Abstract
The goal:
The goal of this work was to give advantage to EUS as endoscopic method in diagnosis and following therapeutic treatment of pancreatic cancer in relation to radiological methods of CT and CTA.
Material and Methods:
The study included 49 patients, 20 women and 29 men hospitalized at the Clinic for gastroenterohepatology, due to suspicion on pancreatic cancer during observed 2 years period. All cancers were histologically and cytologically confirmed. The patients underwent ERCP as a mandatory part of staging and all patients underwent endoscopic ultrasound as well as CT or CT angiography.
Results:
Testing of differences was carried out using Fisher’s exact test in open-source software R. The following characteristics were tested: involvement of the blood vessels, lymph nodes, metastases, tumor size and duodenum infiltration. Results showed statistically significant difference at the 0.05 level for EUS, CT and CT angiography. Risk ratio showed that EUS is less effective in detecting infiltration of blood vessels within a malignant process then CTA where RR=0.52, CI 0.2–1.38, p-value=0.33. EUS and CTA are equal in the diagnosis of enlarged lymph nodes affected by malignancy where RR=1.3, CI 0.75–1.42, p-value=0.09. Comparison according to distant metastases showed that EUS is less effective compared to CT in approximately 30% of cases. In the diagnosis of duodenal infiltration EUS is in 5% of cases less accurate than the CT with the RR=0.95, CI 0.27–3.32, p-value=0.76, but the CTA method is more efficient because the comparison of EUS and CTA showed RR=12.52, CI 0.2–1.38, p-value=0.33. EUS as a diagnostic method is dominant in determining the size of malignant lesions located in the pancreas as compared to CT and CTA.
Conclusion:
EUS as endoscopic method compared to CT and CTA is one of the more invasive methods of examination but due to its ability to be performed immediately, to locate a changes smaller than 5 mm and the target biopsy option, to measure the change and that in many cases determine the relationship of malignant lesions with blood vessels, along with visualization of the surrounding lymph nodes and metastases in neighboring organs, we may give this method an advantage over other methods in the preoperative staging of patients with pancreatic cancer.
Keywords: pancreatic cancer, CTA, EUS, CT, CEA and CA19-9
1. INTRODUCTION
Pancreatic cancer is one of the more common tumors in human pathology. It is more difficult to diagnose it at an early stage, so patients usually come to a doctor with subjective complaints associated with the already formed metastases or infiltration of the adjacent organs. It is considered as fourth leading cause of death in patients with pancreatic carcinoma and 5-year survival rate of the patients is between 15-21% (1). This represents the tumor of the elderly at 60-80 years of age. The exact cause of pancreatic cancer is not known and it is up to two times more common in men, while 60% of cancers are localized in the pancreatic head, in relation to other parts of this gland. Tumor markers CEA and CA 19-9 were, although in high concentration in serum, late markers, combined with the already developed metastases.
Speaking about diagnosis, we can say that regardless of the diagnostic options, diagnosis of pancreatic cancer is late and usually severe abdominal pain, silent jaundice, lead patient to the doctor. Endoscopic ultrasound (EUS) is a cheap method of examination and immediately accessible at the Clinic for gastroenterohepatology. This diagnostic method enables visualizing of the change, its location, possibility to measure its size and gain insight in its relationship with the surrounding blood vessels. Additionally, it provides insight into the liver, stomach and back wall of the stomach and neighboring lymph nodes as well as the duodenal frame and possible metastases in these organs.
EUS allows us to perform targeted pancreatic biopsy of visualized changes and to obtain rapid histopathologic confirmation. Another very important method in the diagnosis of pancreatic cancer is an endoscopic retrograde cholangiopancreatography (ERCP). This is a combined endoscopic-radiographic examination method which is the gold standard in the diagnosis of pancreatic tumors, especially in patients with enlarged bile and pancreatic ducts. Most tumors are ductal adenocarcinomas, which affect and obstruct main pancreatic duct or its branches so ERCP provides best visualization. During examination with brush we can take material for cytologic analysis and in the same time take bioptic material and place a stent around stenosis (2,3). CTA is imaging method that shows good relationship between tumor lesions associated with the surrounding blood vessels and allows surgical-oncological team to take proper attitude in making a definitive preoperative decision about the future treatment of the patient. CT is the diagnostic method which identifies changes above 5mm and below these values it is not accurate. It is suitable for the detection, apart of enlarged lymph nodes also of distant metastases (4).
2. GOAL
The goal of our study was to give the EUS as endoscopic methods the right place in the preoperative staging of patients with pancreatic cancer and to correlate these results with the results of CT and CT angiography, radiology imaging methods.
3. MATERIAL AND METHODS
The study was a prospective-retrospective and was carried out over a period of two years during 2012 and 2013 at the Clinic of Gastroenterohepatology, Clinical Center of Sarajevo University. During the observed period we had 49 hospitalized patients suffering from pancreatic cancer 20 women and 29 men. Patients, apart by sex, were observed by age and the localization of tumor lesions. All the patients underwent percutaneous ultrasound, EUS, ERCP, CT and CT angiography and proximal endoscopy to the lower curve of the duodenum in order to identify infiltrate penetration in the duodenum. In all patients we determined the serum concentration of CEA and CA19-9. Regardless of the localization in all cases, we measured the size of tumor lesions and note it. Biopsy and cytology samples were sent to the Institute of Pathology for histological and cytological analysis, in order to confirm the clinical diagnosis. Statistical testing was performed using Fisher’s exact test in open-source software R.
4. RESULTS AND DISCUSSION
Testing of differences in diagnostic powers of three the methods: EUS, CT and CTA was performed using Fisher’s exact test in open-source software R. Tested are the following characteristics: involvement of blood vessels by infiltrating process (yes-no), involvement of lymph nodes (yes-no), presence of metastases (yes-no), infiltrated duodenum (yes-no) and tumor size (<30 mm, >= 30mm).
Figure 1.

CTA- tumor of pancreatic head with biliary stent implanted
Figure 2.
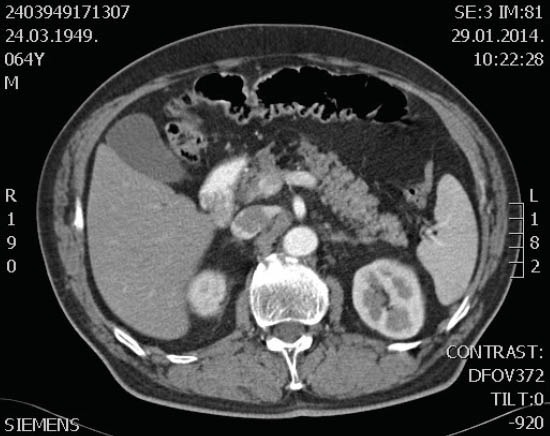
CT of pancreas by contrast method
Figure 3.
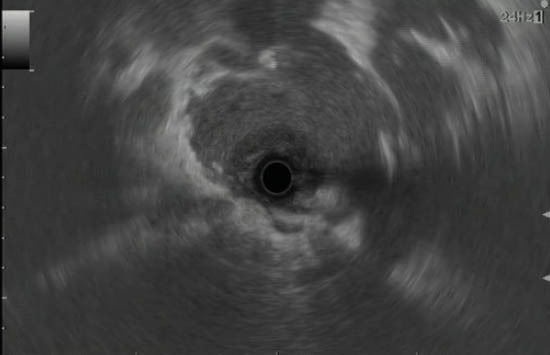
EUS of head of pancreatis cancer
Figure 4.
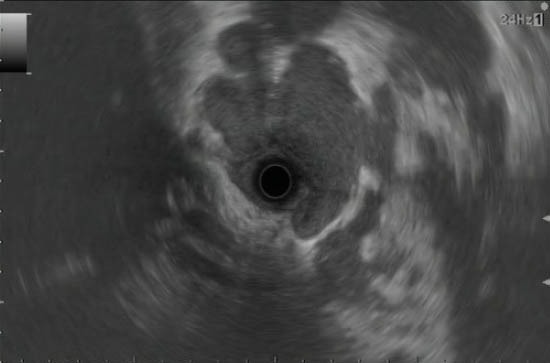
Pancreatic cancer
The difference in the EUS, CT and CTA methods is significant in identifying whether the blood vessels are affected or not. This was determined by using Fisher’s exact test, with which the obtained p-value of 0.0268 confirms that in the diagnosis these three methods significantly differ at the confidence level of 0.05.
Testing was also done for the other features, but it did not provide statistically significant results, so it was decided to analyze the efficiency of the method by pairs using (risk quotient) risk ratio with 95% confidence interval and the corrected p-value.
Risk ratio indicates that EUS is less effective in the diagnosis of vascular involvement then CTA, RR=0.52, CI 0.2–1.38, p-value=0.33.
On the other hand, EUS and CTA are equal in diagnosis whether the lymph nodes are affected with RR=1.3, CI 0.75–1.42), p-value=0.93. However, EUS is more effective than CT in approximately 40%, because the RR=1.37, CI 0.98–1.89, p-value=0.09.
By ability to detect distant metastases EUS is less effective than CT by approximately 30%, because the RR=0.73, CI 0.39–1.36, p-value=0.49, and less efficient then the CTA by approximately 20%, because the RR=0.79, CI 0.42–1.52, p-value=0.69. Thus, in identifying metastasis the most effective is CT, followed by CTA, and then EUS.
When it comes to diagnosing of the duodenum infiltration, EUS is somewhat less effective than CT by approximately 5%, because the RR=0.95, CI 0.27–3.32, p-value=0.76, but both methods showed as slightly less effective than CTA since a comparison of EUS and CTA gives RR=0.52, CI 0.2–1.38), p-value=0.33.
Tumor size is grouped into two categories due to the small sample size in the CT method (4), and CTA (11). In this case it is evident that the proportions in these two groups are similar for all three methods, but by EUS determined size in 38 patients, which directly provides it the advantage of efficiency in tumor diagnostics. In addition, similar proportions confirm its accuracy, so it could be said that in this case EUS is the most effective method.
Comparing our results with the results of other researchers we can say that Zoltan Berger at 2013 and his associates considered that ERCP although invasive, is the most sensitive method in the diagnosis of pancreatic cancer. EUS is highly sensitive examination method which is able to visualize malignant changes below 5 mm in comparison to other methods that cannot do this. Our findings confirm that EUS was the most dominant in detecting changes as well as their size in comparison to other methods. EUS is used in the definitive diagnosis of pancreatic cancer (5). The sensitivity of EUS-FNA in published studies ranging from 80-95% (6).
ERCP is the examination method used for many years but due to our small sample size, we statistically could not prove its dominance in the diagnosis. Jammie C. Wong and associates considered that imaging methods such as CT and CTA play a significant role in the diagnosis of pancreatic cancer. Their flaw is they are not able to visualize small lesions as demonstrated by our research (7). EUS, besides in the diagnosis of primary pancreatic cancer has a major role in the differential diagnosis of pancreatic lesions. According to Gheonei and associates its role is enhanced by using contrast agent for better visualization of pancreatic changes (8).
Canto M.I. and associates investigated the occurrence of pancreatic cancer and connects it with the genetic mutations, as well as with age and is considered that family history has an impact on the development of pancreatic cancer. In his research he concluded that EUS and MRI are better in detecting small pancreatic tumors then CT and that EUS detected significantly fewer lesions than CT in 42.6% of cases as our study show because in the detection of the size and location of tumor lesions EUS was ahead of CT and CTA (9).
Kucera S. and associates in their study gave advantage to EUS with fine needle aspiration in the diagnosis and analysis as well as in the classification of pancreatic cystic lesions (10).
In addition, also seen is CEA increase in cystic fluid of patients with cystic pancreatic cancer as progression actually is followed by an elevated concentration of CEA in cystic fluid. Our study showed high values of CEA and CEA 19-9 which are still late markers of pancreatic adenocarcinoma.
Sahani D.V and associates believes that the CA 19-9 is a tumor marker which is not significant in the early stage of pancreatic carcinoma as demonstrated by our research. He believes that EUS is superior to radiological methods in the diagnosis of early lesions and smaller cancerous lesions of the pancreas. EUS in 90% of cases reveals invasion of the portal vein with a malignant process.
5. CONCLUSION
EUS is proved as a more specific and sensitive method in localization and size of tumors lesion. In relation to CTA is less sensitive in determination of blood vessel infiltration. It is highly sensitive in detection of portal vein infiltration. EUS is more effective in regional lymph nodes affection then CT.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Tamm EP, Balachandran A, Bhosale P, Marcal L. Primary Pancreatic Adenocarcinoma. Appl Radiol. 2008;37(6):26–34. [Google Scholar]
- 2.Berger Z, Bufadee Godoy ME, Navarro Reveco A. Endoscopic Methods in the Diagnosis and Treatment of Pancreatic Cancer. Journal of Cancer Therapy. 2013;4:1–6. [Google Scholar]
- 3.Wang Z, Chen JQ, Liu JL, Qin XG, Huang Y. FDGPET in diagnosis, staging and prognosis of Pancreatic carcinoma: A meta-analisis. World J Gastroenterol. 2013;19(29):4808–4817. doi: 10.3748/wjg.v19.i29.4808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tummala P, Junaidi O, Agarwal B. Imaging of pancreatic cancer: An overview. J Gastrointest Oncol. 2011;2:168–174. doi: 10.3978/j.issn.2078-6891.2011.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saftoiu A, Vilmann P. Role of endoscopic ultrasaund in the diagnosis and staging of pancreatic cancer. J Clin Ultrasaund. 2009;37:1–17. doi: 10.1002/jcu.20534. [DOI] [PubMed] [Google Scholar]
- 6.Fisher JM, Gordon SR, Gardner TB. The impact of prior biliary stenting on the accuracy and complication rate of endoscopic ultrasaund fine-needle aspiration for diagnostic pancreatic adenocarcinoma. Pancreas. 2011;40:21–24. doi: 10.1097/MPA.0b013e3181f66e64. [DOI] [PubMed] [Google Scholar]
- 7.Wong J.C, Raman S. Surgical resectability of pancreatic adenocarcinoma: CTA. Abdom Imaging. 2010;35:471–480. doi: 10.1007/s00261-009-9539-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gheonea ID, Streba CT, Ciurea T, Saftoiu A. Quantitative low mechanical index contrast-enhanced endoscopic uoltrasaund for the differential diagnosis of chronic pseudotumoral pancreatitis and pancreatic cancer. Gastroenterology. 2013;13:2. doi: 10.1186/1471-230X-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canto MI, Harinck F, Hruban RH, Offerhaus GJ, Poley JW, Kamel I, Nio Y, Schulick RSW, Bassi C, Klujit I, Levy MJ, Chak A, Fockens P, Goggins M, Bruno M. International Cancer of the Pancreas Screening (CAPS) Consortium summit on the management of patients with increased risk for familial pancreatic cancer. Gut. 2013;62:339–347. doi: 10.1136/gutjnl-2012-303108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kucera S, Centeno BA, Springett G, Malaf MP, Chen YA, Weber J, Klapman J. Cyst Fluid Carcinoembryonic Antigen Level Is not Predictive of Invasive Cancer in Patients with Intraductal Papillary Mucinous neoplasm of the Pancreas. JOP. J Pancreas (On-line) 2012;13(4):409–413. doi: 10.6092/1590-8577/664. [DOI] [PubMed] [Google Scholar]
- 11.Sahani DV, Shah ZK, Catalano OA, Boland GW, Brugge WR. Radiology of Pancreatic Adenocarcinoma: Current Status of Imaging. J Gastroenterol Hepatol. 2008;23(1):23–33. doi: 10.1111/j.1440-1746.2007.05117.x. [DOI] [PubMed] [Google Scholar]


