Abstract
Introduction:
Family physician is the increasing efforts to promote physician and other human resources in the health care systems.
Goal:
Investigate Human resources situation of the family physician program in six pilot cities in Khuzestan province in the southwest of Iran.
Methods:
A cross-sectional descriptive study was conducted to examine the family physician program in 2011. In this study, 15 healthcare teams in six pilot cities in Iran were assessed. Data was compiled from family physician officer document in vice treatment of Ahwaz University of medical sciences. National instructions of family physician was used to identify current gaps.
Results:
The survey findings indicated that there is a doctor’s shortage about 36% in the health team that deployed in the first level of referral system. Also on the team, the 34% shortage of nurses and 60% shortages of nutrition personnel are seen. Specialists with offices in cities of second referral level, there have not welcomed the program.
Conclusions:
It seems that to facilitate patient access to physicians under contract with family physician program and the referral system in level two and level three, adopting arrangements to attract specialists and improving their maintenance is necessary.
Keywords: primary health care (PHC), family physician program, referral system, human resources
1. INTRODUCTION
Primary Health Care (PHC) was seen as indispensable element of health for all until 2000 in the world (1). It is the first level of contact of individuals, family and public with the national health system, brings health care as close as possible to the people that work and live and forms the first element of ongoing health care process (2). The current primary health care system in the Islamic Republic of Iran was confirmed for reducing the gap between health outcomes in rural and urban areas with an emphasis on improving access to health care (3). Firstly, PHC designed for rural and urban areas, but implemented comprehensive in villages and doesn’t establish in cities practically (4).
In network structure of health care arrangement in Iran referral system has defined (5). Referral system is a process where patients are treated at a lower level of health services, who do not have enough skills by virtue of his qualification and there is fewer facilities to manage a clinical condition, seeks the assistance of a better equipped and specially trained person, with better resources at a higher level, to guide him in handling or to take over the management of a special episode of a clinical condition in a benefit way (6). In large cities, GPs doesn’t have an obvious role as gate-keepers (7). To promote the quality of services, the government has established a health sector reform by introducing a new policy as family physician (8).
At this time, PHC is delivered by family physician team in the rural areas and urban areas in Iran (9). Family physicians provide coordinated health services for people and their families. In addition, they are enable in case finding, treatment, and prevention of disabilities (10). According to this, WHO propose family physician is the core in the world attempts for quality improvement, cost effectiveness, and equity in the health care systems (9).
Family Physician Program has been started since 2005 as a basic health plan in Iran. At the first step, all residents of villages and towns in the country, with under 20,000 people have get advantages in equal conditions and comfortable access to health services from this program. For a team of family physicians was assigned population about 2000 to 4000 people. Family physician teams consist of: GPs, midwives, providers of laboratory services and Pharmaceutical services. Currently, final steps of this program have been launched in Iran (11). If it fully completed, all urban and rural population will be covered.
The Alma Alta Declaration emphasizes on the access of acceptable levels of health for all, active public involvement in planning and organizing health care, and the participation of health care employees from physicians to community health staffs “to work as a health team and to respond to expressed health needs of the community” (12,13).
More resources are allocated to hospital care in most of the developing countries where a small part of the population is covered (14). One of the major barriers in improving the performance of health systems around the world has identified dramatic inequity and inadequate health personnel (15).
After several years of study and debate, the government decided that the development of family medicine as a specialty is benefit to the people (16). Considering that Human resources has an important role in organizational development and evolution (17) And we investigate Status of human resources in health centers for the six cities in Khuzestan province in west sought of Iran.
2. MATERIALS AND METHODS
This cross-sectional descriptive study conducted on 15 health team that established in healthcare centers in six cities consists of Baghmalek, Gotvand, Haftgol, Hendijan, Ramshir and Lali. These cities with populations of 20,000 to 50,000 people formed the first level of family physician program in Khuzestan province. All second and third level referral pathways for each of these six cities are defined.
The study population has been consisted of 196 members of health teams in the first level of referral system in pilot cities of family physician program. Pre-defined checklist have been prepared based on objectives was used to gather information in the first referral level and health team in pilot cities. This checklist was approved by experts and observers Family physician Program. The second and third referral levels data was compiled from family physician officer document in vice treatment of Ahwaz University of medical sciences. In addition to the information in the portal of this officer was used. All of the health team staff was compared based on existing and required position. Further, all of specialist physicians in second and third referral levels were separately compared. To display and summarize data tables, graphs and statistical indicators were used.
3. RESULTS
The family physician program that provide services by 15 health team in health care units in Khozestan province, has covered a population about 165301 people from six cities consist of Lali, Ramshir, Hendijan, Baghmelek, Gotvand and Haftgol [See table 1]. The findings show that Average distance from the first level to the second level is 43.6 km and Average distance from the second level to the third level is 120 km.
Table 1.
Information about pilot cities family physician program at the first referral level
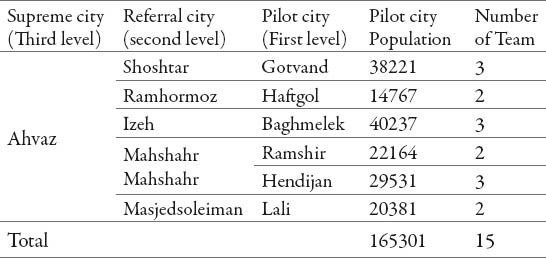
Table number 2 shows health team members include: physician, nurse, midwife, family health officer, health environment officer, Disease Control Experts, psychologist, nutrition officer, medical record officer and cleaner man at the first referral level.
Table 2.
The number of required, existing personnel and the percentage of staff shortage in deployed teams at the first referral level
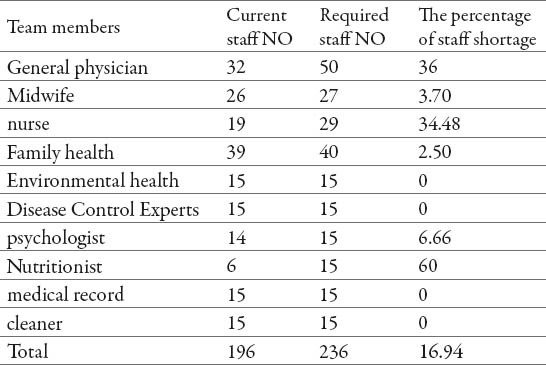
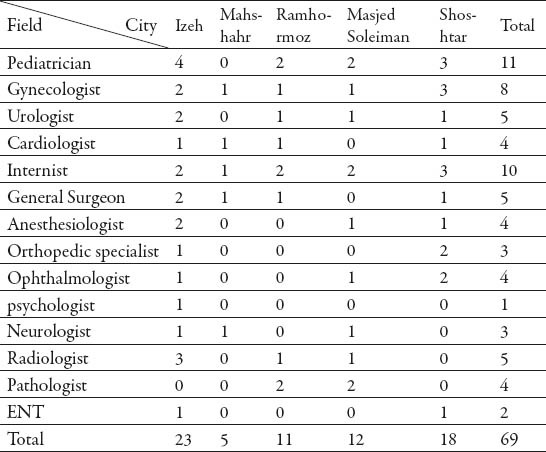
The results indicated that physician- population ratio is less than whatever that considers at national guidelines (1 physician for 4000 people). The most shortage in human resources was in nutritionist (60%) and nursing staff (34.48%) respectively. While, the work forces of health environment, combating with Disease Control Experts, medical records and cleaner 100% is required. In total, about 16.94% of the manpower shortage in the province was. According to Table 3, total number of registered specialists in the family physician program was 69 people. The most number registered specialists was related to Izeh city (23) and the lowest number in Mahshahr city (5). also the most number of registered specialists was pediatrician (11) and the least was psychologist (1), respectively. As we show in graph 1, the most frequency specialist field that registered in family physician program in Ahwaz–the center of Khuzestan province–has been general surgery and the lowest number specialist has been in the fields of plastic surgery, physical medicine, nuclear medicine, nephrology(14 cases) and neurology (1 case in every field.)
Table 3.
Frequency of specialists enrolled in the family physician program in second referral level cities
Graph 1.
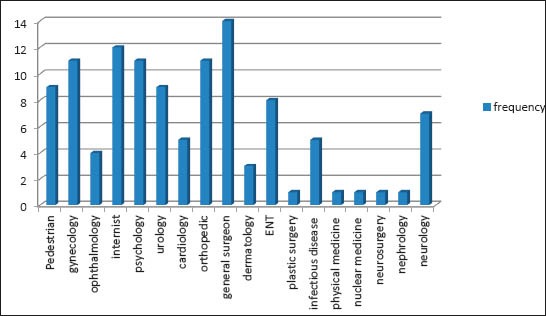
Frequency of specialist field enrolled in the family physician program in Ahwaz city in the third referral system
4. DISCUSSION
As the findings showed, 36% shortage of physician is seen in health teams deployed in the first level which is a significant problem. Despite the importance of all occupations and defined positions in the health teams, the main task of service delivery is related to physician. With the current trend can be expected that the quality of services in the long term, and also the willingness of people using the services of family physicians in this province is reduced. Health team physician at the first level referral system is responsible for diagnosis, treats and refers patient to higher levels. In addition to he/she has an important task to fill and complete patient health record. This deficiency may be interfered in proper completion of patient health records which is the default and requirements of family physician program. So, it is recommended that adequate number of physician must be allocated in this area after proper estimating the target population and according to standard criteria. The use of auxiliary personnel (GP or nurse trained) in a screening system to reduce the workload of doctors and optimum use of their working time is another proposed solution. Various studies have indicated that self- referral is caused emergency units and hospitals are crowded. Workload of Higher levels units can be reduced, if all patients are screened by a GP (18). The shortage of other personnel requirements can also be effective in the quality of services. Given the important role of nurses in family physician program, staff shortages this will affect the quality of service. Therefore, necessary measures should be taken to attract and retain them.
The present findings indicate that physician to population ratio compared with the maximum considered in national guidelines (1 to a maximum of 4,000) is less. It seems that these findings are consistent with another study that reported 40% of family physicians have covering a population of more than 4,000 people in Iran (19). It is worth noting that global standard for every 1,000 people are determined by a physician (20). Sufficient number of professional to meet the needs of population influences on access and using services. In this regards, the distribution of the health workforce can be suggested (21).
Although Physicians may have more motivation and satisfaction, if the population covered by each doctor in the family physician program increases, but comprehensive services and involvement of family physicians in people’s health issues will face challenges. We will be faced with a surplus of general practitioners in the community, despite the inadequacy of the active force, if policies and procedures in physician recruitment in family physician program are to attract doctors less than the standard rate. Hence, revision and review of elimination of executive barriers has higher priority than human resources training. In the other hand, one way to achieve the optimum performance in the program is human resources supply through revising the population is covered by family physician. In addition, it should not be neglected evaluating and removing barriers to maintenance physicians working in the program.
5. CONCLUSION
Forecasting and supply of skilled manpower is a major factor in the success of any plan. Ways to attract and keep staff should be carefully reviewed according to the requirements of each region. It is necessary to adopted arrangements to attract specialists and register them to facilitate patient access to specialist under contract in both second and third level. It seem that use of motivations (financial and non financial) and special privileges for increasing the participation rate of specialists in family physician program, is very effective. Finally, it suggested that to create a tendency for doctors to join and patients to use health services in all levels of referral system, the program is advertised through mass media like radio, TV and newspapers.
Acknowledgment:
We appreciate all family physicians experts working in the vice- chancellor of treatment, Jondishapur University of Medical Sciences in Ahwaz who helped us conducting this project.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Chinnock P. Word health Report calls for return to primary health care approach. Trop IKA, Net. 2008 [Google Scholar]
- 2.World Health Organization(WHO) Geneva: 1978. Alma-Ata Declaration: Primary Health Care. Available at: http://apps.who.int/iris/handle/10665/52703 . [Google Scholar]
- 3.Ministry of Health and Medical Education of Iran & United Nations Children's Fund (UNICEF) Population and health in the Islamic Republic of Iran-demographic and health survey. 2000 [Google Scholar]
- 4.HERIMP. Tehran: Higher Educational and Research Institute in Management and Planning; 2004. Proceedings of a Seminar of Challenges and Development Vision in Iran; pp. 19–26. [Google Scholar]
- 5.Mehrdad R. Health system in Iran. Japan Medical Association J. 2009;52(1):69–73. [Google Scholar]
- 6.Al-Mazrou YY, Al-Shehri S, Rao M. Riyadh: Directorate of Health Centres, Ministry of Health, Al-Helal Press; 1990. Principles and practice of primary health care. [Google Scholar]
- 7.Takian A. Implementing Family Medicine in Iran: Identification of Facilitators and Obstacles. PhD thesis submitted to the University of London, UK. 2009 [Google Scholar]
- 8.Takian A, Rashidian A, Kabir MJ. Expediency and coincidence in re-engineering a health system: an interpretive approach to formation of family medicine in Iran. Health policy and planning. 2011;26(2):163–173. doi: 10.1093/heapol/czq036. [DOI] [PubMed] [Google Scholar]
- 9.Khayyati FM, Esmaeilmotlagh MJ, Kabir Kazemeini H, Gharibi F, Jafari N. The role of family physician in case finding, referral, and insurance coverage in the rural areas. Iranian J Publ Health. 2011;40(3):136–139. [PMC free article] [PubMed] [Google Scholar]
- 10.Khuwaja AK, Khuwaja NK. Screening for diseases in family practice. J Pak Med Assoc. 2005;55(3):116–118. [PubMed] [Google Scholar]
- 11.Taheri M, Amani A, Zahir R, Mohammadi M. Patient satisfaction with Urban and Rural Insurance and Family Physician Program in Iran, Journal of Family and Reproductive Health. 2011;5(2):8–11. [Google Scholar]
- 12.World Health Organization(WHO) & United Nations Children's Fund (UNICEF) Strengthening Human Resources for Primary Health Care, International Conference on Primary Health Care. Alma Ata, USSR. 1978 [Google Scholar]
- 13.Maciocco G, Stefanini A. From Alma-Ata to the Global Fund: the history of international health policy, Revista Brasileira de Saúde Materno Infantil. 2007;7(4):479–486. [Google Scholar]
- 14.De Maeseneer J, Willems S, De Sutter A, Van de Geuchte I, Billings M. Primary health care as a strategy for achieving equitable care. Health Systems Knowledge Network of the World Health Organization's Commission on Social Determinants of Health. 2007 [Google Scholar]
- 15.World Health Organization. Geneva, Switzerland: World Health Organization; 2006. Working Together for Health: The World Health Report 2006. [Google Scholar]
- 16.LeBaron SWM, Schultz SH. Family Medicine in Iran: The Birth of a New Specialty. International Family Medicine. 2005;37(7):502–505. [PubMed] [Google Scholar]
- 17.Abolhalaj M, Hosainy-Parsa SH, Jafari-Sirizi M, Inanlou S. A situational analysis of human resources in Iranian hospitals affiliated with ministry of health in 2008. Journal of Shahrekord University of Medical Sciences. 2010;12(1):60–68. [Google Scholar]
- 18.Baghiani M, Ehrampoosh MH. Tehran: Asar sobhan publications; 2003. Principles of health services; p. 204. [Google Scholar]
- 19.Nasrollahpour Shirvani SD, Raeisee P, Motlagh ME, Kabir MJ, Ashrafian H Amiri. Evaluation of the performance of referral system in family physician program in Iran University of Medical Sciences 2009. Hakim Research Journal. 2010;13(1):19–25. [Google Scholar]
- 20.Farzadi F, Kazem M, Maftoun F, Labaf R, Hasemi G, Tabibzadeh Dezfouli R. General Practitioner Supply: Family Physician Program and Medical Workforce. Payesh. 2009;8(4):415–421. [Google Scholar]
- 21.Harris MF, Furler JS, Mercer SW, Willems SJ. Equity of Access to Quality of Care in Family Medicine. International Journal of Family Medicine. 2011 doi: 10.1155/2011/858131. [DOI] [PMC free article] [PubMed] [Google Scholar]


