Abstract
We report a rare case of pronator teres syndrome in a young female patient. She reported that her right hand grip had weakened and development of tingling sensation in the first-third fingers two months previous. Thenar muscle atrophy was prominent, and hypoesthesia was also examined on median nerve territory. The pronation test and Tinel sign on the proximal forearm were positive. Severe pinch grip power weakness and production of a weak "OK" sign were also noted. Routine electromyography and nerve conduction velocity showed incomplete median neuropathy above the elbow level with severe axonal loss. Surgical treatment was performed because spontaneous recovery was not seen one month later.
Keywords: Pronator teres syndrome, Pronation test, Thenar muscle atrophy, Tinel sign
INTRODUCTION
Pronator teres syndrome (PTS) and anterior interosseous nerve (AIN) syndrome are proximal median neuropathies of the elbow and forearm. Seyfarth first described PTS as a representative proximal forearm median neuropathy9). However, PTS is very rare and can be challenging to diagnose and treat.
Some authors have suggested that the incidence of proximal median neuropathy is 5% (61 of 1128) of all median neuropathies, however the actual incidence of PTS is very rare and limited3,4,6). In fact, our institution did not have any record of PTS operations until recent years, although approximately 80 cases of upper and lower peripheral nerve surgeries including carpal tunnel syndrome (CTS), cubital tunnel syndrome, and other procedures are performed annually. Because proximal median neuropathies have multiple anatomical compression or pathologic lesions, it can be difficult to diagnose PTS among the many median neuropathies and providing a proper treatment strategy can also be challenging. This case study reports treatment of patient with PTS accompanied by muscular branch dysfunction of the median nerve (AIN and recurrent thenar motor nerve) and good surgical result.
CASE REPORT
A 21-year-old female presented with a two-month history of sudden weakness in right hand grip strength and a tingling sensation in the thumb, index, and middle fingers (radial side). There was no neck or shoulder pain, and no precipitating traumatic event to her affected arm was identified. She was previously very healthy and did not have any specific medical history. She had an office job for approximately two years and denied any repetitive hand stress from her job or daily life.
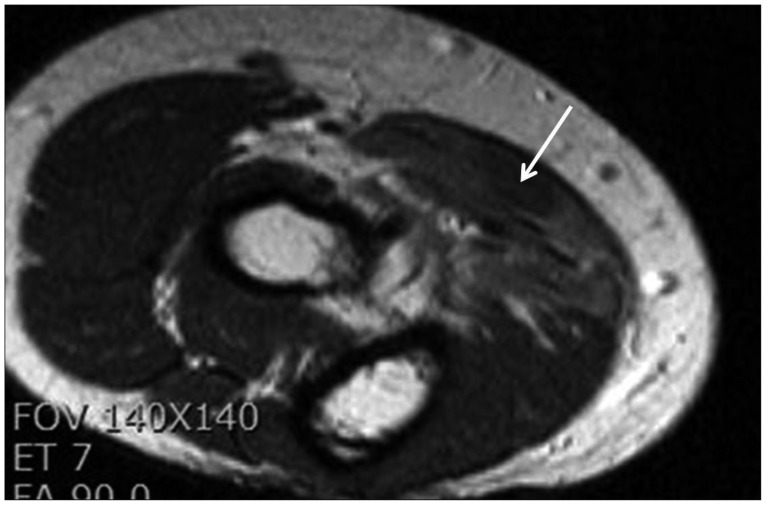
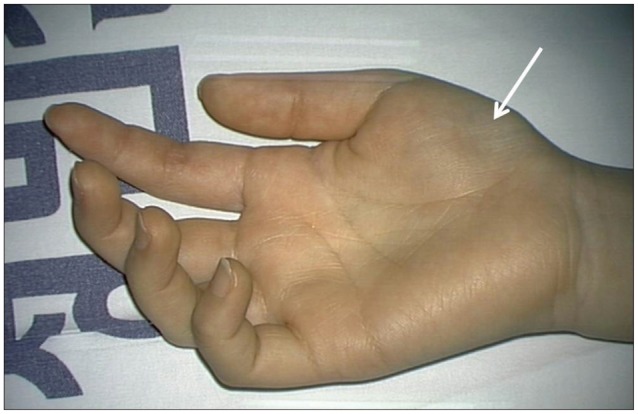
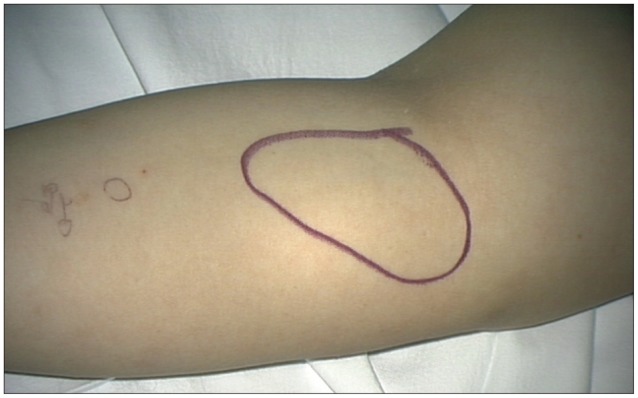
On physical examination, definite thenar muscle atrophy (right hand) was found and the index and middle finger flexion strength was 3/5 (Medical Research Council scale). Thumb abduction strength was 3/5 (Fig. 1), and ring and little finger flexion strength was 5/5. Hypoesthesia was found in the median nerve territory, and deep tendon reflexes of the bilateral upper extremities were within normal limits. At first, we thought CTS was the most likely pathology. Electrodiagnostic studies were performed seven days after the patient was first seen, and electromyographic (EMG) examination revealed abnormal spontaneous activity in the right pronator teres, flexor carpi radialis, pronator quadratus, and abductor pollicis brevis and decreased insertional activity in the right pronator teres, flexor carpi radialis, pronator quadrates, and abductor pollicis brevis muscles. We repeated the physical examination and performed an additional neurologic test for proximal median neuropathy. The patient was able to perform a weak "OK" sign, and had decreased pinch grip strength. The Tinel sign and a forearm compression test were identified only on the volar aspect of the elbow and forearm area (ulnar aspect). She had pain with pronation and discomfort in the forearm under the pronator teres, which was produced by passive supination of the wrist and active pronation from this position against resistance (Fig. 2). T2-weighted magnetic resonance imaging (MRI) of the right proximal forearm showed abnormally increased signal intensity in the pronator teres, flexor carpi radialis, the proximal portion of the flexor digitorum superficialis, and the flexor digitorum profundus innervated by the median nerve (Fig. 3).
Fig. 1.
Right thenar muscle atrophy (arrow).
Fig. 2.
A positive Tinel sign and pronation test are observed on the volar aspect of the proximal forearm.
Fig. 3.
Axial T2-weighted magnetic resonance imaging depicts increased signal intensity in the pronator teres, flexor carpi radialis, flexor digitorum superficialis, and palmaris longus (arrow).
Based on the physical examination, MRI findings, and electrodiagnostic studies, median nerve compression was suspected just distal to the elbow joint. There was no improvement in pain or muscle weakness after one month of conservative care, therefore we decided to proceed with surgery. A 10 cm classic "lazy-S"-shaped skin incision was made from 3 cm distal to the medial epicondyle over the flexor/pronator muscles (Fig. 4). After lysis of bicipital aponeuroses, the median nerve was exposed via pronator teres splitting. Diffuse fascial bands were confirmed around the median nerve and released carefully, and thickened and tight superficial fascia of the pronator teres was found to compress the median nerve. After the superficial fascia of the pronator teres was released along the distal course of the median nerve, a thin grayish discolored median nerve was noticed beneath the pronator teres fascia (Fig. 5). Resection of the tendon origin decompressed the median nerve. The wound was closed in a routine fashion, and a Penrose drain was kept in the wound for about 48 hours. There was no injury to the medial cutaneous nerve of the forearm.
Fig. 4.
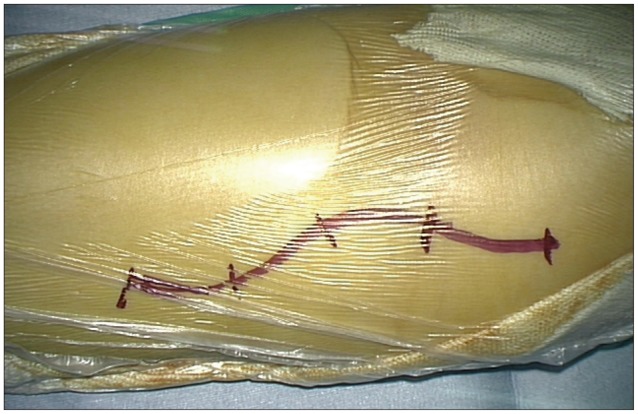
A 10-cm classical "lazy-S" shaped skin incision is made from 3 cm distal to the medial epicondyle over the flexor/pronator muscles.
Fig. 5.
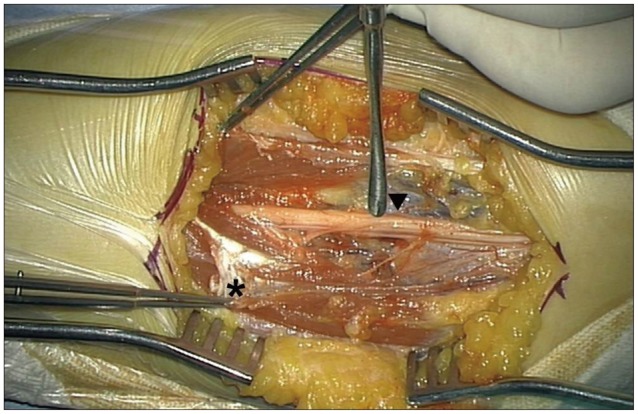
The thickened and tight superficial fascia of the pronator teres (asterisk) compresses the median nerve. After the median nerve was released, a thin, grayish, discolored median nerve (arrowhead) is observed.
One day after surgery, the tingling sensations in the first and -second fingers were much improved, but the middle finger symptoms persisted. One month later, thenar muscle atrophy had improved, the first-second finger symptoms had further improved, and the Tinel sign was negative. Motor power of the first-third fingers had improved to nearly G4-; however, she showed some difficulty in performing dexterous daily living activities. Three months later, motor power of the first-third fingers had improved to nearly G4+, and she showed no difficulty in dexterous activities. Follow-up EMG examination was not performed.
DISCUSSION
Although median neuropathy symptoms can vary substantially according to the site of entrapment, the symptoms can also be very similar and ambiguous. Interestingly, many previous reports showed that multiple cases of PTS were misdiagnosed as CTS or other pathology (13-50%)1,5,7). Moreover, specific neurological testing is not always reliable to distinguish entrapment lesions or identify the specific type of median neuropathy. For example, the pronator compression test and Phalen test can be positive in both CTS and PTS2). PTS can present with pain and numbness in the volar aspect of the elbow and forearm as well as in the hand, and hand grip weakness may be present in CTS and PTS1,7). Bridgeman et al.1) showed that the clinical symptoms of PTS were numbness (58%), weakness (49%), forearm pain (39%), paresthesia (25%), nocturnal paresthesia (2%), a positive Tinel sign over the pronator teres (7%), and tenderness over the pronator teres lesion (12%) in 83 cases of PTS. In addition, although most patients with PTS range between 30-60 years of age, our patient was relatively young (21 years of age). Entrapment of the AIN gives rise to pure motor weakness in the flexor pollicis longus and the radial half of the flexor digitorum profundus, which can cause difficulty in formation of the "OK" sign. Our patient showed symptoms typical of PTS in addition to a partial AIN-syndrome. The etiology of PTS remains unclear, although some authors have reported an immune related or viral-mediated origin10,11).
EMG and nerve conduction velocity (NCV) may be helpful for evaluating proximal median nerve neuropathy patients. Our patient showed a decreased motor conduction velocity of 43.8 m/s, spontaneous muscular fibrillation, and decreased maximal volitional activity on the muscles innervated by the proximal median nerve and the AIN. The measurement level was compatible for confirming PTS.
A typical pattern of muscle denervation is a key for the diagnosis of PTS. Additionally, on MR imaging, patient lesions show abnormally high signal intensity on T2-weighed fat-suppressed images. Decision and timing of surgery and the effectiveness of the surgical approach with PTS treatment can be difficult for the operating surgeon, because of the lack of established objective criteria; there are few treatment strategies in the literature. We opted for early surgical exploration in our patient for several reasons. First, some authors recommend surgical exploration when active denervation of the median nerve is confirmed by electrodiagnostic tests1). The trend toward poorer results in the presence of an abnormal NCV suggests that there may be more extensive involvement and more severe compression in these patients7). Clinically, our patient showed severe thenar muscle atrophy within a relatively short time period (about two-months), which could indicate the progression of axonal loss in the median nerve. Finally, conservative medical treatment did not result in any improvement. Rather her symptoms were slightly aggravated during the one-month follow-up period.
Proximal forearm surgical outcomes have not been usually not as good as those for CTS release4,7). Although the exact reasons for this are unclear, re-adhesion of the median nerve in the surgical field and increased lesions are thought to be the main causes. Second, surgeons have limited surgical experience in proximal median pathology. Third, the proximal median nerve trunk has more individual branches and bundles than the distal median nerve trunk when considering the 'intraneural topographic' aspect. Jabaley et al.5) suggested the 'intraneural topography concept', which explains that individual motor or sensory fascicle compartments can be divided and traced within the main median nerve trunk. Therefore, the proximal median nerve trunk has more complex motor and sensory bundles than the distal trunk. Intraneural topography of the median nerve may provide reasons for the variable symptoms and signs of median neuropathy. Fourth, PTS can arise without prominent compression lesions around the median nerve such as with the spontaneous type or neuritis origin PTS, which can not be resolved with surgery. Some authors have reported that there were no compression origins with proximal median neuropathic patients during operation4,8).
In this case, the surgery outcome was favorable because we identified a prominent tension band or compression lesion around the median nerve which fully decompressed during operation. We propose parameters for tension band or compression lesions around the median nerve based on this case. In our study, the pronator teres (PT) test was positive. The pronator teres test dose not directly stimulate the median nerve, rather the test indirectly stimulates the median nerve by dynamic normal muscle or ligament movement. However, PTS with neuritis may not have a positive, prominent positive PT test.
Thenar muscle atrophy and pseudo-AIN syndrome can also be related to the intraneural topograhy of the median nerve. Although, thenar muscle atrophy is very rare, thenar muscle weakness may be induced by pseudo-AIN syndrome. The recurrent branch of the median nerve to the thenar muscles (opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis) is located near the carpal tunnel ligament; however, our patient had improved thenar muscle atrophy after proximal median nerve release, not carpal tunnel release. Pseudo-AIN syndrome leads to paralysis of the muscles supplied not only by the AIN but also by the other median branch, because the actual site of compression is located more proximal to the origin of the AIN12).
CONCLUSION
This case showed somewhat atypical PTS symptoms patterns including a very young patient and combined thenar muscle atrophy. In similar cases, early surgical exploration can be considered if there is convincing evidence of compression lesions around the median nerve and progressive axonal loss.
References
- 1.Bridgeman C, Naidu S, Kothari MJ. Clinical and electrophysiological presentation of pronator syndrome. Electromyogr Clin Neurophysiol. 2007;47:89–92. [PubMed] [Google Scholar]
- 2.Buchthal F, Rosenfalck A, Trojaborg W. Electrophysiological findings in entrapment of the median nerve at wrist and elbow. J Neurol Neurosurg Psychiatry. 1974;37:340–360. doi: 10.1136/jnnp.37.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gessini L, Jandolo B, Pietrangeli A. Entrapment neuropathies of the median nerve at and above the elbow. Surg Neurol. 1983;19:112–116. doi: 10.1016/0090-3019(83)90405-6. [DOI] [PubMed] [Google Scholar]
- 4.Hartz CR, Linscheid RL, Gramse RR, Daube JR. The pronator teres syndrome : compressive neuropathy of the median nerve. J Bone Joint Surg Am. 1981;63:885–890. [PubMed] [Google Scholar]
- 5.Jabaley ME, Wallace WH, Heckler FR. Internal topography of major nerves of the forearm and hand : a current view. J Hand Surg Am. 1980;5:1–18. doi: 10.1016/s0363-5023(80)80035-9. [DOI] [PubMed] [Google Scholar]
- 6.Nigst H, Dick W. Syndromes of compression of the median nerve in the proximal forearm (pronator teres syndrome; anterior interosseous nerve syndrome) Arch Orthop Trauma Surg. 1979;93:307–312. doi: 10.1007/BF00450231. [DOI] [PubMed] [Google Scholar]
- 7.Olehnik WK, Manske PR, Szerzinski J. Median nerve compression in the proximal forearm. J Hand Surg Am. 1994;19:121–126. doi: 10.1016/0363-5023(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 8.Park IJ, Roh YT, Jeong C, Kim HM. Spontaneous anterior interosseous nerve syndrome : clinical analysis of eleven surgical cases. J Plast Surg Hand Surg. 2013;47:519–523. doi: 10.3109/2000656X.2013.791624. [DOI] [PubMed] [Google Scholar]
- 9.Seyffarth H. pronator teres as cause of lesion of the N. medianus (the pronator syndrome) Acta Psychiatr Neurol Scand Suppl. 1951;74:251–254. [PubMed] [Google Scholar]
- 10.Stutz CM. Neuralgic amyotrophy : Parsonage-Turner Syndrome. J Hand Surg Am. 2010;35:2104–2106. doi: 10.1016/j.jhsa.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 11.van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129(Pt 2):438–450. doi: 10.1093/brain/awh722. [DOI] [PubMed] [Google Scholar]
- 12.Wertsch JJ, Sanger JR, Matloub HS. Pseudo-anterior interosseous nerve syndrome. Muscle Nerve. 1985;8:68–70. doi: 10.1002/mus.880080112. [DOI] [PubMed] [Google Scholar]