ABSTRACT
Purpose: To identify physiotherapists' familiarity with and experience using outcome measures (OMs) along the care continuum for patients undergoing total joint arthroplasty (TJA) of the hip and knee. Views on future use and barriers were also captured. Methods: A stratified random sample of physiotherapists in one Canadian province completed a questionnaire about 19 standardized and clinically feasible OMs. Analyses included descriptive statistics and chi-square and McNemar tests to compare use of OMs for clinical decision making and program evaluation. Results: Of 694 physiotherapists surveyed, 298 (43%) responded. Of these, 172 (58%) treated TJA clients and completed the full questionnaire. A majority worked in public practice settings and >1 care phase (e.g., pre-op, acute, rehab). All physiotherapists reported using ≥1 OM and having greater experience using performance-based measures than patient-reported OMs. OMs were used more often for clinical decision making than for program evaluation. Dissatisfaction with available tools was evident from respondents' comments. Several barriers to using OMs were identified in varied clinical settings and care phases. Conclusions: While physiotherapists use a variety of OMs along the TJA continuum, there remain challenges to routine use across clinical settings, care phases, and patient sub-groups.
Key Words: hip arthroplasty, knee arthroplasty, outcome assessment, survey
RÉSUMÉ
Objectif : Déterminer dans quelle mesure les physiothérapeutes savent bien utiliser les mesures des résultats (MR) sur le continuum des soins chez les patients qui subissent une arthroplastie totale (AT) de la hanche et du genou, ainsi que leur expérience en la matière. On a saisi aussi leur opinion sur l'utilisation future et les obstacles. Méthodes : Un échantillon aléatoire stratifié de physiothérapeutes d'une province du Canada a répondu à un questionnaire sur 19 MR normalisées et faisables sur le plan clinique. Les analyses ont inclus des statistiques descriptives et des tests du chi-carré et de McNemar afin de comparer l'utilisation des MR pour la prise de décisions cliniques et l'évaluation de programmes. Résultats : Sur 694 physiothérapeutes sondés, 298 (43%) ont répondu, dont 172 (58%) ont traité des clients qui ont subi une AT et répondu au questionnaire au complet. Une majorité d'entre eux travaillait en pratique publique et dans >1 phase de soins (p. ex., préopératoires, actifs, réadaptation). Tous les physiothérapeutes ont déclaré utiliser ≥1 MR et avoir plus d'expérience des mesures fondées sur le rendement que des MR déclarées par les patients. Les MR étaient utilisées plus souvent dans la prise de décisions cliniques que dans l'évaluation de programmes. Les commentaires des répondants ont révélé leur insatisfaction face aux outils disponibles. On a défini un certain nombre d'obstacles à l'utilisation des MR dans divers contextes cliniques et phases de soins. Conclusions : Les physiothérapeutes utilisent un éventail de MR sur tout le continuum de l'AT, mais il reste des défis à relever sur le plan de l'utilisation de routine entre les contextes cliniques, les phases de soins et les sous-groupes de patients.
Mots clés : Arthroplastie, remplacement, hanche; arthroplastie, remplacement, genou; physiothérapeutes; évaluation des résultats (soins de santé); questionnaire
Osteoarthritis (OA) is a common disease affecting more than 4.4 million (1 in 8) Canadians.1 By age 40, 20% of adults in the province of British Columbia (BC) have physician-diagnosed OA, and this proportion rises to >30% by age 70.2 Increasing proportions of older people with obesity in the population contribute to the increasing prevalence of OA.1,3 OA is the leading cause of long-term disability among Canadians,3 a major contributor to health care utilization,1 and the primary reason for total joint arthroplasty (TJA) surgery.4 Although disease progression can be slowed and activity limitations reduced by pharmacologic and conservative treatment, OA is incurable.5 In end-stage hip and knee disease, elective TJA surgery becomes the recommended treatment.
Physiotherapists play a key role in treating patients throughout the disease continuum, including those who have undergone TJA.6 In BC, more than13,000 hip and knee TJAs are performed4 each year, resulting in reduced pain, improved function, and improved quality of life.7 Physiotherapy is routinely prescribed following TJA to help patients regain mobility, strength, balance, and function6 and can be delivered through outpatient, home-based, and/or in-patient care. Functional recovery can take 2 or more years.8–11
Because several physiotherapists may treat patients along this continuum and in different settings (e.g., outpatient, in-patient, community), appropriate outcome measures (OMs) for use across varied clinical situations are needed to measure change and quantify the effects of physiotherapy. Standardized outcome measurement (consistent application and scoring across providers and settings) could facilitate clinical decision making,12,13 identification of treatment goals,14 monitoring of patient progress,15 and inter-professional and patient communication.16 Routine use of OMs can help physiotherapists identify variations in both quantity and quality of care17 and inform health care policy.18 However, use of OMs for TJA differs widely among therapists and across settings,19 and little guidance is available regarding the best measures to use clinically.20 Recently, the Osteoarthritis Research Society International (OARSI) published recommendations on a core set of performance-based OMs for use in hip and knee OA and TJA based on international consensus.21 Previous efforts to identify OA core sets have focused on important outcomes rather than on OMs22 or use of the core set as a tool in itself.15 Proposed methods to identify TJA-specific core measures have yet to be undertaken.23 Identifying appropriate OMs for the TJA population will benefit clinicians, patients, researchers, decision makers, and third-party payers. To inform the discussion about a core set of OMs, we surveyed physiotherapists who work with the TJA patient population to ask which OMs they have experience using, which OMs they expect to use in the future, and which OMs they recommend.
Physiotherapists have historically used OMs (e.g., range of motion, strength, and pain) within the “body structure and function” domains of the World Health Organization's International Classification of Functioning, Disability and Health (ICF).14,18,24,25 Although important, data based solely on “body function” (impairment) tend to underestimate disability and do not correlate well with “activity and participation.”24 Therefore, OMs that capture “activity and participation” (involvement in a life situation such as work and leisure) are essential to evaluate the full spectrum of functioning.26,27 “Activity and participation” outcomes include patient-reported OMs (PROMs) and performance-based measures, essential to fully capture functional recovery after TJA.28–30 This study represents a step toward identifying standardized OMs for routine clinical use across physiotherapist providers, settings, and care phases.
Our aim was to determine physiotherapists' familiarity with, current experience using, and views on future use of OMs for clinical decision making and program evaluation along the care continuum for hip and knee TJA. A secondary aim was to understand clinical issues and barriers to using OMs in various practice settings and care phases. The care continuum was defined as beginning when a person is diagnosed with moderate or severe OA of the hip or knee and ending with the return to community activity after TJA.
Methods
Our study used a cross-sectional survey design. The cover letter was designed to be a consent form and indicated to participants that by completing and returning the survey, they were consenting to participate. Ethics approval was received from the University of British Columbia Behavioural Research Ethics Board.
Participants and sampling
Participants consisted of physiotherapists registered with the College of Physical Therapists of British Columbia (CPTBC). We identified physiotherapists most likely to work with people with OA and TJA based on their practice areas (e.g., orthopaedics, gerontology, rheumatology) regardless of practice sector (public or private). To ensure broad representation of physiotherapists treating TJA patients, we used a mixed sampling method that included stratified random sampling for subgroups larger than 100 and complete sampling of smaller subgroups. We identified a total of 694 physiotherapists as potential participants (representing 29% of the total eligible registrants) with the goal of getting approximately 345 responses. This was based on an anticipated 50% response rate (consistent with a similar survey of physiotherapists' use of OMs).16
Questionnaire development and administration
We developed a 13-page paper-based questionnaire with sections requesting information on (1) demographics, (2) PROMs, (3) performance-based OMs, and (4) indicators for prognosis. The 19 selected OMs (see Table 1) were identified by a provincial advisory group based on criteria for reliability, validity, responsiveness, clinical feasibility (ease of administration and scoring), and availability (no licensing or user fee). Measures exclusively in the ICF domains “body structure and function” (e.g., range of motion), with the exception of pain, were excluded because they are already widely used with TJA patients.25,31
Table 1.
ICF Domains Assessed by Each Outcome Measure Included in the Survey
| ICF domain |
||||
|---|---|---|---|---|
| Outcome measure | Body structure or function | Activity | Participation* | Personal contextual factor |
| Patient reported outcome measures (PROMs) | ||||
| Arth SE | X | |||
| EQ-5D | X | X | X (1) | |
| HOOS | X | X | X (?) | |
| KOOS | X | X | X (?) | |
| LEFS | X | X | ||
| NPRS | X | |||
| OHS | X | X | ||
| OKS | X | X | ||
| VNPain | X | |||
| Performance-based outcome measures | ||||
| 6MWT | X | |||
| SLegS—balance | X | |||
| SitTS—repeated stands | X | |||
| Tinetti | X | |||
| TStairC | X | |||
| TUG | X | |||
| WalkS | X | |||
| Other measures | ||||
| BMI | X | |||
| SMBehav | X | |||
| WaistC | X | |||
Only measures that included ≥1 item related to “participation” are noted under this domain; number of items noted in parentheses; (?)=authors' judgment that OM item(s) does not truly reflect “participation.”
Arth SE=Arthritis Self-Efficacy Scale; EQ-5D=European Quality of Life-5 Dimensions; HOOS=Hip disability and Osteoarthritis Outcome Score; KOOS=Knee injury and Osteoarthritis Outcome Score; LEFS=Lower Extremity Functional Scale; NPRS=Numeric Pain Rating Scale; OHS=Oxford Hip Score; OKS=Oxford Knee Score; VNPain=Visual Numeric Pain Scale; 6MWT=6-Minute Walk Test; SLegS=Single Leg Stance; SitTS=Sit to Stand; Tinetti=Tinetti Balance Test; TStairC=Timed Stair Climb; TUG=Timed Up and Go; WalkS=Walking Speed Test; BMI=Body Mass Index; SMBehav=Self-Management Exercise Behaviours; WaistC=Waist circumference.
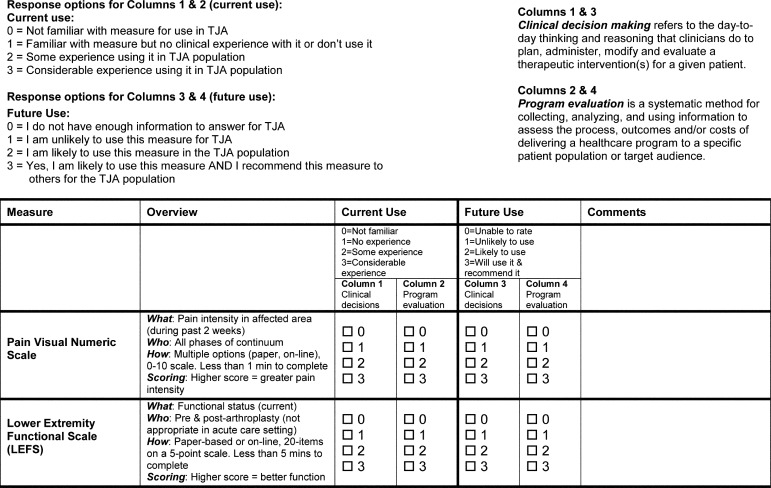
Respondents were asked to rate their familiarity with, experience with, and current use of specific OMs using a four-point ordinal scale (0=not familiar; 3=considerable experience) (Figure 1). For anticipated future use of OMs, our survey used a modified scale (0=unable to rate; 1=unlikely to use; 2=likely to use; 3=will use and recommend). Questions were posed in the contexts of clinical decision making (described as “the day-to-day thinking and reasoning clinicians do for a patient”) and program evaluation (described as “the systematic method for collecting, analyzing, and using information to assess processes and outcomes of delivering a healthcare program”). We provided respondents with a link to a website summarizing the measures. Respondents were invited to comment on each measure and suggest other measures that were not included in the questionnaire. The questionnaire was pilot-tested with 19 physiotherapists who worked with TJA patients along the care continuum, and minor modifications were made as a result of their feedback.
Figure 1.
Excerpts from survey.
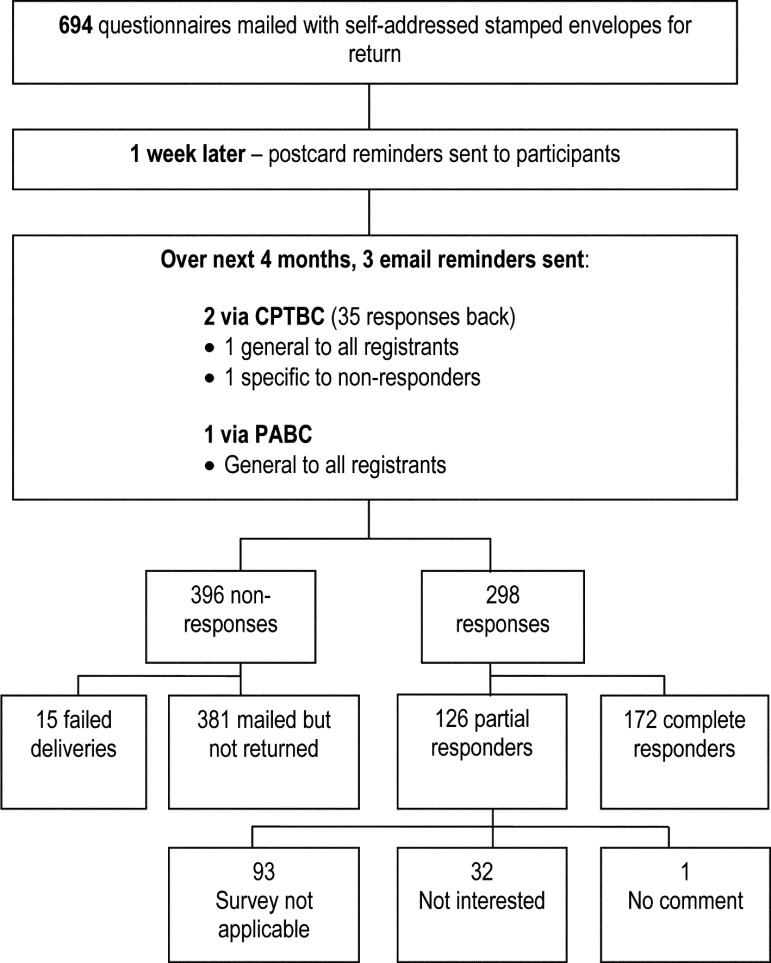
We mailed the questionnaire to physiotherapists with a cover letter of instructions and a self-addressed stamped envelope. To optimize response rates, we sent postcard reminders 7 days after the initial mailing, followed by e-mail reminders (Figure 2). Each mailed survey was assigned a random numeric code to ensure anonymity. When targeted reminders were sent to non-responders, one author accessed the information to provide addresses from the random codes.
Figure 2.
Flowchart of questionnaire mail out and responses.
“Partial responders” were those who completed the demographic section of the questionnaire only. “Complete responders” returned the completed questionnaire.
Data analysis
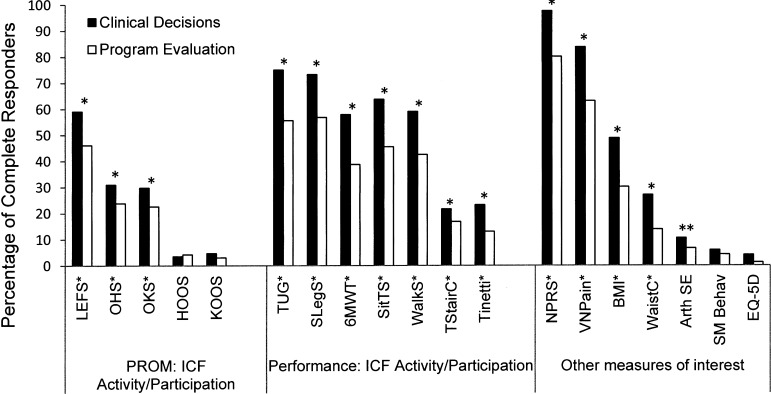
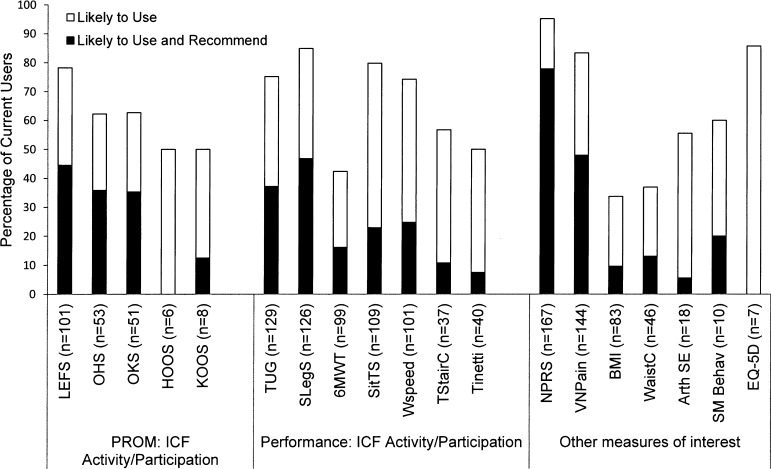
We entered the survey data into an Excel spreadsheet (Microsoft Corp., Redmond, WA), double-checked them for accuracy, and uploaded them to SPSS (v17, SPSS Inc., Chicago, IL). We classified participants as either complete responders (those who completed the survey) or partial responders (those who completed only the demographic information). Cross-tabulations and chi-square tests were performed to compare demographic and practice variables for partial and complete responders, and the McNemar test was performed to compare the use of OMs for clinical decision making versus program evaluation. For these analyses, we dichotomized the ordinal four-point scales (use/don't use). Significance was set at p<0.05. Analyses of responses about participants' experience using the OMs were reported as frequencies and percentages, with graphs enabling visual comparisons between OMs (Figures 3 and 4).
Figure 3.
Comparison of complete responders' current use of outcome measures for clinical decision-making and program evaluation.
n=165–172 (Note: some OMs had missing data).
*significance at p<0.004 between clinical decision use and program evaluation.
**significance at p<0.04.
Figure 4.
Current users' anticipated future use and recommendation of measures for clinical decision-making.
Pairs of authors (CM, MW, RF, MD) performed a thematic analysis of respondents' comments, independently coding comments using an iterative approach. Common or recurring topics were categorized and grouped into sub-themes. Disagreements in coding and categorization were discussed, and the coding scheme was refined as necessary.32 For each theme, we chose representative quotes from the comments.
Results
A total of 298 physiotherapists (43%) responded to the survey; of these, 42% were partial responders who completed demographic information but did not respond to questions about outcome measures, and 58% were complete responders. Primary reasons given for partial responses were that the respondent did not work with TJA patients (74%) or that s/he worked with TJA patients but was not interested in completing the questionnaire (25%).
Table 2 provides demographic and practice characteristics of respondents. Complete responders were mostly female (74%; 127) and represented all provincial health regions. A smaller proportion of complete responders (57%; 96) than of partial responders (72%; 85) worked in urban settings (p=0.036). A larger proportion of complete responders (25%; 43) than of partial responders (13%; 13) had practised for <10 years (p=0.008). Complete responders represented all phases of TJA care, and 40% (73) indicated that they worked in three or four phases from pre-operative through to post-rehabilitation care.
Table 2.
Demographic Characteristics of Responders
| % of Responders |
|||
|---|---|---|---|
| Responders' characteristics | Partial responders (n=126) |
Complete responders (n=172) |
All (n=298) |
| Practice location | |||
| Urban | 72 | 57.1 | 63.3 |
| Mixed rural/urban | 20.3 | 31.5 | 26.9 |
| Rural/remote | 7.6 | 11.3 | 9.8 |
| Years since graduation* | |||
| <10 | 13.4 | 25.4 | 21.1 |
| 10–19 | 23.7 | 30.8 | 28.2 |
| ≥20 | 62.9 | 43.8 | 50.8 |
| Full-time working status | 54.9 | 63.5 | 60.3 |
| Clinical setting† | |||
| Private clinic | 52.6 | 43.9 | 47.1 |
| Public sector | 47.4 | 56.1 | 52.9 |
| Continuum setting† | |||
| In-patient | 26.3 | 16.5 | 20.1 |
| Home/community care | 12.6 | 13.4 | 13.1 |
| Outpatient | 61.1 | 70.1 | 66.8 |
| Continuum phase*† | |||
| No phases | 58.2 | 1.7 | 25.2 |
| Pre-op | 13.2 | 54.4 | 38.6 |
| Post-op | 23.6 | 74.9 | 55.2 |
| Rehab | 23.6 | 66.1 | 49.8 |
| Post rehab | 15.1 | 40.9 | 31.0 |
Chi-square p<0.05.
Some categories were not mutually exclusive, so percentages may total more than 100%.
Familiarity with outcome measures
Of PROMS within the ICF domains “activity and participation,” respondents were most familiar with the Lower Extremity Functional Scale (LEFS) (75%), followed by the Oxford Hip Score (OHS) (62%) and Oxford Knee Score (OKS) (61%). Respondents were least familiar with the Knee disability and Osteoarthritis Outcome Score (KOOS) (24%) and the Hip injury and Osteoarthritis Outcome Score (HOOS) (18%).
Overall, respondents reported more familiarity with performance-based measures than with the above-mentioned PROMS. The timed up-and-go (TUG) test was most familiar to respondents (91%), followed by the Single Leg Stance (SLegS) (89%), 6-Minute Walk Test (6MWT) (83%), Sit to Stand (SitTS) (82%), and Walking Speed Test (WalkS) (80%). The least familiar measures were the Timed Stairs Climb (TStairC) (55%) and Tinetti Balance Test (Tinetti) (49%).
Pain measures were most familiar to responders: 99% were familiar with the Numeric Pain Rating Scale (NPRS) and 94% with the Visual Numeric Pain Scale (VNPain). Respondents varied in their familiarity with prognostic measures and personal contextual factors, which included Body Mass Index (BMI) (88%), Waist circumference (WaistC) (73%), Arthritis Self-Efficacy (Arth SE) (31%); Self-Management for Exercise Behaviours (SMBehav) (19%), and European Quality of Life—5 Dimensions measure (EQ-5D, 14%).
Current use of outcome measures
Most respondents used ≥1 PROM for clinical decision making, the most common being the NPRS (98%). (Figure 3) PROMs with the greatest familiarity ratings showed similar trends, albeit lower values, to reported use: the LEFS (59%) was used most often, whereas <5% of respondents used the KOOS and HOOS. The LEFS, OHS, and OKS were used more often for clinical decision making than for program evaluation (p<0.001 to p=0.002).
Most respondents (95%) reported using ≥1 performance-based measure for clinical decision making; the TUG test was used most often (75%). All performance-based measures were used more often for clinical decision making than for program evaluation (p<0.001 to p=0.004).
Current use of other measures of interest ranged from 49% for BMI to 6% for the SMBehav tool. A greater proportion of respondents used pain scales, BMI, and WaistC for clinical decision making than for program evaluation (all at p<0.001).
Future and recommended use of outcome measures
Of the “activity and participation” PROMs, the LEFS received the highest ratings for both future use (78%) and recommended use (45%). Of the just over 50 current users of the OHS and OKS, almost two-thirds reported that they are likely to use these measures in the future, and one-third recommended them. (Figure 4) Through post-hoc analysis of PROMs identified by ≥10 respondents working in at least three phases of care and reporting “considerable experience,” we found three PROMs with the highest ratings for future use and recommended use: the LEFS, which 91% (21/23) of respondents recommended and expected to use in the future, and the OKS/OHS (82%, 9/11).
Of the performance-based measures, the SLegS received the highest rating for future use (85%), and almost half of complete responders would recommend its use to others. Despite high familiarity and moderate use of the 6MWT, ratings for future use were modest (42%), and even fewer (16%) said they would recommend it. Through post-hoc analysis of performance-based measures identified by ≥10 respondents working in at least three phases of care and reporting “considerable experience,” we found four measures with high ratings for future use and recommended use: SLegS (77%, 27/35), TUG (65%, 13/20), WalkS (57%, 8/14), and 6MWT (50%, 5/10).
Our data also show that >90% of current users are likely to use the NPRS in the future, 78% would recommend it for clinical decisions, and approximately 80% would recommend its future use for program evaluation.
The other measures of interest most frequently listed were range of motion using a goniometer (29 respondents) and strength testing (19 respondents) using undefined methods. The only “activity and participation” PROMs suggested by more than one respondent were the Patient Specific Functional Scale and the Health Assessment Questionnaire—Disability Index, a tool not validated for OA-related TJA.28 One suggested performance-based measure was the Berg Balance Scale. Many respondents reported using unspecified gait analysis methods and recording use of gait aids.
Subjective comments
Clinical feasibility dominated respondents' comments; under this overarching theme, four sub-themes emerged (see Box 1):
Diverse and contrasting attitudes, beliefs, and knowledge about outcome measurement in general and specific measures. While some respondents questioned the value of using any standardized tool, others supported the practice and self-identified a knowledge gap about OMs.
Certain patient subgroups present challenges to standardized outcome measurement in TJA: (a) elderly, frail, or cognitively impaired patients who have difficulty completing many of the OMs, have greater functional disability, and are typically not included in OM validation studies; (b) patients with language and cultural barriers that pose challenges for safe and correct OM administration (there is also a perceived lack of translated and culturally sensitive tools); and (c) young and fit patients who may not suit some standardized OMs because of lack of relevance and potential ceiling effects.
Not all OMs are appropriate for all phases and settings along the care continuum. Comments ranged from a lack of resources, space, and time for administering and scoring measures in a busy acute-care setting to the appropriateness of using specific performance-based measures on patients with end-stage OA in the immediate pre-operative phase.
Many physiotherapists are dissatisfied with currently available tools. Respondents identified several barriers to using specific tools in a standardized way. Several reported using alternate or less formal methods and other tools to measure similar concepts for a given OM. Standardized OM administration combined with subjective or informal scoring and interpretation was also common.
Box 1. Representative Quotes for Themes Arising from Subjective Analysis.
Theme 1: Diverse views on value of outcome measurement for TJA
I would be very happy to be told what the gold standard tests/measures are and incorporate them into my practice.
It would be really fantastic to come out with a complete package of info to share with more remote colleagues.
It would be useful to have one outcome measure that could be used throughout the continuum … and the province, so that we all speak the same language.
… use of outcome measures in this population is redundant. Why keep measuring when we know there will be improvement?
No outcome measure will ever replace my expertise to assess a patient; it can only be a guide.
Theme 2: Patient subgroups
-
Elderly, frail, or cognitively impaired:
The age of clients and multiple health conditions make testing difficult at times.
Somewhat difficult to render quality data when past medical history includes dementia. (regarding SitTS)
-
Language or cultural barriers:
Language barrier may prevent full use of measurement tools with given caseload. (regarding several tools)
-
Young and fit patients:
Not a focus in my patient caseload—a very fit group in general. (regarding TUG)
Theme 3: Appropriateness of OMs across care phases and settings
most outcome measures not useful in acute care
difficult to use consistently in community setting (regarding TStairC & WalkS)
Theme 4: Dissatisfaction with currently available OMs
I observe safety and balance on using stairs but don't time it. (regarding TStairC)
Tried [TUG] in [total hip arthroplasty] population—has a ceiling effect.
I use Berg Balance instead. (regarding SLegS)
Discussion
Physiotherapists treating patients along the TJA continuum use a variety of “activity and participation” OMs to inform clinical decisions and evaluate program effectiveness. Eight of 19 OMs were used by most respondents. The high use of pain tools is not surprising, as pain is both a primary indication for TJA and an important outcome.26,28 The reported 100% use of one or more standardized OMs is higher than previously reported among physiotherapists in clinical practice.16,33 More than 75% of respondents were unfamiliar with the KOOS/HOOS and EQ-5D, despite their described use in the TJA literature.7,19,28
Our finding that performance-based measures are used more often to assess “activity and participation” may reflect their clinical utility and greater responsiveness to change relative to PROMs, especially in the post-operative phase.29 Alternatively, physiotherapists may recognize and value the fact that different OMs capture distinct but equally important aspects of patient functioning and that a combination of PROM and performance-based OMs is necessary.33–37 The OARSI advisory group has recommended five performance-based tests as a core set (30-s chair-stand test, 40 m fast-paced walk test, a stair-climb test, TUG, and 6MWT), the first three of which constitute the minimal core set.21 Our results indicate that, with the exception of a timed stair-climb test, the majority of respondents have experience using these core OMs, and more than half of those who have considerable experience with WalkS, TUG, and 6MWT expect to use and recommend these OMs in the future.
Over 90% of respondents used pain OMs, and many reported using range of motion and strength measures, consistent with previously reported reliance on these OMs.19,24 A recent survey of 394 Dutch physiotherapists in private practice similarly found that pain and range of motion were the two most frequently used OMs.35 Although valid and practical across all phases of care and clinical settings, these measures have weak associations with “activity and participation.”24 This is relevant because of the value patients place on activity and participation soon after TJA.38
Factors reported in our study as likely to contribute to variability in OM use include familiarity with the OMs; appropriateness for use with varied subgroups; available time, space, and resources in different settings; and perceived value of routinely using OMs. Similar barriers and facilitators to OM use have previously been reported.13,16,35,39 Our study, however, is the first to identify the issues associated with using the same OMs across care settings and phases. Increasing use of OMs with TJA patients will require not only identifying appropriate OMs but also developing implementation strategies to facilitate their incorporation into daily practice.
For most OMs, less than half of current users report they are likely to use the measure in the future, a smaller proportion than previously reported.16 This suggests that physiotherapists are not satisfied with the OMs currently available. Consistent use of a core set of OMs has been proposed to enhance professional and patient communication,36 but measures in this core set need to be freely available and involve a minimal administration and scoring burden.20 The costs and licensing requirements of the widely used Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)40 and Oxford Hip and Knee Scores41,42 present a significant barrier to their routine clinical use among physiotherapists. Therefore, of the PROMs included in the questionnaire, only the commonly used LEFS43 and the less familiar HOOS/KOOS tools44,45 may currently be appropriate for routine clinical use. When establishing a core set of OMs, it will be important to note that more respondents used broadly applicable OMs (e.g., LEFS, NPRS) that facilitate clinical decisions than condition-specific OMs (e.g., OHS/OKS). Their usefulness across a variety of patient populations may help physiotherapists work more efficiently.46
The HOOS and KOOS are joint-specific tools intended for use with younger, active people with OA of the hip and knee, respectively. They incorporate the WOMAC and are more sensitive and responsive than the WOMAC in younger or more active patients.47 The LEFS is designed specifically to measure function with a variety of lower-extremity orthopaedic conditions, including OA. The LEFS addresses more complex functioning and sporting activity to capture a similarly broad of scope of patient health and functioning as the HOOS/KOOS; however, therapists need to use additional measures to assess pain and quality of life constructs. Thus, while the HOOS/KOOS take longer to complete and score, they are more comprehensive and allow calculation of a WOMAC score.47 The region-specific design of the LEFS permits its use across diverse patient populations, which may be an advantage in some clinical settings.46 Physiotherapists need more exposure to and experience with the HOOS/KOOS tools before they can make informed choices and further recommendations.
The various performance-based “activity and participation” measures pose different challenges for physiotherapists related to space, time, resources, and patient feasibility and safety. Respondents' greater use of performance-based measures over PROMs likely reflects their training and confidence in applying and interpreting functional tests. It may be easier for physiotherapists to associate findings on a performance test (e.g., poor static balance) with the appropriate therapeutic intervention (e.g., balance exercises) than to determine the appropriate intervention from a score on a multi-item tool on which balance is one question. However, performance-based measures represent a snapshot of a person's functioning at a particular time, whereas PROMs reflect a patient's longer-term (e.g., “over the last 4 weeks”) perception of his or her abilities.36
Our study has several limitations. First, the response rate could compromise the internal validity of the findings. However, our sample was representative of physiotherapists registered with the provincial College, and the response rate is similar to those of related surveys.16,35 Second, the term “outcome measure” was not defined on the questionnaire, and this may have influenced responses, particularly to the question on what other OMs participants used. Another limitation is that physiotherapists who responded to the survey may have been more likely than non-responders to use OMs.48 The survey did not define “some” or “considerable” experience using the OMs, so the extent of use is unknown; overestimation of therapists' perceived and reported use of OMs is another possibility, as previous studies35 and our group's recent chart audit of physiotherapists' recorded use of OMs with TKA clients suggest.31 Furthermore, we could not determine what proportion of physiotherapists administer OMs but fail to score, record, and interpret them. Finally, this survey may have limited external validity beyond British Columbia.
Conclusion
Physiotherapists use a wide variety of OMs when treating people with OA or TJA; however, our results suggest that there are challenges to the consistent use of most of these measures across care settings and phases of treatment. Respondents have more experience with performance-based measures and are more likely to use and recommend them over PROMs. The disparity between respondents' current use and their recommendation for future use of OMs may indicate dissatisfaction with the current choice of OMs, or it may suggest that respondents feel insufficiently experienced to make recommendations. Several structural, procedural, practitioner, and patient factors were identified as barriers to OM use. Contrasting views emerged about the clinical value of routinely using standardized OMs. Our findings confirm a need to develop a core set of appropriate OMs that include both PROM and performance-based measures along with resources to facilitate their routine use throughout the TJA continuum.
Key messages
What is already known on this topic
Numerous outcome measures (OMs) with sound psychometric properties are available for use with people with hip or knee osteoarthritis (OA) undergoing total joint arthroplasty (TJA) surgery; however, there is marked variation in their use. It is also known that patient-reported outcome measures (PROMs) tend to over-estimate positive change in the early post-operative period. Many barriers to routine use of OMs in physiotherapy practice have been documented, but little is known about the use of PROMs and performance-based measures in day-to-day physiotherapy practice along the TJA continuum and across care settings.
What this study adds
To our knowledge, this study is the first to document physiotherapists' familiarity with and experience using standardized OMs in patients with hip/knee OA and who have undergone TJA. This study demonstrates that physiotherapists are likely to use a combination of performance-based OMs to support clinical decisions and program evaluation, since no single measure is comprehensive or clinically feasible across all care phases and settings. Although physiotherapists in BC routinely use at least one OM to inform their clinical care of these patients, their comments suggest some dissatisfaction with the feasibility and applicability of existing tools.
Physiotherapy Canada 2014; 66(3);274–285; doi:10.3138/ptc.2013-34
References
- 1.Bombardier C, Hawker G, Mosher D. The impact of arthritis in Canada: Today and over the next 30 years [Internet] Toronto: Arthritis Alliance of Canada; 2011. [cited 2013 Aug 13]. Available from: http://www.arthritisalliance.ca. [Google Scholar]
- 2.Kopec JA, Rahman MM, Berthelot JM, et al. Descriptive epidemiology of osteoarthritis in British Columbia, Canada. J Rheumatol. 2007;34(2):386–93. Medline:17183616. [PubMed] [Google Scholar]
- 3.Badley EM. The effect of osteoarthritis on disability and health care use in Canada. J Rheumatol Suppl. 1995;43:19–22. Medline:7752126. [PubMed] [Google Scholar]
- 4.Canadian Institute for Health Information (CIHI) Hip and Knee Replacements in Canada: Canadian Joint Replacement Registry 2013 Annual Report [Internet] Ottawa: The Institute; 2013. [cited 2013 Aug 13]. Available from: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC51. [Google Scholar]
- 5.Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64(4):465–74. doi: 10.1002/acr.21596. http://dx.doi.org/10.1002/acr.21596. Medline:22563589. [DOI] [PubMed] [Google Scholar]
- 6.Westby MD. Rehabilitation and total joint arthroplasty. Clin Geriatr Med. 2012;28(3):489–508. doi: 10.1016/j.cger.2012.05.005. http://dx.doi.org/10.1016/j.cger.2012.05.005. Medline:22840310. [DOI] [PubMed] [Google Scholar]
- 7.Ethgen O, Bruyère O, Richy F, et al. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A(5):963–74. doi: 10.2106/00004623-200405000-00012. Medline:15118039. [DOI] [PubMed] [Google Scholar]
- 8.Milner CE. Is gait normal after total knee arthroplasty? Systematic review of the literature. J Orthop Sci. 2009;14(1):114–20. doi: 10.1007/s00776-008-1285-8. http://dx.doi.org/10.1007/s00776-008-1285-8. Medline:19214698. [DOI] [PubMed] [Google Scholar]
- 9.Noble PC, Gordon MJ, Weiss JM, et al. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431(431):157–65. doi: 10.1097/01.blo.0000150130.03519.fb. http://dx.doi.org/10.1097/01.blo.0000150130.03519.fb. Medline:15685070. [DOI] [PubMed] [Google Scholar]
- 10.Bade MJ, Stevens-Lapsley JE. Restoration of physical function in patients following total knee arthroplasty: an update on rehabilitation practices. Curr Opin Rheumatol. 2012;24(2):208–14. doi: 10.1097/BOR.0b013e32834ff26d. http://dx.doi.org/10.1097/BOR.0b013e32834ff26d. Medline:22249349. [DOI] [PubMed] [Google Scholar]
- 11.Rasch A, Dalén N, Berg HE. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop. 2010;81(2):183–8. doi: 10.3109/17453671003793204. http://dx.doi.org/10.3109/17453671003793204. Medline:20367414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kennedy DM, Stratford PW, Robarts S, et al. Using outcome measure results to facilitate clinical decisions the first year after total hip arthroplasty. J Orthop Sports Phys Ther. 2011;41(4):232–40. doi: 10.2519/jospt.2011.3516. http://dx.doi.org/10.2519/jospt.2011.3516. Medline:21289460. [DOI] [PubMed] [Google Scholar]
- 13.Wedge FM, Braswell-Christy J, Brown CJ, et al. Factors influencing the use of outcome measures in physical therapy practice. Physiother Theory Pract. 2012;28(2):119–33. doi: 10.3109/09593985.2011.578706. http://dx.doi.org/10.3109/09593985.2011.578706. Medline:21877943. [DOI] [PubMed] [Google Scholar]
- 14.Lohmann S, Decker J, Müller M, et al. The ICF forms a useful framework for classifying individual patient goals in post-acute rehabilitation. J Rehabil Med. 2011;43(2):151–5. doi: 10.2340/16501977-0657. Medline:21234515. [DOI] [PubMed] [Google Scholar]
- 15.Pisoni C, Giardini A, Majani G, et al. International Classification of Functioning, Disability and Health (ICF) core sets for osteoarthritis. A useful tool in the follow-up of patients after joint arthroplasty. Eur J Phys Rehabil Med. 2008;44(4):377–85. Medline:18469736. [PubMed] [Google Scholar]
- 16.Jette DU, Halbert J, Iverson C, et al. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89(2):125–35. doi: 10.2522/ptj.20080234. http://dx.doi.org/10.2522/ptj.20080234. Medline:19074618. [DOI] [PubMed] [Google Scholar]
- 17.McGrail K, Bryan S, Davis J. Let's all go to the PROM: the case for routine patient-reported outcome measurement in Canadian healthcare. Healthc Pap. 2011;11(4):8–18, discussion 55–8. doi: 10.12927/hcpap.2012.22697. Medline:22543287. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. International Classification of Functioning, Disability and Health (ICF) [Internet] Geneva: The Organization; 2001. [cited 2004 Mar 3]. Available from: http://www.who.int/classifications/icf/ [Google Scholar]
- 19.Riddle DL, Stratford PW, Bowman DH. Findings of extensive variation in the types of outcome measures used in hip and knee replacement clinical trials: a systematic review. Arthritis Rheum. 2008;59(6):876–83. doi: 10.1002/art.23706. http://dx.doi.org/10.1002/art.23706. Medline:18512725. [DOI] [PubMed] [Google Scholar]
- 20.Collins NJ, Roos EM. Patient-reported outcomes for total hip and knee arthroplasty: commonly used instruments and attributes of a “good” measure. Clin Geriatr Med. 2012;28(3):367–94. doi: 10.1016/j.cger.2012.05.007. http://dx.doi.org/10.1016/j.cger.2012.05.007. Medline:22840304. [DOI] [PubMed] [Google Scholar]
- 21.Dobson F, Hinman RS, Roos EM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(8):1042–52. doi: 10.1016/j.joca.2013.05.002. http://dx.doi.org/10.1016/j.joca.2013.05.002. Medline:23680877. [DOI] [PubMed] [Google Scholar]
- 22.Dreinhöfer K, Stucki G, Ewert T, et al. ICF core sets for osteoarthritis. J Rehabil Med. 2004;44(44 Suppl):75–80. doi: 10.1080/16501960410015498. Medline:15370752. [DOI] [PubMed] [Google Scholar]
- 23.Riddle DL, Stratford PW, Singh JA, et al. Variation in outcome measures in hip and knee arthroplasty clinical trials: a proposed approach to achieving consensus. J Rheumatol. 2009;36(9):2050–6. doi: 10.3899/jrheum090356. http://dx.doi.org/10.3899/jrheum090356. Medline:19738212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finch E, Brooks D, Stratford PW, et al. Physical rehabilitation outcome measures: a guide to enhanced clinical decision-making. 2nd ed. Hamilton (ON): BC Decker; 2002. [Google Scholar]
- 25.Haigh R, Tennant A, Biering-Sørensen F, et al. The use of outcome measures in physical medicine and rehabilitation within Europe. J Rehabil Med. 2001;33(6):273–8. doi: 10.1080/165019701753236464. http://dx.doi.org/10.1080/165019701753236464. Medline:11766957. [DOI] [PubMed] [Google Scholar]
- 26.Rastogi R, Davis AM, Chesworth BM. A cross-sectional look at patient concerns in the first six weeks following primary total knee arthroplasty. Health Qual Life Outcomes. 2007;5(1):48. doi: 10.1186/1477-7525-5-48. http://dx.doi.org/10.1186/1477-7525-5-48. Medline:17678532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Westby MD, Backman CL. Patient and health professional views on rehabilitation practices and outcomes following total hip and knee arthroplasty: a focus group study. [cited 2011 Dec 15];BMC Health Services Research [Internet] 2010 May;10:119. doi: 10.1186/1472-6963-10-119. Available from: http://www.biomedcentral.com/content/pdf/1472-6963-10-119.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alviar MJ, Olver J, Brand C, et al. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011;43(5):374–81. doi: 10.2340/16501977-0801. http://dx.doi.org/10.2340/16501977-0801. Medline:21448553. [DOI] [PubMed] [Google Scholar]
- 29.Stratford PW, Kennedy DM, Maly MR, et al. Quantifying self-report measures' overestimation of mobility scores postarthroplasty. Phys Ther. 2010;90(9):1288–96. doi: 10.2522/ptj.20100058. http://dx.doi.org/10.2522/ptj.20100058. Medline:20592271. [DOI] [PubMed] [Google Scholar]
- 30.Stratford PW, Kennedy DM, Riddle DL. New study design evaluated the validity of measures to assess change after hip or knee arthroplasty. J Clin Epidemiol. 2009;62(3):347–52. doi: 10.1016/j.jclinepi.2008.06.008. http://dx.doi.org/10.1016/j.jclinepi.2008.06.008. Medline:18834709. [DOI] [PubMed] [Google Scholar]
- 31.McAuley C, Harrison K, Rebman M. Rate of recovery of knee flexion and extension after total knee replacement. Unpublished report. 2009.
- 32.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–6. doi: 10.1136/bmj.320.7227.114. http://dx.doi.org/10.1136/bmj.320.7227.114. Medline:10625273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gandhi R, Tsvetkov D, Davey JR, et al. Relationship between self-reported and performance-based tests in a hip and knee joint replacement population. Clin Rheumatol. 2009;28(3):253–7. doi: 10.1007/s10067-008-1021-y. http://dx.doi.org/10.1007/s10067-008-1021-y. Medline:18853222. [DOI] [PubMed] [Google Scholar]
- 34.Alviar MJ, Olver J, Brand C, et al. Do patient-reported outcome measures in hip and knee arthroplasty rehabilitation have robust measurement attributes? A systematic review. J Rehabil Med. 2011;43(7):572–83. doi: 10.2340/16501977-0828. http://dx.doi.org/10.2340/16501977-0828. Medline:21607295. [DOI] [PubMed] [Google Scholar]
- 35.Swinkels RAHM, van Peppen RPS, Wittink H, et al. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. [cited 2012 Dec 15];BMC Musculoskeletal Disorders [Internet] 2011 May;12:106. doi: 10.1186/1471-2474-12-106. Available from: http://www.biomedcentral.com/content/pdf/1471-2474-12-106.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol. 2006;59(2):160–7. doi: 10.1016/j.jclinepi.2005.07.012. http://dx.doi.org/10.1016/j.jclinepi.2005.07.012. Medline:16426951. [DOI] [PubMed] [Google Scholar]
- 37.Unnanuntana A, Mait JE, Shaffer AD, et al. Performance-based tests and self-reported questionnaires provide distinct information for the preoperative evaluation of total hip arthroplasty patients. J Arthroplasty. 2012;27(5):770–5, e1. doi: 10.1016/j.arth.2011.08.005. http://dx.doi.org/10.1016/j.arth.2011.08.005. Medline:21958935. [DOI] [PubMed] [Google Scholar]
- 38.Rastogi R, Chesworth BM, Davis AM. Change in patient concerns following total knee arthroplasty described with the International Classification of Functioning, Disability and Health: a repeated measures design. Health Qual Life Outcomes. 2008;6(1):112. doi: 10.1186/1477-7525-6-112. http://dx.doi.org/10.1186/1477-7525-6-112. Medline:19077246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duncan EA, Murray J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: a systematic review. [cited 2012 Dec 15];BMC Health Serv Res [Internet] 2012 Apr;12:96. doi: 10.1186/1472-6963-12-96. Available from: http://www.biomedcentral.com/content/pdf/1472-6963-12-96.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. Medline:3068365. [PubMed] [Google Scholar]
- 41.Dawson J, Fitzpatrick R, Murray D, et al. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80(1):63–9. doi: 10.1302/0301-620x.80b1.7859. http://dx.doi.org/10.1302/0301-620X.80B1.7859. Medline:9460955. [DOI] [PubMed] [Google Scholar]
- 42.Dawson J, Fitzpatrick R, Carr A, et al. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–90. Medline:8666621. [PubMed] [Google Scholar]
- 43.Binkley JM, Stratford PW, Lott SA, et al. North American Orthopaedic Rehabilitation Research Network. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther. 1999;79(4):371–83. Medline:10201543. [PubMed] [Google Scholar]
- 44.Nilsdotter A, Lohmander L, Klassbo M, et al. Hip disability and osteoarthritis outcome score (HOOS)—validity and responsiveness in total hip replacement. [cited 2012 Dec 15];BMC Musculoskelet Disord [Internet] 2003 May;4:10. doi: 10.1186/1471-2474-4-10. Available from: http://www.biomedcentral.com/content/pdf/1471-2474-4-10.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. http://dx.doi.org/10.2519/jospt.1998.28.2.88. Medline:9699158. [DOI] [PubMed] [Google Scholar]
- 46.Brazier JE, Harper R, Munro J, et al. Generic and condition-specific outcome measures for people with osteoarthritis of the knee. Rheumatology (Oxford) 1999;38(9):870–7. doi: 10.1093/rheumatology/38.9.870. http://dx.doi.org/10.1093/rheumatology/38.9.870. Medline:10515649. [DOI] [PubMed] [Google Scholar]
- 47.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1(1):17. doi: 10.1186/1477-7525-1-17. http://dx.doi.org/10.1186/1477-7525-1-17. Medline:12801417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dillman DA. Mail and Internet surveys: the tailored design method. 2nd ed. Hoboken (NJ): Wiley; 2000. [Google Scholar]