Abstract
The aetiology of dyspepsia is unknown in the majority of patients. Helicobacter pylori (H pylori) is the cause in a subset of patients. A non invasive test to assess the presence of H pylori is recommended in the management of patients under the age of 50 presenting to a family practitioner with dyspepsia. A urea breath test or a stool antigen test are the most reliable non invasive tests. Eradication of H pylori will reduce the risk to the patient with dyspepsia of developing a peptic ulcer, reduce the complication rate if prescribed non-steroid anti-inflammatory drugs and later reduce the risk of gastric cancer. The recommended treatment for non ulcer dyspepsia associated with a H pylori infection should be a 10-d course of treatment with a PPI and two antibiotics. Treatment efficacy should be assessed four weeks after completing treatment with a urea breath test or a stool antigen test.
Keywords: Functional dyspepsia, Helicobacter pylori, Triple therapy, Urea breath test
INTRODUCTION
Dyspepsia or indigestion is an unsatisfactory term as it describes a spectrum of conditions. It has other limitations as there is no similar word in all languages. The patient does not volunteer symptoms and the diagnosis depends on a doctor’s interpretation of the patient’s complaint. Symptoms are vague and varied but for research and clinical purposes are grouped as reflux, ulcer like, motility or non specific[1].
Since the aetiology of dyspepsia is uncertain, it is not surprising that (Helicobacter pylori) H pylori has been implicated in dyspepsia. Large population studies have shown that the bacteria is found more frequently in dyspeptic patients compared to controls. Peptic ulcer relapse and remit and it is possible that at the time of endoscopy an ulcer is not present and then the patient is diagnosed with non ulcer dyspepsia as the bacteria will be present[2]. There is unequivocal evidence that infection with H pylori is the principal cause of peptic ulcer disease. The organism is present in 85%-95% of patients with peptic ulcer disease, and treating the infection is effective in healing these ulcers. Treatment to eradicate H pylori results in permanent cure of peptic ulcer disease, whereas 60%-80% of such patients relapse within a year if treated with anti-secretory drugs alone[3].
The evidence for an association between H pylori and non-ulcer dyspepsia is more uncertain. Many trials evaluating the efficacy of H pylori eradication treatment for non-ulcer dyspepsia have been poorly designed and have given conflicting results but there is a clear indication that H pylori eradication treatment is effective in at least a subset of patients with non-ulcer dyspepsia.
INVESTIGATING DYSPEPSIA
Patients presenting to a primary care physician with symptoms referable to the upper gastrointestinal tract are usually treated empirically with a proton pump inhibitor (PPI) or are assessed for the presence of H pylori by a non-invasive test. The recommended non invasive tests are a urea breath test or a stool antigen test. A serology test is considered less reliable and is not recommended. Consensus guidelines have recommended a test and treat approach to patients with H pylori[4,5]. This has been controversial as the response to treatment has been equivocal. In a double blind study the test and treat approach has been vindicated in non investigated dyspepsia in patients presenting to a family practitioner. In a study of 294 patients who were randomised to triple therapy of a PPI and two antibiotics, clarithromycin and metronidazole for one week or a PPI and placebo antibiotic the patients were evaluated monthly for one year[6]. The results of this randomised control led study demonstrate a significant benefit of a H pylori “test and treat” strategy at primary care level (Figure 1).
Figure 1.
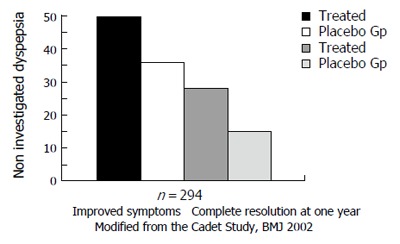
Significant improvements in complete resolution of symptoms in patients successfully treated of H pylori infection.
Endoscopy
Investigated dyspepsia describes patients who had an endoscopy and in whom no mucosal lesions are found, but are found to have an H pylori infection on biopsy. Systematic review of randomised controlled trials comparing H pylori eradication with placebo or another drug treatment has been published[7]. In this analysis the trial reports were reviewed according to predefined eligibility and quality criteria. Twelve trials were included in the systematic review, nine of which evaluated dyspepsia at 3-12 mo in 2541 patients. H pylori eradication treatment was significantly superior to placebo in treating non-ulcer dyspepsia (relative risk reduction 9% (95% confidence interval 4% to 14%)). One case of dyspepsia being cured for every 15 people treated. H pylori eradication cost £56 per dyspepsia-free month during first year after treatment. The conclusion of this comprehensive data review is that H pylori eradication is cost effective treatment for non-ulcer dyspepsia in infected patients.
Test and treat vs endoscopy
A number of economic models were developed suggesting that eradication models were developed suggesting that eradication of H pylori might be cost saving in dyspepsia. Silverstein et al reported that the 1 year medical charges for the initial management of an incident episode of dyspepsia were $2163 for prompt upper endoscopy versus $2123 for empirical therapy, a difference of only 2%; the decision was a toss-up across all age groups and clinical strata applying medical charges[8]. Other models support empirical H pylori therapy as being less costly. Fendrick et al[9] in a model restricted to persons with symptoms suggesting peptic ulcer disease, reported that the most expensive strategy was endoscopy and biopsy for H pylori at $1584, while the costs per patient treated were lowest for serologic testing for H pylori (and treating seropositive cases) at $894 and empirical anti-secretory therapy combined with antibiotics (for all cases) at $818. Only if an upper endoscopy cost $500 or less was an endoscopy strategy superior.
Ofman et al[10] in a model of H pylori-positive patients with dyspepsia, found that empirical treatment was less expensive ($820 vs $1276), largely due to less upper endoscopy (52%). They calculated that endoscopy related costs had to be reduced by 96% before initial endoscopy and H pylori treatment were similarly cost-effective. Other models have suggested benefits may be marginal[11] or will take at least 5 years to accrue[12]. Upper gastrointestinal radiology is still practiced in some primary care settings but was not a cost-effective alternative to a H pylori test and treat strategy. In another US model[13], the test and treat approach is cost effective compared to prompt endoscopy. The benefit is more apparent if there is a high prevalence of peptic ulcer and of H pylori infection in the population. The value of this approach decreases when the prevalence rate of the infection falls. The critical prevalence below which the test and treat is less effective although still an option is 15%[14].
The yield from endoscopy in patients being in-vestigated for dyspepsia increases with advancing age but is low[15]. Missing early (and hence curable) gastric cancer is often of greatest concern to the clinician con-templating empirical therapy, especially in an older patient[16,17]. Fear of gastric cancer has to be taken into account when planning the management of dyspepsia. A practical approach to investigate patients with endoscopy presenting with dyspepsia should be made for alarm signs and not on the basis of age alone, reflecting the balance of benefit and harm from endoscopy. Empirical management without formal diagnosis is appropriate for most patients: reviewing the patient history, lifestyle, over-the-counter medicines, and providing a course of proton-pump inhibitors and/or H pylori test and treatment. Patients with ongoing symptoms require at least annual review to discuss symptoms and lifestyle, and as appropriate, encourage stepping down prescribed medication and returning to self-care. A new strategy included in the step down process is the use of therapies ‘on-demand’.
However, there is inconclusive evidence that patients without alarm signs will benefit subsequently from endosocpy, while investigation involves a small but real risk of harm[18].
Long term studies
The effectiveness of a test and treat strategy, is confirmed in long term studies. In two long term follow up studies of almost 7 years the benefits of eradication were still apparent[19,20]. In a short term prospective study from my unit of 90 patients with non ulcer dyspepsia, no clinical or endoscopic evidence of other peptic biliary, pancreatic or malignant disease; all had evidence of H pylori infection were randomised to bismuth alone, antibiotics alone or a combination of bismuth and antibiotics. Overall H pylori eradication was achieved in 49% of patients, although gastritis improved in those in whom the bacteria was eliminated whereas symptoms score were similar in patients where the infection persisted or was eradicated[21] when assessed at four weeks. However, a follow-up study at one year of these patients showed the patients in whom the bacteria persisted required additional treatment and in were more symptomatic compared to those who were eradicated of the bacteria.
The same patients when reviewed at a 5-yr follow up showed that patients who were successfully treated were more likely to be asymptomatic and none developed a duodenal ulcer. Where as up to 20% developed an ulcer when the bacteria was still present (Figure 2)[22].
Figure 2.
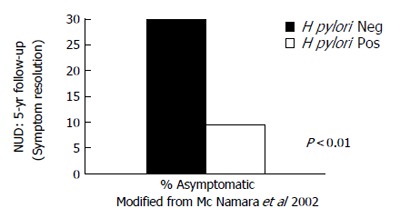
Patients who had H pylori eradicated were less symptomatic at 5 years compared to patients who had persistent H pylori infection.
PATHOGENESIS
There is some evidence that H pylori-associated dyspepsia is caused by the effect of the bacterium on acid secretion[23]. H pylori infection causes increased fasting and post-prandial serum gastrin levels and decreased gastric mucosal concentrations of stomatostatin abnormalities which are corrected following eradication[24-27].
Gastrin-releasing peptide is a neuro-peptide that mimics the physiological responses of the stomach to a meal. After intravenous infusion of gastrin-releasing peptide, patients with peptic ulcers and H pylori infection have a six-fold increase in acid secretion and patients with non-ulcer dyspepsia and H pylori have a four-fold increase, whereas asymptomatic H pylori positive individuals have a two-and-a-half-fold increase in stimulated acid secretion, when compared to asymptomatic controls who do not have H pylori infection[28]. This would suggest that non-ulcer dyspepsia may represent part of a spectrum of H pylori-induced disease. The spectrum ranges from an asymptomatic carrier state, through an ulcer-free dyspeptic period to finally developing a peptic ulcer.
Further work from my unit suggest that mast cells are found in H pylori negative dyspeptic patients, compared to H pylori positive patients suggesting a different mechanism of symptoms in H pylori negative dyspepsia[29].
TREATMENT
It has been suggested that the eradication rates in patients with non ulcer dyspepsia is not as successful in patients with duodenal ulcer[30]. The possible explanation is that the bacteria colonisation is not as dense and that the gastritis is not as severe allowing poorer penetration of antibiotics. It emphasis the need for compliance. Smoking is associated with a lower success in treatment and may serve as surrogate marker for compliance. The treatment is complex and it is know that individuals who have received third level education achieve only 50% compliance to a five day course of antibiotics. Patient education is vital for successful treatment. They should be warned of possible side effects such as diarrhoea and antibiotic sensitivity. Diarrhoea is usually transient and self limiting and occasionally cases of clostridium difficile have been reported.
New options in the treatment armamentarium against H pylori provide hope of higher eradication rates. The use of a more prolonged 10-d course of therapy rather then the traditional 7-d course, and quadruple rather than triple therapy may lead to higher eradication rates. In a French study of 2571 patients, the use of 10-d therapy as opposed to 7-d therapy was associated with higher eradication rates- 83.9% compared with 70.6%[30]. A meta-analysis of 13 studies evaluated lengthening triple therapy beyond 7 d. Only randomised trails comparing 7-d triple therapy with either 10 or 14 d triple therapy were included. In the intention to treat analysis, pooled 10 and 14 d therapies lead to better results than 7 d schedules. However, in head-to-head comparisons, although a trend for higher cure rates was found with longer therapy, only 14-d therapies were found to be significantly better than 7-d therapy. Looking at intention-to-treat analysis, 10 d therapy compared with 7-d therapy lead to a 3% increased eradication rate-from 80 to 83% - whereas, 14-d therapy compared with 7-d therapy led to a 9% increased eradication rate from 72 to 81%[31].
CONCLUSION
A test and treat strategy is the preferred option for patients with dyspepsia presenting to primary carer physicians. The benefit of this are apparent in long term studies. The additional benefit of eradication of the bacteria will prevent subsequent development of an ulcer and the complication that might ensue if prescribed NSAIDs later and reduce the risk of gastric cancer. Treatment compliance is essential. The preferred treatment is a PPI based triple therapy, which should be given for a period of at least 10 d.
Footnotes
S- Editor Pan BR E- Editor Liu WF
References
- 1.O'Morain C, Gilvarry J. Eradication of Helicobacter pylori in patients with non-ulcer dyspepsia. Scand J Gastroenterol. 1993;196 Suppl:30–33. doi: 10.3109/00365529309098340. [DOI] [PubMed] [Google Scholar]
- 2.Mc Namara DA, Buckley M, O’Morain CA. Nonulcer dyspepsia. Current concepts and management. Gastroenterol Clin North Am. 2000;29:807–818. doi: 10.1016/s0889-8553(05)70148-5. [DOI] [PubMed] [Google Scholar]
- 3.Lee JM, Deasy E, O’Morain CA. Helicobacter pylori eradication therapy: a discrepancy between current guidelines and clinical practice. Eur J Gastroenterol Hepatol. 2000;12:433–437. [PubMed] [Google Scholar]
- 4.Malfertheiner P, Megraud F, O’Morain C, Hungin AP, Jones R, Axon A, Graham DY, Tytgat G. Current concepts in the management of Helicobacter pylori infection--the Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther. 2002;16:167–180. doi: 10.1046/j.1365-2036.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 5.Talley NJ. American Gastroenterological Association medical position statement: evaluation of dyspepsia. Gastroenterology. 2005;129:1753–1755. doi: 10.1053/j.gastro.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Chiba N, Veldhuyzen Van Zanten SJ, Escobedo S, Grace E, Lee J, Sinclair P, Barkun A, Armstrong D, Thomson AB. Economic evaluation of Helicobacter pylori eradication in the CADET-Hp randomized controlled trial of H. pylori-positive primary care patients with uninvestigated dyspepsia. Aliment Pharmacol Ther. 2004;19:349–358. doi: 10.1111/j.1365-2036.2004.01865.x. [DOI] [PubMed] [Google Scholar]
- 7.Moayyedi P, Soo S, Deeks J, Forman D, Mason J, Innes M, Delaney B. Systematic review and economic evaluation of Helicobacter pylori eradication treatment for non-ulcer dyspepsia. Dyspepsia Review Group. BMJ. 2000;321:659–664. doi: 10.1136/bmj.321.7262.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverstein MD, Petterson T, Talley NJ. Initial endoscopy or empirical therapy with or without testing for Helicobacter pylori for dyspepsia: a decision analysis. Gastroenterology. 1996;110:72–83. doi: 10.1053/gast.1996.v110.pm8536890. [DOI] [PubMed] [Google Scholar]
- 9.Fendrick AM, Chernew ME, Hirth RA, Bloom BS. Alternative management strategies for patients with suspected peptic ulcer disease. Ann Intern Med. 1995;123:260–268. doi: 10.7326/0003-4819-123-4-199508150-00003. [DOI] [PubMed] [Google Scholar]
- 10.Ofman JJ, Etchason J, Fullerton S, Kahn KL, Soll AH. Management strategies for Helicobacter pylori-seropositive patients with dyspepsia: clinical and economic consequences. Ann Intern Med. 1997;126:280–291. doi: 10.7326/0003-4819-126-4-199702150-00004. [DOI] [PubMed] [Google Scholar]
- 11.Sonnenberg A, Townsend WF, Müller AD. Evaluation of dyspepsia and functional gastrointestinal disorders: a cost-benefit analysis of different approaches. Eur J Gastroenterol Hepatol. 1995;7:655–659. [PubMed] [Google Scholar]
- 12.Briggs AH, Sculpher MJ, Logan RP, Aldous J, Ramsay ME, Baron JH. Cost effectiveness of screening for and eradication of Helicobacter pylori in management of dyspeptic patients under 45 years of age. BMJ. 1996;312:1321–1325. doi: 10.1136/bmj.312.7042.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rich M, Scheiman JM, Tierney W, Fendrick AM. Is upper gastrointestinal radiography a cost-effective alternative to a Helicobacter pylori "test and treat" strategy for patients with suspected peptic ulcer disease. Am J Gastroenterol. 2000;95:651–658. doi: 10.1111/j.1572-0241.2000.01837.x. [DOI] [PubMed] [Google Scholar]
- 14.Ladabaum U, Chey WD, Scheiman JM, Fendrick AM. Re-appraisal of non-invasive management strategies for uninvestigated dyspepsia: a cost-minimization analysis. Aliment Pharmacol Ther. 2002;16:1491–1501. doi: 10.1046/j.1365-2036.2002.01306.x. [DOI] [PubMed] [Google Scholar]
- 15.Talley NJ, Silverstein MD, Agreus L, Nyren O, Sonnenberg A, Holtmann G. AGA technical review: evaluation of dyspepsia. American Gastroenterological Association. Gastroenterology. 1998;114:582–595. doi: 10.1016/s0016-5085(98)70542-6. [DOI] [PubMed] [Google Scholar]
- 16.Hallissey MT, Allum WH, Jewkes AJ, Ellis DJ, Fielding JW. Early detection of gastric cancer. BMJ. 1990;301:513–515. doi: 10.1136/bmj.301.6751.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mason JM, Delaney B, Moayyedi P, Thomas M, Walt R. Managing dyspepsia without alarm signs in primary care: new national guidance for England and Wales. Aliment Pharmacol Ther. 2005;21:1135–1143. doi: 10.1111/j.1365-2036.2005.02445.x. [DOI] [PubMed] [Google Scholar]
- 18.Lassen AT, Hallas J, Schaffalitzky de Muckadell OB. Helicobacter pylori test and eradicate versus prompt endoscopy for management of dyspeptic patients: 6.7 year follow up of a randomised trial. Gut. 2004;53:1758–1763. doi: 10.1136/gut.2004.043570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laheij RJ, van Rossum LG, Heinen N, Jansen JB. Long-term follow-up of empirical treatment or prompt endoscopy for patients with persistent dyspeptic symptoms. Eur J Gastroenterol Hepatol. 2004;16:785–789. doi: 10.1097/01.meg.0000108366.19243.3a. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy C, Patchett S, Collins RM, Beattie S, Keane C, O’Morain C. Long-term prospective study of Helicobacter pylori in nonulcer dyspepsia. Dig Dis Sci. 1995;40:114–119. doi: 10.1007/BF02063953. [DOI] [PubMed] [Google Scholar]
- 21.Patchett S, Beattie S, Leen E, Keane C, O’Morain C. Eradicating Helicobacter pylori and symptoms of non-ulcer dyspepsia. BMJ. 1991;303:1238–1240. doi: 10.1136/bmj.303.6812.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNamara D, Buckley M, Gilvarry J, O’Morain C. Does Helicobacter pylori eradication affect symptoms in nonulcer dyspepsia: a 5-year follow-up study. Helicobacter. 2002;7:317–321. doi: 10.1046/j.1523-5378.2002.00104.x. [DOI] [PubMed] [Google Scholar]
- 23.El-Omar E, Penman I, McColl K E L. A substantial proportion of H pylori positive NUD patietns have the same disturbance of acid secretion as DU patients. Gut. 1993;4:S49. doi: 10.1136/gut.36.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McColl KE, Fullarton GM, Chittajalu R, el Nujumi AM, MacDonald AM, Dahill SW, Hilditch TE. Plasma gastrin, daytime intragastric pH, and nocturnal acid output before and at 1 and 7 months after eradication of Helicobacter pylori in duodenal ulcer subjects. Scand J Gastroenterol. 1991;26:339–346. doi: 10.3109/00365529109025052. [DOI] [PubMed] [Google Scholar]
- 25.Levi S, Beardshall K, Swift I, Foulkes W, Playford R, Ghosh P, Calam J. Antral Helicobacter pylori, hypergastrinaemia, and duodenal ulcers: effect of eradicating the organism. BMJ. 1989;299:1504–1505. doi: 10.1136/bmj.299.6714.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prewett EJ, Smith JT, Nwokolo CU, Hudson M, Sawyerr AM, Pounder RE. Eradication of Helicobacter pylori abolishes 24-hour hypergastrinaemia: a prospective study in healthy subjects. Aliment Pharmacol Ther. 1991;5:283–290. doi: 10.1111/j.1365-2036.1991.tb00029.x. [DOI] [PubMed] [Google Scholar]
- 27.Moss SF, Legon S, Bishop AE, Polak JM, Calam J. Effect of Helicobacter pylori on gastric somatostatin in duodenal ulcer disease. Lancet. 1992;340:930–932. doi: 10.1016/0140-6736(92)92816-x. [DOI] [PubMed] [Google Scholar]
- 28.el-Omar E, Penman I, Dorrian CA, Ardill JE, McColl KE. Eradicating Helicobacter pylori infection lowers gastrin mediated acid secretion by two thirds in patients with duodenal ulcer. Gut. 1993;34:1060–1065. doi: 10.1136/gut.34.8.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall W, Buckley M, Crotty P, O’Morain CA. Gastric mucosal mast cells are increased in Helicobacter pylori-negative functional dyspepsia. Clin Gastroenterol Hepatol. 2003;1:363–369. doi: 10.1053/s1542-3565(03)00184-8. [DOI] [PubMed] [Google Scholar]
- 30.Broutet N, Tchamgoue S, Pereira E, Lamouliatte H, Salamon R, Megraud F. Risk factors for failure of Helicobacter pylori therapy--results of an individual data analysis of 2751 patients. Aliment Pharmacol Ther. 2003;17:99–109. doi: 10.1046/j.1365-2036.2003.01396.x. [DOI] [PubMed] [Google Scholar]
- 31.McLoughlin R, Racz I, Buckley M, O'Connor HJ, O'Morain C. Therapy of Helicobacter pylori. Helicobacter. 2004;9 Suppl 1:42–48. doi: 10.1111/j.1083-4389.2004.00251.x. [DOI] [PubMed] [Google Scholar]


