Abstract
The mucosal surfaces of the respiratory, gastrointestinal and urogenital tracts are covered by a layer of epithelial cells that are responsible for sensing and promoting a host immune response in order to establish the limits not only for commensal microorganisms but also for foreign organisms or particles. This is a remarkable task as the human body represents a composite of about 10 trillion human-self cells plus non-self cells from autochthonous or indigenous microbes that outnumber human cells 10:1. Hence, the homeostasis of epithelial cells that line mucosal surfaces relies on a fine-tuned immune system that patrols the boundaries between human and microbial cells. In the case of the intestine, the epithelial layer is composed of at least six epithelial cell lineages that act as a physiological barrier in addition to aiding digestion and the absorption of nutrients, water and electrolytes. In this review, we highlight the immense role of the intestinal epithelium in coordinating the mucosal innate immune response.
Keywords: Intestine, Inflammation, Epithelial cells, Innate immunity, Microbes, Human
Keeping the boundaries
As a barrier, the intestinal mucosa is well organized with absorptive enterocytes forming a layer of columnar-shaped cells or microvillus epithelium. This layer separates the intestinal lumen (mucosal) from the sub-epithelial lamina propria or basolateral domain (serosal) in which the mucosal immune cells reside. Moreover, a mucus layer covers the intestinal lumen, further restricting any contact between microorganisms and epithelial cells. This mucus layer is composed of mucin glycoproteins and trefoil peptides that are secreted by goblet cells located in both the villus and crypt epithelium of the entire intestinal tract. Humans possess at least 18 mucin-type glycoproteins. MUC2 is the predominant component of the mucin layer found in both the small and large bowel; in addition, intestinal trefoil factor 3 (TFF3) is co-expressed with MUC2. A wealth of evidence suggests that the mucin/trefoil layer protects the intestinal epithelium from luminal pathogens and bacterial toxins and, at the same time, promotes wound repair (Kindon et al. 1995; de Repentigny et al. 2000; Kalabis et al. 2006). Experiments in mice, for example, have shown that the absence of MUC2 expression is associated with rapid weight loss and enhanced mortality (Bergstrom et al. 2010). Moreover, a comparison of patients suffering from inflammatory bowel disease (IBD) with healthy controls has provided evidence of a thinning of the mucus layer associated with augmentation of Streptococcus in Crohn’s disease (CrD) and of Lactobacillus in ulcerative colitis (Fyderek et al. 2009), increased villous injury (Sharpe et al. 2010) and heightened infiltration of bacteria and inflammatory cells (Corazziari 2009). These examples illustrate the important role that the mucus layer plays in forming a protective barrier to the lining of epithelial cells.
Immunoglobulin A (IgA) offers another protective strategy that thwarts pathogen invasion to the intestinal epithelium. Undifferentiated crypt enterocytes secrete IgA into the intestinal lumen via the polymeric immunoglobulin receptor (pIgR; Mostov 1994). Inside the epithelial cell, IgA can deactivate bacterial lipoproteins. Once in the lumen, IgA binds to the mucus layer located above the epithelial surface, where it aids in inhibiting the permeability and adherence of microorganisms and also neutralizes their toxins. Therefore, IgA plays an important role in maintaining the balance between the host and its indigenous bacteria or incoming pathogens by limiting their localization to the lumen (Apodaca et al. 1991). Indeed, IgA represents the most abundant immunoglobulin found in the gut.
Furthermore, a wide range of antimicrobial peptides (AMPs), inflammatory mediators and signaling molecules are secreted by Paneth cells, which also assist in the maintenance of microbial homeostais within the gastrointestinal (GI) tract (Keshav 2006). AMPs are cationic molecules produced to defend the host against insult by microbial pathogens. These molecules act as lytic enzymes that disturb the microbial cell membrane structure and/or its function (Ganz 1999). At least three primary AMPs are expressed in the gut: defensins, lyzozymes and cathelicidins.
Defensins represent the predominant family of AMPs in mammals and possess a wide spectrum of antimicrobial activity (even at micromolar concentrations) against bacteria, fungi and some enveloped viruses. AMPs attach to the microbial membrane and disrupt it by forming a pore that leads to the efflux of ions and nutrients. Three types of human defensins have been identified and these differ with respect to the arrangement of their cysteine residues and the organization of their disulfide bridges: (1) α-defensins are mainly expressed in neutrophils and natural killer (NK) cells but are also found in granules of Paneth cells within the small intestine (Ouellette and Selsted 1996); (2) β- defensins are produced by numerous epithelial (Diamond and Bevins 1998; Fehlbaum et al. 2000) and nonepithelial (Garcia et al. 2001) cells; and (3) non-human θ-defensins are found in the granules of leukocytes (Tang et al. 1999) and bone marrow (Leonova et al. 2001) of the rhesus macaque.
The role of α-defensins in GI mucosal immunity has been previously documented for human α-defensin-5 (HD-5) by using transgenic mice (Wilson et al. 1999; Vaishnava et al. 2008). Salzman et al. (2003) have found that the expression of HD-5 in transgenic mice is associated with resistance to orally administered Salmonella enterica serovar Typhimurium. In this study, transgenic mice recover following an initial onset of illness (12 h post-infection), whereas wild-type mice present 100% mortality after 24 h of infection. Moreover, the titer of Salmonella typhimurium recovered from wild-type mice is three log-fold greater than that recovered from transgenic mice (Salzman et al. 2003). Interestingly, α-defensins are released exclusively by Paneth cells, which primarily reside in the small intestine and yet this protein can be found at relevant concentrations in the lumen of the distal colon, suggesting that it can resist degradation/proteolysis all the way through the intestine, thus emphasizing its role as a key player in colonic mucosal immunity (Mastroianni and Ouellette 2009).
Deficiency of α-defensin activity in patients with inflamed intestine is associated with not only tolerance to pathogens but also tolerance to indigenous intestinal microbiota (Duchmann et al. 1995; Salzman et al. 2007). This suggests that some primary defect in antibacterial α-defensins might lead to chronic inflammation. More recently, Salzman and collaborators (2010) have performed an extensive analysis on the changes that occur within the intestinal microbiota when comparing homozygous with heterozygous strains of transgenic mice encoding human Paneth cell α-defensin 5 (DEFA5). This team of investigators has found that mice lacking α-defensins show a significant increase in Firmicutes while at the same time exhibiting a decrease in Bacteroidetes as compared with mice over-expressing α-defensin. This finding implies that α-defensins, specifically DEFA5, play a fundamental role in altering the bacterial composition of the intestinal microbiota (Salzman et al. 2010).
β-Defensins are antimicrobial peptides that reside at the epithelial surface and are involved in host defense against both bacteria and fungi. These defensins are continuously expressed throughout the GI tract, where they play a role in controlling the microbial population. For example, human β-defensin 1 (HBD1) is constitutively expressed by epithelial cells in the small intestine (Zhao et al. 1996) and is effective in eradicating Escherichia coli and S. typhimurium (Schröder 1999; De Smet and Contreras 2005). Other human β-defensins, such as HBD2 and HBD3, are widely expressed within the epithelium of various tissues including the intestine. These β-defensins have antimicrobial activity against Gram-negative bacteria (E. coli and P. aeruginosa), several Gram-positive bacteria (Streptococcus pyogenes, Streptococcus pneumoniae, Staphylococcus aureus, Staphylococcus carnosus, multiresistant S. aureus strains and even the vancomycinresistant Enterococcus faecium) and yeasts (Candida albicans, Saccharomyces cerevisiae and Malassezia furfur; Jia et al. 2001).
β-Defensins also trigger the activation and degranulation of mast cells, liberating histamine and prostaglandin D2 (Bensch et al. 1995). Increased levels of histamine have been associated with CrD (Knutson et al. 1990) and with ulcerative colitis (Raithel et al. 1995), raising the possibility that the active involvement of histamine in the pathogenesis of these diseases results from the action of β-defensins on mast cells degranulation.
Lyzozymes and cathelicidins are additional AMPs that reside within the intestinal niche. Lysozymes represent mureinolytic enzymes that are produced in the human GI tract by Paneth cells. These enzymes are able to catalyze the hydrolysis of murein on the bacterial cell wall, providing effective protection against Gram-positive infection (Fleming 1922). The human cathelicidin, LL-37, is also expressed by intestinal epithelial cells (Hase et al. 2002, 2003; Tollin et al. 2003) and, like the other AMPs, is involved in microbial homeostasis within the GI tract. As an example, Iimura et al. (2005) have found that the intestinal epithelium of mice lacking the murine homolog of human LL-37 exhibits high susceptibility to colonization by the lumen microbiota. In addition, in the gastric epithelium, gastric epithelial cells infected with Helicobacter pylori appear to up-regulate the production of LL-37 (Hase et al. 2003). Such regulation is inferred to be crucial for maintaining the balance between the host mucosal response and gastric pathogen survival mechanisms, which can cause a lifetime of chronic infection. On the other hand, evidence is available that the expression of LL-37 is downregulated in biopsies taken from Shigella-infected patients, particularly in early infection; this might contribute to the pathogenesis caused by the bacterium (Islam et al. 2001)
Collectively, this first line of defense staged by epithelial cells operates in a coordinated fashion to maintain boundaries and homeostasis. Epithelial cells products, such as mucus, AMPs and the release of IgA, keep autochthonous bacterial communities under growth-expansion control. In addition, these epithelial cell products exert a direct effect against incoming pathogenic insults.
Coming closer: direct interaction with the intestinal epithelial cell
To overcome the primary line of host defense, many microbes have evolved strategies to counter this initial attack and gain access to the basolateral epithelial domain in which the immune cells reside. Microfold cells (M cells) are associated with the transepithelial vesicular trafficking of antigens and microorganisms, including pathogens and indigenous microbes, from the intestinal lumen into the underlying gut-associated lymphoid tissue (GALT). The structure of this specialized epithelial cell is quite distinct compared with the rest of the cells in the epithelium. M cells lack an apical rigid brush border and instead, the membrane surface elaborates micro-projections that facilitate efficient endocytosis and transcytosis of microorganisms. The basolateral side of the M cells is invaginated forming a large intra-epithelial “pocket” in which immune cells such as T and B lymphocytes and macrophages reside (Neutra and Kraehenbuhl 2003).
Bacterial internalization into and translocation across the M cells triggers the generation of IgA within the basolateral space. Bacterial translocation across M cells also promotes the proliferation of antigen-specific B lymphoblasts that migrate throughout the blood stream to the intestinal mucosa, where differentiation into plasma cells occurs (Neutra and Kraehenbuhl 2003). Based on infections carried out in ligated ileal loops in rabbits and in monkeys, M cells represent a major entry site of Shigella flexneri at early stages of infection (Sansonetti et al. 1996). Once S. flexneri gains access to the basolateral domain, this organism is able to infect the intestinal epithelium prompting an intense inflammatory reaction manifested clinically as the passage of bloody diarrhea. Evidence has also been presented that M cells are a major entry site of S. typhimurium (Jones et al. 1994; Marchetti et al. 2004), Yersinia enterocolitica and Yersinia pseudotuberculosis (Grutzkau et al. 1990; Marra and Isberg 1997).
However, given the vast epithelial surface area relative to the M cell surface area in the human large intestine (far less than 1%), othermechanisms allowing access to the basolateral membrane domain most probably exist (Perdomo et al. 1994). We have proposed that S. flexneri alters the intestinal barrier function, specifically the tight junctional complex (TJC), which in turn facilitates the paracellular passage of the organism through the intestinal epithelial barrier (Sakaguchi et al. 2002). The TJC is a specialized membrane domain at the most apical region of polarized epithelial cells. Together, the tight junction proteins, claudins and occludins form the major structural component of the tight junctional strands that seal the intercellular space and delineate apical from basolateral domains. The claudins (Furuse et al. 1998) and occludins (Furuse et al. 1993; Ando-Akatsuka et al. 1996) interact with the PDZ domains of the zonula occludens proteins ZO-1 and ZO-2 (Furuse et al. 1994; Itoh et al. 1999), which bind directly to actin filaments at their COOHterminal regions, enabling them to function as cross-linkers between tight junction strands and actin filaments (Wittchen et al. 1999; Fanning et al. 1998; Itoh et al. 1999). The breakdown of TJC integrity occurs in response to bacterial products such as Clostridium perfringens enterotoxin (Sonoda et al. 1999), cytotoxic necrotizing factor 1 from E. coli (Oswald et al. 1994), Clostridium difficile toxins (Nusrat et al. 1995; Nusrat et al. 2001), Bordetella dermonecrotic toxin (Horiguchi et al. 1995) and zonula occludens toxin from Vibrio cholerae (Fasano et al. 2000). The invasion of intestinal epithelial cells by Salmonella typhi can also disturb the TJC seal (Chen et al. 1996), whereas enteropathogenic E. coli de-phosphorylate and dissociate occludin from TJC (Simonovic et al. 2000).
The intestinal epithelium has also evolved receptors, such as the extracellular Toll-like receptors (TLRs) and the intracellular Nod-like receptors, to identify pathogens or pathogen-associated molecular patterns (PAMPs) that have breached the epithelial barrier by the recognition of conserved microbial elements such as flagellin, peptidoglycan, lipopolysaccharide (LPS) and formylated peptides. In general, upon specific microbial recognition, these receptors recruit adaptor proteins, such as MyD88, TRIF, TIRAP, TRAM and Rip2, which elicit the activation of signaling cascades that regulate the expression of nuclear factor kappa-B (NF-κB), mitogen-activated protein kinases (MAPK), or caspase-dependent signaling pathways. This activation induces the expression of pro-inflammatory and antimicrobial mediators, including interleukin (IL)-6, tumor necrosis factor alpha (TNF-α) and IL-1β (Kawai and Akira 2006).
In particular, TLRs represent a conventional pattern recognition system of innate immunity with the remarkable ability to discriminate between distinct variant microbial structures/molecules from self (microbiota or commensal bacteria) and non-self, pathogenic microbes (Takeda et al. 2003). Thus, these receptors are able to orchestrate the production of inflammatory cytokines, chemotactic factors and antimicrobial products in response to certain intestinal cues (Bogunovic et al. 2007; Cario and Podolsky 2000; Abreu et al. 2001). To date, at least 11 TLR human homologs have been identified. The molecular structure of TLRs comprises three domains: (1) the extracellular domain, which exhibits a repeated leucine-rich motif, (2) the transmembranal domain and (3) the globular domain or Toll/IL-1 receptor domain localized within the cytoplasm. In addition, the location of each TLR on the extracellular cell surface determines ligand specificity and accessibility.
TLR4 is one of the best-studied TLRs. This receptor is crucial for the recognition of LPS, a major component of the outer membrane of Gram-negative bacteria. Indeed, lack of response to the LPS challenge has been associated with tlr4 gene mutations or deletions (Hoshino et al. 1999; Poltorak et al. 1998; Qureshi et al. 1999). TLR4 is located at the apical pole of differentiated intestinal epithelial cells. However, in vitro challenge of intestinal cell lines with LPS has been shown to promote TLR4 redistribution. For example, Cario et al. (2002) have demonstrated that the trafficking of TLR4 via transcytosis to the basolateral domain occurs following LPS-basolateral stimulation of differentiated T84 cells. Whereas the role of TLR4 on the basolateral domain remains to be determined, one study has revealed this receptor to be located at the epithelial basolateral domain during active ulcerative colitis (Cario and Podolsky 2000). Conversely, TLR5 is constitutively expressed at the basolateral domain of the intestinal epithelium and recognizes bacterial flagella. In this location, TLR5 serves as a molecular beacon by providing a mechanism in which only those microbes that invade or translocate flagellin, such as S. typhimurium but not commensal bacteria, induce intestinal epithelia to orchestrate an inflammatory response (Lyons et al. 2004; Gewirtz et al. 2001).
Additionally, the intracellular and surface expression of TLR9 has been detected in the intestinal cell line (HT-29). TLR9, which recognizes bacterial/viral DNA and unmethylated CpG dideoxynucleotides, has been associated with the proliferation of B cells and the activation of macrophages and dendritic cells (Hemmi et al. 2000). Moreover, HT-29 cells infected with DNA from Salmonella enterica serovar Dublin exhibit an increased expression of TLR9 at the cell surface (Ewaschuk et al. 2007). Thus, the polarized but not static distribution, of TLRs on the intestinal epithelium seems to be governed by microbial stimulation, supporting the sentinel role of TLRs in GI mucosal immunity.
The intracellular recognition of PAMPs is facilitated by NOD-like receptors (NLRs). The NLRs possess a protein-protein interaction domain at the N-terminus; this is commonly composed of a caspase recruitment domain (CARD) or pyrin domain (PYD). The CARD and PYD domains represent essential elements of protein recognition critical for downstream signaling and are both involved in apoptosis and inflammation. NLRs also contain a nucleotide-binding oligomerization domain (NOD) that establishes self-oligomerization during NLR activation and a C-terminal leucine-rich repeat for PAMPs recognition.
The best-characterized NLRs are NOD1 and NOD2, both of which represent pattern recognition receptors that identify different structural core motifs derived from peptidoglycan, a main constituent of bacterial cell walls. NOD1 is ubiquitously expressed by intestinal epithelial cells, whereas only monocytes, macrophages, dendritic cells and intestinal Paneth cells express NOD2. These two NLRs interact with an adaptor protein (Rip2), subsequently promoting the activation of the NF-κB and MAPK pathways (Girardin et al. 2001; Pauleau and Murray 2003).
Bacteria equipped with secretion systems, such as Samonella and Helicobacter, or those that produce pore- forming toxins, such as the pneumolysin of Streptococcus pneumoniae, the anthrolysin O of Bacillus anthracis, or the α-toxin of Staphylococcus aureus, can promote the internalization of peptidoglycan fragments from extracellular bacteria into the cytoplasm of epithelial cells, thus activating intracellular NOD receptors. Alternatively, a human oligopeptide transporter (hPepT1), which is expressed in inflamed but not in non-inflamed colonic epithelial cells, can carry out the transport of bacterial derivates, such as N-formylated tripeptide N-formylmethionylleucyl-phenylalanine (fMLP) produced by E. coli and muramyl-dipeptides from the bacterial cell wall, into the cytosol of colonic epithelial cells; this might elicit the host immune response via NOD-like receptors recognition (Vavricka et al. 2004; Merlin et al. 2001; Charrier and Merlin 2006). In addition, NOD1/2 can be recruited to the plasma-cell membrane from its intracellular localization, allowing a third method of NODdependent immune response activation (Barnich et al. 2005; Kufer et al. 2008).
NOD2 is also known as the CARD receptor 15 (CARD15) and is highly expressed in Paneth cells; its stimulation promotes the activation of NF-κB and production of α- defensins. In addition, evidence exists for the role of NOD2 as an antibacterial modulator that restricts Salmonella proliferation in the intestinal epithelial cells (Hisamatsu et al. 2003). Mutations in NOD2 also lead to significant deficiency of HD5 and HD6; this has been associated with ileal CrD (Wehkamp et al. 2005; Nuding et al. 2007) and chronic inflammation in IBD (Arijs et al. 2009). In a landmark study, Ogura et al. (2001) determined the association between frame-shift mutations of the nod2 gene and patients with CrD. Indeed, one of the models proposed for the development of CrD suggests that mutations in NOD2 might alter the mucosal host–microbial interactions through the modulation of α-defensins expression and are thus a risk factor for the disease (Cho 2008). Moreover, Biswas and colleagues (2010) have discovered that NOD2-deficient mice develop a Th1-depedent granulomatous inflammation of the ileum when infected with Helicobacter hepaticus.
Recent studies have also revealed the involvement of NOD2 expression in the homeostasis of the intestinal microbiota. As an example, Petnicki-Ocwieja et al. (2009) have found that (1) NOD2 expression is activated by normal microbiota and that germ-free mice express significantly fewer receptors than wild-type mice; (2) the NOD2-deficient mouse harbors an increased load of indigenous resident bacteria in its intestine and that this phenomenon is independent of Rip2 expression; and (3) NOD2-deficient mice are less able to eradicate pathogens. Therefore, functional NOD2 appears to restrict chronic intestinal inflammation and in a feedback fashion, NOD2 and indigenous microbiota maintain the balance in the intestine by restricting the establishment of pathogens.
Concluding remarks
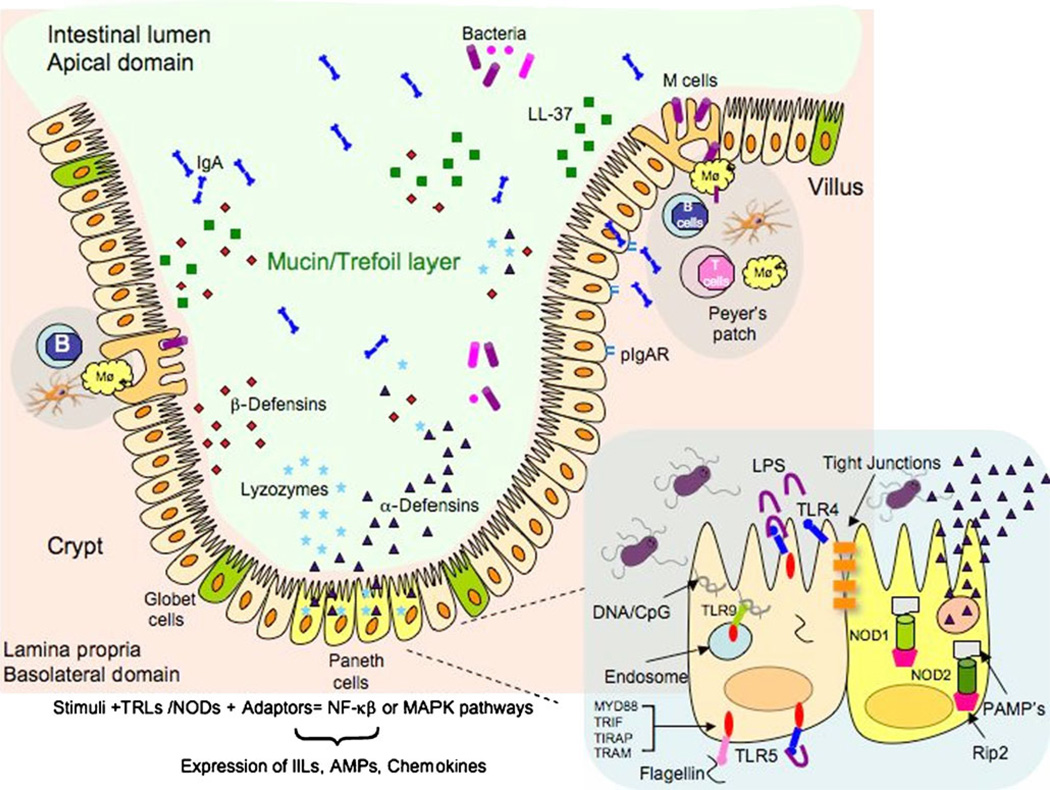
A representation of the role of epithelial cells in the immunity of the intestinal mucosal is presented in Fig. 1. We have highlighted the main functions of intestinal epithelial cells in their various roles as a mucosal barrier and in innate mucosal immunity. The intestinal epithelium represents the first line of defense and is sufficiently equipped and finely tuned to face frequent challenges from self and non-self, transient and resident microorganisms. However, this intestinal barrier also co-evolved with normal and pathogenic flora. Thus, a diverse mucosal immune response exists to maintain a homeostatic host-commensal balance, to signal when such boundaries have been disrupted, and to respond appropriately to pathogenic insult or injury during disease.
Fig. 1.
Representation of intestinal epithelial cell activities that regulate innate mucosal immunity (AMPs antimicrobial peptides, IILs interleukins, IgA immunoglobulin A, pIgAR polimeric immunoglobulin A receptor, LL-37 human cathelicidin, LPS lipopolysaccharide, M cells microfold cells, Mϕ macrophage, MAPK mitogen-activated protein kinases, MYD88, TRIF, TIRAP, TRAM, Rip2 adaptor proteins, NF-κB nuclear factor kappa-B, NOD Nucleotide-binding oligomerization domain, PAMP’s pathogen-associated molecular patterns, TLR Toll-like receptors)
Abbreviations
- AMPs
Antimicrobial peptides
- CARD
Caspase recruitment domain
- CrD
Crohn’s disease
- GALT
Gut-associated lymphoid tissue
- GI
Gastrointestinal
- IBD
Irritable bowel disease
- IL
Interleukins
- IgA
Immunoglobulin A
- pIgAR
Polimeric immunoglobulin A receptor
- LPS
Lipopolysaccharide
- M cells
Microfold cells
- MAPK
Mitogen-activated protein kinases
- NF-κB
Nuclear factor kappa-B
- NK
Natural killer
- NOD
Nucleotide-binding oligomerization domain
- NLRs
NOD-like receptors
- PAMPs
Pathogen-associated molecular patterns
- PYD
Pyrin domain
- TLR
Toll-like receptors
References
- Abreu MT, Vora P, Faure E, Thomas LS, Arnold ET, Arditi M. Decreased expression of Toll-like receptor-4 and MD-2 correlates with intestinal epithelial cell protection against dysregulated proinflammatory gene expression in response to bacterial lipopolysaccharide. J Immunol. 2001;167:1609–1616. doi: 10.4049/jimmunol.167.3.1609. [DOI] [PubMed] [Google Scholar]
- Ando-Akatsuka Y, Saitou M, Hirase T, Kishi M, Sakakibara A, Itoh M, Yonemura S, Furuse M, Tsukita S. Interspecies diversity of the occludin sequence: cDNA cloning of human, mouse, dog, and rat-kangaroo homologues. J Cell Biol. 1996;133:43–47. doi: 10.1083/jcb.133.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apodaca G, Bomsel M, Arden J, Breitfeld PP, Tang K, Mostov KE. The polymeric immunoglobulin receptor. A model protein to study transcytosis. J Clin Invest. 1991;87:1877–1882. doi: 10.1172/JCI115211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arijs I, De Hertogh G, Lemaire K, Quintens R, Van Lommel L, Van Steen K, Leemans P, Cleynen I, Van Assche G, Vermeire S, Geboes K, Schuit F, Rutgeerts P. Mucosal gene expression of antimicrobial peptides in inflammatory bowel disease before and after first infliximab treatment. PLoS ONE. 2009;4:e7984. doi: 10.1371/journal.pone.0007984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnich N, Aguirre JE, Reinecker HC, Xavier R, Podolsky DK. Membrane recruitment of NOD2 in intestinal epithelial cells is essential for nuclear factor-{kappa}B activation in muramyl dipeptide recognition. J Cell Biol. 2005;170:21–26. doi: 10.1083/jcb.200502153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensch KW, Raida M, Magert HJ, Schulz-Knappe P, Forssmann WG. hBD-1: a novel beta-defensin from human plasma. FEBS Lett. 1995;368:331–335. doi: 10.1016/0014-5793(95)00687-5. [DOI] [PubMed] [Google Scholar]
- Bergstrom KS, Kissoon-Singh V, Gibson DL, Ma C, Montero M, Sham HP, Ryz N, Huang T, Velcich A, Finlay BB, Chadee K, Vallance BA. Muc2 protects against lethal infectious colitis by disassociating pathogenic and commensal bacteria from the colonic mucosa. PLoS Pathog. 2010;6:e1000902. doi: 10.1371/journal.ppat.1000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas A, Liu YJ, Hao L, Mizoguchi A, Salzman NH, Bevins CL, Kobayashi KS. Induction and rescue of Nod2-dependent Th1-driven granulomatous inflammation of the ileum. Proc Natl Acad Sci USA. 2010;107:14739–14744. doi: 10.1073/pnas.1003363107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogunovic M, Dave SH, Tilstra JS, Chang DT, Harpaz N, Xiong H, Mayer LF, Plevy SE. Enteroendocrine cells express functional Toll-like receptors. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1770–G1783. doi: 10.1152/ajpgi.00249.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cario E, Podolsky DK. Differential alteration in intestinal epithelial cell expression of toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect Immun. 2000;68:7010–7017. doi: 10.1128/iai.68.12.7010-7017.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cario E, Brown D, McKee M, Lynch-Devaney K, Gerken G, Podolsky DK. Commensal-associated molecular patterns induce selective toll-like receptor-trafficking from apical membrane to cytoplasmic compartments in polarized intestinal epithelium. Am J Pathol. 2002;160:165–173. doi: 10.1016/S0002-9440(10)64360-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charrier L, Merlin D. The oligopeptide transporter hPepT1: gateway to the innate immune response. Lab Invest. 2006;86:538–546. doi: 10.1038/labinvest.3700423. [DOI] [PubMed] [Google Scholar]
- Chen LM, Hobbie S, Galan JE. Requirement of CDC42 for Salmonella-induced cytoskeletal and nuclear responses. Science. 1996;274:2115–2118. doi: 10.1126/science.274.5295.2115. [DOI] [PubMed] [Google Scholar]
- Cho JH. The genetics and immunopathogenesis of inflammatory bowel disease. Nat Rev Immunol. 2008;8:458–466. doi: 10.1038/nri2340. [DOI] [PubMed] [Google Scholar]
- Corazziari ES. Intestinal mucus barrier in normal and inflamed colon. J Pediatr Gastroenterol Nutr. 2009;48(Suppl 2):S54–S55. doi: 10.1097/MPG.0b013e3181a117ea. [DOI] [PubMed] [Google Scholar]
- de Repentigny L, Aumont F, Bernard K, Belhumeur P. Characterization of binding of Candida albicans to small intestinal mucin and its role in adherence to mucosal epithelial cells. Infect Immun. 2000;68:3172–3179. doi: 10.1128/iai.68.6.3172-3179.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Smet K, Contreras R. Human antimicrobial peptides: defensins, cathelicidins and histatins. Biotechnol Lett. 2005;27:1337–1347. doi: 10.1007/s10529-005-0936-5. [DOI] [PubMed] [Google Scholar]
- Diamond G, Bevins CL. Beta-defensins: endogenous antibiotics of the innate host defense response. Clin Immunol Immunopathol. 1998;88:221–225. doi: 10.1006/clin.1998.4587. [DOI] [PubMed] [Google Scholar]
- Duchmann R, Kaiser I, Hermann E, Mayet W, Ewe K, Meyer zum Buschenfelde KH. Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease (IBD) Clin Exp Immunol. 1995;102:448–455. doi: 10.1111/j.1365-2249.1995.tb03836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewaschuk JB, Backer JL, Churchill TA, Obermeier F, Krause DO, Madsen KL. Surface expression of Toll-like receptor 9 is upregulated on intestinal epithelial cells in response to pathogenic bacterial DNA. Infect Immun. 2007;75:2572–2579. doi: 10.1128/IAI.01662-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanning AS, Jameson BJ, Jesaitis LA, Anderson JM. The tight junction protein ZO-1 establishes a link between the transmembrane protein occludin and the actin cytoskeleton. J Biol Chem. 1998;273:29745–29753. doi: 10.1074/jbc.273.45.29745. [DOI] [PubMed] [Google Scholar]
- Fasano A, Not T, Wang W, Uzzau S, Berti I, Tommasini A, Goldblum SE. Zonulin, a newly discovered modulator of intestinal permeability, and its expression in coeliac disease. Lancet. 2000;355:1518–1519. doi: 10.1016/S0140-6736(00)02169-3. [DOI] [PubMed] [Google Scholar]
- Fehlbaum P, Rao M, Zasloff M, Anderson GM. An essential amino acid induces epithelial beta-defensin expression. Proc Natl Acad Sci USA. 2000;97:12723–12728. doi: 10.1073/pnas.220424597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming A. On a remarkable bacteriolytic element found in tissues and secretions. Proc R Soc Lond [Biol] 1922;39:306–317. [Google Scholar]
- Furuse M, Hirase T, Itoh M, Nagafuchi A, Yonemura S, Tsukita S. Occludin: a novel integral membrane protein localizing at tight junctions. J Cell Biol. 1993;123:1777–1788. doi: 10.1083/jcb.123.6.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse M, Itoh M, Hirase T, Nagafuchi A, Yonemura S, Tsukita S. Direct association of occludin with ZO-1 and its possible involvement in the localization of occludin at tight junctions. J Cell Biol. 1994;127:1617–1626. doi: 10.1083/jcb.127.6.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse M, Fujita K, Hiiragi T, Fujimoto K, Tsukita S. Claudin-1 and-2: novel integral membrane proteins localizing at tight junctions with no sequence similarity to occludin. J Cell Biol. 1998;141:1539–1550. doi: 10.1083/jcb.141.7.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fyderek K, Strus M, Kowalska-Duplaga K, Gosiewski T, Wedrychowicz A, Jedynak-Wasowicz U, Sladek M, Pieczarkowski S, Adamski P, Kochan P, Heczko PB. Mucosal bacterial microflora and mucus layer thickness in adolescents with inflammatory bowel disease. World J Gastroenterol. 2009;15:5287–5294. doi: 10.3748/wjg.15.5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz T. Defensins and host defense. Science. 1999;286:420–421. doi: 10.1126/science.286.5439.420. [DOI] [PubMed] [Google Scholar]
- Garcia JR, Jaumann F, Schulz S, Krause A, Rodriguez-Jimenez J, Forssmann U, Adermann K, Kluver E, Vogelmeier C, Becker D, Hedrich R, Forssmann WG, Bals R. Identification of a novel, multifunctional beta-defensin (human beta-defensin 3) with specific antimicrobial activity. Its interaction with plasma membranes of Xenopus oocytes and the induction of macrophage chemoattraction. Cell Tissue Res. 2001;306:257–264. doi: 10.1007/s004410100433. [DOI] [PubMed] [Google Scholar]
- Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol. 2001;167:1882–1885. doi: 10.4049/jimmunol.167.4.1882. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Tournebize R, Mavris M, Page AL, Li X, Stark GR, Bertin J, DiStefano PS, Yaniv M, Sansonetti PJ, Philpott DJ. CARD4/Nod1 mediates NF-kappaB and JNK activation by invasive Shigella flexneri. EMBO Rep. 2001;2:736–742. doi: 10.1093/embo-reports/kve155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grutzkau A, Hanski C, Hahn H, Riecken EO. Involvement of M cells in the bacterial invasion of Peyer’s patches: a common mechanism shared by Yersinia enterocolitica and other enteroinvasive bacteria. Gut. 1990;31:1011–1015. doi: 10.1136/gut.31.9.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hase K, Eckmann L, Leopard JD, Varki N, Kagnoff MF. Cell differentiation is a key determinant of cathelicidin LL-37/human cationic antimicrobial protein 18 expression by human colon epithelium. Infect Immun. 2002;70:953–963. doi: 10.1128/iai.70.2.953-963.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hase K, Murakami M, Iimura M, Cole SP, Horibe Y, Ohtake T, Obonyo M, Gallo RL, Eckmann L, Kagnoff MF. Expression of LL-37 by human gastric epithelial cells as a potential host defense mechanism against Helicobacter pylori. Gastroenterology. 2003;125:1613–1625. doi: 10.1053/j.gastro.2003.08.028. [DOI] [PubMed] [Google Scholar]
- Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H, Matsumoto M, Hoshino K, Wagner H, Takeda K, Akira S. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740–745. doi: 10.1038/35047123. [DOI] [PubMed] [Google Scholar]
- Hisamatsu T, Suzuki M, Reinecker HC, Nadeau WJ, McCormick BA, Podolsky DK. CARD15/NOD2 functions as an antibacterial factor in human intestinal epithelial cells. Gastroenterology. 2003;124:993–1000. doi: 10.1053/gast.2003.50153. [DOI] [PubMed] [Google Scholar]
- Horiguchi Y, Senda T, Sugimoto N, Katahira J, Matsuda M. Bordetella bronchiseptica dermonecrotizing toxin stimulates assembly of actin stress fibers and focal adhesions by modifying the small GTP-binding protein rho. J Cell Sci. 1995;108:3243–3251. doi: 10.1242/jcs.108.10.3243. [DOI] [PubMed] [Google Scholar]
- Hoshino K, Takeuchi O, Kawai T, Sanjo H, Ogawa T, Takeda Y, Takeda K, Akira S. Cutting edge: Toll-like receptor 4 (TLR4)-deficient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J Immunol. 1999;162:3749–3752. [PubMed] [Google Scholar]
- Iimura M, Gallo RL, Hase K, Miyamoto Y, Eckmann L, Kagnoff MF. Cathelicidin mediates innate intestinal defense against colonization with epithelial adherent bacterial pathogens. J Immunol. 2005;174:4901–4907. doi: 10.4049/jimmunol.174.8.4901. [DOI] [PubMed] [Google Scholar]
- Islam D, Bandholtz L, Nilsson J, Wigzell H, Christensson B, Agerberth B, Gudmundsson G. Downregulation of bactericidal peptides in enteric infections: a novel immune escape mechanism with bacterial DNA as a potential regulator. Nat Med. 2001;7:180–185. doi: 10.1038/84627. [DOI] [PubMed] [Google Scholar]
- Itoh M, Furuse M, Morita K, Kubota K, Saitou M, Tsukita S. Direct binding of three tight junction-associated MAGUKs, ZO- 1, ZO-2, and ZO-3, with the COOH termini of claudins. J Cell Biol. 1999;147:1351–1363. doi: 10.1083/jcb.147.6.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia HP, Schutte BC, Schudy A, Linzmeier R, Guthmiller JM, Johnson GK, Tack BF, Mitros JP, Rosenthal A, Ganz T, McCray PB., Jr Discovery of new human beta-defensins using a genomics-based approach. Gene. 2001;263:211–218. doi: 10.1016/s0378-1119(00)00569-2. [DOI] [PubMed] [Google Scholar]
- Jones BD, Ghori N, Falkow S. Salmonella typhimurium initiates murine infection by penetrating and destroying the specialized epithelial M cells of the Peyer’s patches. J Exp Med. 1994;180:15–23. doi: 10.1084/jem.180.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalabis J, Rosenberg I, Podolsky DK. Vangl1 protein acts as a downstream effector of intestinal trefoil factor (ITF)/TFF3 signaling and regulates wound healing of intestinal epithelium. J Biol Chem. 2006;281:6434–6441. doi: 10.1074/jbc.M512905200. [DOI] [PubMed] [Google Scholar]
- Kawai T, Akira S. TLR signaling. Cell Death Differ. 2006;13:816–825. doi: 10.1038/sj.cdd.4401850. [DOI] [PubMed] [Google Scholar]
- Keshav S. Paneth cells: leukocyte-like mediators of innate immunity in the intestine. J Leukoc Biol. 2006;80:500–508. doi: 10.1189/jlb.1005556. [DOI] [PubMed] [Google Scholar]
- Kindon H, Pothoulakis C, Thim L, Lynch-Devaney K, Podolsky DK. Trefoil peptide protection of intestinal epithelial barrier function: cooperative interaction with mucin glycoprotein. Gastroenterology. 1995;109:516–523. doi: 10.1016/0016-5085(95)90340-2. [DOI] [PubMed] [Google Scholar]
- Knutson L, Ahrenstedt O, Odlind B, Hallgren R. The jejunal secretion of histamine is increased in active Crohn’s disease. Gastroenterology. 1990;98:849–854. doi: 10.1016/0016-5085(90)90006-m. [DOI] [PubMed] [Google Scholar]
- Kufer TA, Kremmer E, Adam AC, Philpott DJ, Sansonetti PJ. The pattern-recognition molecule Nod1 is localized at the plasma membrane at sites of bacterial interaction. Cell Microbiol. 2008;10:477–486. doi: 10.1111/j.1462-5822.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- Leonova L, Kokryakov VN, Aleshina G, Hong T, Nguyen T, Zhao C, Waring AJ, Lehrer RI. Circular minidefensins and posttranslational generation of molecular diversity. J Leukoc Biol. 2001;70:461–464. [PubMed] [Google Scholar]
- Lyons S, Wang L, Casanova JE, Sitaraman SV, Merlin D, Gewirtz AT. Salmonella typhimurium transcytoses flagellin via an SPI2-mediated vesicular transport pathway. J Cell Sci. 2004;117:5771–5780. doi: 10.1242/jcs.01500. [DOI] [PubMed] [Google Scholar]
- Marchetti M, Sirard JC, Sansonetti P, Pringault E, Kerneis S. Interaction of pathogenic bacteria with rabbit appendix M cells: bacterial motility is a key feature in vivo. Microbes Infect. 2004;6:521–528. doi: 10.1016/j.micinf.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Marra A, Isberg RR. Invasin-dependent and invasin-independent pathways for translocation of Yersinia pseudotuberculosis across the Peyer’s patch intestinal epithelium. Infect Immun. 1997;65:3412–3421. doi: 10.1128/iai.65.8.3412-3421.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastroianni JR, Ouellette AJ. Alpha-defensins in enteric innate immunity: functional Paneth cell alpha-defensins in mouse colonic lumen. J Biol Chem. 2009;284:27848–27856. doi: 10.1074/jbc.M109.050773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlin D, Si-Tahar M, Sitaraman SV, Eastburn K, Williams I, Liu X, Hediger MA, Madara JL. Colonic epithelial hPepT1 expression occurs in inflammatory bowel disease: transport of bacterial peptides influences expression of MHC class 1 molecules. Gastroenterology. 2001;120:1666–1679. doi: 10.1053/gast.2001.24845. [DOI] [PubMed] [Google Scholar]
- Mostov KE. Transepithelial transport of immunoglobulins. Annu Rev Immunol. 1994;12:63–84. doi: 10.1146/annurev.iy.12.040194.000431. [DOI] [PubMed] [Google Scholar]
- Neutra MSP, Kraehenbuhl JP. Role of intestinal M cells in microbial pathogenesis. In: Hecht G, editor. Microbial pathogenesis and the intestinal cell. Washington, DC: ASM; 2003. pp. 23–42. [Google Scholar]
- Nuding S, Fellermann K, Wehkamp J, Stange EF. Reduced mucosal antimicrobial activity in Crohn’s disease of the colon. Gut. 2007;56:1240–1247. doi: 10.1136/gut.2006.118646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusrat A, Giry M, Turner JR, Colgan SP, Parkos CA, Carnes D, Lemichez E, Boquet P, Madara JL. Rho protein regulates tight junctions and perijunctional actin organization in polarized epithelia. Proc Natl Acad Sci USA. 1995;92:10629–10633. doi: 10.1073/pnas.92.23.10629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusrat A, Eichel-Streiber C von, Turner JR, Verkade P, Madara JL, Parkos CA. Clostridium difficile toxins disrupt epithelial barrier function by altering membrane microdomain localization of tight junction proteins. Infect Immun. 2001;69:1329–1336. doi: 10.1128/IAI.69.3.1329-1336.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Britton H, Moran T, Karaliuskas R, Duerr RH, Achkar JP, Brant SR, Bayless TM, Kirschner BS, Hanauer SB, Nunez G, Cho JH. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- Oswald E, Sugai M, Labigne A, Wu HC, Fiorentini C, Boquet P, O’Brien AD. Cytotoxic necrotizing factor type 2 produced by virulent Escherichia coli modifies the small GTP-binding proteins Rho involved in assembly of actin stress fibers. Proc Natl Acad Sci USA. 1994;91:3814–3818. doi: 10.1073/pnas.91.9.3814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellette AJ, Selsted ME. Paneth cell defensins: endogenous peptide components of intestinal host defense. FASEB J. 1996;10:1280–1289. doi: 10.1096/fasebj.10.11.8836041. [DOI] [PubMed] [Google Scholar]
- Pauleau AL, Murray PJ. Role of nod2 in the response of macrophages to Toll-like receptor agonists. Mol Cell Biol. 2003;23:7531–7539. doi: 10.1128/MCB.23.21.7531-7539.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdomo JJ, Gounon P, Sansonetti PJ. Polymorphonuclear leukocyte transmigration promotes invasion of colonic epithelial monolayer by Shigella flexneri. J Clin Invest. 1994;93:633–643. doi: 10.1172/JCI117015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petnicki-Ocwieja T, Hrncir T, Liu YJ, Biswas A, Hudcovic T, Tlaskalova-Hogenova H, Kobayashi KS. Nod2 is required for the regulation of commensal microbiota in the intestine. Proc Natl Acad Sci USA. 2009;106:15813–15818. doi: 10.1073/pnas.0907722106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- Qureshi ST, Lariviere L, Leveque G, Clermont S, Moore KJ, Gros P, Malo D. Endotoxin-tolerant mice have mutations in Toll-like receptor 4 (Tlr4) J Exp Med. 1999;189:615–625. doi: 10.1084/jem.189.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raithel M, Matek M, Baenkler HW, Jorde W, Hahn EG. Mucosal histamine content and histamine secretion in Crohn’s disease, ulcerative colitis and allergic enteropathy. Int Arch Allergy Immunol. 1995;108:127–133. doi: 10.1159/000237129. [DOI] [PubMed] [Google Scholar]
- Sakaguchi T, Kohler H, Gu X, McCormick BA, Reinecker HC. Shigella flexneri regulates tight junction-associated proteins in human intestinal epithelial cells. Cell Microbiol. 2002;4:367–381. doi: 10.1046/j.1462-5822.2002.00197.x. [DOI] [PubMed] [Google Scholar]
- Salzman NH, Ghosh D, Huttner KM, Paterson Y, Bevins CL. Protection against enteric salmonellosis in transgenic mice expressing a human intestinal defensin. Nature. 2003;422:522–526. doi: 10.1038/nature01520. [DOI] [PubMed] [Google Scholar]
- Salzman NH, Underwood MA, Bevins CL. Paneth cells, defensins, and the commensal microbiota: a hypothesis on intimate interplay at the intestinal mucosa. Semin Immunol. 2007;19:70–83. doi: 10.1016/j.smim.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Salzman NH, Hung K, Haribhai D, Chu H, Karlsson-Sjoberg J, Amir E, Teggatz P, Barman M, Hayward M, Eastwood D, Stoel M, Zhou Y, Sodergren E, Weinstock GM, Bevins CL, Williams CB, Bos NA. Enteric defensins are essential regulators of intestinal microbial ecology. Nat Immunol. 2010;11:76–83. doi: 10.1038/ni.1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansonetti PJ, Arondel J, Cantey JR, Prevost MC, Huerre M. Infection of rabbit Peyer’s patches by Shigella flexneri: effect of adhesive or invasive bacterial phenotypes on follicle-associated epithelium. Infect Immun. 1996;64:2752–2764. doi: 10.1128/iai.64.7.2752-2764.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schröder JM. Epithelial antimicrobial peptides: innate local host response elements. Cell Mol Life Sci. 1999;56:32–46. doi: 10.1007/s000180050004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe SM, Qin X, Lu Q, Feketeova E, Palange DC, Dong W, Sheth SU, Lee MA, Reino D, Xu DZ, Deitch EA. Loss of the intestinal mucus layer in the normal rat causes gut injury, but not toxic mesenteric lymph nor lung injury. Shock. 2010;34:475–481. doi: 10.1097/SHK.0b013e3181dc3ff5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonovic I, Rosenberg J, Koutsouris A, Hecht G. Enteropathogenic Escherichia coli dephosphorylates and dissociates occludin from intestinal epithelial tight junctions. Cell Microbiol. 2000;2:305–315. doi: 10.1046/j.1462-5822.2000.00055.x. [DOI] [PubMed] [Google Scholar]
- Sonoda N, Furuse M, Sasaki H, Yonemura S, Katahira J, Horiguchi Y, Tsukita S. Clostridium perfringens enterotoxin fragment removes specific claudins from tight junction strands: evidence for direct involvement of claudins in tight junction barrier. J Cell Biol. 1999;147:195–204. doi: 10.1083/jcb.147.1.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda K, Kaisho T, Akira S. Toll-like receptors. Annu Rev Immunol. 2003;21:335–376. doi: 10.1146/annurev.immunol.21.120601.141126. [DOI] [PubMed] [Google Scholar]
- Tang YQ, Yuan J, Osapay G, Osapay K, Tran D, Miller CJ, Ouellette AJ, Selsted ME. A cyclic antimicrobial peptide produced in primate leukocytes by the ligation of two truncated alpha-defensins. Science. 1999;286:498–502. doi: 10.1126/science.286.5439.498. [DOI] [PubMed] [Google Scholar]
- Tollin M, Bergman P, Svenberg T, Jornvall H, Gudmundsson GH, Agerberth B. Antimicrobial peptides in the first line defence of human colon mucosa. Peptides. 2003;24:523–530. doi: 10.1016/s0196-9781(03)00114-1. [DOI] [PubMed] [Google Scholar]
- Vaishnava S, Behrendt CL, Ismail AS, Eckmann L, Hooper LV. Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc Natl Acad Sci USA. 2008;105:20858–20863. doi: 10.1073/pnas.0808723105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavricka SR, Musch MW, Chang JE, Nakagawa Y, Phanvijhitsiri K, Waypa TS, Merlin D, Schneewind O, Chang EB. hPepT1 transports muramyl dipeptide, activating NF-kappaB and stimulating IL-8 secretion in human colonic Caco2/bbe cells. Gastroenterology. 2004;127:1401–1409. doi: 10.1053/j.gastro.2004.07.024. [DOI] [PubMed] [Google Scholar]
- Wehkamp J, Salzman NH, Porter E, Nuding S, Weichenthal M, Petras RE, Shen B, Schaeffeler E, Schwab M, Linzmeier R, Feathers RW, Chu H, Lima H, Jr, Fellermann K, Ganz T, Stange EF, Bevins CL. Reduced Paneth cell alpha-defensins in ileal Crohn’s disease. Proc Natl Acad Sci USA. 2005;102:18129–18134. doi: 10.1073/pnas.0505256102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson CL, Ouellette AJ, Satchell DP, Ayabe T, Lopez-Boado YS, Stratman JL, Hultgren SJ, Matrisian LM, Parks WC. Regulation of intestinal alpha-defensin activation by the metalloproteinase matrilysin in innate host defense. Science. 1999;286:113–117. doi: 10.1126/science.286.5437.113. [DOI] [PubMed] [Google Scholar]
- Wittchen ES, Haskins J, Stevenson BR. Protein interactions at the tight junction. Actin has multiple binding partners, and ZO-1 forms independent complexes with ZO-2 and ZO-3. J Biol Chem. 1999;274:35179–35185. doi: 10.1074/jbc.274.49.35179. [DOI] [PubMed] [Google Scholar]
- Zhao C, Wang I, Lehrer RI. Widespread expression of beta-defensin hBD-1 in human secretory glands and epithelial cells. FEBS Lett. 1996;396:319–322. doi: 10.1016/0014-5793(96)01123-4. [DOI] [PubMed] [Google Scholar]