Abstract
Objective
Sinus surgery is one of the most frequently performed surgical operations. The objective was to determine if rates of surgery have changed over the last 10 years.
Study Design
Secondary data analysis of the State Ambulatory Surgery Database of Florida.
Methods
We calculated population adjusted rates of ambulatory sinus surgery for all adults, 2000–2009.
Result
There was a substantial decrease in the proportion of patients who had surgery in a hospital setting and a substantial increase in patients who had surgery with image guidance. Population-adjusted rates of sinus surgery increased over the study period, from a mean of 104 cases per 100,000 population in 2000 to 129 per 100,000 in 2009 (p<0.001). Procedure rates also increased, from a mean of 226 per 100,000 in 2000 to 316 per 100,000 in 2009 (p<0.001). Rates of frontal sinus procedures more than doubled, and rates of cases in which all 4 sinuses were treated tripled during the same time period. A greater number of sinus procedures was associated with use of image guidance, and high annual surgical case volume. The strongest predictor was the individual surgeon.
Conclusion
Rates of sinus surgery increased over the study period, with more patients undergoing surgery and more procedures per surgical case. The strong association of procedural patterns with specific surgeons in sinusitis care highlights the importance of future investigations to examine training, technological, and reimbursement factors that may influence surgeons’ clinical decision-making for this common condition.
Keywords: Adult rhinology, outcomes research, statistics
Introduction
Sinusitis is one of the most prevalent chronic illnesses in the United States, consistently reported by 13%–14% of adults annually for the last 20 years.1,2 Most sinusitis care is provided by primary care physicians, with 17 million ambulatory care visits each year.3 Patients who fail to improve with medical therapy may undergo sinus surgery.
More than 250,000 sinus operations are performed annually4—one of the most frequent surgical procedures after septoplasty (260,000).4,5 Absolute indications for sinus surgery include orbital or intracranial infection, invasive fungal infection, neoplasm, or spinal fluid leak, but these indications are present in a minority of patients with sinusitis.6 Most patients have relative indications for surgery—principally sinus disease that is persistent and symptomatic despite medical therapy.
For the typical patient with sinusitis, the clinical question is whether surgery would provide additional benefit over medical treatment. Clinical evidence to inform this decision is based on observational studies in tertiary care practices. These studies are subject to selection bias and we do not know how much we can apply the findings of these studies to less highly selected patient populations. In the absence of robust clinical evidence, non-evidence based factors may influence sinusitis treatment decisions. In other aspects of medical care with large knowledge deficits, medical treatment may be influenced by factors that otherwise would not influence treatment—e.g., patients’ preferences, physicians’ experience and training, anecdotal evidence, and medicolegal factors.7–11
In the case of sinusitis, the end result of these influential factors may be that surgeons vary widely in the threshold to operate. In this study, we sought to describe the current practice of endoscopic sinus surgery and to identify aspects of surgery with the most variation as a possible indication of clinical uncertainty. We hypothesized non-clinical factors, other than patient demographics, contribute to variation in sinus surgery. If true, it may be possible to improve the quality of sinusitis care by identifying non-clinical influential factors and their relative influence in clinical decision-making.
Methods
Data Source and Subjects
We used the State Ambulatory Surgery Database (SASD) of Florida. SASD is a product of the Healthcare Cost and Utilization Project, conducted by the federal Agency for Healthcare Research and Quality.12 The Florida SASD is one of the largest and most ethnically diverse SASD datasets and, unlike many other states, includes records from hospital-affiliated and freestanding surgery centers and thus contains a 100% sample of ambulatory surgeries each year.
Compilation of the Analytic Dataset
We defined the study cohort from Florida SASD files using Current Procedural and Terminology (CPT) codes for years 2000–2009. Endoscopic sinus procedures have supplanted traditional sinus surgery procedures over the last 15–20 years13 and therefore we limited our analysis to CPT codes for endoscopic sinus surgery (CPT 31256, 31267, 31254, 31255, 31276, 31287, 31288).
We excluded patients <18 years of age because they are not representative of the majority of patients who undergo sinus surgery. We also excluded 2026 patients with missing data for gender, age, zip code, surgeon identifier, race, primary payer, or hospital ambulatory surgery center type as well as non-Florida residents, leaving 94,152 observations for analysis.
Candidate Covariate Factors
We obtained patient demographic information including age, gender, race, primary expected payer, and location of surgery at either a hospital or an ambulatory surgery facility. In addition, we created a covariate, “nasal surgery” to describe whether or not septum or inferior turbinate operations were performed (CPT 30520, 30130, 30140, 30200, 30210, 30801, 30802, 30930), and a covariate, “image guidance” to describe whether image guidance technology (navigational assistance for surgical dissection) was used (CPT 61795).
We used hospital service areas to perform population analyses. Each hospital service area is geographically defined by the residents located near the hospital who receive a high percentage of care at the local facility.14 Residents in a community with only one hospital tend to be uniform in that most patients seek care at the local facility. Residents in a community located between two hospital facilities may be divided in their hospital use and this would be reflected by two different hospital service areas. In contrast, hospital referral regions are defined by the presence of cardiovascular surgery and neurosurgery and are tertiary care facilities.7 Endoscopic sinus surgery is largely performed in community hospitals, not tertiary care facilities, notwithstanding the fact that some patients are referred to specialists. For this reason, we felt hospital service area was the appropriate level of analysis. We assigned each patient to the respective hospital service area by using the zip code variable from the SASD file and the crosswalk file from the Dartmouth Atlas project (2006).15 The crosswalk file is a spreadsheet that assigns each ZIP code to a hospital service area according to where a plurality of patients residing in that ZIP code receive their medical care. This enabled subsequent calculation of rates of surgery standardized to local population sizes. In addition, we obtained unique surgeon identifiers from the SASD file and created a continuous variable to describe each surgeon’s annual sinus surgery case volume by summing the total number of discharges for endoscopic sinus surgery.
Statistical Analyses
To describe use of sinus surgery over time, we described population-adjusted rates for each procedure (e.g. maxillary, ethmoid, frontal, and sphenoid procedures) of interest by year. For these rates the numerator was the number of specific operations each year and the denominator was the number of patients residing in each hospital service area by age and gender, using United States population data for the state of Florida.16
In order to further explore changes in population-adjusted rates of surgery over time, we defined the primary outcome for each patient discharge (“cases”) as the count of sinus procedures performed (“procedures”). Sinus surgery entails a surgical procedure to enlarge the natural opening of 1 or more of the 4 pairs of sinuses. Each sinus procedure is coded individually: maxillary (31256 or 31267), ethmoid (31254 or 31255), frontal (31276) and sphenoid (31287 or 31288). We defined the outcome (# sinus procedures/case) as the count of sinuses operated upon (range 1–4). This dataset do not distinguish between unilateral versus bilateral sinus procedures. For this reason, paired procedures, e.g. bilateral maxillary procedures, were only counted as a single procedure, “maxillary.” Likewise, an anterior ethmoidectomy on one side, and a complete ethmoidectomy on the contralateral side, was counted as a single procedure, “ethmoid.” A case with both maxillary and ethmoid procedures was counted as two sinus procedures. We used the χ2 test to compare patient factors and surgeon case volume across patients undergoing sinus surgery.
We used a multilevel Poisson model for the primary outcome—extent of sinus surgery, expressed as a count of the number of sinus procedures per case.17,18 We first fit an empty model with no explanatory variables, and 3 nested levels: patient as level 1, surgeon as level 2, and hospital service area as level 3 (Stata command xtmepoisson). For level 1 models, we included patient demographic, nasal surgery and image guidance variables as predictors of sinus surgery extent. For level 2 models accounting for clustering of variance at the level of individual surgeons, we specified the model with random effects to account for variable effects of unobserved surgeon-level factors. Of note, level 3 models did not explain additional variance in the outcome beyond levels 1 and 2; therefore, only findings from level 1 and level 2 models are presented below.
We performed all analyses with Stata (version 12.0, Stata Corp, College Station, TX). We used two-tailed tests with p<0.05 as the level of statistical significance. The University of Michigan Institutional Review Board deemed this study of publicly available de-identified information exempt from human subjects review.
Results
Characteristics of the patients at the beginning versus at end of this 10-year period (Table 1) differed significantly in many respects. Between 2000 and 2009 there was a substantial decrease in the unadjusted proportion of patients who had surgery in a hospital setting versus a free-standing ambulatory surgery facility, and a substantial increase in the proportion of patients who had surgery with image guidance. Time trends in age, race/ethnicity, primary expected payer, and the proportion of patients receiving concomitant nasal surgery were comparatively modest but were statistically significant.
Table 1.
Characteristics of patients undergoing sinus surgery -- Florida, 2000 versus 2009
| 2000 | 2009 | P | |
|---|---|---|---|
| Case count | 8138 | 10242 | |
| Mean age (SD) | 48.6 (15.5) | 50.2 (16.1) | <0.001 |
| Female (%) | 50.8 | 50.8 | 0.9 |
| Race/ethnicity (%) | <0.001 | ||
| White | 84.6 | 80.9 | |
| Hispanic | 7.0 | 8.6 | |
| Black | 5.0 | 6.0 | |
| Other | 3.4 | 4.6 | |
| Expected primary payer (%) | <0.001 | ||
| Private insurance | 75.2 | 69.8 | |
| Medicare | 19.2 | 22.4 | |
| Medicaid | 1.7 | 2.35 | |
| Other | 3.9 | 5.5 | |
| Hospital (%) | 62.7 | 50.0 | <0.001 |
| Nasal surgery (%) | 53.2 | 55.5 | <0.001 |
| Image guidance (%) | 3.1 | 17.3 | <0.001 |
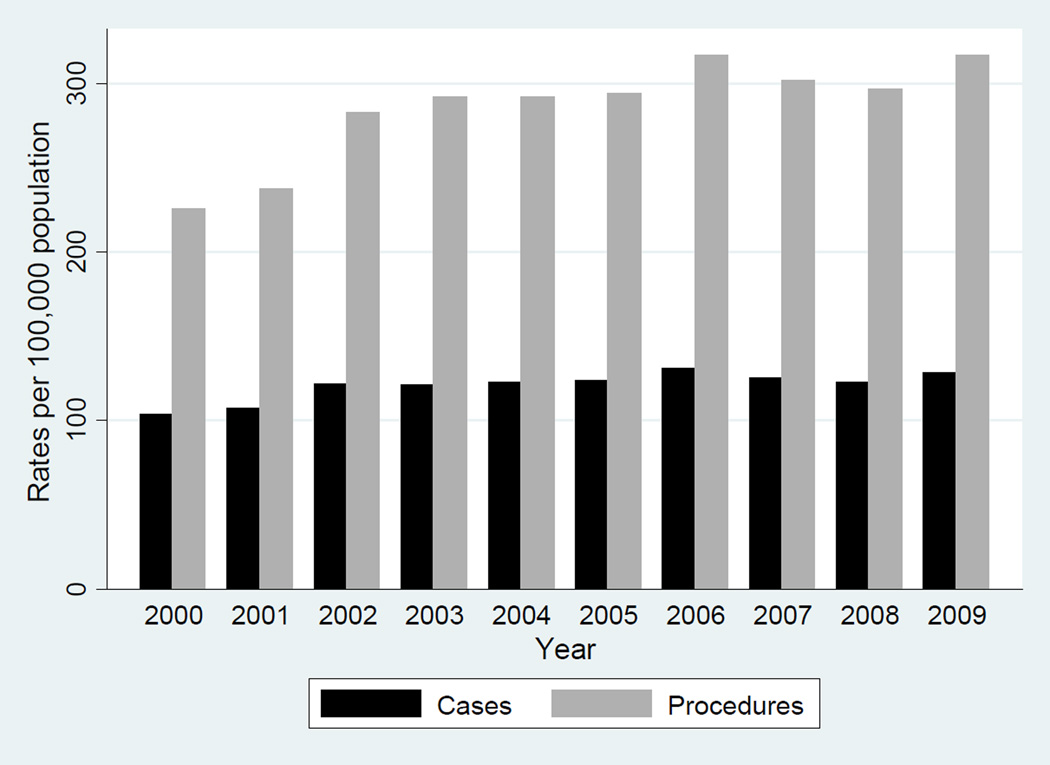
Population-adjusted rates of sinus surgery cases increased over the study period, from an annual mean of 104 cases per 100,000 population in 2000 to 129 per 100,000 in 2009 (p<0.001). Procedure rates also increased, from a mean of 226 per 100,000 in 2000 to 316 per 100,000 in 2009 (p<0.001), consistent with trends over the entire study period (Table 2 and Figure 1).
Table 2.
Population-adjusted rates of sinus surgery – Florida, 2000 versus 2009
| 2000 | 2009 | ||||
|---|---|---|---|---|---|
| Annual Mean (SD) |
Annual Mean (SD) |
Increase | 95% CI for Increase |
P value | |
| Cases | 104.0 (74.6) | 128.9 (80.0) | 24.8 | 22.6, 27.1 | P<0.001 |
| Procedures | 225.8 (167.4) | 316.3 (208.2) | 90.5 | 85.0, 96.1 | P<0.001 |
Rates per 100,000 population, standardized for age and gender by hospital service area
Figure 1.
Trends in population-adjusted rates (per 100,000 population) of sinus surgery cases and procedures – Florida, 2000–2009.
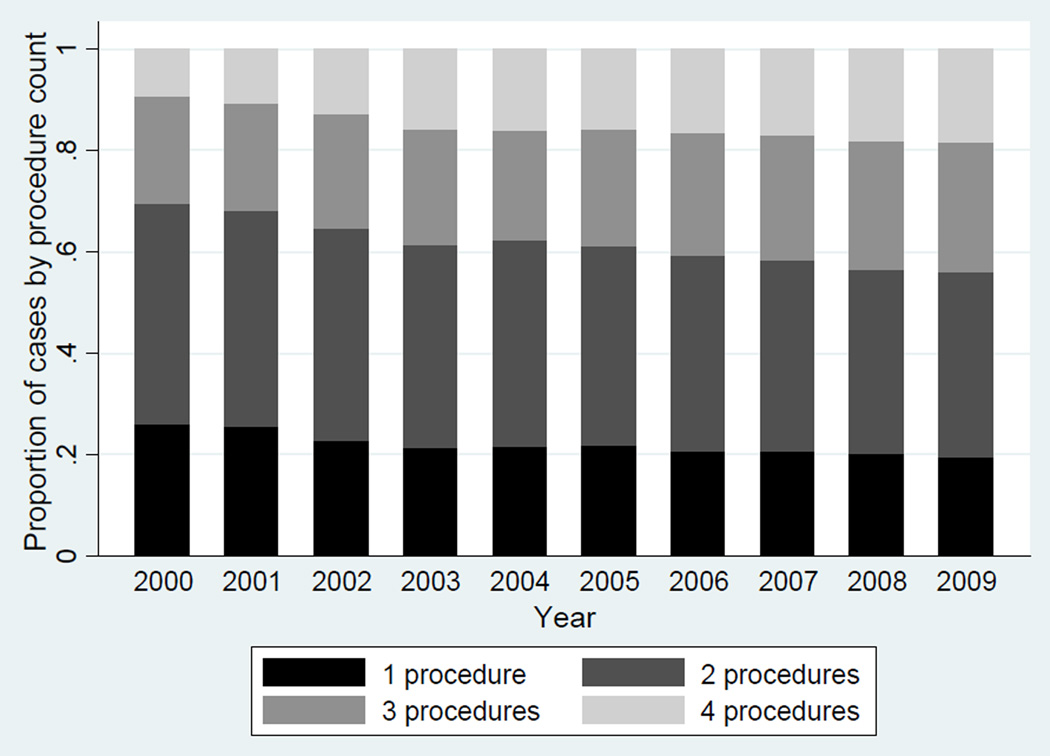
Between 2000 and 2009, population-adjusted rates of all types of sinus procedures increased, with two trends that were particularly salient. Rates of frontal sinus procedures more than doubled, and rates of cases in which all 4 sinuses were treated tripled during the same time period (Table 3 and Figure 2).
Table 3.
Population-adjusted rates of sinus surgery procedures – Florida, 2000 versus 2009. Procedure types are rank-ordered by mean annual rate of procedure in 2009.
| 2000 | 2009 | ||||
|---|---|---|---|---|---|
| Procedure type | Annual Mean (SD) |
Annual Mean (SD) |
Increase (%) |
95% CI for increase |
P Value |
| Maxillary sinus | 84.1 (78.0) | 111.4 (86.7) | 27.4 (32) | 25.0, 29.8 | <0.001 |
| Ethmoid sinus | 89.8 (78.5) | 108.3 (89.4) | 18.5 (21) | 16.1, 21.0 | <0.001 |
| Frontal sinus | 10.4 (26.6) | 26.3 (49.6) | 15.9 (153) | 14.7, 17.1 | <0.001 |
| Sphenoid sinus | 16.4 (41.7) | 25.1 (47.3) | 8.7 (53) | 7.4, 10.0 | <0.001 |
| All 4 sinuses* | 2.3 (11.2) | 6.9 (19.2) | 4.6 (200) | 4.1, 5.0 | <0.001 |
Rates per 100,000 population, standardized for age and gender by hospital service area
Maxillary, ethmoid, sphenoid, and frontal sinus procedures performed
Figure 2.
Comparative proportions of sinus surgery cases by procedure count – Florida, 2000–2009.
Multilevel Analyses
In the adjusted model at level 1 (patients only), we found image guidance was the variable most strongly associated with the number of sinus procedures (Table 4, column 2). Adjusted for time trends, use of image guidance was associated with 18% more sinus procedures per case (95% CI: 16.75%, 19.91%).
Table 4.
Patient-level Factors and Surgeon Case Volume Associated with Number of Procedures per Case
| Unadjusted Patient Level |
Adjusted Patient Level |
Adjusted Patient and Surgeon Levels |
|
|---|---|---|---|
| IRR (SE) 95% CI |
IRR (SE) 95% CI |
IRR (SE) 95% CI |
|
| Female |
#.95 (.004) .95–.96 |
#.95 (.004) .95–.96 |
# .95 (.004) .94–.96 |
| Race/ethnicity | |||
| White | Reference | ##Reference | Reference |
| Black | 1.00 (.010) .99–1.02 |
1.01 (.010) .99–1.03 |
1.02 (.010) 1.00–1.04 |
| Hispanic | .99 (.008) .98–1.01 |
.98 (.008) .96–1.0 |
.99 (.009) .97–1.01 |
| Other | 1.02 (.011) 1.00–1.03 |
.99 (.011) .97–1.02 |
1.00 (.012) .98–1.03 |
| Expected primary payer | |||
| Medicare | ##Reference | ##Reference | Reference |
| Medicaid | .93 (.017) .90–.97 |
.99 (.019) .95–1.02 |
1.00 (.020) .96–1.04 |
| Private insurance | 1.00 (.005) 1.00–1.01 |
1.03 (.008) 1.01–1.04 |
1.01 (.008) 1.00–1.03 |
| Other | .97 (.011) .95–.99 |
1.00 (.013) .97–1.02 |
1.01 (.013) .98–1.03 |
| Hospital | 1.00 (.004) .99–1.01 |
1.01 (.004) 1.00–1.01 |
#1.02 (.006) 1.01–1.03 |
| Nasal surgery |
#.98 (.004) .97–.98 |
#.97 (.004) .96–.98 |
#.96 (.005) .96–.97 |
| Image guidance |
#1.21 (.008) 1.19–1.22 |
#1.18 (.008) 1.17–1.20 |
#1.21 (.010) 1.19–1.23 |
| Surgeon case volume |
#1.002 (.0001) 1.00–1.00 |
||
| Surgeon-specific random effects variance | 0.17 (0.0034) .16–.18 |
||
IRR Incidence rate ratio
SE Standard error
Models were adjusted for study year.
P<0.05 for comparison
P < 0.05 for comparison across entire group
With respect to patient gender and age, male gender was significantly associated with more procedures per case compared with female gender, with a 5% difference in the average number of procedures per case. Increased age (>65 years versus <35 years) was associated with additional procedures per case (data not shown).
Next we considered the surgeons. The number of surgeons in the dataset was fairly consistent over time—annual mean 431 (410–451). The annual case volume per surgeon varied substantially (annual median 15 cases; range 1–235).
In the adjusted level 2 model (patients + surgeons) we found that race and expected primary payer were no longer significant, gender remained significant, and hospital location became a significant predictor of the number of sinus procedures performed per case. The variable, sinus case volume, which describes the surgeon’s annual number of sinus cases, was also a statistically significant predictor. The effect of surgeon case volume for a surgeon with 200 sinus cases annually versus 20 cases annually was a 48% higher association with an additional sinus procedure per case.
However, most notably, the level 2 model found that approximately 17% of the observed variance in sinus procedures performed during the study period was attributable to variation at the level of the surgeon—independent of his annual case volume (Table 4, column 3). This amount of variance was substantially more than the share explained by patient demographics, nasal surgery, image guidance, and the surgeon case volume combined (1%).
Discussion
This study demonstrates that the total number of sinus procedures has increased over the last 10 years at the population level in a large state (Florida)—chiefly attributable to a marked increase in the number of sinus procedures performed per patient case, with a comparatively modest increase in the number of patients with sinusitis who undergo surgery. Additionally, we find that frontal sinus procedures increased 153%, and that operations in which all 4 sinus procedures were performed increased 200% over the study period.
The findings we report build upon Venkatraman’s study,13 which demonstrated increased rates of endoscopic sinus surgery among Medicare patients, and Psaltis’s study,19 which demonstrated increased numbers endoscopic sinus surgery procedures. Because we analyzed 10 years of data and because we report growth in sinus surgery as a rate, our findings substantially build upon the Psaltis report that was limited to 3 years of procedure counts and did not control for the size or changes in size of the reference population.
Although we do not have a clinical explanation for these changes, this study did not include patient-level covariates that might explain these findings. While the prevalence and severity of sinus disease are not expected to have increased during the study period,1,2 a limitation of this study is that we do not have information on disease severity, such as CT, endoscopy, or quality of life scores. In addition to clinical factors, there may be non-clinical factors, at the patient and provider level, that partially explain this finding. It is possible that increased patient acceptance of sinus surgery, technological advances, and a greater numbers of surgeons trained in endoscopic sinus surgery techniques have contributed to the growth in endoscopic sinus procedures. Over the last two decades, traditional sinus surgery techniques have been replaced with endoscopic techniques because of the improved visualization and shorter patient recovery times20 consequently, more surgeons have been trained in endoscopic techniques during this time and it is now a routine part of residency training and surgical practice.
Surgical instrumentation has also evolved during this time and two specific innovations, image guidance and balloon dilation, may have contributed to perceived ease and safety of endoscopic sinus surgery. Image guidance was introduced in the 1990s and was initially used primarily in academic and tertiary care rhinology settings because of the cost of the device. Over time, image guidance has become more widespread and now a majority of practitioners surveyed report access to the technology.21 Balloon dilation technology is a more recent development, introduced in 2006.22–25 The sinus balloon may be threaded through natural sinus opening using a guide wire. Inflation of the balloon dilates the sinus opening, and neither bone nor mucosa is resected. The extent to which sinus balloon devices contributed to the observed increase in sinus procedures per case cannot be determined with this dataset. However, in 2011 new CPT codes specific for balloon sinus surgery were introduced. Future research using these new CPT codes may be able to discern the proportion of growth of frontal sinus surgery attributable to this new technology.
Our initial hypothesis, that variations in sinus surgery are driven by non-clinical factors, appears strongly supported by this analysis. The multilevel model demonstrated that the individual surgeon accounts for the majority of variance in the number of sinus procedures performed during each case. In fact, even patient-level factors (gender, nasal surgery, and image guidance) statistically significantly associated with sinus procedure patterns were comparatively weak determinants of the procedures performed when surgeon identity was taken into account. This point highlights two important limitations of this study which must be understood so the findings are not taken out of context. First, our analysis was restricted to the procedures performed, and we could not analyze clinical presentations and outcomes. It is possible that changes in patients’ presentation or desires for different clinical outcomes over the study duration led surgeons to modify their practice patterns over time. From these data, we cannot know whether the changes in procedural patterns led to positive, negative, or negligible changes in patients’ outcomes. A second important limitation is that we lack information about referral patterns and surgeon case mix that may impact surgeon case volume. This study design did not differentiate a rhinology specialist with a complex case mix from a general otolaryngologist with a less complex case mix.”
Our inability to distinguish unilateral from bilateral procedures may be perceived as a limitation. We recognize this perspective but we believe the salient perspective is the location of the sinuses—i.e. extent of surgical dissection. Other limitations of this study include those common to analyses based on administrative data—i.e., that procedures and diagnoses may have been miscoded and therefore are subject to errors of omission and commission. Furthermore, we chose Florida because the ambulatory surgical data for this state are particularly robust and have been used in other studies indicative of broader patterns of care,26–29 but it is possible that patterns in other states may have differed and the results of this single state are not necessarily representative of the broader US population.
Conclusion
In conclusion, we find that during 2000–2009 rates of sinus surgery in Florida increased at the population level, as measured by the number of operations and the number of procedures performed during each operation. Patients with a greater number of procedures performed during surgery were more likely to have had concomitant use of image guidance, and to have had surgery performed by a surgeon with a high annual case volume. However, the strongest predictor was the individual surgeon. The strong association of procedural patterns with specific surgeons in sinusitis care highlights the importance of future investigations to examine training, technological, and reimbursement factors that may influence surgeons’ clinical decision-making for this common condition.
Acknowledgements
The authors wish to thank the Dow Division of Health Services Research, Department of Urology, University of Michigan, for use of the State Ambulatory Surgery Dataset.
Grant support for this project was provided from the Michigan Institute for Clinical and Health Research (NCATS UL1RR0249863).
Footnotes
The authors have no financial interests, disclosures or conflicts of interest regarding the content of this original manuscript.
References
- 1.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Vital Health Stat 10. 2010 Dec;(249):1–207. [PubMed] [Google Scholar]
- 2.Prevalence of selected chronic conditions. United States, 1979–81. Vital Health Stat 10. 1986 Jul;(155):1–66. [PubMed] [Google Scholar]
- 3.Sharp HJ, Denman D, Puumala S, Leopold DA. Treatment of acute and chronic rhinosinusitis in the United States, 1999–2002. Arch Otolaryngol Head Neck Surg. 2007 Mar;133(3):260–265. doi: 10.1001/archotol.133.3.260. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope. 2010 Mar;120(3):635–638. doi: 10.1002/lary.20777. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya N. Ambulatory pediatric otolaryngologic procedures in the United States: characteristics and perioperative safety. Laryngoscope. 2010 Apr;120(4):821–825. doi: 10.1002/lary.20852. [DOI] [PubMed] [Google Scholar]
- 6.Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007 Sep;137(3 Suppl):S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 7.Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE. Variation profiles of common surgical procedures. Surgery. 1998 Nov;124(5):917–923. [PubMed] [Google Scholar]
- 8.Wennberg JE, Barnes BA, Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med. 1982;16(7):811–824. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- 9.Leape LL, Park RE, Solomon DH, Chassin MR, Kosecoff J, Brook RH. Does inappropriate use explain small-area variations in the use of health care services? JAMA. 1990 Feb 2;263(5):669–672. [PubMed] [Google Scholar]
- 10.Chassin MR. Explaining geographic variations. The enthusiasm hypothesis. Med Care. 1993 May;31(5 Suppl):YS37–YS44. doi: 10.1097/00005650-199305001-00006. [DOI] [PubMed] [Google Scholar]
- 11.Chassin MR, Kosecoff J, Park RE, et al. Does inappropriate use explain geographic variations in the use of health care services? A study of three procedures. JAMA. 1987 Nov 13;258(18):2533–2537. [PubMed] [Google Scholar]
- 12.HCUP State Ambulatory Surgery Databases (SASD) Healthcare Cost and Utilization Project (HCUP) Rockville, MD.: Agency for Healthcare Research and Quality; 200–2009. www.hcup-us.ahrq.gov/sasdoverview.jsp. [Google Scholar]
- 13.Venkatraman G, Likosky DS, Zhou W, Finlayson SR, Goodman DC. Trends in endoscopic sinus surgery rates in the Medicare population. Arch Otolaryngol Head Neck Surg. 2010 May;136(5):426–430. doi: 10.1001/archoto.2010.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wennberg J, Gittelsohn Small area variations in health care delivery. 1973 Dec 14;182(4117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 15.The Dartmouth Institute for Health Policy and Clinical Practice. The Dartmouth Atlas of Health Care. http://www.dartmouthatlas.org/. [Google Scholar]
- 16.Census. U.S. Population estimates for Florida. Available from: http://www.census.gov/popest/intercensal/state/ST-EST00INT-02.html.
- 17.Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. Journal of the American Statistical Association. 1993;88:9–25. [Google Scholar]
- 18.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2nd ed. College Station, TX: Stata Press; 2008. [Google Scholar]
- 19.Psaltis AJ, Soler ZM, et al. "Changing trends in sinus and septal surgery, 2007 to 2009". Int Forum Allergy Rhinol. 2012;2(5):357–361. doi: 10.1002/alr.21036. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy DW, Zinreich SJ, Rosenbaum AE, Johns ME. Functional endoscopic sinus surgery. Theory and diagnostic evaluation. Arch Otolaryngol. 1985 Sep;111(9):576–582. doi: 10.1001/archotol.1985.00800110054002. [DOI] [PubMed] [Google Scholar]
- 21.Justice JM, Orlandi RR. An update on attitudes and use of image-guided surgery. Int Forum Allergy Rhinol. 2012 Mar-Apr;2(2):155–159. doi: 10.1002/alr.20107. [DOI] [PubMed] [Google Scholar]
- 22.Brown CL, Bolger WE. Safety and feasibility of balloon catheter dilation of paranasal sinus ostia: a preliminary investigation. Ann Otol Rhinol Laryngol. 2006 Apr;115(4):293–299. doi: 10.1177/000348940611500407. discussion 300-291. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed J, Pal S, Hopkins C, Jayaraj S. Functional endoscopic balloon dilation of sinus ostia for chronic rhinosinusitis. Cochrane Database Syst Rev. 2011;(7):CD008515. doi: 10.1002/14651858.CD008515.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Weiss RL, Church CA, Kuhn FA, Levine HL, Sillers MJ, Vaughan WC. Long-term outcome analysis of balloon catheter sinusotomy: two-year follow-up. Otolaryngol Head Neck Surg. 2008 Sep;139(3) Suppl 3:S38–S46. doi: 10.1016/j.otohns.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Kuhn FA, Church CA, Goldberg AN, et al. Balloon catheter sinusotomy: one-year follow-up--outcomes and role in functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2008 Sep;139(3) Suppl 3:S27–S37. doi: 10.1016/j.otohns.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Hollenbeck BK, Hollingsworth JM, Dunn RL, Zaojun Y, Birkmeyer JD. Ambulatory surgery center market share and rates of outpatient surgery in the elderly. Surg Innov. Dec 17;(4):340–345. doi: 10.1177/1553350610377211. [DOI] [PubMed] [Google Scholar]
- 27.Hollingsworth JM, Krein SL, Birkmeyer JD, et al. Opening ambulatory surgery centers and stone surgery rates in health care markets. J Urol. 2010 Sep;184(3):967–971. doi: 10.1016/j.juro.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 28.Hollingsworth JM, Krein SL, Ye Z, Kim HM, Hollenbeck BK. Opening of ambulatory surgery centers and procedure use in elderly patients: data from Florida. Arch Surg. Feb;146(2):187–193. doi: 10.1001/archsurg.2010.335. [DOI] [PubMed] [Google Scholar]
- 29.Hollingsworth JM, Ye Z, Strope SA, Krein SL, Hollenbeck AT, Hollenbeck BK. Urologist ownership of ambulatory surgery centers and urinary stone surgery use. Health Serv Res. 2009 Aug;44(4):1370–1384. doi: 10.1111/j.1475-6773.2009.00966.x. [DOI] [PMC free article] [PubMed] [Google Scholar]