.8) | 2.2 (0.8) |
Between-group differences p≤0.05 are shown in bold.
p=0.036.
p=0.001.
GTA=Greater Toronto Area; GIM=General Internal Medicine.
The discharge planning process
The majority of respondents (≥79%) reported that the primary method of coordinating discharge planning was verbal communication, most frequently during daily rounds (89.7%), or informal “on the fly” conversations (79.5%). Less frequently, discharge planning included written electronic communication (33.3%) or occurred via telephone referral (12.8%).
According to respondents, all health professionals play a role in discharge planning, but the most common representatives were physiotherapists, occupational therapists, social workers, physicians, “charge” nurses, and CCAC representatives.
Discharge risk-assessment tools were almost never used for discharge planning; instead, the majority of respondents reported that hospital policies or processes guided discharge planning. For example, respondents reported that patients are designated for an Alternate Level of Care (ALC) when deemed medically stable (97.3%), that discharge planning begins on the day of admission (67.6%), CCAC timeline referral policies (62.2%), and that the estimated discharge date (EDD) is determined as soon as the patient is stable (56.8%).
Factors involved in discharge
Regardless of practice type, setting, or unit characteristics, physiotherapists' top patient-related considerations in discharge decision making were mobility, discharge destination, and family supports. Availability of CCAC supports and patient cognition were identified as additional considerations.
Of the five institutional or clinical factors identified as playing a role in discharge planning, communication between members of the inter-professional team was ranked as most important, while awareness of other team members' roles was ranked as least important. Respondents identified the same factors in the same order of importance regardless of practice setting, albeit with a smaller percentage of community-based physiotherapists choosing these factors.
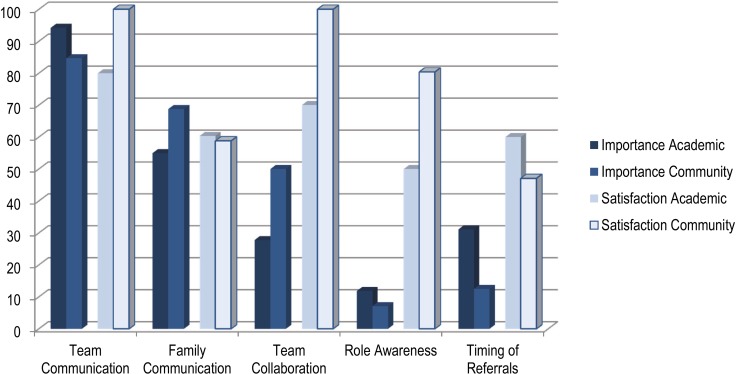
The majority of respondents reported being very or somewhat satisfied with role awareness, collaboration between the inter-professional team, and timing of referrals in their facility, although there was less satisfaction in academic than in community teaching facilities. Satisfaction rankings also tended to be higher than the importance ascribed to these same factors (see Figure 1).
Figure 1.
The importance of and satisfaction with the “most important” and “somewhat important” discharge factors.
Internal factors
The majority of respondents reported sometimes (73.0%) or very often (13.5%) facing pressure to decrease in-patient length of stay (LOS) despite the physiotherapists' assessment that a patient was not ready or faced potential safety risks if discharged. The respondents' impression was that pressure to discharge comes most often from the physician/medical team and less frequently from the flow/discharge coordinator or nursing team. Only sometimes did respondents feel that by the time of discharge, patients have returned to their previous level of function or that discharge is determined by the physiotherapist. Respondents always or frequently felt that their discharge recommendations were supported by the team, that discharge destinations were closely aligned with physiotherapy recommendations, and that discharge was aimed at decreasing LOS. We found no significant differences between academic and community hospitals with respect to these factors (see Table 2 for details).
Table 2.
Frequency of Occurrence of Events Regarding Discharge Planning
| Academic, % (No.)* |
Community, % (No.)* |
|||
|---|---|---|---|---|
| Discharge… | Always+Frequently | Sometimes | Always+Frequently | Sometimes |
| is driven by the aim of decreasing LOS | 80.0 (16) | 15.0 (3) | 87.2 (15) | 11.8 (2) |
| recommendations by physiotherapists are team-supported | 95.0 (19) | 5.0 (1) | 100.0 (17) | 0.0 (0) |
| destinations are aligned with PT recommendations | 95.0 (19) | 5.0 (1) | 82.3 (14) | 17.6 (3) |
| communications to patient/family are timely | 65.0 (13) | 35.0 (7) | 88.3 (15) | 11.8 (2) |
| is driven by the health care team | 45.0 (9) | 50.0 (10) | 64.7 (11) | 35.3 (6) |
| is determined by the Physiotherapist | 70.0 (14) | 25.0 (5) | 58.9 (10) | 41.2 (7) |
| patient status has returned to baseline | 35.0 (7) | 25.0 (5) | 47.1 (8) | 47.1 (8) |
Percentage (number) of respondents who ranked the frequency of occurrence for each statement as “always,” “frequently,” or “sometimes.” Percentages may not add up to 100%, as data for the “rarely” and “never” categories are not shown.
LOS=length of stay.
Respondents identified organizational processes, practices, or policies such as system-based pressure; patients' and families' lack of awareness about discharge planning policies or processes; and the timing of referrals as the biggest internal barriers to effective discharge from a GIM unit. Other reported barriers were the lack of communication or collaboration between team members and discharge risks not being clearly identified at admission.
External factors
The greatest external barriers to effective discharge from a GIM unit were identified as a lack of resources, including the availability of long-term care (LTC) or rehabilitation beds; overall lack of CCAC support for physiotherapy follow-up; and unrealistic patient or family expectations of the availability and type of post-discharge support.
Role of CCACs in discharge planning
The main roles that respondents ascribed to CCACs in discharge planning were determining the location of care provision after discharge, assessing patient requirements, coordinating necessary post-discharge services/equipment, and establishing and maintaining a communication strategy between the health care team and patients and their families.
The majority (61.1%) of respondents reported that CCACs communicate post-discharge plans to the physiotherapist or inter-professional team before the patient's discharge. In general, while respondents were very (4.5%) or somewhat satisfied (50.0%) with the overall support that CCACs provide to patients and their families after discharge, 18.2% were somewhat or very dissatisfied with this support. In addition, almost half (45.5%) were somewhat or very dissatisfied with the PT follow-up from CCACs.
Ideal discharge planning
Respondents described the ideal discharge planning process as requiring a highly functional team that uses inter-professional collaborative practice and effective communication strategies to ensure that the patient is safe and ready to be discharged to the appropriate destination and as not driven primarily by hospital process or policy. The team must also work in partnership with patients and their families to ensure their awareness and understanding of the discharge plan and date. In the ideal process, all services and required equipment would be arranged before discharge, and the patient and family would receive sufficient education to feel prepared and confident. One respondent described this experience as an example of an ideal discharge plan:
“Full team collaboration … regarding discharge plans and all CCAC services were in place. Family was provided with the vendor list for equipment rentals and picked up the equipment before [the] patient was discharged. Patient's family didn't have to wait for prescriptions/discharge forms to be complete as they were prepared the day before. Family came in the morning to pick [the] patient up and left the hospital within 10 min of arrival.”
Professional concerns:
More than three-quarters of respondents reported experiencing ethical dilemmas or concerns that resulted in dissatisfaction with the discharge planning process. Four main themes emerged:
-
(1)Disrespect: Physiotherapists felt disrespected when their recommendations were not taken into consideration for discharge planning:When I come into work and patients I considered unsafe are gone—makes me feel as if my role is unimportant and not considered by the team.A patient lived alone in an area of the GTA where there was a wait list for CCAC services. She needed a bit more practice on the stairs before being safe for discharge; however, due to hospital pressure to find inpatient beds for ER admissions, and even though the team was aware of the physiotherapist's reservations and concerns for patient safety at home, the patient was discharged anyway.
-
(2)Disagreement: Respondents perceived a lack of agreement within the team or between the team and patients and their families regarding recommendations:Medical team wanting to discharge patients who, while medically ready, are not mobility, cognitively, and/or socially ready.Making recommendations for discharge (i.e., rehab) at the request of the family when it is not indicated.
-
(3)Destination: Physiotherapists reported situations in which patients are discharged to an inappropriate location or that no ideal discharge destination exists:Family insists on a discharge destination that is not the best option or unrealistic for patient.Patient will benefit from rehab to improve function but is declined by rehab because final discharge destination is long-term care facilities.
-
(4)Resource challenges: Respondents reported that discharge may occur even when resources are not adequate to meet patient needs once discharged or when families may not be able to advocate effectively for resources:Sometimes you know the CCAC services will not be adequate enough to support these patients, who really should be going for LTC placement for optimal safety and care.Oftentimes we have patients waiting for rehab. We are able to increase their function while in hospital and then they go home, oftentimes due to the pressure of the hospital because they are an ambulatory patient. It is not satisfying because if these patients were to have gone to rehab they would likely had more strength, endurance, and balance to manage more safely at home and would have been close to their baseline level of function.
Physiotherapy curriculum and training
Over 85% of respondents felt somewhat unprepared (44.4%) or not at all prepared (41.7%) by their physiotherapy educational program to participate in the realities of discharge planning. All respondents indicated that their experience, training, and instruction occurred during clinical placements, not classroom training. As one respondent noted, even in the practical setting, this training was not always realistic:
Lessons were not practical-based and only focused on the “ideal safe discharge,” and not all discharges are 100% PT safe by the book. Some people are discharged “at risk.” Clinical placements are not always a lot of experience and patients are typically the more straightforward patients.
Discussion
While our sample size was small, it included representation from both academic and community teaching hospitals and from smaller and larger GIM units. For the most part, we found no demographic differences between these subsets. For these reasons, we are confident that our findings are representative of physiotherapists' discharge experiences.
Of particular interest is our finding that respondents performed at least twice as many treatments as assessments per day. In contrast, other studies have identified the role of rehabilitation professionals in acute-care environments as being primarily to assess and plan for discharge.10–13 Patients are known to experience significant functional decline during hospitalization14–16; the pressure to decrease LOS reduces the amount of treatment time available to help improve patient mobility and overall functional status before discharge. It has been suggested17 that positive benefits derived from increased time invested in the treatment of older adults include improved recovery, increased likelihood of returning to baseline function, decreased hospital readmissions, and reduced hospital costs. Therefore, both the discharge planning process and physiotherapists' involvement should begin early after admission to help to maintain functional ability. Physiotherapists in community hospitals spent longer time in treatment activities than those in academic hospitals. While we do not know the reason for this, we postulate that the structure of the work day, activities, and expectations may be different in different practice settings. For example, physiotherapists in academic hospitals may be more involved in teaching and research activities, leaving less time for participation in direct patient-care activities. In our sample, community-based physiotherapists were older and had more clinical experience than their younger colleagues in academic centres, which may translate into more efficient time management allowing for more treatment time.
Respondents, regardless of experience or practice location, identified similar practice issues in discharge planning. We were not surprised to find that mobility status was ranked as the most important factor in discharge planning, given a physiotherapist's role in assessing and treating physical function and mobility.8 Masley and colleagues18 found that the major concerns for physiotherapists in the acute-care setting were patient mobility and safety, with the goal of determining an optimal plan of care and finding an appropriate discharge setting. Also not unexpected was the finding that discharge destination, available supports, knowledge of the patient's living situation, and requirements for mobilization were identified as important.7 Other important findings from the current study were that discharge planning begins on the day of admission and that the primary method for coordinating discharge planning is via verbal communication, most frequently during daily rounds. These findings are consistent with established discharge planning models, such as the Transitional Care Model (TCM)19 and the Acute Care for the Elderly (ACE) model,20 that focus on early intervention by an interdisciplinary team, including physiotherapists, for a comprehensive and effective discharge from acute care. These models demonstrate that improved recovery, increased likelihood of patients' functional status returning to baseline function, and decreased hospital readmissions and costs can be achieved through comprehensive planning and teamwork.
The impact of internal and external factors
The most important internal factor affecting discharge planning, according to respondents, is facility-specific discharge policies. Almost all respondents recognized physiotherapists' key role in discharge planning, but not in setting the actual discharge date, which they saw as primarily driven by hospital policies. For example, the EDD policy outlines the importance of minimizing LOS and is often used upon admission to establish the discharge date. Implementation of such policies was perceived to exert pressure on the team to determine a discharge destination and date regardless of physiotherapists' perception of patient readiness. External barriers such as lack of optimal post-discharge supports or destinations also increase this pressure.
The role of the CCAC
Overall, respondents had a thorough and realistic understanding of the role of the CCAC in agreement with that described by the Ministry of Health and Long-Term Care (MOHLTC) website.3 Respondents valued the CCAC's important role in partnering and collaborating with other key health sector stakeholders to address, meet, or enhance service needs of patients in the community.
Inter-professional collaboration and communication
Our finding that eight or more health professionals are involved in the discharge planning process indicates that, in agreement with earlier studies,7,21–23 inter-professional collaboration and communication are essential components of this planning. However, the informal nature of communication and the lack of clarity and timeliness, especially with patients and their families, were highlighted as concerns. Deliberate attention and future efforts need to rely less on informal or serendipitous interactions that occur outside of established team meetings, where not all team members have the opportunity to be involved in or aware of the latest discussion. An example may be typified by spontaneous conversations such as “glad I caught you, can we discuss Mr. M and our plan?” Improved team communication is essential, particularly concerning timeliness of referrals and patients' functional status, to ensure that everyone is working toward the same functional goals. Effective (timely, clear, and transparent) communication with patients and their families also plays an essential role in ensuring continuity of care during discharge planning; it is especially important to keep them informed about the patient's status, pending discharge date, and plans.24,25 The most effective communication allows patients and families adequate time and opportunities to ask questions about their discharge and receive answers.25,26 Although our respondents felt that the team listens to their discharge recommendations, these recommendations may not always be put into practice, which decreases physiotherapist satisfaction with the process. We suspect there may also have been a difference in how respondents defined “team”; that is, whether they operationally defined it as the traditional rehabilitation (physiotherapy, occupational therapy, speech-language pathology) team or the full inter-professional team. Respondents may have felt that their rehabilitation colleagues are generally more supportive and in agreement with their recommendations than other team members are.
Ethical dilemmas
Respondents' comments highlight the discrepancies between reality and the expectations of the team and the patient or family,27 which lead to numerous ethical dilemmas resulting in moral distress.
Carpenter28(p.70) has written that “moral distress is associated with individual practitioners' experiences of loss of personal and professional integrity when their desire to maintain professional standards, achieve the best outcomes for clients and act as advocates for clients within complex health care environments cannot be realized.” Respondents' comments recount situations in which the physiotherapist advocated for the patient's needs, but their ideal plan was not put into practice because of barriers such as those identified in the survey. Nalette29 has described the concept of constrained physical therapist practice, in which the physiotherapist understands what the patient needs but may be compelled to provide less than the necessary care because of internal constraints (e.g., not having good communication or advocacy skills) or external constraints (e.g., hospital policy). Physiotherapists therefore need to be mindful of the patient's story, which will help to morally engage their compassion, thus putting into practice a virtue of the physiotherapy profession, which may help to relieve their own moral stress.29 Our findings indicate that, although the external barriers to effective discharge planning are factors that an individual physiotherapist may have little to no control over, our respondents are valued members of the team and know that their efforts are directed toward the best discharge plan for their patient, within the context of their immediate environment.
Blau and colleagues30 also found similar themes of loss of control, stress, and disheartenment among acute-care physiotherapists. A major source of discontent among physiotherapists was not being able to spend the desired amount of time with patients, but they were able to deal with the stress by finding the “silver lining” in their work. Physiotherapists were proud of being professionals and felt they provided excellent patient care. They also valued having good collegial relationships, similar to our finding of high satisfaction with team collaboration.
Physiotherapy curriculum and discharge planning
Physiotherapists involved in training students need to be aware that graduates entering acute-care environments, where discharge planning is a key part of physiotherapy practice, feel underprepared for this responsibility. Not surprisingly, respondents' learning about discharge planning occurred almost exclusively during their practical training. Clinicians must be more cognizant of their responsibility to educate students on the breadth of the physiotherapist's role and provide supervised opportunities to be involved in “messy” and “complicated” discharge planning situations. Enhancing academic curricula to increase experiential learning and provide interactive inter-professional education sessions will give students the opportunity to develop the problem-solving, communication, and advocacy skills they need to be leaders within the team. Curtis and colleagues31 have suggested that clinicians acting as clinical instructors should have better training and should not let students practise in protected environments; instead, clinicians should share their management strategies in the complicated acute-care environment, such as time management and understanding discharge options.
Recommendations to improve discharge planning
Although discharge risk-assessment tools are known to improve the continuity, efficiency, and quality of the discharge planning process,32–34 studies have shown35 that when such tools are used, their results are not consistently used; systemic pressures may overrule implementation of findings. While most respondents in our study did not use discharge risk-assessment tools in their facility, consistently using these tools and basing discharge recommendations on objective data would support evidence-based decision making. One study reported that decreasing LOS was associated with an increased risk of readmission and that increasing staffing levels reduced readmission rates.36 Our respondents strongly advocated for increased structural and personnel resources, such as increased rehabilitation staffing on acute medical units, increased capacity of in-patient and outpatient rehabilitation programs, and increased CCAC services, as ways to improve the discharge process. It is particularly interesting to note that premature discharges and inadequate community supports were seen to overwhelmingly influence readmissions. It has been recommended that older patients with multiple co-morbidities may benefit from a more comprehensive discharge plan that appropriately addresses their individual challenges,37 which could be facilitated by a cohesive team with access to the time and resources to successfully implement it.
Our study has some limitations relating to the convenience sample chosen for the study and the methodology used. The questionnaires were sent only to physiotherapists working in GIM units; thus, our respondents were only a subset of all physiotherapists working in academic and community teaching hospitals in Ontario, and our results may not represent the discharge experiences of all physiotherapists. Further, it is possible that physiotherapists who have had unsatisfactory experiences with discharge planning may be more likely to participate in a study on this topic, resulting in a potential non-response bias. The process we used to distribute the questionnaire (relying on PL's or Managers to distribute the survey to their staff) may have posed practical limitations and affected the study's response rate.
Conclusion
Discharge planning in an acute-care environment is a complex process involving a variety of factors. It requires an understanding of the individuals involved (patients, families, health care team), the environment (supports and resources required for successful transition to the discharge destination), the processes influencing the plan (facility and provincial policies), and how all these factors coordinate.7 The discharge experience is made even more challenging by an aging population that consists of many people who are admitted to hospitals with multiple co-morbidities. Physiotherapists play an integral role within the inter-professional team in ensuring successful discharge planning;.6 In particular, physiotherapists have much to contribute to discharge planning by taking into consideration patients' functional status, mobility, the importance of family or CCAC supports, and patient cognition. As integral team members, physiotherapists support the inter-professional team's clinical decision-making with respect to determining the most appropriate time and destination for patient discharge.9,18
The results of this study correspond well to issues identified by the Ontario Discharge Planning and Alternate Level of Care Policy Task Team.38 These include hospital system issues such as lack of inter-professional communication and collaboration, inadequate community resources, and inadequate patient and family education regarding discharge planning. Their recommendations to improve this process include having a clear discharge policy, timeliness and transparency in inter-professional and patient and family communication, family education, and ongoing support after discharge.24 Shepperd et al.39 indicated a high level of communication between the discharge planning team and the providers of services outside the hospital as being crucial to the process. The Ontario Home and Community Care Council40 identified transition planning as a key quality process influencing discharge planning from acute care to community. It is essential to encourage health providers to communicate with each other across complex organizational boundaries to support this transition.
Findings from our study highlight the essential supportive role physiotherapists play in the discharge planning process and identify the impact of both internal (policy) and external (resources) factors on their expectations and actual experience in discharge planning. Increasing or reallocating staffing resources would allow for more physiotherapy intervention to work toward optimizing patients' functional levels in preparation for the transition from acute care to home. More time for patient and family interaction and education could address the barriers of communication as well. Studies of ACE models have shown that functional decline associated with hospitalization in the elderly and overall costs of hospital stays can be decreased by increasing resources in the acute-care setting.41
Key Messages
What is already known on this topic
Issues in discharge planning include lack of inter-professional communication and collaboration, inadequate community resources, and inadequate patient and family education. Recommendations to improve the discharge process include having a clear discharge policy; timeliness and transparency in inter-professional, patient, and family communication, including communication between hospital staff and service providers in the community; family education; and ongoing support after discharge. It is essential to support and encourage health care providers to communicate with each other across complex organizational boundaries to support patients' transition from acute care to community.
What this study adds
Physiotherapists play a key role in discharge planning by considering multiple factors affecting a patient's return to function after discharge. The gap between physiotherapists' expectations for optimal discharge plans and clinical reality can lead to ethical dilemmas, less than ideal patient discharges, and greater likelihood of readmission. The use of a discharge risk-assessment tool, timely and transparent communication within the team and with patients as partners in care decisions, increasing resource allocation, and enhanced physiotherapy student preparation can provide patients and their families with better discharge plans.
Physiotherapy Canada 2014; 66(3);254–263; doi:10.3138/ptc.2013-12
References
- 1.Ontario's Local Health Integration Networks. What are LHINs? [Internet] The Networks; 2014. [cited 2013 Dec 15]. [updated 2013 Dec 15]. Available from: http://www.lhins.on.ca/aboutlhin.aspx. [Google Scholar]
- 2.Ontario Ministry of Health and Long-Term Care. Ontario's Action Plan for Health Care [Internet] Toronto: The Ministry; 2012. [cited 2013 Dec 14]. [updated 2013 Jan 22]. Available from: http://www.health.gov.on.ca/en/ms/ecfa/healthy_change/docs/rep_healthychange.pdf. [Google Scholar]
- 3.Ontario Ministry of Health and Long-Term Care. Community Care Access Centre client services policy manual. [Internet] Toronto: The Ministry; 2006. [cited 2013 Dec 14]. [updated 2012 Dec 19]. Available from: http://www.health.gov.on.ca/english/providers/pub/manuals/ccac/cspm_sec_1/1-8.html. [Google Scholar]
- 4.Employment and Social Development Canada. Canadians in context—aging population [Internet] ESDC; [cited 2013 Dec 14]. [updated 2013 Dec 14]. Available from: http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=33. [Google Scholar]
- 5.Office of the Auditor General of Ontario. 2010 annual report. Section 3.02: discharge of hospital patients [Internet] Toronto: The Office; 2010. [cited 2013 Dec 14]. [updated 2010] Available from: http://www.auditor.on.ca/en/reports_en/en10/2010ar_en.pdf. [Google Scholar]
- 6.Jette DU, Grover L, Keck CP. A qualitative study of clinical decision making in recommending discharge placement from the acute care setting. Phys Ther. 2003;83(3):224–36. Medline:12620087. [PubMed] [Google Scholar]
- 7.Wong E, Yam C, Cheung A, et al. Barriers to effective discharge planning: a qualitative study investigating the perspectives of frontline healthcare professionals. [cited 2013 Sep 17];BMC Health Serv Res [Internet] 2011 Sep 29;11:242–51. doi: 10.1186/1472-6963-11-242. Available from: http://www.biomedcentral.com/1472-6963/11/242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Physiotherapy Association. Essential competency profile for physiotherapists in Canada October 2009 [Internet] Ottawa: The Association; 2009. [cited 2013 Dec 14]. [updated 2012 Jul 10]. Available from: http://www.physiotherapy.ca/getmedia/fe802921-67a2-4e25-a135-158d2a9c0014/Essential-Competency-Profile-2009_EN.pdf.aspx. [Google Scholar]
- 9.Smith BA, Fields CJ, Fernandez N. Physical therapists make accurate and appropriate discharge recommendations for patients who are acutely ill. Phys Ther. 2010;90(5):693–703. doi: 10.2522/ptj.20090164. http://dx.doi.org/10.2522/ptj.20090164. Medline:20299410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lake A, Quraishi F, Heck CS, et al. The role of occupational therapy in acute care across Canada; Poster session presented at Occupations and Practice through Time: Canadian Association of Occupational Therapists Conference; 2012 June 6–9; Quebec City, QC. [Google Scholar]
- 11.Griffin SD. Occupational therapy practice in acute care neurology and orthopaedics. J Allied Health. 2002;31(1):35–42. Medline:11905392. [PubMed] [Google Scholar]
- 12.Griffin SD, McConnell D. Australian occupational therapy practice in acute care settings. Occup Ther Int. 2001;8(3):184–97. doi: 10.1002/oti.145. http://dx.doi.org/10.1002/oti.145. Medline:11823882. [DOI] [PubMed] [Google Scholar]
- 13.Blaga L, Robertson L. The nature of occupational therapy practice in acute physical care settings. New Zealand Journal of Occupational Therapy. 2008;55(2):11–8. doi: 10.3109/11038128.2012.737369. [DOI] [PubMed] [Google Scholar]
- 14.Courtney MD, Edwards HE, Chang AM, et al. A randomised controlled trial to prevent hospital readmissions and loss of functional ability in high risk older adults: a study protocol. [cited 2013 Sep 17];BMC Health Serv Res [Internet] 2011 Aug 23;23(11):202–8. doi: 10.1186/1472-6963-11-202. Available from: http://www.biomedcentral.com/1472-6963/11/202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buurman BM, Parlevliet JL, van Deelen BA, et al. A randomised clinical trial on a comprehensive geriatric assessment and intensive home follow-up after hospital discharge: the Transitional Care Bridge. [cited 2013 Sep 17];BMC Health Serv Res [Internet] 2010 Oct 29;29(10):296–304. doi: 10.1186/1472-6963-10-296. Available from: http://www.biomedcentral.com/1472-6963/10/296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim SC, Doshi V, Castasus B, et al. Factors causing delay in discharge of elderly patients in an acute care hospital. [cited 2013 Sep 17];Ann Acad Med Singapore [Internet] 2006 Jan 1;35(1):27–32. Available from: http://www.annals.edu.sg/pdf/35VolNo1200601/V35N1p27.pdf. [PubMed] [Google Scholar]
- 17.Eyres L, Unsworth CA. Occupational therapy in acute hospitals: the effectiveness of a pilot program to maintain occupational performance in older clients. Aust Occup Ther J. 2005;52(3):218–24. http://dx.doi.org/10.1111/j.1440-1630.2005.00498.x. [Google Scholar]
- 18.Masley PM, Havrilko CL, Mahnensmith MR, et al. Physical therapist practice in the acute care setting: a qualitative study. Phys Ther. 2011;91(6):906–19. doi: 10.2522/ptj.20100296. http://dx.doi.org/10.2522/ptj.20100296. Medline:21511991. [DOI] [PubMed] [Google Scholar]
- 19.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–20. doi: 10.1001/jama.281.7.613. http://dx.doi.org/10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 20.Covinsky KE, Palmer RM, Kresevic DM, et al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Jt Comm J Qual Improv. 1998;24(2):63–76. doi: 10.1016/s1070-3241(16)30362-5. Medline:9547681. [DOI] [PubMed] [Google Scholar]
- 21.Watts R, Gardner H. Nurses' perceptions of discharge planning. Nurs Health Sci. 2005;7(3):175–83. doi: 10.1111/j.1442-2018.2005.00229.x. http://dx.doi.org/10.1111/j.1442-2018.2005.00229.x. Medline:16083480. [DOI] [PubMed] [Google Scholar]
- 22.Atwal A. Nurses' perceptions of discharge planning in acute health care: a case study in one British teaching hospital. J Adv Nurs. 2002;39(5):450–8. doi: 10.1046/j.1365-2648.2002.02310.x. http://dx.doi.org/10.1046/j.1365-2648.2002.02310.x. Medline:12175354. [DOI] [PubMed] [Google Scholar]
- 23.Calkins DR, Davis RB, Reiley P, et al. Patient–physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan. Arch Intern Med. 1997;157(9):1026–30. http://dx.doi.org/10.1001/archinte.1997.00440300148014. Medline:9140275. [PubMed] [Google Scholar]
- 24.Bauer M, Fitzgerald L, Haesler E, et al. Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence. J Clin Nurs. 2009;18(18):2539–46. doi: 10.1111/j.1365-2702.2008.02685.x. http://dx.doi.org/10.1111/j.1365-2702.2008.02685.x. Medline:19374695. [DOI] [PubMed] [Google Scholar]
- 25.Bull MJ. Patients' and professionals' perceptions of quality in discharge planning. J Nurs Care Qual. 1994;8(2):47–61. doi: 10.1097/00001786-199401000-00009. http://dx.doi.org/10.1097/00001786-199401000-00009. Medline:8312594. [DOI] [PubMed] [Google Scholar]
- 26.Clare J, Hofmeyer A. Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice. Aust J Adv Nurs. 1998;16(1):7–13. Medline:9807277. [PubMed] [Google Scholar]
- 27.Wells DL, Martin DK, Moorhouse A, et al. An integrated model of discharge planning for acutely-ill elderly patients. Can J Nurs Leadersh. 1999;12(3):6–12. doi: 10.12927/cjnl.1999.19079. http://dx.doi.org/10.12927/cjnl.1999.19079. Medline:11094933. [DOI] [PubMed] [Google Scholar]
- 28.Carpenter C. Moral distress in physical therapy practice. Physiother Theory Pract. 2010;26(2):69–78. doi: 10.3109/09593980903387878. [DOI] [PubMed] [Google Scholar]
- 29.Nalette E. Constrained physical therapist practice: an ethical case analysis of recommending discharge placement from the acute care setting. Phys Ther. 2010;90(6):939–52. doi: 10.2522/ptj.20050399. http://dx.doi.org/10.2522/ptj.20050399. Medline:20413578. [DOI] [PubMed] [Google Scholar]
- 30.Blau R, Bolus S, Carolan T, et al. The experience of providing physical therapy in a changing health care environment. Phys Ther. 2002;82(7):648–57. Medline:12088462. [PubMed] [Google Scholar]
- 31.Curtis KA, Martin T. Perceptions of acute care physical therapy practice: issues for physical therapist preparation. Phys Ther. 1993;73(9):581–94, discussion 594–8. doi: 10.1093/ptj/73.9.581. Medline:8356107. [DOI] [PubMed] [Google Scholar]
- 32.Boronowski LE, Shorter CM, Miller WC. Measurement properties of the Occupational Therapy Discharge Needs Screen. Can J Occup Ther. 2012;79(4):248–56. doi: 10.2182/cjot.2012.79.4.6. [DOI] [PubMed] [Google Scholar]
- 33.Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients--development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354–60. doi: 10.1002/jhm.129. http://dx.doi.org/10.1002/jhm.129. Medline:17219528. [DOI] [PubMed] [Google Scholar]
- 34.Slade A, Fear J, Tennant A. Identifying patients at risk of nursing home admission: the Leeds Elderly Assessment Dependency Screening tool (LEADS) [cited 2013 Sep 17];BMC Health Serv Res [Internet] 2006 Mar 13;13(6):31–9. doi: 10.1186/1472-6963-6-31. Available from: http://www.biomedcentral.com/1472-6963/6/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anthony MK, Hudson-Barr DC. Successful patient discharge. A comprehensive model of facilitators and barriers. J Nurs Adm. 1998;28(3):48–55. doi: 10.1097/00005110-199803000-00010. http://dx.doi.org/10.1097/00005110-199803000-00010. Medline:9524550. [DOI] [PubMed] [Google Scholar]
- 36.Heggestad T. Do hospital length of stay and staffing ratio affect elderly patients' risk of readmission? A nation-wide study of Norwegian hospitals. [cited 2013 Sep 17];Health Serv Res [Internet] 2002 Jun;37(3):647–65. doi: 10.1111/1475-6773.00042. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1434663/?report=classic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Preyde M, Chapman T. Psychosocial profile of elderly patients discharged from a community hospital. Soc Work Health Care. 2007;45(2):77–95. doi: 10.1300/J010v45n02_05. http://dx.doi.org/10.1300/J010v45n02_05. Medline:17954444. [DOI] [PubMed] [Google Scholar]
- 38.Discharge Planning and ALC Policy Task Team. Discharge from hospital: literature review [Internet] The Team; 2006. [cited 2013 Sep 17]. [updated 2006 Nov]. Available from: http://www.nelhin.on.ca/uploadedFiles/Public_Community/Report_and_Publications/ALC/Literature_Review_Hospital_Dis.pdf. [Google Scholar]
- 39.Shepperd S, Parkes J, McClaran J, et al. Discharge planning from hospital to home (review) [Internet] The Cochrane Collaboration; 2008. [cited 2013 Sep 17]. Available from: http://hospitalmedicine.ucsf.edu/improve/literature/discharge_committee_literature/preparing_patients_at_discharge/discharge_planning_from_hospital_to_home_shepperd_cochrane_collaboration.pdf. [Google Scholar]
- 40.Vanderbent S. Strategies for transition planning in Ontario's Local Health Integration Networks. Healthc Q. 2005;8(3):78–81. doi: 10.12927/hcq.2005.17158. http://dx.doi.org/10.12927/hcq.2005.17158. [DOI] [PubMed] [Google Scholar]
- 41.Barnes DE, Palmer RM, Kresevic DM, et al. Acute care for elders units produced shorter hospital stays at lower cost while maintaining patients' functional status. Health Aff (Millwood) 2012;31(6):1227–36. doi: 10.1377/hlthaff.2012.0142. http://dx.doi.org/10.1377/hlthaff.2012.0142. Medline:22665834. [DOI] [PMC free article] [PubMed] [Google Scholar]