Abstract
Chronic hepatitis B (CHB) is a condition of global prevalence and its sequelae include cirrhosis and hepatocellular carcinoma. The natural history of CHB is a complex interplay of virological, environmental and host factors. The dynamic relationship between the virus and host evolves over the duration of the infection and different phases of the disease have been observed and described. These have been conceptualized in terms of the state of balance between the host immune system and the hepatitis B virus and have been given the labels immune tolerant, immune clearance, immune control and immune escape although other nomenclature is also used. Host factors, such as age at infection, determine progression to chronicity. Virological factors including hepatitis B viral load, mutations and genotype also have an impact on the adverse outcomes of the infection, as do hepatotoxic cofactors such as alcohol. Our understanding of the natural history of CHB has evolved significantly over the past few decades and characterizing the phase of disease of CHB remains an integral part of managing this virus in the clinic.
Keywords: Hepatitis B, Fibrosis, Natural history, Hepatitis B e antigen, Liver, Cirrhosis, Hepatocellular carcinoma, Genotype
Core tip: Hepatitis B is a disease of worldwide significance. It involves a complex interplay of viral, host and environmental factors. This review article on the natural history of chronic hepatitis B focuses on the phases of disease. We outline the historical development of these concepts. We describe the specific characteristics of different phases, e.g., the patterns of alanine transaminase abnormalities in the hepatitis B e antigen positive immune clearance phase. Lastly, we review some of the more recent data in relation to the outcomes of various phases, in particular the development of cirrhosis and hepatocellular carcinoma.
EPIDEMIOLOGY: GLOBAL
Hepatitis B is a major, worldwide, public health problem. Current World Health Organization estimates for the prevalence of hepatitis B infection are that 240 million people have chronic infection and that approximately 600000 people die every year due to the acute or chronic complications of the virus[1]. Estimates from around 2004 suggested that 2 billion people worldwide have been exposed to the hepatitis B virus (HBV)[2]. The rates of chronic carriage of hepatitis B surface antigen (HBsAg) can be up to 20% or more in some countries, and the proportion of patients with serology reflecting previous exposure to HBV (hepatitis B core Ab and hepatitis B surface Ab) can be up to 70%-95%[3]. Asia and the Western Pacific have the highest proportion of chronic hepatitis B (CHB) with 75% of the world’s CHB population being concentrated in these countries[4]. Globally overall, 30% of cirrhosis and 53% of hepatocellular carcinoma (HCC) has been calculated to be attributable to hepatitis B infection. In certain regions of the world e.g., Africa and China, that proportion is even higher[5]. The prevalence of HBV infection varies in different countries[6]. Countries of low, medium and high prevalence have been identified and these differ in many ways including predominant mode of transmission and age at infection[7,8] (Table 1). The natural history of CHB is considered to evolve through a number of clinical phases reflecting different points in the host-virus immune relationship. These phases have differing patterns of HBV viral load, hepatitis B e antigen (HBeAg) status and serum transaminase concentration. The concept of different phases has been critical to our understanding of CHB. It gives clues to the likely time and mode of infection, provides prognostic information on likelihood of fibrosis progression and directs clinicians on the appropriate course of management.
Table 1.
Geographical variation in hepatitis B prevalence and patterns of transmission[8]
| Pattern of prevalence | Geographical area | Percent of population HBsAg positive | Predominant age at infection | Predominant mode of transmission |
| High ≥ 8% | Southeast Asia, China, Pacific Islands, Sub- Saharan Africa | 8%-20% | Perinatal and early childhood | Maternal-infant, percutaneous (e.g., unsterile medical equipment used in vaccination, traditional medicine practices) |
| Intermediate 2%-7% | Eastern Europe, the Mediterranean basin, Middle East, Central and South Asia, Japan, Central and South America | 2%-7% | Early childhood/adolescence | Percutaneous (e.g., horizontal transmission between children through open wounds/cuts), sexual |
| Low < 2% | United States and Canada, Western Europe, Australia and New Zealand | 0.2%-0.5% | Adult | Sexual, percutaneous (e.g., intravenous drug use) |
HBsAg: Hepatitis B surface antigen.
NATURAL HISTORY OF HBV INFECTION
The natural history of CHB is determined by a complex interplay of viral, host and environmental factors (Figure 1)[9]. The influence of specific virological factors, on the course of CHB, is being increasingly recognized. For example, genotype can influence timing of seroconversion, but there is also evidence of an impact on adverse clinical outcomes. Genotype C compared to B[10] and genotype D compared to A[11] have been associated with more severe liver disease. The risk of developing HCC has been suggested to be increased in young patients with genotype B (especially those < 35 years)[12]. Specific viral mutations have been shown to be an independent risk factor for advanced liver disease, in particular the basal core promotor mutation[13]. HBV DNA levels have been shown to be a very strong predictor of cirrhosis and HCC in a cohort of over 3000 patients[14,15]. Environmental influences including co-infection with other hepatitis viruses (C or D) or human immunodeficiency virus, coexistent sources of liver injury such as in alcoholic or fatty liver disease and exposure to other infectious agents such as schistosomiasis or carcinogens like aflatoxin in parts of the developing world, also have a bearing on the development of cirrhosis or HCC in hepatitis B patients[16].
Figure 1.
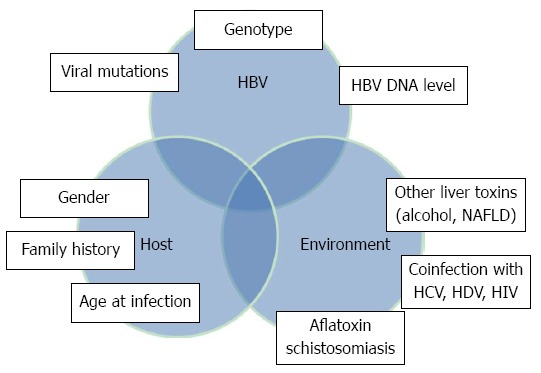
Factors interacting to affect the natural history of chronic hepatitis B. HBV: Hepatitis B virus; HIV: Human immunodeficiency virus; HDV: Hepatitis D virus; HCV: Hepatitis C virus; NAFLD: Non-alcoholic fatty liver disease.
The host immunological response plays a key role in the natural history of HBV, both at the time of acute infection (in determining whether viral clearance ensues) and during chronic infection where the injury to the liver is caused primarily by the host immune cells, rather than from direct viral cytopathic effect. Progression from acute to chronic infection is thought to occur in about 90% of patients infected perinatally, approximately 20% of patients infected during childhood and < 5% of patients infected as adults[9].
HISTORICAL OVERVIEW OF HBV AND THE PHASES OF DISEASE
Blumberg et al[17] reported in 1967 on the discovery of a novel antibody found in the serum of a multiply transfused hemophilia patient. This antibody reacted with only 1 of 24 sera against which it was tested. The reacting serum came from an Australian aborigine hence the antigen was named the “Australia antigen”. Shortly afterwards it was noted that this viral protein was associated with hepatitis, especially “long incubation” viral hepatitis[18] and post transfusion hepatitis[19]. The Australia antigen was subsequently renamed HBsAg and it was noted that HBsAg positive patients could fall into 2 clinical categories; those with evidence of liver disease (abnormal alanine aminotransferase (ALT) and necroinflammation on liver biopsy) and those without, who were termed “healthy” HBsAg carriers[20,21].
The natural history of HBV infection was then observed by groups from different parts of the world and differences in the serological profiles and clinical courses of HBV infected patients from these different regions emerged. For example, an early follow-up study by Hoofnagle of 25 HBsAg and HBeAg positive individuals showed loss of HBeAg and normalisation of ALT in 13, while in the other 12 HBeAg persisted as did elevation of ALT[22]. Loss of HBeAg and development of antibodies to this antigen (HBeAb) represents “e-antigen seroconversion” a state that heralds a change in the host’s reaction to the virus[22,23]. Therefore 2 sequential phases of CHB were proposed; a “replicative” and “non-replicative” phase. However, observation of Asian patients identified an early phase with HBeAg positivity and very high HBV DNA levels but normal ALT and liver histology. This was noted in both children and young adults who had presumably acquired HBV perinatally. It was thought to represent an initial immune tolerant phase and this was a further integral contribution to the understanding of HBV’s natural history[24,25]. A fourth phase of HBV was subsequently added to the natural history schema in which viral replication returned in patients positive for HBeAb and this was associated with abnormal liver tests. This phase was described as “reactivation”[26-28].
CLASSIFICATION OF PHASES OF DISEASE OF CHB
The nomenclature for the phases of disease has evolved over time and varies slightly between different international societies. For example, the National Institutes of Health sponsored workshops in the United States in 2000 and 2006 defined 3 phases of chronic HBV infection: the “immune tolerant phase”, the “immune active phase” (encompassing both HBeAg positive and HBeAg negative patients with elevated ALT, although with different thresholds for HBV DNA elevation) and the “inactive” hepatitis B phase[29,30]. This followed on partly from the clinic-pathological work of Chu et al[24] in the 1980s. Meanwhile at a 2006 workshop in Frankfurt of the European viral hepatitis educational initiative, the terminology “immune tolerant”, “immune clearance”, “immune control” and “immune escape” was used. They were applied to the 4, largely sequential, HBeAg positive (phases 1 and 2) and HBeAg negative (phases 3 and 4) CHB disease states[31] (Figure 2). The term “recovery phase”, for resolved hepatitis B (HBsAg negative, HBcAb positive) has also been proposed[16,32]. Australian guidelines published by the Digestive Health Foundation of the Gastroenterological Society of Australia in 2009 also use the 4 phase immune based terminology[33]. Currently, the guidelines of the 3 major international associations for the study of liver disease, American Association of the study of liver diseases (AASLD), European Association for the study of the liver (EASL) and Asian Pacific Association for the study of the liver (APASL) use similar definitions to describe the phases but slightly different nomenclature as outlined in Table 2[34-36]. It must be noted that not all patients with CHB go through all phases. Furthermore the duration of time spent in different phases differs and transition from one phase to the next may be so fast that distinct phases may not be recognizable in clinical practice.
Figure 2.
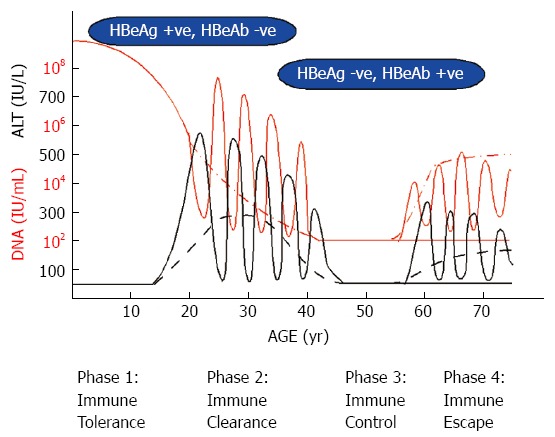
Natural history and phases of chronic hepatitis B. The figure represents the possible courses of perinatally acquired chronic hepatitis B and progression through different phases. The red line represents hepatitis B virus DNA with fluctuations in viral load during flares while dashed red represents an alternative course. The black line represents alanine aminotransferase (ALT) with the dashed black line representing persistent elevation of ALT while the solid line represents intermittent elevation of ALT and flares. HBeAg: Hepatitis B e antigen; HBeAb: Antibodies to HBeAg.
Table 2.
Phases of disease in chronic hepatitis B
| Phase 1 | Phase 2 | Phase 3 | Phase 4 | |
| Immune tolerance | Immune clearance | Immune control | Immune escape | |
| Serology | HBeAg positive | HBeAg positive | HBeAg negative | HBeAg negative |
| HBeAb negative | HBeAb negative | HBeAb positive | HBeAb positive | |
| ALT (IU/mL) | Persistently normal | Persistently or intermittently abnormal | Persistently normal | Persistently or intermittently abnormal |
| HBV DNA (IU/mL) | Very high (usually > 2 × 106-2 × 107) | High but less so than in Immune tolerant phase | < 2000 IU/mL (but up to 20000 IU/mL) | > 2000 IU/mL (fluctuating) |
| Liver histology | Normal or mild hepatitis | Moderate or severe necroinflammation and fibrosis | Normal or mild inflammation | Moderate to severe inflammation and fibrosis ± cirrhosis |
| Specific features | Age usually young (< 20-30 yr). Phase absent or very short in Mediterranean CHB | Intermittent flares or ongoing mild elevation of ALT. Ends with seroconversion to HBeAb positive state | May have serum HBsAg levels < 1000 IU/mL | Predominance of HBV with precore/basal core promotor mutations |
| Alternative nomenclature | Immunotolerant | HBeAg positive immune active (AASLD)/immune reactive HBeAg positive phase (EASL) | Inactive HBsAg carrier state (EASL and AASLD)/residual or inactive chronic HBV infection (APASL) | HBeAg negative CHB (EASL)/reactivation or relapse (APASL) |
Adapted from Ref [33]. CHB: Chronic hepatitis B; AASLD: American Association of the study of liver diseases; EASL: European Association for the study of the liver; APASL: Asian Pacific Association for the study of the liver; ALT: Alanine aminotransferase; HBV: Hepatitis B virus; HBsAg: Hepatitis B surface antigen; HBeAg: Hepatitis B e antigen.
IMMUNE TOLERANT PHASE
The key features of this phase are HBeAg positivity, very high serum HBV DNA levels (usually > 2 × 106-2 × 107 IU/mL) but normal ALT levels and minimal or absent inflammation or fibrosis on liver biopsy. Current Australian guidelines include HBV DNA levels of > 20000 IU/mL for definition of this phase. The immune tolerant phase is classically seen in Asian children infected perinatally with HBV and can last for several decades[37]. The phase is also seen in childhood acquired, horizontal infection but is thought to be of much shorter duration[38]. An early study by Lok and Lai in Chinese children in the immune tolerant phase (43 HBeAg positive children, median age 10, followed for a median of 24 mo) showed that HBV DNA levels were highest in the youngest children. They also demonstrated that while average ALT levels were similar at the first and last follow-up visits, being 25 and 20 IU/mL respectively, mild transient elevations of ALT, sometimes accompanied by changes in HBV DNA were noted during follow-up[25]. Liver histology in the immune tolerant phase shows non-specific histologic change[39]. A 2007 study from Hong Kong of paired liver biopsies showed little or no histological fibrosis on initial liver biopsy (median fibrosis Ishak stage 1) in 57 adult immune tolerant patients and a very low rate of progression over 5 years[40]. A paired transient elastography study with liver stiffness measurements in HBeAg positive patients, 74 in the immune tolerant phase and 137 in the immune reactive phase, similarly found low rates of fibrosis progression, 4.2% and 6.6% for the aforementioned groups respectively, over a 42 mo period[41]. In contrast, Lai et al[42] recently found that a fibrosis stage of 2 or greater could be seen in 18% of HBeAg-positive subjects with persistently normal ALT (defined as ALT < 40 on at least 2 occasions over at least 6 mo). However, the authors acknowledge that few of their persistently normal ALT patients truly fit the picture of immune tolerance being older or with lower viral loads. They suggest that the term be reserved for young patients with HBV DNA > 108 copies/mL and “low normal” ALT[42]. The “loss” of immune tolerance typically occurs during the second and third decades[8] and was noted to occur at a median age of 30.7 years in a retrospective study of 40 HBeAg positive patients with normal ALT and HBV DNA > 107 copies/mL[43]. Increasing age has been shown to predict adverse outcomes in HBeAg positive patients[42,44]. These data therefore make it important for clinicians to be vigilant in evaluating and monitoring older HBeAg positive patients in the immune tolerant phase of disease - especially those with “high normal” or minimally elevated ALTs or intermittent elevation of ALT. Biopsy has been advocated for immune tolerant patients who are older than 40 years to assess degree of histologic damage[34]. Treatment has not generally been recommended during the immune tolerant phase because of the lack of proven efficacy. Early studies in children treated during the immune tolerant phase did not show increased rates of seroconversion either with interferon (IFN) or lamivudine[45,46]. However a recent case control study of 28 children in the immune tolerant phase, treated with lamivudine for 8 wk followed by IFN alpha for 44 wk, showed durable HBeAg seroconversion in 10/28 (36%) and HBsAg clearance in 6/28 (21.4%) after a mean follow-up of 21 mo[47].
IMMUNE CLEARANCE PHASE
The immune clearance phase is a phase of HBeAg positive CHB, characterized by intermittent or persistent elevation of ALT levels and high HBV DNA levels, although not as high as in the immune tolerant phase. This is a period of immune mediated liver damage as evidenced by necroinflammation on liver biopsy and varying degrees of fibrosis. A typical feature of this phase is the occurrence of spontaneous flares which represent an intensification of the immune response to HBV. Flares are often preceded by an increase in the HBV DNA level and thus may be precipitated by the increased levels of replicating wild-type virus[48] although the cause of this remains unclear. There are no strict definitions or criteria for flares however in early work done by several Asian groups the studies generally used ALT greater than 5-times the upper limit of normal (ULN) or an absolute elevation in ALT greater than 300 IU/mL. Histologically there is evidence of acute lobular hepatitis superimposed on changes of chronic viral hepatitis[49] but severe changes of bridging necrosis have also been described. Clinically, most flares are asymptomatic but some may be accompanied by symptoms of acute hepatitis. Hepatic decompensation can occur in approximately 5% of flares and has been shown to be predicted by HBV DNA levels of > 1.55 × 109 copies/mL (approximately 2.88 × 107 IU/mL)[50]. Flares may rarely result in fatality[51]. Factors predicting HBeAg seroconversion following a flare include alpha fetoprotein (AFP) greater than 100 ng/mL, presence of bridging necrosis on liver biopsy and also the degree of ALT elevation[52]. The chance of HBeAg seroconversion within 3 mo of a flare in patients with peak ALT levels > 5 × ULN was 46.4%. This was compared with 27.2% and 35.6% in patients with peak ALT levels 1.5-2 times ULN and 2-5 times ULN respectively. Those with peak ALT > 5 ULN as well as peak AFP levels > 100 ng/mL in this study had the highest chance of HBeAg seroconversion (57%) within three mo of the exacerbation[53]. The frequency with which flares occur was studied by Liaw et al[54] who found that in 237 HBeAg positive patients (mean follow-up of 24.5 mo), 199 episodes of flare (defined as ALT > 300 IU/mL) were noted in 148 (62%) patients. ALT flares are more common in men than women which may account for the higher rates of cirrhosis in men[55]. Although flares are a well recognized and frequent part of the natural course of hepatitis B, it is certainly wise also to consider superimposed infections with other hepatotropic viruses (hepatitis A, hepatitis C and hepatitis D) especially in patients with possible risk factors. The postpartum period, when immune reconstitution occurs following the relative immunosuppression of pregnancy, is a time of significant risk for HBV immune-mediated flares[56]. Although some data suggest that the prognosis following acute flares (ALT > 6 × ULN) is good, with a low rate of complications long term[57], severe acute exacerbation complicated by subacute hepatic failure carries an increased risk of cirrhosis[58]. In other patients there may be several abortive attempts at seroconversion associated with flares, with loss of HBeAg but then seroreversion (reappearance of HBeAg) being seen, especially in patients who have not yet developed HBeAb[59]. This, likewise, increases progression of fibrosis. The duration of the immune clearance phase has been shown recently to have a strong impact on the development of complications. Those who seroconvert after the age of 40 have a significantly higher risk of developing cirrhosis, HCC and HBeAg negative CHB than those whose seroconversion occurs before the age of 30 years[60].
OTHER PATTERNS OF ALT ABNORMALITY IN THE IMMUNE CLEARANCE PHASE: INDICATIONS FOR TREATMENT
In contrast to the dramatic ALT elevation seen in flares, Chu et al[61] showed that a certain proportion of patients only experience transient and mild elevation of serum ALT levels prior to seroconversion. There are also other data that suggest that the insidious but persistent damage caused by low level inflammation, manifest as ALT levels 1-2 × ULN portends the worst prognosis and the highest cumulative risk of developing complications of cirrhosis or HCC. These data were from a mixed cohort of HBeAg positive (39%) and negative patients whose median age at presentation was 38, however, the cumulative risk was similar in both the HBeAg positive and HBeAg negative patients[57]. Other data also show that a positive association between ALT and liver related morbidity begins at an ALT of > 20 IU/mL in women and > 30 IU/mL in men[62].
Thus, liver injury during the immune clearance phase of CHB may come about by different mechanisms. The guidelines for treatment published by APASL in 2008[36] and the AASLD in 2009[34] suggest that HBeAg positive patients aged less than 40 years with minimally elevated ALT (< 2 × ULN) need not be treated but may be observed. The 2012 EASL guidelines[35] allow that treatment may be considered in patients with ALT above ULN if they have a liver biopsy showing at least moderate necroinflammation and/or fibrosis whilst for those with “obviously active CHB” (defined as ALT > 2 × ULN and HBV DNA > 20000), treatment may be begun without liver biopsy. Decisions about institution of treatment in HBeAg positive CHB must be informed by knowledge of the likely course of disease and probable outcomes. Varying thresholds for defining the ULN for ALT complicate matters further. It seems likely that, in future, the management of HBeAg positive hepatitis B, will need to include lower thresholds for ALT and different ones for men and women. It also seems important that decisions about treatment should take into account age, since the risk of fibrosis increases with age and the likelihood of sustained viral suppression (a prolonged immune control phase) decreases with increasing age at seroconversion[60].
HBEAG TO HBEAB SEROCONVERSION
Various factors impact on the timing of HBeAg seroconversion, including age, genotype and age at acquisition of virus. In perinatally infected Asians, there is a prolonged period of immune tolerance and low rate of clearance of HBeAg until later life. Recent data from Hong Kong show that in a cohort of 1400 Chinese patients, approximately 15% of 441 patients in the 46-55 years age bracket were still HBeAg positive, and 20% of 352 in the 36-45 years age bracket were HBeAg positive[63]. The mean age of HBeAg seroconversion in 240 Asian immune tolerant patients was 31.3 ± 7 years[61]. In the Mediterranean area, there are differences in the age of seroconversion reported from centers in Italy vs Greece. For example, in a long term follow-up study of 70 Caucasian patients in Verona Italy, the mean age at seroconversion was 30 years (range: 13-65 years)[64]. However, numerous Greek studies have shown that seroconversion has occurred in almost 80% of patients by the second decade of life[8]. Genotype also impacts on the timing of seroconversion. In a retrospective study of 273 Chinese patients (122 with genotype B and 147 with genotype C), it was found that HBeAg seroconversion in genotype B patients occurred approximately 1 decade earlier than in genotype C patients[65]. Multivariate analysis showed that high ALT (baseline and during follow-up), age > 30 years and genotype B were independent factors associated with spontaneous HBeAg seroconversion[65]. Genotype D is also known to have a later seroconversion while, in contrast, genotype A is associated with earlier seroconversion[66].
It is interesting to consider the potential impact of better nutrition and living conditions (as well as viral co-infection) on immune response. A Canadian study of 70 adopted Asian-born children who were recruited at a mean age of 2 years, found that 75% had seroconverted over the subsequent 13 years. The viral genotype was not characterized in this study[67].
OUTCOMES OF HBEAG POSITIVE CHB AND SEROCONVERSION
HBeAg to HBeAb seroconversion may be followed by a prolonged and ideally lifelong transition to the inactive carrier state with eventual HBsAg loss. However, reaching this state of quiescence can take time, and following seroconversion there may be reversion to HBeAg positivity. In 512 Chinese patients aged 1-75 years, followed over 3 years, 7.8% of patients showed reversion from HBeAg negativity to an HBeAg positive state whilst 32.3% of HBeAg positive patients cleared HBeAg over the course of follow-up[59]. In terms of clinical outcomes, Chu et al[61] showed that the rate of development of cirrhosis in a group of 240 HBeAg positive patients followed up from the immune tolerant phase through to HBeAb seroconversion was 5%. The mean age at study entry was 27.6 ± 6.2 years and the mean age at HBeAg seroconversion was 31.3 ± 7 years. The annual incidence of cirrhosis was 0.5% and the factors predictive of the development of cirrhosis were age at HBeAg/HBeAb seroconversion and relapse of hepatitis which was seen in 15% of patients following HBeAg to HBeAb seroconversion.
Chen and Liaw[60] followed 483 patients from the time of confirmed HBeAb seroconversion and found that over a mean period of follow-up of 11.7 years, HBeAg negative hepatitis developed in 34%, cirrhosis in 10% and HCC in 2.5%. However, the rates of HBeAg negative hepatitis and cirrhosis were significantly higher (at 67% and 43% respectively) in patients whose seroconversion occurred after age 40. The lowest risk was in patients who seroconverted before the age of 30 (31% risk of HBeAg negative hepatitis and 3.7% of cirrhosis). Following seroconversion, the duration of remission, prior to relapse with HBeAg negative CHB, was significantly shorter in those whose seroconversion occurred after the age of 40 compared to those with seroconversion before age 30 years (6.2 years vs 9.5 years, P = 0.004).
IMMUNE CONTROL PHASE
Loss of HBeAg, development of HBeAb, normalization of ALT and reduction of HBV DNA levels to undetectable or very low levels signifies clinical remission of CHB and entry into the phase of “immune control” or the “inactive carrier state”. This phase of disease has had varying titles, as well as definitions over time. The ideal cut-off level of HBV DNA to define this state has been contested over the last few years, decreasing from 100000 copies/mL to 30000 copies/mL[29,68] and further still more recently. Most current guidelines use the level of 2000 IU/mL[34] although acknowledging that levels up to 20000 IU/mL may be seen[35]. The REVEAL-HBV study identified an increased risk for the development of cirrhosis and HCC beginning at a threshold of 2000 IU/mL[14,15]. However several recent studies have lent support to use of the threshold of 20000 IU/mL in place of 2000 IU/mL to define the inactive carrier state. Chen et al[69] looked at 62 patients with persistently normal ALT over 10 years and found HBV DNA levels were largely < 20000 IU/mL. Furthermore, a review of 6 studies of HBeAg negative patients with persistently normal ALT found that significant histological liver disease was rare in patients with persistently normal ALT, based on strict criteria, even in patients with HBV DNA up to 20000 IU/mL[70]. It is important that a patient should be shown to have normal ALT levels and 2-3 HBV DNA levels in the appropriate range (ideally < 2000 IU/mL) over the course of at least 1 year prior to classification into this phase of disease, since HBeAg negative CHB may run a fluctuating course. The prognosis for patients in the inactive carrier state is good. Although transition to HBeAg negative CHB can occur in approximately one third of patients[60,71], this risk decreases with time. Chu et al[72] reported that the proportional increase in risk of relapse was lower with longer follow-up, e.g., the cumulative incidence of relapse was 10.2% at 5 years and 17.4% at 10 years (7.2% increase from 6th to 10th year of follow up). Relapse however was seen in only 19.3% after 15 years, and 20.2% of patients at 20 years (representing only a 1.9% and 0.9% increase respectively for the 5 year blocks during the second decade of follow-up). It was reported to be negligible after 20 years of follow-up.
HBEAG NEGATIVE CHB
The state of active liver disease associated with HBeAg negativity due to the presence of mutations in the precore and/or basal core promotor region of HBV[73], was first recognized in countries around the Mediterranean basin. It has subsequently been recognized to be globally prevalent[74] and is currently the main form of CHB worldwide[75]. Patients in the HBeAg negative CHB phase are older and have higher rates of fibrosis than HBeAg positive patients[44]. A feature of this phase is also the fluctuating nature of ALT abnormality. Tai et al[76] showed that, in a group of 3673 HBeAg negative patients who began a 3 year followup period with normal ALT, those with an increase of ALT to at least 2 times ULN (ULN defined as 36 IU/mL) had a higher incidence of cirrhosis, HCC and mortality compared with those who maintained persistently normal ALT. The importance of HBV DNA concentration in this phase has also been shown in the REVEAL-HBV studies in which 85% of the cohort were HBeAg negative and in whom the risk of cirrhosis and HCC were correlated strongly with HBV DNA levels[14,15].
RESOLVED HEPATITIS B
In addition to the 4 phases outlined above, the EASL 2012[35] and AASLD 2009[34] guidelines also define the HBsAg negative phase, after HBsAg loss. In this phase low level HBV replication may persist with HBV DNA detectable in the liver, although usually not in the serum. The rates of HBsAg clearance was evaluated by Liaw et al[77] in a large cohort of patients divided into 2 groups, 984 with “CHB” (69.3% HBeAg positive) and 1598 “chronic HBV carriers” (with normal ALT, 28% HBeAg positive). HBsAg loss was noted in 19/984 (1.9%) patients with “CHB” and 35/1598 (2.2%) chronic HBV carriers with normal ALT followed up for 4 ± 2.3 years and 2.7 ± 1.4 years respectively. This translates to an annual rate of 0.5% in CHB patients and 0.8% in chronic carriers. HBsAg clearance only occurred after HBeAg seroconversion. The rate of HBsAg loss in this study is slightly higher than a previous small Asian study of HBsAg clearance in patients followed for at least 6 mo, in which only 1 of 323 chronic carriers cleared HBsAg[78]. However, the rates are lower than in older Caucasian group studies. Whilst loss of HBsAg is the closest endpoint we have to a cure from HBV infection, it should be appreciated that viral DNA can be archived within the host genome in the form of covalently closed circular DNA (cccDNA). The significance of resolved hepatitis B has gained importance especially in the setting of immunosuppression due to the risk of HBV reactivation. Some patients with HBsAg loss may still have detectable HBV DNA in the serum (occult HBV) and these individuals are particularly vulnerable to HBV reactivation following chemotherapy for hematological malignancies and breast cancer, and chemotherapy regimens that contain either steroids or rituximab[79,80].
NATURAL HISTORY OF ADULT-ACQUIRED HEPATITIS B
Although it is suggested that the rate of chronicity from adult-acquired hepatitis B is rare[81], the actual rates reported are variable. A recent study of 215 untreated patients from Japan, (mean age 31.8 years) with acute hepatitis B, found that 21 (9.8%) developed chronic infection defined as persistent HBsAg for > 6 mo. However, all but 6 (2.8%) had cleared HBsAg by 12 mo, and 5 of the 6 were genotype A. The rates of chronicity at 6 mo were 12.4% in genotype A, 3.8% in genotype B and 8.2% in genotype C. Looked at another way, 6% of genotype A patients with acute infection transitioned to chronicity. The authors propose that criteria for chronic infection be changed to HBsAg persistence at 12 mo rather than 6 mo in adult acquired hepatitis B. They report that higher HBV DNA levels and HBsAg levels early in the course of infection correlated with likelihood of chronicity[82].
CONCLUSION
Our understanding of the natural history of CHB has evolved greatly over the past 40 or so years. Further new studies continue to add information about differences in serological markers between different phases of disease. Nguyen et al[83] showed that the level of quantitative HBsAg could help differentiate between patients in various phases of CHB infection, being highest in patients in the immune tolerant phase of disease and lowest in those in the HBeAg negative low replicative phase. Specific virological factors can impact on natural history, for example, the likelihood of progression to chronicity (genotype in adult acquired HBV) and the risk of cirrhosis or HCC (HBV DNA level and BCP mutations). External factors including co-infection with HCV or HDV and other causes of liver injury can also influence the development of advanced fibrosis. Characteristics of the host, especially age at time of seroconversion and immune competence in those with resolved hepatitis B, also have a bearing on the future course of the disease. The phases of CHB as outlined above have been elucidated through the work of groups from all over the world over the past 40 years. They provide a useful framework within which to interpret overall risk for individual patients and remain a central part of the clinical assessment. Our conceptualization of the natural history of hepatitis B has evolved significantly over time, but it is likely that future insights will continue to improve our understanding of this complex virus and its dynamic interaction with its human host.
Footnotes
P- Reviewer: He ST, Hudacko R, Tetsuya T, Yang YF S- Editor: Gou SX L- Editor: Cant MR E- Editor: Liu XM
References
- 1.World Health Organization. Hepatitis B, fact sheet no.204, July. 2012. p. [cited 2012 Jul 16]. Available from: http://www.who.int/mediacentre/factsheets/fs204/en/index.
- 2.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 3.Previsani N, Lavanchy D. Hepatitis B. 2002. Available from: http://www.who.int/csr/disease/hepatitis/HepatitisB_whocdscsrlyo2002_2.pdf.
- 4.Gust ID. Epidemiology of hepatitis B infection in the Western Pacific and South East Asia. Gut. 1996;38 Suppl 2:S18–S23. doi: 10.1136/gut.38.suppl_2.s18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529–538. doi: 10.1016/j.jhep.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Margolis HS, Alter MJ, Hadler SC. Hepatitis B: evolving epidemiology and implications for control. Semin Liver Dis. 1991;11:84–92. doi: 10.1055/s-2008-1040427. [DOI] [PubMed] [Google Scholar]
- 7.Zuckerman A. Hepatitis Viruses. In: Baron S, editor. Medical Microbiology. 4 ed. Galveston Texas: The University of Texas medical Branch at Galveston; 1996. pp. 849–863. [Google Scholar]
- 8.Liaw YF, Brunetto MR, Hadziyannis S. The natural history of chronic HBV infection and geographical differences. Antivir Ther. 2010;15 Suppl 3:25–33. doi: 10.3851/IMP1621. [DOI] [PubMed] [Google Scholar]
- 9.Yim HJ, Lok AS. Natural history of chronic hepatitis B virus infection: what we knew in 1981 and what we know in 2005. Hepatology. 2006;43:S173–S181. doi: 10.1002/hep.20956. [DOI] [PubMed] [Google Scholar]
- 10.Chu CM, Liaw YF. Genotype C hepatitis B virus infection is associated with a higher risk of reactivation of hepatitis B and progression to cirrhosis than genotype B: a longitudinal study of hepatitis B e antigen-positive patients with normal aminotransferase levels at baseline. J Hepatol. 2005;43:411–417. doi: 10.1016/j.jhep.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Thakur V, Guptan RC, Kazim SN, Malhotra V, Sarin SK. Profile, spectrum and significance of HBV genotypes in chronic liver disease patients in the Indian subcontinent. J Gastroenterol Hepatol. 2002;17:165–170. doi: 10.1046/j.1440-1746.2002.02605.x. [DOI] [PubMed] [Google Scholar]
- 12.Kao JH, Chen PJ, Lai MY, Chen DS. Hepatitis B genotypes correlate with clinical outcomes in patients with chronic hepatitis B. Gastroenterology. 2000;118:554–559. doi: 10.1016/s0016-5085(00)70261-7. [DOI] [PubMed] [Google Scholar]
- 13.Kao JH, Chen PJ, Lai MY, Chen DS. Basal core promoter mutations of hepatitis B virus increase the risk of hepatocellular carcinoma in hepatitis B carriers. Gastroenterology. 2003;124:327–334. doi: 10.1053/gast.2003.50053. [DOI] [PubMed] [Google Scholar]
- 14.Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73. doi: 10.1001/jama.295.1.65. [DOI] [PubMed] [Google Scholar]
- 15.Iloeje UH, Yang HI, Su J, Jen CL, You SL, Chen CJ. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 2006;130:678–686. doi: 10.1053/j.gastro.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 16.McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009;49:S45–S55. doi: 10.1002/hep.22898. [DOI] [PubMed] [Google Scholar]
- 17.Blumberg BS, Gerstley BJ, Hungerford DA, London WT, Sutnick AI. A serum antigen (Australia antigen) in Down‘s syndrome, leukemia, and hepatitis. Ann Intern Med. 1967;66:924–931. doi: 10.7326/0003-4819-66-5-924. [DOI] [PubMed] [Google Scholar]
- 18.Giles JP, McCollum RW, Berndtson LW, Krugman S. Relation of Australia-SH antigen to the willowbrook MS-2 strain. N Engl J Med. 1969;281:119–122. doi: 10.1056/NEJM196907172810302. [DOI] [PubMed] [Google Scholar]
- 19.Blumberg BS, Sutnick AI, London WT. Hepatitis and leukemia: their relation to Australia antigen. Bull N Y Acad Med. 1968;44:1566–1586. [PMC free article] [PubMed] [Google Scholar]
- 20.Szmuness W, Prince AM. Epidemiologic patterns of viral hepatitis in eastern Europe in the light of recent findings concerning the serum hepatitis antigen. J Infect Dis. 1971;123:200–212. doi: 10.1093/infdis/123.2.200. [DOI] [PubMed] [Google Scholar]
- 21.Hadziyannis S, Merikas G, Panetsos S, Kourepi M. Hepatitis associated antigen carriers among blood donors in Greece. Am J Dis Child. 1972;123:381–383. doi: 10.1001/archpedi.1972.02110100113041. [DOI] [PubMed] [Google Scholar]
- 22.Hoofnagle JH, Dusheiko GM, Seeff LB, Jones EA, Waggoner JG, Bales ZB. Seroconversion from hepatitis B e antigen to antibody in chronic type B hepatitis. Ann Intern Med. 1981;94:744–748. doi: 10.7326/0003-4819-94-6-744. [DOI] [PubMed] [Google Scholar]
- 23.Realdi G, Alberti A, Rugge M, Bortolotti F, Rigoli AM, Tremolada F, Ruol A. Seroconversion from hepatitis B e antigen to anti-HBe in chronic hepatitis B virus infection. Gastroenterology. 1980;79:195–199. [PubMed] [Google Scholar]
- 24.Chu CM, Karayiannis P, Fowler MJ, Monjardino J, Liaw YF, Thomas HC. Natural history of chronic hepatitis B virus infection in Taiwan: studies of hepatitis B virus DNA in serum. Hepatology. 1985;5:431–434. doi: 10.1002/hep.1840050315. [DOI] [PubMed] [Google Scholar]
- 25.Lok AS, Lai CL. A longitudinal follow-up of asymptomatic hepatitis B surface antigen-positive Chinese children. Hepatology. 1988;8:1130–1133. doi: 10.1002/hep.1840080527. [DOI] [PubMed] [Google Scholar]
- 26.Bonino F, Rosina F, Rizzetto M, Rizzi R, Chiaberge E, Tardanico R, Callea F, Verme G. Chronic hepatitis in HBsAg carriers with serum HBV-DNA and anti-HBe. Gastroenterology. 1986;90:1268–1273. doi: 10.1016/0016-5085(86)90395-1. [DOI] [PubMed] [Google Scholar]
- 27.Hadziyannis SJ, Lieberman HM, Karvountzis GG, Shafritz DA. Analysis of liver disease, nuclear HBcAg, viral replication, and hepatitis B virus DNA in liver and serum of HBeAg Vs. anti-HBe positive carriers of hepatitis B virus. Hepatology. 1983;3:656–662. doi: 10.1002/hep.1840030505. [DOI] [PubMed] [Google Scholar]
- 28.Lok AS, Hadziyannis SJ, Weller IV, Karvountzis MG, Monjardino J, Karayiannis P, Montano L, Thomas HC. Contribution of low level HBV replication to continuing inflammatory activity in patients with anti-HBe positive chronic hepatitis B virus infection. Gut. 1984;25:1283–1287. doi: 10.1136/gut.25.11.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lok AS, Heathcote EJ, Hoofnagle JH. Management of hepatitis B: 2000--summary of a workshop. Gastroenterology. 2001;120:1828–1853. doi: 10.1053/gast.2001.24839. [DOI] [PubMed] [Google Scholar]
- 30.Hoofnagle JH, Doo E, Liang TJ, Fleischer R, Lok AS. Management of hepatitis B: summary of a clinical research workshop. Hepatology. 2007;45:1056–1075. doi: 10.1002/hep.21627. [DOI] [PubMed] [Google Scholar]
- 31.Thomas HC. Best practice in the treatment of chronic hepatitis B: a summary of the European Viral Hepatitis Educational Initiative (EVHEI) J Hepatol. 2007;47:588–597. doi: 10.1016/j.jhep.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45:507–539. doi: 10.1002/hep.21513. [DOI] [PubMed] [Google Scholar]
- 33.Australia DHFGSo. Australian and New Zealand Chronic Hepatitis B (CHB) Recommendations. Booklet of the Digestive Health Foundation 2009/10; 2nd Edition: 1-58. Available from: http://www.gesa.org.au/files/editor_upload/File/Professional/CHB.pdf.
- 34.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 35.European Association for the Study of the Live. Clinical Practice Guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 36.Liaw YF, Leung N, Kao JH, Piratvisuth, T, Gane E, Han KH, Guan R, Lau GK, Locarnini S; Chronic Hepatitis B Guideline Working Party of the Asian-Pacific Association for the Study of the Liver. Asian-Pacific consensus statement on the management of chronichepatitis B: a 2008 update. Hepatol Int. 2008;2:263–283. doi: 10.1007/s12072-008-9080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lok AS. Natural history and control of perinatally acquired hepatitis B virus infection. Dig Dis. 1992;10:46–52. doi: 10.1159/000171343. [DOI] [PubMed] [Google Scholar]
- 38.Hadziyannis SJ. Natural history of chronic hepatitis B in Euro-Mediterranean and African countries. J Hepatol. 2011;55:183–191. doi: 10.1016/j.jhep.2010.12.030. [DOI] [PubMed] [Google Scholar]
- 39.Chang MH, Hwang LY, Hsu HC, Lee CY, Beasley RP. Prospective study of asymptomatic HBsAg carrier children infected in the perinatal period: clinical and liver histologic studies. Hepatology. 1988;8:374–377. doi: 10.1002/hep.1840080231. [DOI] [PubMed] [Google Scholar]
- 40.Hui CK, Leung N, Yuen ST, Zhang HY, Leung KW, Lu L, Cheung SK, Wong WM, Lau GK. Natural history and disease progression in Chinese chronic hepatitis B patients in immune-tolerant phase. Hepatology. 2007;46:395–401. doi: 10.1002/hep.21724. [DOI] [PubMed] [Google Scholar]
- 41.Wong GL, Chan HL, Yu Z, Chan HY, Tse CH, Wong VW. Liver fibrosis progression in chronic hepatitis B patients positive for hepatitis B e antigen: a prospective cohort study with paired transient elastography examination. J Gastroenterol Hepatol. 2013;28:1762–1769. doi: 10.1111/jgh.12312. [DOI] [PubMed] [Google Scholar]
- 42.Lai M, Hyatt BJ, Nasser I, Curry M, Afdhal NH. The clinical significance of persistently normal ALT in chronic hepatitis B infection. J Hepatol. 2007;47:760–767. doi: 10.1016/j.jhep.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 43.Andreani T, Serfaty L, Mohand D, Dernaika S, Wendum D, Chazouillères O, Poupon R. Chronic hepatitis B virus carriers in the immunotolerant phase of infection: histologic findings and outcome. Clin Gastroenterol Hepatol. 2007;5:636–641. doi: 10.1016/j.cgh.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 44.Croagh CM, Bell SJ, Slavin J, Kong YX, Chen RY, Locarnini S, Desmond PV. Increasing hepatitis B viral load is associated with risk of significant liver fibrosis in HBeAg-negative but not HBeAg-positive chronic hepatitis B. Liver Int. 2010;30:1115–1122. doi: 10.1111/j.1478-3231.2010.02267.x. [DOI] [PubMed] [Google Scholar]
- 45.Torre D, Tambini R. Interferon-alpha therapy for chronic hepatitis B in children: a meta-analysis. Clin Infect Dis. 1996;23:131–137. doi: 10.1093/clinids/23.1.131. [DOI] [PubMed] [Google Scholar]
- 46.Jonas MM, Mizerski J, Badia IB, Areias JA, Schwarz KB, Little NR, Greensmith MJ, Gardner SD, Bell MS, Sokal EM. Clinical trial of lamivudine in children with chronic hepatitis B. N Engl J Med. 2002;346:1706–1713. doi: 10.1056/NEJMoa012452. [DOI] [PubMed] [Google Scholar]
- 47.Poddar U, Yachha SK, Agarwal J, Krishnani N. Cure for immune-tolerant hepatitis B in children: is it an achievable target with sequential combo therapy with lamivudine and interferon? J Viral Hepat. 2013;20:311–316. doi: 10.1111/jvh.12007. [DOI] [PubMed] [Google Scholar]
- 48.Perrillo RP. Acute flares in chronic hepatitis B: the natural and unnatural history of an immunologically mediated liver disease. Gastroenterology. 2001;120:1009–1022. doi: 10.1053/gast.2001.22461. [DOI] [PubMed] [Google Scholar]
- 49.Perrillo RP, Campbell CR, Sanders GE, Regenstein FG, Bodicky CJ. Spontaneous clearance and reactivation of hepatitis B virus infection among male homosexuals with chronic type B hepatitis. Ann Intern Med. 1984;100:43–46. doi: 10.7326/0003-4819-100-1-43. [DOI] [PubMed] [Google Scholar]
- 50.Jeng WJ, Sheen IS, Liaw YF. Hepatitis B virus DNA level predicts hepatic decompensation in patients with acute exacerbation of chronic hepatitis B. Clin Gastroenterol Hepatol. 2010;8:541–545. doi: 10.1016/j.cgh.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 51.Sheen IS, Liaw YF, Tai DI, Chu CM. Hepatic decompensation associated with hepatitis B e antigen clearance in chronic type B hepatitis. Gastroenterology. 1985;89:732–735. doi: 10.1016/0016-5085(85)90566-9. [DOI] [PubMed] [Google Scholar]
- 52.Liaw YF, Chu CM, Huang MJ, Sheen IS, Yang CY, Lin DY. Determinants for hepatitis B e antigen clearance in chronic type B hepatitis. Liver. 1984;4:301–306. doi: 10.1111/j.1600-0676.1984.tb00942.x. [DOI] [PubMed] [Google Scholar]
- 53.Yuen MF, Yuan HJ, Hui CK, Wong DK, Wong WM, Chan AO, Wong BC, Lai CL. A large population study of spontaneous HBeAg seroconversion and acute exacerbation of chronic hepatitis B infection: implications for antiviral therapy. Gut. 2003;52:416–419. doi: 10.1136/gut.52.3.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liaw YF, Yang SS, Chen TJ, Chu CM. Acute exacerbation in hepatitis B e antigen positive chronic type B hepatitis. A clinicopathological study. J Hepatol. 1985;1:227–233. doi: 10.1016/s0168-8278(85)80050-7. [DOI] [PubMed] [Google Scholar]
- 55.Lok AS, Lai CL. Acute exacerbations in Chinese patients with chronic hepatitis B virus (HBV) infection. Incidence, predisposing factors and etiology. J Hepatol. 1990;10:29–34. doi: 10.1016/0168-8278(90)90069-4. [DOI] [PubMed] [Google Scholar]
- 56.Sinha S, Kumar M. Pregnancy and chronic hepatitis B virus infection. Hepatol Res. 2010;40:31–48. doi: 10.1111/j.1872-034X.2009.00597.x. [DOI] [PubMed] [Google Scholar]
- 57.Yuen MF, Yuan HJ, Wong DK, Yuen JC, Wong WM, Chan AO, Wong BC, Lai KC, Lai CL. Prognostic determinants for chronic hepatitis B in Asians: therapeutic implications. Gut. 2005;54:1610–1614. doi: 10.1136/gut.2005.065136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chu CM. Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol. 2000;15 Suppl:E25–E30. doi: 10.1046/j.1440-1746.2000.02097.x. [DOI] [PubMed] [Google Scholar]
- 59.Lok AS, Lai CL, Wu PC, Leung EK, Lam TS. Spontaneous hepatitis B e antigen to antibody seroconversion and reversion in Chinese patients with chronic hepatitis B virus infection. Gastroenterology. 1987;92:1839–1843. doi: 10.1016/0016-5085(87)90613-5. [DOI] [PubMed] [Google Scholar]
- 60.Chen YC, Chu CM, Liaw YF. Age-specific prognosis following spontaneous hepatitis B e antigen seroconversion in chronic hepatitis B. Hepatology. 2010;51:435–444. doi: 10.1002/hep.23348. [DOI] [PubMed] [Google Scholar]
- 61.Chu CM, Hung SJ, Lin J, Tai DI, Liaw YF. Natural history of hepatitis B e antigen to antibody seroconversion in patients with normal serum aminotransferase levels. Am J Med. 2004;116:829–834. doi: 10.1016/j.amjmed.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 62.Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328:983. doi: 10.1136/bmj.38050.593634.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fung J, Seto WK, Lai CL, Yuen J, Wong DK, Yuen MF. Profiles of HBV DNA in a large population of Chinese patients with chronic hepatitis B: implications for antiviral therapy. J Hepatol. 2011;54:195–200. doi: 10.1016/j.jhep.2010.06.031. [DOI] [PubMed] [Google Scholar]
- 64.Fattovich G, Olivari N, Pasino M, D’Onofrio M, Martone E, Donato F. Long-term outcome of chronic hepatitis B in Caucasian patients: mortality after 25 years. Gut. 2008;57:84–90. doi: 10.1136/gut.2007.128496. [DOI] [PubMed] [Google Scholar]
- 65.Chu CJ, Hussain M, Lok AS. Hepatitis B virus genotype B is associated with earlier HBeAg seroconversion compared with hepatitis B virus genotype C. Gastroenterology. 2002;122:1756–1762. doi: 10.1053/gast.2002.33588. [DOI] [PubMed] [Google Scholar]
- 66.Liu CJ, Kao JH. Global perspective on the natural history of chronic hepatitis B: role of hepatitis B virus genotypes A to J. Semin Liver Dis. 2013;33:97–102. doi: 10.1055/s-0033-1345716. [DOI] [PubMed] [Google Scholar]
- 67.Marx G, Martin SR, Chicoine JF, Alvarez F. Long-term follow-up of chronic hepatitis B virus infection in children of different ethnic origins. J Infect Dis. 2002;186:295–301. doi: 10.1086/341508. [DOI] [PubMed] [Google Scholar]
- 68.Manesis EK, Papatheodoridis GV, Sevastianos V, Cholongitas E, Papaioannou C, Hadziyannis SJ. Significance of hepatitis B viremia levels determined by a quantitative polymerase chain reaction assay in patients with hepatitis B e antigen-negative chronic hepatitis B virus infection. Am J Gastroenterol. 2003;98:2261–2267. doi: 10.1111/j.1572-0241.2003.07715.x. [DOI] [PubMed] [Google Scholar]
- 69.Chen YC, Huang SF, Chu CM, Liaw YF. Serial HBV DNA levels in patients with persistently normal transaminase over 10 years following spontaneous HBeAg seroconversion. J Viral Hepat. 2012;19:138–146. doi: 10.1111/j.1365-2893.2011.01450.x. [DOI] [PubMed] [Google Scholar]
- 70.Papatheodoridis GV, Manolakopoulos S, Liaw YF, Lok A. Follow-up and indications for liver biopsy in HBeAg-negative chronic hepatitis B virus infection with persistently normal ALT: a systematic review. J Hepatol. 2012;57:196–202. doi: 10.1016/j.jhep.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 71.Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, Liaw YF. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522–1527. doi: 10.1053/jhep.2002.33638. [DOI] [PubMed] [Google Scholar]
- 72.Chu CM, Liaw YF. Spontaneous relapse of hepatitis in inactive HBsAg carriers. Hepatol Int. 2007;1:311–315. doi: 10.1007/s12072-007-9002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hadziyannis S, Vassilopoulos D. Hepatitis B e Antigen-Negative Chronic Hepatitis B. Hepatology. 2001;34(4 Pt 1):617–624. doi: 10.1053/jhep.2001.27834. [DOI] [PubMed] [Google Scholar]
- 74.Funk ML, Rosenberg DM, Lok AS. World-wide epidemiology of HBeAg-negative chronic hepatitis B and associated precore and core promoter variants. J Viral Hepat. 2002;9:52–61. doi: 10.1046/j.1365-2893.2002.00304.x. [DOI] [PubMed] [Google Scholar]
- 75.Hadziyannis SJ. Milestones and perspectives in viral hepatitis B. Liver Int. 2011;31 Suppl 1:129–134. doi: 10.1111/j.1478-3231.2010.02406.x. [DOI] [PubMed] [Google Scholar]
- 76.Tai DI, Lin SM, Sheen IS, Chu CM, Lin DY, Liaw YF. Long-term outcome of hepatitis B e antigen-negative hepatitis B surface antigen carriers in relation to changes of alanine aminotransferase levels over time. Hepatology. 2009;49:1859–1867. doi: 10.1002/hep.22878. [DOI] [PubMed] [Google Scholar]
- 77.Liaw YF, Sheen IS, Chen TJ, Chu CM, Pao CC. Incidence, determinants and significance of delayed clearance of serum HBsAg in chronic hepatitis B virus infection: a prospective study. Hepatology. 1991;13:627–631. [PubMed] [Google Scholar]
- 78.Wu TT, Hsu HC, Chen DS, Sheu JC, Su IJ, Chen SL, Chuang SM. Clearance of hepatitis B surface antigen (HBsAg) after surgical resection of hepatocellular carcinoma. J Hepatol. 1987;4:45–51. doi: 10.1016/s0168-8278(87)80008-9. [DOI] [PubMed] [Google Scholar]
- 79.Yeo W, Chan TC, Leung NW, Lam WY, Mo FK, Chu MT, Chan HL, Hui EP, Lei KI, Mok TS, et al. Hepatitis B virus reactivation in lymphoma patients with prior resolved hepatitis B undergoing anticancer therapy with or without rituximab. J Clin Oncol. 2009;27:605–611. doi: 10.1200/JCO.2008.18.0182. [DOI] [PubMed] [Google Scholar]
- 80.Lubel JS, Angus PW. Hepatitis B reactivation in patients receiving cytotoxic chemotherapy: diagnosis and management. J Gastroenterol Hepatol. 2010;25:864–871. doi: 10.1111/j.1440-1746.2010.06243.x. [DOI] [PubMed] [Google Scholar]
- 81.Tassopoulos NC, Papaevangelou GJ, Sjogren MH, Roumeliotou-Karayannis A, Gerin JL, Purcell RH. Natural history of acute hepatitis B surface antigen-positive hepatitis in Greek adults. Gastroenterology. 1987;92:1844–1850. doi: 10.1016/0016-5085(87)90614-7. [DOI] [PubMed] [Google Scholar]
- 82.Yotsuyanagi H, Ito K, Yamada N, Takahashi H, Okuse C, Yasuda K, Suzuki M, Moriya K, Mizokami M, Miyakawa Y, et al. High levels of hepatitis B virus after the onset of disease lead to chronic infection in patients with acute hepatitis B. Clin Infect Dis. 2013;57:935–942. doi: 10.1093/cid/cit348. [DOI] [PubMed] [Google Scholar]
- 83.Nguyen T, Thompson AJ, Bowden S, Croagh C, Bell S, Desmond PV, Levy M, Locarnini SA. Hepatitis B surface antigen levels during the natural history of chronic hepatitis B: a perspective on Asia. J Hepatol. 2010;52:508–513. doi: 10.1016/j.jhep.2010.01.007. [DOI] [PubMed] [Google Scholar]


